Abstract
The purpose of this article is to present the surgical removal of a broken endodontic file from the periapical region of the distal root of a mandibular first molar. The methods of diagnosis and measurement of the distance of the instrument to the adjacent vital structures in the periapical region was done with simple means and in an economical manner.
Keywords: Fractured endodontic instrument, mandibular first molar, periapical surgery
Introduction
Fracture of root canal instruments is one of the most troublesome incidents in endodontic therapy. Several studies focused on factors influencing defects of endodontic instruments after clinical use, and some recommendations were given to minimize the risk of instrument breakage.1-3
It is reported that the prevalence of broken instruments ranges from 0.5% to 5%.4-7 If the broken file impedes adequate cleaning of the canal beyond the obstruction, prognosis might be adversely affected.8 Many a times, this lead to failure of root canal therapy and burdened the patients with anxiety.9,10 Strindberg found a statistically significant 19% higher failure frequency for cases in which there was instrument breakage compared with cases without breakage.11 Therefore, the best option in the management of root canal instrument fracture is removal.12 Several techniques and devices have been used for the removal of broken instruments.13-15 Difficult cases are occasionally encountered in which the separated file cannot be retrieved from the canal.8 Intentionally leaving a fragment in the root canal might be considered when non-surgical removal has been attempted without success.16 In addition, vigorous reduction of the dentinal walls of the root canal space might cause perforation of the canal wall. This can adversely affect the prognosis of teeth.17
Endodontic instruments rarely separate beyond the apical foramen. The fractured segment, always accompanied with bacteria and dentine debris, is a foreign object and might cause inflammation.18,19 Moreover, patients often regard the fractured segment as “a broken needle” and suffer psychologically. Therefore, an attempt to remove the segment from such cases with a surgical approach is often necessary. Before surgery, the precise position and size of the fractured instrument should be understood as well as its relation to the root apex and surrounding anatomic structures.20
The aim of the article is to present a case that used RVG to locate and successfully remove a fractured endodontic instrument partially beyond the apical foramen using a surgical approach.
Case Report
A 32-year-old Indian female patient came to the Department of Conservative Dentistry and Endodontics at our institute with a complaint of pain in the lower left posterior region. On clinical and radio graphical examination, it was diagnosed as a case of irreversible pulpitis due to a deep carious lesion involving the pulp and it was indicated for root canal treatment. Medical history was unremarkable.
After access opening, cleaning and shaping was initiated. Rotary protapers (Dentsply Maillefer, Ballaigues, Switzerland) were used with a 64:1 reduction gear Rotary endodontic hand piece (NSK, Nakanishi, Japan).
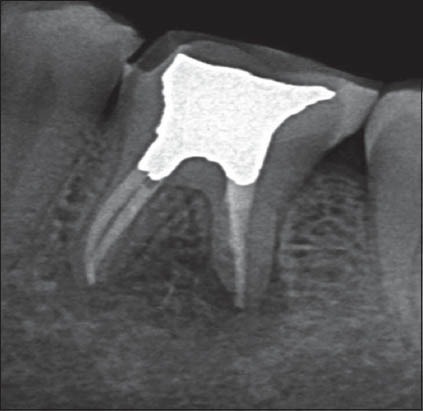
In the process of cleaning and shaping, a 5 mm segment of F2 rotary protaper got fractured in the apical 1/3rd of the distal canal (Figure 1). A decision to remove the instrument non-surgically was undertaken with the consent of the patient.
Figure 1.

Broken instrument in the apical third.
In an attempt to remove the file using microsonics, the file got accidentally pushed into the canal such that 2/3rd of the file was beyond the periapex and 1/3rd inside the canal (Figure 2).
Figure 2.

Instrument got pushed beyond to the periapex measurement with radiographic marker (10 mm).
The tooth was temporized and the patient was informed regarding the mishap and kept under observation for a week. During the recall, the patient gave a positive history for pain on mastication and a decision was made to surgically remove the fragment.
Pre-operative preparations
A 19 gauge wire of a known length (10 mm) was used as a radiographic marker and was taped to the sensor, while taking the RVG. The radiographic marker was then measured on the RVG to calculate any elongation or shortening of the image (Figure 2). The RVG was taken to measure: (1) The exact size of the fractured instrument, (2) the distance from the reference point (Distobuccal cusp) to the apex of the tooth, and (3) the distance from the reference point to the upper border inferior alveolar canal. The actual size of the marker was compared with the size of the marker on the RVG and the above mentioned measurements were made. In our case, the pre-determined length of the radiographic marker coincided with its length on the RVG. Therefore all measurements were directly carried out using the RVG software.
Procedure
The procedure was performed under local anesthesia 2% lignocaine with 1:2,00,000 adrenaline. A crevicular incision was given from the mesial aspect of the mandibular left first pre-molar till the distal aspect of the mandibular left second molar and a distal releasing incision extending into the vestibule was taken to raise a triangular flap. Subperiosteal reflection was done. A 5 mm bony window was prepared through the buccal cortex corresponding to the distal root apex of the molar at the previously calculated length (Figure 3). The instrument was carefully visualized and then removed with a mosquito forceps. A post-operative radiograph was taken to confirm complete removal of the fractured segment (Figure 4). Next, the distal canal was obturated using 6% gutta-percha and 4% accessory cones and AH plus Sealer (Dentsply, Maillefer). The gutta-percha was burnished at the apical end of the distal canal with a hot burnisher. The wound was then curetted, and irrigation was done with normal saline. Demineralised freeze dried bone allograft was used to graft the surgical site and closure was done with 3-0 silk. Patient was prescribed amoxicillin 500 mg/8 h for 7 days, ibuprofen 600 mg/8 h for 3 days, and 0.12% chlorhexidine gluconate mouthwash thrice a day for 7 days. After 7 days, the patient was recalled for suture removal. Routine endodontic therapy was then carried out later under rubber dam application, and the mesial canals were obturated and a post-endodontic restoration was done. At the 6 month recall examination, the mandibular left first molar was asymptomatic with progressive regeneration of the periapical bone (Figure 5).
Figure 3.

Bony window created.
Figure 4.

Instrument removal done.
Figure 5.
Six months postoperative radiograph.
Discussion
Endodontic procedural errors, such as under-filling, over-filling, fractured instruments, and root perforations and ledges, increase the risk of post-treatment disease largely as a result of the inability to eliminate intra-radicular microorganisms from the infected root canal.19 When an instrument fractures during root canal preparation, there are three basic approaches to deal with the problem: (i) Remove it; (ii) bypass and seal it within the root canal; or (iii) block the root canal with it.21-23
A thorough history, clinical examination, and good quality periapical radiographs are essential for pre-operative diagnosis of teeth scheduled to undergo apical surgery.24
Periapical surgery in mandibular molars presents certain technical difficulties such as the close proximity of the apices to the mandibular canal, difficult access to the roots due to their posterior location and their lingual inclination and type and thickness of the buccal plate.25,26
The close proximity of the pathologic process to the mandibular canal can be a difficult surgical problem in terms of protecting this vital structure from damage. Wesson and Gale found a sensory disturbance of variable duration in the lower lip after 20%-21% of mandibular molar procedures.27
Periapical radiography is limited by the fact that information is rendered in only two dimensions. Interpretation is more difficult when the background pattern is complex.28 The use of computed tomography (CT) scans has enabled evaluation of the true extent of periapical lesions and their spatial relationship to important anatomical landmarks.29
The introduction of cone-beam CT represented an important new development in dentomaxillofacial radiology and precipitated a shift from 2 to 3 dimensional data acquisition, image reconstruction, and visualization.30
Conclusion
Precise location of the fractured segment was predicted and removed with the aid of modern gadgets and tooth was successfully treated without any complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None
References
- 1.Shen Y, Haapasalo M, Cheung GS, Peng B. Defects in nickel-titanium instruments after clinical use. Part 1: Relationship between observed imperfections and factors leading to such defects in a cohort study. J Endod. 2009;35(1):129–32. doi: 10.1016/j.joen.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 2.Shen Y, Coil JM, McLean AG, Hemerling DL, Haapasalo M. Defects in nickel-titanium instruments after clinical use. Part 5: Single use from endodontic specialty practices. J Endod. 2009;35(10):1363–7. doi: 10.1016/j.joen.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Shen Y, Coil JM, Haapasalo M. Defects in nickel-titanium instruments after clinical use. Part 3: A 4-year retrospective study from an undergraduate clinic. J Endod. 2009;35(2):193–6. doi: 10.1016/j.joen.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Spili P, Parashos P, Messer HH. The impact of instrument fracture on outcome of endodontic treatment. J Endod. 2005;31(12):845–50. doi: 10.1097/01.don.0000164127.62864.7c. [DOI] [PubMed] [Google Scholar]
- 5.Knowles KI, Hammond NB, Biggs SG, Ibarrola JL. Incidence of instrument separation using LightSpeed rotary instruments. J Endod. 2006;32(1):14–6. doi: 10.1016/j.joen.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Wolcott S, Wolcott J, Ishley D, Kennedy W, Johnson S, Minnich S, et al. Separation incidence of protaper rotary instruments: A large cohort clinical evaluation. J Endod. 2006;32(12):1139–41. doi: 10.1016/j.joen.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Iqbal MK, Kohli MR, Kim JS. A retrospective clinical study of incidence of root canal instrument separation in an endodontics graduate program: A PennEndo database study. J Endod. 2006;32(11):1048–52. doi: 10.1016/j.joen.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Fors UG, Berg JO. A method for the removal of broken endodontic instruments from root canals. J Endod. 1983;9(4):156–9. doi: 10.1016/S0099-2399(83)80038-7. [DOI] [PubMed] [Google Scholar]
- 9.Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498–504. doi: 10.1016/S0099-2399(07)80180-4. [DOI] [PubMed] [Google Scholar]
- 10.Siqueira JF., Jr Aetiology of root canal treatment failure: Why well-treated teeth can fail. Int Endod J. 2001;34(1):1–10. doi: 10.1046/j.1365-2591.2001.00396.x. [DOI] [PubMed] [Google Scholar]
- 11.Strindberg LZ. The dependence of the results of pulp therapy on certain factors. Acta Odontol Scand. 1956;14(Suppl 21):1–156. [Google Scholar]
- 12.Machtou P, Reit C. Non-surgical retreatment. In: Bergenholtz G, Hørsted-Bindslev P, Reit C, editors. Textbook of Endodontology. 1st ed. Oxford: Blackwell Munksgaard Ltd; 2003. pp. 300–10. [Google Scholar]
- 13.Alomairy KH. Evaluating two techniques on removal of fractured rotary nickel-titanium endodontic instruments from root canals: An in vitro study. J Endod. 2009;35(4):559–62. doi: 10.1016/j.joen.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 14.Okiji T. Modified usage of the Masserann kit for removing intracanal broken instruments. J Endod. 2003;29(7):466–7. doi: 10.1097/00004770-200307000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Hülsmann M. Removal of silver cones and fractured instruments using the Canal Finder System. J Endod. 1990;16(12):596–600. doi: 10.1016/s0099-2399(07)80203-2. [DOI] [PubMed] [Google Scholar]
- 16.Hülsmann M, Schinkel I. Influence of several factors on the success or failure of removal of fractured instruments from the root canal. Endod Dent Traumatol. 1999;15(6):252–8. doi: 10.1111/j.1600-9657.1999.tb00783.x. [DOI] [PubMed] [Google Scholar]
- 17.Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: The Toronto study. Phases I and II: Orthograde retreatment. J Endod. 2004;30(9):627–33. doi: 10.1097/01.don.0000129958.12388.82. [DOI] [PubMed] [Google Scholar]
- 18.Kaufman A, Neuman H. Iatrogenic damages caused by dental procedures. Foreign bodies in the oral cavity. Quintessence Int Dent Dig. 1983;14(3):361–6. [PubMed] [Google Scholar]
- 19.Lin LM, Rosenberg PA, Lin J. Do procedural errors cause endodontic treatment failure? J Am Dent Assoc. 2005;136(2):187–93. doi: 10.14219/jada.archive.2005.0140. [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Ni L, Yu C, Shi L, Qin R. Utilizing spiral computerized tomography during the removal of a fractured endodontic instrument lying beyond the apical foramen. Int Endod J. 2010;43(12):1143–51. doi: 10.1111/j.1365-2591.2010.01780.x. [DOI] [PubMed] [Google Scholar]
- 21.Nagai O, Tani N, Kayaba Y, Kodama S, Osada T. Ultrasonic removal of broken instruments in root canals. Int Endod J. 1986;19(6):298–304. doi: 10.1111/j.1365-2591.1986.tb00493.x. [DOI] [PubMed] [Google Scholar]
- 22.Saunders JL, Eleazer PD, Zhang P, Michalek S. Effect of a separated instrument on bacterial penetration of obturated root canals. J Endod. 2004;30(3):177–9. doi: 10.1097/00004770-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Suter B, Lussi A, Sequeira P. Probability of removing fractured instruments from root canals. Int Endod J. 2005;38(2):112–23. doi: 10.1111/j.1365-2591.2004.00916.x. [DOI] [PubMed] [Google Scholar]
- 24.Reit C, Petersson K, Molven O. Textbook of Endodontology. 1st ed. Oxford, UK: Blackwell Publishing Ltd; 2003. Diagnosis of pulpal and periradicular disease; pp. 9–18. [Google Scholar]
- 25.Littner MM, Kaffe I, Tamse A, Dicapua P. Relationship between the apices of the lower molars and mandibular canal – A radiographic study. Oral Surg Oral Med Oral Pathol. 1986;62(5):595–602. doi: 10.1016/0030-4220(86)90326-9. [DOI] [PubMed] [Google Scholar]
- 26.Rud J, Rud V, Munksgaard EC. Periapical healing of mandibular molars after root-end sealing with dentine-bonded composite. Int Endod J. 2001;34(4):285–92. doi: 10.1046/j.1365-2591.2001.00383.x. [DOI] [PubMed] [Google Scholar]
- 27.Wesson CM, Gale TM. Molar apicectomy with amalgam root-end filling: Results of a prospective study in two district general hospitals. Br Dent J. 2003;195(12):707–14. doi: 10.1038/sj.bdj.4810834. [DOI] [PubMed] [Google Scholar]
- 28.Kundel HL, Revesz G. Lesion conspicuity, structured noise, and film reader error. AJR Am J Roentgenol. 1976;126(6):1233–8. doi: 10.2214/ajr.126.6.1233. [DOI] [PubMed] [Google Scholar]
- 29.Cotti E, Vargiu P, Dettori C, Mallarini G. Computerized tomography in the management and follow-up of extensive periapical lesion. Endod Dent Traumatol. 1999;15(4):186–9. doi: 10.1111/j.1600-9657.1999.tb00799.x. [DOI] [PubMed] [Google Scholar]
- 30.Okano T, Harata Y, Sugihara Y, Sakaino R, Tsuchida R, Iwai K, et al. Absorbed and effective doses from cone beam volumetric imaging for implant planning. Dentomaxillofac Radiol. 2009;38(2):79–85. doi: 10.1259/dmfr/14769929. [DOI] [PubMed] [Google Scholar]


