Abstract
Traditional clinical measurements such as probing pocket depth, bleeding on probing, clinical attachment loss; plaque index and radiographs used for periodontal diagnosis are often of limited usefulness as they are indicators of previous periodontal disease rather than present disease activity. A literature search was carried out to find out all the available tests that indicate periodontal disease markers in saliva. All major databases were searched to compile the information on published reports between 1999 and 2014. The list of biomarkers available to date is compiled and presented in a table format. Each biomarker is discussed separately based on the available evidence. Based on the evidence, it can be concluded that several sensitive salivary indicators of periodontitis are available to detect the presence, severity and response to treatment. Further studies are warranted to analyze the sensitivity and reliability of these indicators that might help in developing non-invasive tests that could help in the diagnosis of periodontal disease.
Keywords: Biomarkers, diagnosis, periodontal disease, saliva
Introduction
Saliva, an oral fluid derived from the major and minor salivary glands has been used in the past few decades as a diagnostic fluid. It is secreted mainly by three pairs of major salivary gland and numerous minor salivary glands located at various oral mucosal sites.1 The saliva derives additional constituents from serum, gingival crevicular fluid (GCF), and oral mucosal transudate, making it appealing as a potential diagnostic fluid reflective of circulating levels of these biomarkers in blood. It contains a highly complex mixture of substances and biomarkers that are used for diagnosing local and systemic diseases, or monitoring the effect of treatment.2 The use of saliva as a diagnostic fluid has been hindered, mainly because of our lack of understanding of the biomolecules present in saliva and their relevance to disease etiology, combined with the lack of high-sensitivity detection systems. Currently, with improved efficiency and accuracy of the technology, salivary diagnostics has been made into a clinical and commercial reality. Also collection of saliva is safe, non-invasive, and simple, and can be collected repeatedly with minimum discomfort to the patient.
Periodontitis is a multifactorial chronic non-reversible inflammatory disease affecting the supporting structures of dentition, initiated and propagated through a complex interaction between periopathogens and the host defense system.3 It starts with a microbial infection, followed by a host mediated destruction of periodontal tissues caused by hyper activity of leukocytes and generation of cytokines, eicosanoids and matrix metalloproteinases.3-5 Clinically, the disease progress with loss of attachment to root surface, formation of a deep pocket, alveolar bone resorption, and subsequent loss of tooth. It is the most common disease affecting the oral cavity after dental caries and the major cause of tooth loss, thereby affecting the quality of individual’s life. Therefore, early diagnosis and control of the disease is the paramount goal for clinicians.6
Traditional clinical measurements, such as probing pocket depth, bleeding on probing, and clinical attachment loss, which are used for periodontal diagnosis, are often of only limited usefulness because they are indicators of previous periodontal disease rather than present disease activity.7 Knowing the disease activity might help in early intervention in patients with the disease. This review of the literature focuses the attention on the biochemical markers in saliva that appear to be promising in the future for periodontal diagnosis, as well as some contemporary diagnostic tests available.
Materials and Methods
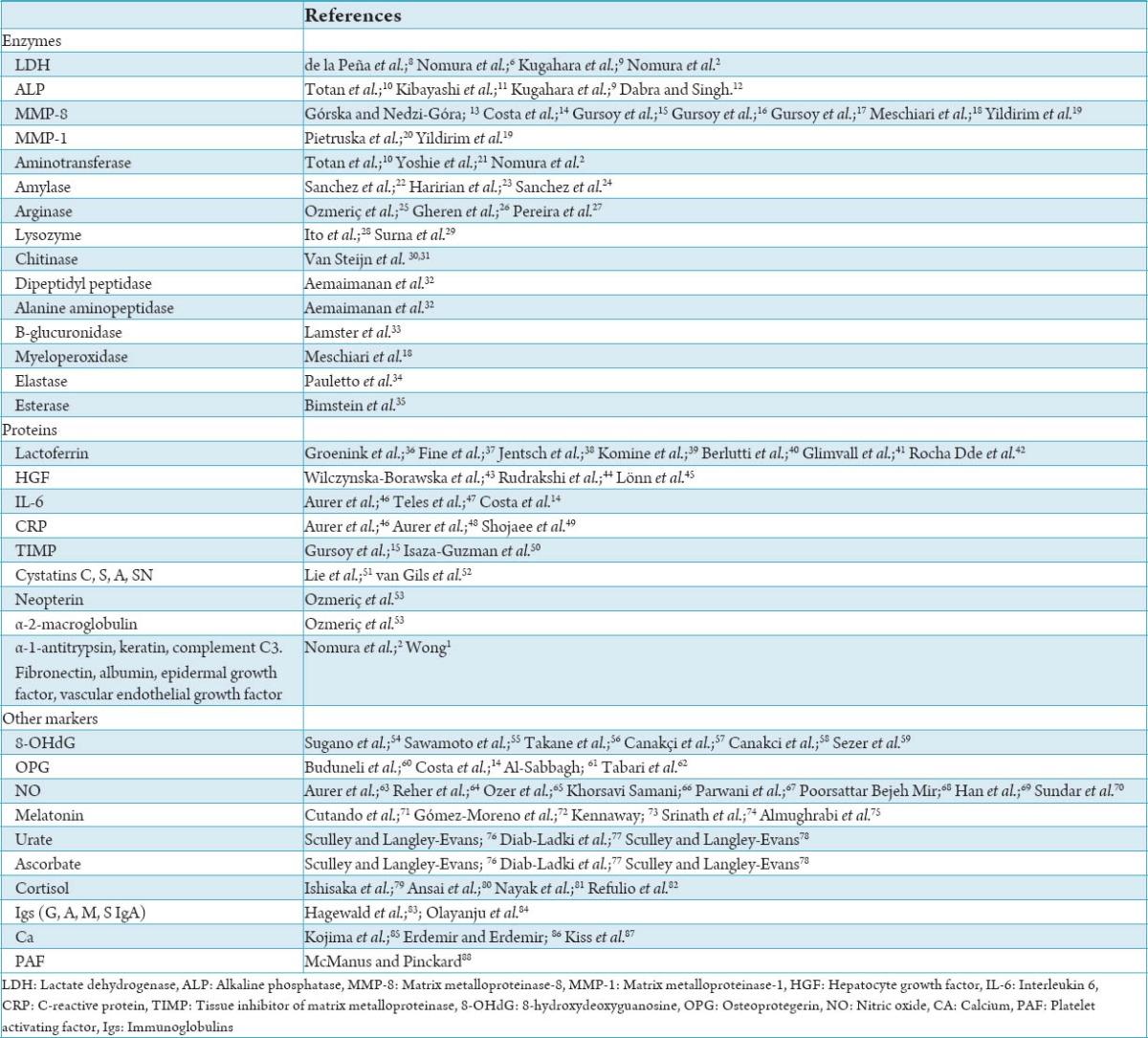
Two authors independently searched the Medline, EMBASE, Cochrane Library, Web of Science, Google Scholar and Scopus databases for relevant studies. The search was carried out by using a combined text and the MeSH search strategies: Using the key words “saliva” or “salivary” and “biomarker” and “periodontitis” or “diagnostic or prognostic indicator.” Publications in English between 1999 and 2014, which estimated saliva as a marker in the diagnosis, assessment of the severity or response to treatment is included. Due to the large number of markers used and the lack of a sufficient number of studies dealing with each maker, the accuracy and predictability of the marker is not considered in this systematic review. The markers are listed in a table with relevant references (Table 1).
Table 1.
Salivary biomarkers in periodontal diseases.
Lactate dehydrogenase
Lactate dehydrogenase (LDH) is a ubiquitous enzyme that plays a significant role in the clinical diagnosis of pathologic processes. Salivary LDH was found to be the most useful enzyme for the screening of periodontitis. Studies showed increased LDH activity in the saliva of subjects with increased probing depth than in individuals with healthy periodontium.89 Among the LDH isoenzymes, LDH4 and LDH5 dominated in whole saliva samples and are predominantly produced by gingival fibroblasts.90 A study by Nomura et al.6 showed that LDH4 and LDH5 were dominant in samples of whole saliva and can be used as a parameter for the screening of periodontal disease. A reduction in salivary LDH was observed in a study after ultrasonic scaling and could be used as a prognostic indicator.8 Salivary LDH has also been used as a screening test to detect the presence of periodontitis in pregnant women.9 The predictive value of periodontal disease progression by assessment of salivary LDH and the total count of Porphyromonas gingivalis, Prevotella intermedia was also established by Nomura et al.2 Yoshie et al21 showed that salivary LDH levels reflect inflammation and destruction of periodontal tissue, suggesting it as a clinically useful marker following periodontal therapy.
Matrix metalloproteinase
Matrix metalloproteinase (MMP) are zinc-dependent endopeptidases and a leading enzyme in degradation of extracellular collagen matrix. They are derived mainly from polymorphonuclear leukocytes during acute stages of periodontal disease.91 The specific proteolytic enzyme secreted by neutrophils and macrophages, the Collagenase-2 also called MMP-8 plays an important role in the pathogenesis of periodontal disease.15,92 MMP is the most potent proteinase to initiate the destruction of Type I and III collagen.15 This critical feature makes MMP-8 important in the pathogenesis of periodontal disease. MMP-8 is up-regulated not only in affected tissues, but also in the secreted, disease affected oral fluids such as saliva and GCF due to the permeability of the sulcular epithelium. Salivary MMP-8 have been found to be four times higher in subjects with periodontitis.93 This indicates that elevated levels of MMP-8 is reflective of the collagen degradation phase of periodontitis and may be useful for monitoring disease activity.93,94 Ramseier et al.95 showed that a combination of salivary MMP-8 and certain anaerobic periodontal pathogens such as P. gingivalis or Treponema denticola present in subgingival biofilms could predict the status of periodontal disease.
Esterase
Levels of salivary esterase has been found higher in periodontitis patient than in healthy subjects.35,96 Furthermore, a positive correlation between salivary esterase and formation of calculus was found.97 Esterase levels were reduced after periodontal treatment. Hence, monitoring esterase levels may be indicative of efficacy of periodontal treatment.98
Lysozyme
Lysozyme activity in saliva combats plaque accumulation, which is the main culprit of periodontal disease.99-101 Therefore, reduced levels of this enzyme may be suggestive of future periodontal disease.29
Chitinase
Chitinase plays a role in the defense against chitin containing pathogens. Studies showed that this enzyme was raised in the saliva of periodontitis patients and decreased after treatment.30
Aspartate aminotransferase
Studies demonstrated the usefulness of the levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), in the diagnosis, prognosis, and treatment of periodontal disease.6,10 Moreover, they also showed that salivary AST, ALT and LDH levels were significantly decreased after oral prophylaxis.21 Nomura et al.2 evaluated AST, ALT and LDH levels in patients with treated periodontitis and progressive periodontitis. The levels of these biomarkers tended to be higher in subjects who developed periodontitis. They concluded that ALT and P. gingivalis combination is the most promising diagnostic tool for predicting periodontal disease progression.
Alkaline phosphatase
Alkaline phosphatase (ALP) has also been used as a possible indicator for gingival inflammation and bone resorption. It has been found that untreated adult periodontitis exhibited higher level of ALP in whole saliva than in healthy controls.9-12
Lactoferrin
Lactoferrin was intensely up-regulated in mucosal secretions during gingival inflammation and also detected at a high concentration in saliva of patients with periodontal disease compared with healthy patients.36
Cysteine
Cystatins are cysteine protease inhibitors that can modulate tissue destruction in periodontal diseases. Volatile sulphur compounds seem to be directly involved in the pathogenesis and maintenance of periodontal tissue lesions. The concentration of some of the sulfur compounds such as cysteine, cysteinylglycine, and glutathione is significantly higher in periodontitis patients.102 The increase of cysteine in periodontitis could be related to some proteolytic activity of bacteria in the oral cavity. The increased concentration of these sulfur compounds present in saliva of patients and their strong correlation with the periodontal probing pocket depth, make these molecules suitable as markers for the severity of periodontitis.103 An increased cystatin activity in whole saliva of gingivitis and periodontitis subjects was reported by enhanced synthesis of some acinar proteins.104,105 The cysteine level showed a significant reduction in whole saliva after periodontal treatment.106 Studies have revealed that smoking is associated with lower cystatin activity and output of Cystatin C increased during gingival inflammation.51,52
C-reactive protein
C-reactive protein (CRP), produced by liver, is a systemic marker released during acute phase of an inflammatory response. Circulating CRP reaches saliva via GCF or salivary glands. Studies reported high levels of CRP in association with chronic and aggressive periodontal diseases.107,108 Various observations were made which revealed that higher the levels of CRP, the more severe are the periodontal disease. In addition, elevated serum CRP is a strong independent risk factor for the development of cardiovascular disease (CVD), which establishes a link with periodontal disease. Therefore, salivary CRP may represent a novel method for diagnosing and monitoring CVD and periodontal diseases.
Epithelial keratins
Along with other constituents, saliva contains epithelial cells from the lining of the oral cavity, but input of crevicular or pocket epithelial cells to the total number of salivary epithelial cells is not known.109 McLaughlin et al.110 studied the keratin level in GCF and demonstrated that the keratin concentration was significantly higher at sites exhibiting signs of periodontitis compared with healthy sites.
Platelet activating factor
A correlation have been found between salivary platelet activating factor, a potent phospholipid inflammatory mediator, level and the extent of periodontal disease and post-treatment.111
Hepatocyte growth factor
Ohshima et al.112 demonstrated a correlation between salivary hepatocyte growth factor (HGF) level and the number of deep pockets exceeding 4 mm.112 HGF acts as mitogen and antiapoptic factor for various kinds of epithelial cells. Fibronectin is a glycoprotein, which mediates adhesion between cells. P. gingivalis fimbriae bind to salivary fibronectin resulting in reduced salivary fibronectin in periodontitis.44,45
Osteoprotegerin
Osteoprotegerin (OPG) is a glycoprotein that inhibits osteoclast differentiation and promoting bone-resorption. The salivary receptor activator of nuclear factor kappa-B ligand/OPG ratio may be helpful in the screening and diagnosis of periodontitis.62 OPG concentrations were elevated in patients with periodontitis.14
8-hydroxydeoxyguanosine
The neutrophils play a central role in the initial host inflammatory response to the periodontal pathogens, which leads to enhanced oxidative stress. Oxidative stress induces DNA damage, including oxidation of nucleosides. 8-hydroxydeoxyguanosine (8-OHdG) is an oxidized nucleoside that is excreted in the bodily fluids with DNA. Takane et al.113 have demonstrated that the mean 8-OHdG level in saliva is a useful marker to screen periodontal disease. The level of 8-OHdG can be also used as a prognostic indicator to monitor the progression of periodontal disease.56 Canakçi et al.57,58 studied the 8-OHdG levels in saliva and mitochondrial DNA deletions in gingival tissue of patients with chronic periodontitis. They established that the salivary 8-OHdG level may signify premature oxidative mitochondrial DNA damage in diseased gingival tissue and could serve as a marker of periodontitis. The 8-OHdG levels in saliva reflect the load of periodontal pathogens and could be a useful biomarker for assessing periodontal status accurately, and for evaluating the efficacy of periodontal treatment.55,59
Nitric oxide
Nitric oxide (NO), which is synthesized from L-arginine by NO synthase, plays a protective role in infectious diseases. NO has been linked to etiopathogenesis of inflammatory periodontal disease and is expressed in saliva.114 Salivary NO levels can be utilized as a good indicator of the inflammatory status of the periodontium, and evaluating its levels in saliva by Griess reaction on a photoelectric colorimeter is a reliable, accurate and faster method to estimate the level of inflammation in periodontal tissues.67,69 A higher level of salivary NO was observed in patients with periodontitis in comparison to the healthy individuals and can be used as a valuable screening tool for periodontitis.66,68
Immunoglobulin
Immunoglobulins (Igs) have an influence on oral microbiota as they interfere in adherence and bacterial metabolism. Higher concentrations of Ig A, Ig G, and Ig M have been found in periodontal disease as compared with healthy patients83 and their concentration drops significantly following treatment.115
Melatonin
Melatonin is a hormone, which is involved in the control of the circadian rhythm, but also acts as an antioxidant and immune modulator.116 Periodontitis may be triggered by a shortage of antioxidants to balance increased oxidative stress. Melatonin acts as an antioxidative, anti-inflammatory, and bone-preserving agent suggesting a role in periodontal disease.117 Studies have shown decreased salivary melatonin levels in periodontitis patients.71,74,118 Salivary melatonin levels may be related to periodontal inflammation possibly due to its antioxidant abilities, and its estimation in saliva act as a risk indicator for the severity of periodontal disease.119
Cortisol
Stress has been advocated as a risk factor for periodontitis. Studies showed a positive relationship between periodontitis and the cortisol level in saliva. Elevated levels of serum cortisol associated with stress exert an inhibition on the immune response to inflammation. Salivary cortisol levels were used to evaluate the role of stress in periodontal disease.80,120,121
Calcium
Calcium (Ca) ion present in saliva has been intensively studied for its correlation with periodontal disease. Elevated levels were correlated with good dental health in young subjects, but no relation was detected with periodontal disease or bone loss as measured from dental radiographs.122 However in another study, Ca and Ca to phosphate ratio were higher in periodontitis patients compared with controls.123 The authors concluded that the high level of Ca in saliva was characteristic of periodontitis.
Bacteria
Periodontitis is an inflammatory disease initiated through interactions with colonizing of periodontal pathogens subgingivally.124 Longitudinal studies have evaluated periodontal pathogen counts in saliva and their connection to periodontal disease. P. gingivalis, Actinobacillus actinomycetemcomitans, Tannerella forsythia, P. intermedia, and T. denticola have been attributed as prognostic biomarkers for disease progression.125,126 However, these studies did not specify, which bacterial species can be used for identification of individuals at risk of disease progression. Saygun et al.127 reported that salivary counts of P. gingivalis, T. forsythia and P. intermedia appear to have the potential to identify the presence of periodontitis.127 Similarly, von Troil-Lindén et al.128 studied the salivary levels of A. actinomycetemcomitans, P. gingivalis, P. intermedia, Campylobacter rectus, and Peptostreptococcus micros and related their levels to clinical periodontal status in 40 subjects with varying degrees of periodontitis. Furthermore, Nomura et al.2 studied the salivary counts of periodontal bacteria in patients with treated periodontitis and progressive periodontitis and reported statistically significant increase in P. gingivalis and P. intermedia levels in progressive periodontitis group. Conversely, T. forsythia did not show the same increase. Association between the gingivitis and the presence of Mycoplasma species in saliva has also been reported.129 Association between oral microbial levels and Plaque and gingival index scores were reported, and it was concluded that the test can serve as an indicator of gingival inflammation. The existence of bacteria in saliva provide information about the bacterial challenge by periodontal tissue, in the initiation of disease and tissue response.130
Conclusion
Saliva, an exocrine secretion of the salivary glands, consists of water, electrolytes, enzymes, Ig, mucosal glycoproteins and numerous antimicrobial proteins, growth factors and regulatory peptides.131 Development of innovative diagnostic tests to detect active phases of periodontal disease and to identify individuals at higher risk for future disease occurrence is the focus of numerous clinical investigations. With the advent of highly sensitive techniques, traces of markers can be accurately established in saliva. Saliva contains locally and systemically derived mediators of periodontal disease, including pathogens, host-response, and bone-specific markers. Most biomarkers in GCF and saliva are indicators of inflammatory events that precede the destruction of the alveolar bone.132 As a diagnostic fluid, saliva offers distinctive advantages over serum because it can be collected non-invasively. With the advantages of an easy, safe, cost-effective, and non-invasive diagnostic approach, saliva shows a high potential for monitoring periodontal disease. New developments in proteomics of saliva and gene transfer technologies applied to the salivary glands will facilitate development of biomarkers with diagnostic and/or prognostic value.
Footnotes
Source of Support: Nil
Conflict of Interest: None
References
- 1.Wong DT. Salivary diagnostics powered by nanotechnologies, proteomics and genomics. J Am Dent Assoc. 2006;137(3):313–21. doi: 10.14219/jada.archive.2006.0180. [DOI] [PubMed] [Google Scholar]
- 2.Nomura Y, Shimada Y, Hanada N, Numabe Y, Kamoi K, Sato T, et al. Salivary biomarkers for predicting the progression of chronic periodontitis. Arch Oral Biol. 2012;57(4):413–20. doi: 10.1016/j.archoralbio.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 3.Bascones A, Noronha S, Gómez M, Mota P, Gónzalez Moles MA, Villarroel Dorrego M. Tissue destruction in periodontitis: Bacteria or cytokines fault? Quintessence Int. 2005;36(4):299–306. [PubMed] [Google Scholar]
- 4.Nussbaum G, Shapira L. How has neutrophil research improved our understanding of periodontal pathogenesis? J Clin Periodontol. 2011;38(Suppl 11):49–59. doi: 10.1111/j.1600-051X.2010.01678.x. [DOI] [PubMed] [Google Scholar]
- 5.Preshaw PM, Taylor JJ. How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis? J Clin Periodontol. 2011;38(Suppl 11):60–84. doi: 10.1111/j.1600-051X.2010.01671.x. [DOI] [PubMed] [Google Scholar]
- 6.Nomura Y, Tamaki Y, Tanaka T, Arakawa H, Tsurumoto A, Kirimura K, et al. Screening of periodontitis with salivary enzyme tests. J Oral Sci. 2006;48(4):177–83. doi: 10.2334/josnusd.48.177. [DOI] [PubMed] [Google Scholar]
- 7.Sexton WM, Lin Y, Kryscio RJ, Dawson DR, 3rd, Ebersole JL, Miller CS. Salivary biomarkers of periodontal disease in response to treatment. J Clin Periodontol. 2011;38(5):434–41. doi: 10.1111/j.1600-051X.2011.01706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de la Peña VA, Dios PD, Rodríguez-Nuñez I, Rodríguez-Segade S. Effect of ultrasonic scaling on salivary lactate dehydrogenase. Am J Dent. 2005;18(2):113–5. [PubMed] [Google Scholar]
- 9.Kugahara T, Shosenji Y, Ohashi K. Screening for periodontitis in pregnant women with salivary enzymes. J Obstet Gynaecol Res. 2008;34(1):40–6. doi: 10.1111/j.1447-0756.2007.00681.x. [DOI] [PubMed] [Google Scholar]
- 10.Totan A, Greabu M, Totan C, Spinu T. Salivary aspartate aminotransferase, alanine aminotransferase and alkaline phosphatase: Possible markers in periodontal diseases? Clin Chem Lab Med. 2006;44(5):612–5. doi: 10.1515/CCLM.2006.096. [DOI] [PubMed] [Google Scholar]
- 11.Kibayashi M, Tanaka M, Nishida N, Kuboniwa M, Kataoka K, Nagata H, et al. Longitudinal study of the association between smoking as a periodontitis risk and salivary biomarkers related to periodontitis. J Periodontol. 2007;78(5):859–67. doi: 10.1902/jop.2007.060292. [DOI] [PubMed] [Google Scholar]
- 12.Dabra S, Singh P. Evaluating the levels of salivary alkaline and acid phosphatase activities as biochemical markers for periodontal disease: A case series. Dent Res J (Isfahan) 2012;9(1):41–5. doi: 10.4103/1735-3327.92942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Górska R, Nedzi-Góra M. The effects of the initial treatment phase and of adjunctive low-dose doxycycline therapy on clinical parameters and MMP-8, MMP-9, and TIMP-1 levels in the saliva and peripheral blood of patients with chronic periodontitis. Arch Immunol Ther Exp (Warsz) 2006;54(6):419–26. doi: 10.1007/s00005-006-0047-6. [DOI] [PubMed] [Google Scholar]
- 14.Costa PP, Trevisan GL, Macedo GO, Palioto DB, Souza SL, Grisi MF, et al. Salivary interleukin-6, matrix metalloproteinase-8, and osteoprotegerin in patients with periodontitis and diabetes. J Periodontol. 2010;81(3):384–91. doi: 10.1902/jop.2009.090510. [DOI] [PubMed] [Google Scholar]
- 15.Gursoy UK, Könönen E, Pradhan-Palikhe P, Tervahartiala T, Pussinen PJ, Suominen-Taipale L, et al. Salivary MMP-8, TIMP-1, and ICTP as markers of advanced periodontitis. J Clin Periodontol. 2010;37(6):487–93. doi: 10.1111/j.1600-051X.2010.01563.x. [DOI] [PubMed] [Google Scholar]
- 16.Gursoy UK, Könönen E, Pussinen PJ, Tervahartiala T, Hyvärinen K, Suominen AL, et al. Use of host- and bacteria-derived salivary markers in detection of periodontitis: A cumulative approach. Dis Markers. 2011;30(6):299–305. doi: 10.3233/DMA-2011-0788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gursoy UK, Könönen E, Huumonen S, Tervahartiala T, Pussinen PJ, Suominen AL, et al. Salivary type I collagen degradation end-products and related matrix metalloproteinases in periodontitis. J Clin Periodontol. 2013;40(1):18–25. doi: 10.1111/jcpe.12020. [DOI] [PubMed] [Google Scholar]
- 18.Meschiari CA, Marcaccini AM, Santos Moura BC, Zuardi LR, Tanus-Santos JE, Gerlach RF. Salivary MMPs, TIMPs, and MPO levels in periodontal disease patients and controls. Clin Chim Acta. 2013;421:140–6. doi: 10.1016/j.cca.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Yildirim E, Kormi I, Basoglu ÖK, Gürgün A, Kaval B, Sorsa T, et al. Periodontal health and serum, saliva matrix metalloproteinases in patients with mild chronic obstructive pulmonary disease. J Periodontal Res. 2013;48(3):269–75. doi: 10.1111/jre.12004. [DOI] [PubMed] [Google Scholar]
- 20.Pietruska M, Pietruski J, Skurska A, Bernaczyk A, Zak J, Zelazowska B, et al. Assessment of aprotinin influence on periodontal clinical status and matrix metalloproteinases 1, 2 and their tissue inhibitors saliva concentrations in patients with chronic periodontitis. Adv Med Sci. 2009;54(2):239–46. doi: 10.2478/v10039-009-0027-2. [DOI] [PubMed] [Google Scholar]
- 21.Yoshie H, Tai H, Kobayashi T, Oda-Gou E, Nomura Y, Numabe Y, et al. Salivary enzyme levels after scaling and interleukin-1 genotypes in Japanese patients with chronic periodontitis. J Periodontol. 2007;78(3):498–503. doi: 10.1902/jop.2007.060216. [DOI] [PubMed] [Google Scholar]
- 22.Sánchez GA, Miozza V, Delgado A, Busch L. Determination of salivary levels of mucin and amylase in chronic periodontitis patients. J Periodontal Res. 2011;46(2):221–7. doi: 10.1111/j.1600-0765.2010.01332.x. [DOI] [PubMed] [Google Scholar]
- 23.Haririan H, Bertl K, Laky M, Rausch WD, Böttcher M, Matejka M, et al. Salivary and serum chromogranin A and a-amylase in periodontal health and disease. J Periodontol. 2012;83(10):1314–21. doi: 10.1902/jop.2012.110604. [DOI] [PubMed] [Google Scholar]
- 24.Sánchez GA, Miozza VA, Delgado A, Busch L. Relationship between salivary mucin or amylase and the periodontal status. Oral Dis. 2013;19(6):585–91. doi: 10.1111/odi.12039. [DOI] [PubMed] [Google Scholar]
- 25.Ozmeriç N, Elgün S, Uraz A. Salivary arginase in patients with adult periodontitis. Clin Oral Investig. 2000;4(1):21–4. doi: 10.1007/s007840050108. [DOI] [PubMed] [Google Scholar]
- 26.Gheren LW, Cortelli JR, Rodrigues E, Holzhausen M, Saad WA. Periodontal therapy reduces arginase activity in saliva of patients with chronic periodontitis. Clin Oral Investig. 2008;12(1):67–72. doi: 10.1007/s00784-007-0146-8. [DOI] [PubMed] [Google Scholar]
- 27.Pereira AL, Cortelli SC, Aquino DR, Franco GC, Cogo K, Rodrigues E, et al. Reduction of salivary arginine catabolic activity through periodontal therapy. Quintessence Int. 2012;43(9):777–87. [PubMed] [Google Scholar]
- 28.Ito T, Komiya-Ito A, Arataki T, Furuya Y, Yajima Y, Yamada S, et al. Relationship between antimicrobial protein levels in whole saliva and periodontitis. J Periodontol. 2008;79(2):316–22. doi: 10.1902/jop.2008.070348. [DOI] [PubMed] [Google Scholar]
- 29.Surna A, Kubilius R, Sakalauskiene J, Vitkauskiene A, Jonaitis J, Saferis V, et al. Lysozyme and microbiota in relation to gingivitis and periodontitis. Med Sci Monit. 2009;15(2):CR66–73. [PubMed] [Google Scholar]
- 30.Van Steijn GJ, Amerongen AV, Veerman EC, Kasanmoentalib S, Overdijk B. Effect of periodontal treatment on the activity of chitinase in whole saliva of periodontitis patients. J Periodontal Res. 2002;37(4):245–9. doi: 10.1034/j.1600-0765.2002.00330.x. [DOI] [PubMed] [Google Scholar]
- 31.Van Steijn GJ, Amerongen AV, Veerman EC, Kasanmoentalib S, Overdijk B. Chitinase in whole and glandular human salivas and in whole saliva of patients with periodontal inflammation. Eur J Oral Sci. 1999;107(5):328–37. doi: 10.1046/j.0909-8836.1999.eos107503.x. [DOI] [PubMed] [Google Scholar]
- 32.Aemaimanan P, Sattayasai N, Wara-aswapati N, Pitiphat W, Suwannarong W, Prajaneh S, et al. Alanine aminopeptidase and dipeptidyl peptidase IV in saliva of chronic periodontitis patients. J Periodontol. 2009;80(11):1809–14. doi: 10.1902/jop.2009.090233. [DOI] [PubMed] [Google Scholar]
- 33.Lamster IB, Kaufman E, Grbic JT, Winston LJ, Singer RE. Beta-glucuronidase activity in saliva: Relationship to clinical periodontal parameters. J Periodontol. 2003;74(3):353–9. doi: 10.1902/jop.2003.74.3.353. [DOI] [PubMed] [Google Scholar]
- 34.Pauletto NC, Liede K, Nieminen A, Larjava H, Uitto VJ. Effect of cigarette smoking on oral elastase activity in adult periodontitis patients. J Periodontol. 2000;71(1):58–62. doi: 10.1902/jop.2000.71.1.58. [DOI] [PubMed] [Google Scholar]
- 35.Bimstein E, Small PA, Jr, Magnusson I. Leukocyte esterase and protein levels in saliva, as indicators of gingival and periodontal diseases in children. Pediatr Dent. 2004;26(4):310–5. [PubMed] [Google Scholar]
- 36.Groenink J, Walgreen-Weterings E, Nazmi K, Bolscher JG, Veerman EC, van Winkelhoff AJ, et al. Salivary lactoferrin and low-Mr mucin MG2 in Actinobacillus actinomycetemcomitans-associated periodontitis. J Clin Periodontol. 1999;26(5):269–75. doi: 10.1034/j.1600-051x.1999.260501.x. [DOI] [PubMed] [Google Scholar]
- 37.Fine DH, Furgang D, Beydouin F. Lactoferrin iron levels are reduced in saliva of patients with localized aggressive periodontitis. J Periodontol. 2002;73(6):624–30. doi: 10.1902/jop.2002.73.6.624. [DOI] [PubMed] [Google Scholar]
- 38.Jentsch H, Sievert Y, Göcke R. Lactoferrin and other markers from gingival crevicular fluid and saliva before and after periodontal treatment. J Clin Periodontol. 2004;31(7):511–4. doi: 10.1111/j.1600-051X.2004.00512.x. [DOI] [PubMed] [Google Scholar]
- 39.Komine K, Kuroishi T, Ozawa A, Komine Y, Minami T, Shimauchi H, et al. Cleaved inflammatory lactoferrin peptides in parotid saliva of periodontitis patients. Mol Immunol. 2007;44(7):1498–508. doi: 10.1016/j.molimm.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 40.Berlutti F, Pilloni A, Pietropaoli M, Polimeni A, Valenti P. Lactoferrin and oral diseases: Current status and perspective in periodontitis. Ann Stomatol (Roma) 2011;2(3-4):10–8. [PMC free article] [PubMed] [Google Scholar]
- 41.Glimvall P, Wickström C, Jansson H. Elevated levels of salivary lactoferrin, a marker for chronic periodontitis? J Periodontal Res. 2012;47(5):655–60. doi: 10.1111/j.1600-0765.2012.01479.x. [DOI] [PubMed] [Google Scholar]
- 42.Rocha Dde M, Zenóbio EG, Van Dyke T, Silva KS, Costa FO, Soares RV. Differential expression of salivary glycoproteins in aggressive and chronic periodontitis. J Appl Oral Sci. 2012;20(2):180–5. doi: 10.1590/S1678-77572012000200010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilczynska-Borawska M, Borawski J, Kovalchuk O, Chyczewski L, Mysliwiec M, Stokowska W. Unexpected effect of haemodialysis on salivary hepatocyte growth factor. Nephrol Dial Transplant. 2005;20(12):2869–70. doi: 10.1093/ndt/gfi129. [DOI] [PubMed] [Google Scholar]
- 44.Rudrakshi C, Srinivas N, Mehta DS. A comparative evaluation of hepatocyte growth factor levels in gingival crevicular fluid and saliva and its correlation with clinical parameters in patients with and without chronic periodontitis: A clinico-biochemical study. J Indian Soc Periodontol. 2011;15(2):147–51. doi: 10.4103/0972-124X.84384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lönn J, Johansson CS, Nakka S, Palm E, Bengtsson T, Nayeri F, et al. High concentration but low activity of hepatocyte growth factor in periodontitis. J Periodontol. 2014;85(1):113–22. doi: 10.1902/jop.2013.130003. [DOI] [PubMed] [Google Scholar]
- 46.Aurer A, Aurer-Kozelj J, Stavljenic-Rukavina A, Kalenic S, Ivic-Kardum M, Haban V. Inflammatory mediators in saliva of patients with rapidly progressive periodontitis during war stress induced incidence increase. Coll Antropol. 1999;23(1):117–24. [PubMed] [Google Scholar]
- 47.Teles RP, Likhari V, Socransky SS, Haffajee AD. Salivary cytokine levels in subjects with chronic periodontitis and in periodontally healthy individuals: A cross-sectional study. J Periodontal Res. 2009;44(3):411–7. doi: 10.1111/j.1600-0765.2008.01119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aurer A, Jorgic-Srdjak K, Plancak D, Stavljenic-Rukavina A, Aurer-Kozelj J. Proinflammatory factors in saliva as possible markers for periodontal disease. Coll Antropol. 2005;29(2):435–9. [PubMed] [Google Scholar]
- 49.Shojaee M, Fereydooni Golpasha M, Maliji G, Bijani A, Aghajanpour Mir SM, Mousavi Kani SN. C - reactive protein levels in patients with periodontal disease and normal subjects. Int J Mol Cell Med. 2013;2(3):151–5. [PMC free article] [PubMed] [Google Scholar]
- 50.Isaza-Guzmán DM, Arias-Osorio C, Martínez-Pabón MC, Tobón-Arroyave SI. Salivary levels of matrix metalloproteinase (MMP)-9 and tissue inhibitor of matrix metalloproteinase (TIMP)-1:A pilot study about the relationship with periodontal status and MMP-9(-1562C/T) gene promoter polymorphism. Arch Oral Biol. 2011;56(4):401–11. doi: 10.1016/j.archoralbio.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 51.Lie MA, Loos BG, Henskens YM, Timmerman MF, Veerman EC, van der Velden U, et al. Salivary cystatin activity and cystatin C in natural and experimental gingivitis in smokers and non-smokers. J Clin Periodontol. 2001;28(10):979–84. doi: 10.1034/j.1600-051x.2001.028010979.x. [DOI] [PubMed] [Google Scholar]
- 52.van Gils PC, Brand HS, Timmerman MF, Veerman EC, van der Velden U, van der Weijden GA. Salivary cystatin activity and cystatin C in experimental gingivitis in non-smokers. J Clin Periodontol. 2003;30(10):882–6. doi: 10.1034/j.1600-051x.2003.00394.x. [DOI] [PubMed] [Google Scholar]
- 53.Ozmeriç N, Baydar T, Bodur A, Engin AB, Uraz A, Eren K, et al. Level of neopterin, a marker of immune cell activation in gingival crevicular fluid, saliva, and urine in patients with aggressive periodontitis. J Periodontol. 2002;73(7):720–5. doi: 10.1902/jop.2002.73.7.720. [DOI] [PubMed] [Google Scholar]
- 54.Sugano N, Yokoyama K, Oshikawa M, Kumagai K, Takane M, Tanaka H, et al. Detection of Streptococcus anginosus and 8-hydroxydeoxyguanosine in saliva. J Oral Sci. 2003;45(4):181–4. doi: 10.2334/josnusd.45.181. [DOI] [PubMed] [Google Scholar]
- 55.Sawamoto Y, Sugano N, Tanaka H, Ito K. Detection of periodontopathic bacteria and an oxidative stress marker in saliva from periodontitis patients. Oral Microbiol Immunol. 2005;20(4):216–20. doi: 10.1111/j.1399-302X.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- 56.Takane M, Sugano N, Ezawa T, Uchiyama T, Ito K. A marker of oxidative stress in saliva: Association with periodontally-involved teeth of a hopeless prognosis. J Oral Sci. 2005;47(1):53–7. doi: 10.2334/josnusd.47.53. [DOI] [PubMed] [Google Scholar]
- 57.Canakçi CF, Canakçi V, Tatar A, Eltas A, Sezer U, Ciçek Y, et al. Increased salivary level of 8-hydroxydeoxyguanosine is a marker of premature oxidative mitochondrial DNA damage in gingival tissue of patients with periodontitis. Arch Immunol Ther Exp (Warsz) 2009;57(3):205–11. doi: 10.1007/s00005-009-0026-9. [DOI] [PubMed] [Google Scholar]
- 58.Canakci CF, Cicek Y, Yildirim A, Sezer U, Canakci V. Increased levels of 8-hydroxydeoxyguanosine and malondialdehyde and its relationship with antioxidant enzymes in saliva of periodontitis patients. Eur J Dent. 2009;3(2):100–6. [PMC free article] [PubMed] [Google Scholar]
- 59.Sezer U, Ciçek Y, Canakçi CF. Increased salivary levels of 8-hydroxydeoxyguanosine may be a marker for disease activity for periodontitis. Dis Markers. 2012;32(3):165–72. doi: 10.3233/DMA-2011-0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Buduneli N, Biyikoglu B, Sherrabeh S, Lappin DF. Saliva concentrations of RANKL and osteoprotegerin in smoker versus non-smoker chronic periodontitis patients. J Clin Periodontol. 2008;35(10):846–52. doi: 10.1111/j.1600-051X.2008.01310.x. [DOI] [PubMed] [Google Scholar]
- 61.Al-Sabbagh M, Alladah A, Lin Y, Kryscio RJ, Thomas MV, Ebersole JL, et al. Bone remodeling-associated salivary biomarker MIP-1a distinguishes periodontal disease from health. J Periodontal Res. 2012;47(3):389–95. doi: 10.1111/j.1600-0765.2011.01445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tabari ZA, Azadmehr A, Tabrizi MA, Hamissi J, Ghaedi FB. Salivary soluble receptor activator of nuclear factor kappa B ligand/osteoprotegerin ratio in periodontal disease and health. J Periodontal Implant Sci. 2013;43(5):227–32. doi: 10.5051/jpis.2013.43.5.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aurer A, Aleksic J, Ivic-Kardum M, Aurer J, Culo F. Nitric oxide synthesis is decreased in periodontitis. J Clin Periodontol. 2001;28(6):565–8. doi: 10.1034/j.1600-051x.2001.028006565.x. [DOI] [PubMed] [Google Scholar]
- 64.Reher VG, Zenóbio EG, Costa FO, Reher P, Soares RV. Nitric oxide levels in saliva increase with severity of chronic periodontitis. J Oral Sci. 2007;49(4):271–6. doi: 10.2334/josnusd.49.271. [DOI] [PubMed] [Google Scholar]
- 65.Ozer L, Elgun S, Ozdemir B, Pervane B, Ozmeric N. Arginine-nitric oxide-polyamine metabolism in periodontal disease. J Periodontol. 2011;82(2):320–8. doi: 10.1902/jop.2010.100199. [DOI] [PubMed] [Google Scholar]
- 66.Khorsavi Samani M, Poorsattar Bejeh Mir A, Kashiri M, Gujeq D. Introducing cut-points for salivary nitric oxide to distinguish periodontitis from the normal periodontium. Minerva Stomatol. 2012;61(10):443–8. [PubMed] [Google Scholar]
- 67.Parwani SR, Chitnis PJ, Parwani RN. Salivary nitric oxide levels in inflammatory periodontal disease - a case-control and interventional study. Int J Dent Hyg. 2012;10(1):67–73. doi: 10.1111/j.1601-5037.2011.00508.x. [DOI] [PubMed] [Google Scholar]
- 68.Poorsattar Bejeh Mir A. Does the level of salivary nitric oxide independently estimate to which extent periodontium is affected? Int J Dent Hyg. 2012;10(4):292. doi: 10.1111/j.1601-5037.2011.00535.x. [DOI] [PubMed] [Google Scholar]
- 69.Han DH, Kim MS, Shin HS, Park KP, Kim HD. Association between periodontitis and salivary nitric oxide metabolites among community elderly Koreans. J Periodontol. 2013;84(6):776–84. doi: 10.1902/jop.2012.120237. [DOI] [PubMed] [Google Scholar]
- 70.Sundar NM, Krishnan V, Krishnaraj S, Hemalatha VT, Alam MN. Comparison of the salivary and the serum nitric oxide levels in chronic and aggressive periodontitis: A biochemical study. J Clin Diagn Res. 2013;7(6):1223–7. doi: 10.7860/JCDR/2013/5386.3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cutando A, Galindo P, Gómez-Moreno G, Arana C, Bolaños J, Acuña-Castroviejo D, et al. Relationship between salivary melatonin and severity of periodontal disease. J Periodontol. 2006;77(9):1533–8. doi: 10.1902/jop.2006.050287. [DOI] [PubMed] [Google Scholar]
- 72.Gómez-Moreno G, Cutando-Soriano A, Arana C, Galindo P, Bolaños J, Acuña-Castroviejo D, et al. Melatonin expression in periodontal disease. J Periodontal Res. 2007;42(6):536–40. doi: 10.1111/j.1600-0765.2007.00978.x. [DOI] [PubMed] [Google Scholar]
- 73.Kennaway D. Re: “salivary and gingival crevicular fluid melatonin in periodontal health and disease”. J Periodontol. 2010;81(8):1102. doi: 10.1902/jop.2010.100141. [DOI] [PubMed] [Google Scholar]
- 74.Srinath R, Acharya AB, Thakur SL. Salivary and gingival crevicular fluid melatonin in periodontal health and disease. J Periodontol. 2010;81(2):277–83. doi: 10.1902/jop.2009.090327. [DOI] [PubMed] [Google Scholar]
- 75.Almughrabi OM, Marzouk KM, Hasanato RM, Shafik SS. Melatonin levels in periodontal health and disease. J Periodontal Res. 2013;48(3):315–21. doi: 10.1111/jre.12010. [DOI] [PubMed] [Google Scholar]
- 76.Sculley DV, Langley-Evans SC. Salivary antioxidants and periodontal disease status. Proc Nutr Soc. 2002;61(1):137–43. doi: 10.1079/pns2001141. [DOI] [PubMed] [Google Scholar]
- 77.Diab-Ladki R, Pellat B, Chahine R. Decrease in the total antioxidant activity of saliva in patients with periodontal diseases. Clin Oral Investig. 2003;7(2):103–7. doi: 10.1007/s00784-003-0208-5. [DOI] [PubMed] [Google Scholar]
- 78.Sculley DV, Langley-Evans SC. Periodontal disease is associated with lower antioxidant capacity in whole saliva and evidence of increased protein oxidation. Clin Sci (Lond) 2003;105(2):167–72. doi: 10.1042/CS20030031. [DOI] [PubMed] [Google Scholar]
- 79.Ishisaka A, Ansai T, Soh I, Inenaga K, Yoshida A, Shigeyama C, et al. Association of salivary levels of cortisol and dehydroepiandrosterone with periodontitis in older Japanese adults. J Periodontol. 2007;78(9):1767–73. doi: 10.1902/jop.2007.070044. [DOI] [PubMed] [Google Scholar]
- 80.Ansai T, Soh I, Ishisaka A, Yoshida A, Awano S, Hamasaki T, et al. Determination of cortisol and dehydroepiandrosterone levels in saliva for screening of periodontitis in older Japanese adults. Int J Dent. 2009;2009:280737. doi: 10.1155/2009/280737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nayak SU, Nayak DG, Uppoor AS, Pai KK. Evaluation of cortisol levels in gingival crevicular fluid and saliva in anxious and non-anxious patients with chronic periodontitis. Dent Res J (Isfahan) 2013;10(4):474–81. [PMC free article] [PubMed] [Google Scholar]
- 82.Refulio Z, Rocafuerte M, de la Rosa M, Mendoza G, Chambrone L. Association among stress, salivary cortisol levels, and chronic periodontitis. J Periodontal Implant Sci. 2013;43(2):96–100. doi: 10.5051/jpis.2013.43.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hägewald S, Bernimoulin JP, Köttgen E, Kage A. Salivary IgA subclasses and bacteria-reactive IgA in patients with aggressive periodontitis. J Periodontal Res. 2002;37(5):333–9. doi: 10.1034/j.1600-0765.2002.00337.x. [DOI] [PubMed] [Google Scholar]
- 84.Olayanju OA, Rahamon SK, Joseph IO, Arinola OG. Salivary immunoglobulin classes in Nigerians with periodontitis. J Contemp Dent Pract. 2012;13(2):163–6. doi: 10.5005/jp-journals-10024-1114. [DOI] [PubMed] [Google Scholar]
- 85.Kojima T, Andersen E, Sanchez JC, Wilkins MR, Hochstrasser DF, Pralong WF, et al. Human gingival crevicular fluid contains MRP8 (S100A8) and MRP14 (S100A9), two calcium-binding proteins of the S100 family. J Dent Res. 2000;79(2):740–7. doi: 10.1177/00220345000790020701. [DOI] [PubMed] [Google Scholar]
- 86.Erdemir EO, Erdemir A. The detection of salivary minerals in smokers and non-smokers with chronic periodontitis by the inductively coupled plasma-atomic emission spectrophotometry technique. J Periodontol. 2006;77(6):990–5. doi: 10.1902/jop.2006.050202. [DOI] [PubMed] [Google Scholar]
- 87.Kiss E, Sewon L, Gorzó I, Nagy K. Salivary calcium concentration in relation to periodontal health of female tobacco smokers: A pilot study. Quintessence Int. 2010;41(9):779–85. [PubMed] [Google Scholar]
- 88.McManus LM, Pinckard RN. PAF, a putative mediator of oral inflammation. Crit Rev Oral Biol Med. 2000;11(2):240–58. doi: 10.1177/10454411000110020701. [DOI] [PubMed] [Google Scholar]
- 89.Nagler RM, Lischinsky S, Diamond E, Klein I, Reznick AZ. New insights into salivary lactate dehydrogenase of human subjects. J Lab Clin Med. 2001;137(5):363–9. doi: 10.1067/mlc.2001.114710. [DOI] [PubMed] [Google Scholar]
- 90.Huang JS, Liu TZ, Bhatnagar RS. Creatine kinase and lactate dehydrogenase isoenzyme patterns in cultured normal and pathological gingival fibroblasts. J Formos Med Assoc. 1990;89(2):126–31. [PubMed] [Google Scholar]
- 91.Sodek J, Overall CM. Matrix metalloproteinases in periodontal tissue remodelling. Matrix Suppl. 1992;1:352–62. [PubMed] [Google Scholar]
- 92.Sorsa T, Tjäderhane L, Konttinen YT, Lauhio A, Salo T, Lee HM, et al. Matrix metalloproteinases: Contribution to pathogenesis, diagnosis and treatment of periodontal inflammation. Ann Med. 2006;38(5):306–21. doi: 10.1080/07853890600800103. [DOI] [PubMed] [Google Scholar]
- 93.Miller CS, King CP, Jr, Langub MC, Kryscio RJ, Thomas MV. Salivary biomarkers of existing periodontal disease: A cross-sectional study. J Am Dent Assoc. 2006;137(3):322–9. doi: 10.14219/jada.archive.2006.0181. [DOI] [PubMed] [Google Scholar]
- 94.Todorovic T, Dozic I, Vicente-Barrero M, Ljuskovic B, Pejovic J, Marjanovic M, et al. Article in English, Spanish] Salivary enzymes and periodontal disease. Med Oral Patol Oral Cir Bucal. 2006;11(2):E115–9. [PubMed] [Google Scholar]
- 95.Ramseier CA, Kinney JS, Herr AE, Braun T, Sugai JV, Shelburne CA, et al. Identification of pathogen and host-response markers correlated with periodontal disease. J Periodontol. 2009;80(3):436–46. doi: 10.1902/jop.2009.080480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nakamura M, Slots J. Salivary enzymes. Origin and relationship to periodontal disease. J Periodontal Res. 1983;18(6):559–69. doi: 10.1111/j.1600-0765.1983.tb00393.x. [DOI] [PubMed] [Google Scholar]
- 97.Raus FJ, Tarbet WJ, Miklos FL. Salivary enzymes and calculus formation. J Periodontal Res. 1968;3(3):232–5. doi: 10.1111/j.1600-0765.1968.tb01925.x. [DOI] [PubMed] [Google Scholar]
- 98.Zambon JJ, Nakamura M, Slots J. Effect of periodontal therapy on salivary enzymatic activity. J Periodontal Res. 1985;20(6):652–9. doi: 10.1111/j.1600-0765.1985.tb00850.x. [DOI] [PubMed] [Google Scholar]
- 99.Brandtzaeg P, Mann WV., Jr A comparative study of the lysozyme activity of human gingival pocket fluid, serum, and saliva. Acta Odontol Scand. 1964;22:441–55. doi: 10.3109/00016356409028217. [DOI] [PubMed] [Google Scholar]
- 100.Markkanen H, Syrjänen SM, Alakuijala P. Salivary IgA, lysozyme and beta 2-microglobulin in periodontal disease. Scand J Dent Res. 1986;94(2):115–20. doi: 10.1111/j.1600-0722.1986.tb01374.x. [DOI] [PubMed] [Google Scholar]
- 101.Suomalainen K, Saxén L, Vilja P, Tenovuo J. Peroxidases, lactoferrin and lysozyme in peripheral blood neutrophils, gingival crevicular fluid and whole saliva of patients with localized juvenile periodontitis. Oral Dis. 1996;2(2):129–34. doi: 10.1111/j.1601-0825.1996.tb00213.x. [DOI] [PubMed] [Google Scholar]
- 102.Zappacosta B, Manni A, Persichilli S, Scribano D, Minucci A, Lazzaro D, et al. HPLC analysis of some sulphur compounds in saliva: Comparison between healthy subjects and periodontopathic patients. Clin Chim Acta. 2003;338(1-2):57–60. doi: 10.1016/j.cccn.2003.07.019. [DOI] [PubMed] [Google Scholar]
- 103.Zappacosta B, Manni A, Persichilli S, Boari A, Scribano D, Minucci A, et al. Salivary thiols and enzyme markers of cell damage in periodontal disease. Clin Biochem. 2007;40(9-10):661–5. doi: 10.1016/j.clinbiochem.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 104.Henskens YM, van den Keijbus PA, Veerman EC, Van der Weijden GA, Timmerman MF, Snoek CM, et al. Protein composition of whole and parotid saliva in healthy and periodontitis subjects. Determination of cystatins, albumin, amylase and IgA. J Periodontal Res. 1996;31(1):57–65. doi: 10.1111/j.1600-0765.1996.tb00464.x. [DOI] [PubMed] [Google Scholar]
- 105.Henskens YM, Van der Velden U, Veerman EC, Nieuw Amerongen AV. Cystatin C levels of whole saliva are increased in periodontal patients. Ann N Y Acad Sci. 1993;694:280–2. doi: 10.1111/j.1749-6632.1993.tb18364.x. [DOI] [PubMed] [Google Scholar]
- 106.Henskens YM, van der Weijden FA, van den Keijbus PA, Veerman EC, Timmerman MF, van der Velden U, et al. Effect of periodontal treatment on the protein composition of whole and parotid saliva. J Periodontol. 1996;67(3):205–12. doi: 10.1902/jop.1996.67.3.205. [DOI] [PubMed] [Google Scholar]
- 107.D’Aiuto F, Ready D, Tonetti MS. Periodontal disease and C-reactive protein-associated cardiovascular risk. J Periodontal Res. 2004;39(4):236–41. doi: 10.1111/j.1600-0765.2004.00731.x. [DOI] [PubMed] [Google Scholar]
- 108.Christodoulides N, Mohanty S, Miller CS, Langub MC, Floriano PN, Dharshan P, et al. Application of microchip assay system for the measurement of C-reactive protein in human saliva. Lab Chip. 2005;5(3):261–9. doi: 10.1039/b414194f. [DOI] [PubMed] [Google Scholar]
- 109.Wilton JM, Curtis MA, Gillett IR, Griffiths GS, Maiden MF, Sterne JA, et al. Detection of high-risk groups and individuals for periodontal diseases: Laboratory markers from analysis of saliva. J Clin Periodontol. 1989;16(8):475–83. doi: 10.1111/j.1600-051x.1989.tb02323.x. [DOI] [PubMed] [Google Scholar]
- 110.McLaughlin WS, Kirkham J, Kowolik MJ, Robinson C. Human gingival crevicular fluid keratin at healthy, chronic gingivitis and chronic adult periodontitis sites. J Clin Periodontol. 1996;23(4):331–5. doi: 10.1111/j.1600-051x.1996.tb00554.x. [DOI] [PubMed] [Google Scholar]
- 111.Rasch MS, Mealey BL, Prihoda TJ, Woodard DS, McManus LM. The effect of initial periodontal therapy on salivary platelet-activating factor levels in chronic adult periodontitis. J Periodontol. 1995;66(7):613–23. doi: 10.1902/jop.1995.66.7.613. [DOI] [PubMed] [Google Scholar]
- 112.Ohshima M, Fujikawa K, Akutagawa H, Kato T, Ito K, Otsuka K. Hepatocyte growth factor in saliva: A possible marker for periodontal disease status. J Oral Sci. 2002;44(1):35–9. doi: 10.2334/josnusd.44.35. [DOI] [PubMed] [Google Scholar]
- 113.Takane M, Sugano N, Iwasaki H, Iwano Y, Shimizu N, Ito K. New biomarker evidence of oxidative DNA damage in whole saliva from clinically healthy and periodontally diseased individuals. J Periodontol. 2002;73(5):551–4. doi: 10.1902/jop.2002.73.5.551. [DOI] [PubMed] [Google Scholar]
- 114.Batista AC, Silva TA, Chun JH, Lara VS. Nitric oxide synthesis and severity of human periodontal disease. Oral Dis. 2002;8(5):254–60. doi: 10.1034/j.1601-0825.2002.02852.x. [DOI] [PubMed] [Google Scholar]
- 115.Seemann R, Hägewald SJ, Sztankay V, Drews J, Bizhang M, Kage A. Levels of parotid and submandibular/sublingual salivary immunoglobulin A in response to experimental gingivitis in humans. Clin Oral Investig. 2004;8(4):233–7. doi: 10.1007/s00784-004-0280-5. [DOI] [PubMed] [Google Scholar]
- 116.Kumasaka S, Shimozuma M, Kawamoto T, Mishima K, Tokuyama R, Kamiya Y, et al. Possible involvement of melatonin in tooth development: Expression of melatonin 1a receptor in human and mouse tooth germs. Histochem Cell Biol. 2010;133(5):577–84. doi: 10.1007/s00418-010-0698-6. [DOI] [PubMed] [Google Scholar]
- 117.Cutando A, Gómez-Moreno G, Arana C, Acuña-Castroviejo D, Reiter RJ. Melatonin: Potential functions in the oral cavity. J Periodontol. 2007;78(6):1094–102. doi: 10.1902/jop.2007.060396. [DOI] [PubMed] [Google Scholar]
- 118.Cutando A, Gómez-Moreno G, Villalba J, Ferrera MJ, Escames G, Acuña-Castroviejo D. Relationship between salivary melatonin levels and periodontal status in diabetic patients. J Pineal Res. 2003;35(4):239–44. doi: 10.1034/j.1600-079x.2003.00075.x. [DOI] [PubMed] [Google Scholar]
- 119.Bertl K, Schoiber A, Haririan H, Laky M, Steiner I, Rausch WD, et al. Non-surgical periodontal therapy influences salivary melatonin levels. Clin Oral Investig. 2013;17(4):1219–25. doi: 10.1007/s00784-012-0801-6. [DOI] [PubMed] [Google Scholar]
- 120.Genco RJ, Ho AW, Kopman J, Grossi SG, Dunford RG, Tedesco LA. Models to evaluate the role of stress in periodontal disease. Ann Periodontol. 1998;3(1):288–302. doi: 10.1902/annals.1998.3.1.288. [DOI] [PubMed] [Google Scholar]
- 121.Mengel R, Bacher M, Flores-De-Jacoby L. Interactions between stress, interleukin-1beta, interleukin-6 and cortisol in periodontally diseased patients. J Clin Periodontol. 2002;29(11):1012–22. doi: 10.1034/j.1600-051x.2002.291106.x. [DOI] [PubMed] [Google Scholar]
- 122.Sewón L, Mäkelä M. A study of the possible correlation of high salivary calcium levels with periodontal and dental conditions in young adults. Arch Oral Biol. 1990;(35 Suppl):211S–2. doi: 10.1016/0003-9969(90)90160-c. [DOI] [PubMed] [Google Scholar]
- 123.Sewón L, Söderling E, Karjalainen S. Comparative study on mineralization-related intraoral parameters in periodontitis-affected and periodontitis-free adults. Scand J Dent Res. 1990;98(4):305–12. doi: 10.1111/j.1600-0722.1990.tb00977.x. [DOI] [PubMed] [Google Scholar]
- 124.Socransky SS. Relationship of bacteria to the etiology of periodontal disease. J Dent Res. 1970;49(2):203–22. doi: 10.1177/00220345700490020401. [DOI] [PubMed] [Google Scholar]
- 125.Haffajee AD, Socransky SS, Smith C, Dibart S. Relation of baseline microbial parameters to future periodontal attachment loss. J Clin Periodontol. 1991;18(10):744–50. doi: 10.1111/j.1600-051x.1991.tb00066.x. [DOI] [PubMed] [Google Scholar]
- 126.Tran SD, Rudney JD, Sparks BS, Hodges JS. Persistent presence of Bacteroides forsythus as a risk factor for attachment loss in a population with low prevalence and severity of adult periodontitis. J Periodontol. 2001;72(1):1–10. doi: 10.1902/jop.2001.72.1.1. [DOI] [PubMed] [Google Scholar]
- 127.Saygun I, Nizam N, Keskiner I, Bal V, Kubar A, Açikel C, et al. Salivary infectious agents and periodontal disease status. J Periodontal Res. 2011;46(2):235–9. doi: 10.1111/j.1600-0765.2010.01335.x. [DOI] [PubMed] [Google Scholar]
- 128.von Troil-Lindén B, Torkko H, Alaluusua S, Jousimies-Somer H, Asikainen S. Salivary levels of suspected periodontal pathogens in relation to periodontal status and treatment. J Dent Res. 1995;74(11):1789–95. doi: 10.1177/00220345950740111201. [DOI] [PubMed] [Google Scholar]
- 129.Holt RD, Wilson M, Musa S. Mycoplasmas in plaque and saliva of children and their relationship to gingivitis. J Periodontol. 1995;66(2):97–101. doi: 10.1902/jop.1995.66.2.97. [DOI] [PubMed] [Google Scholar]
- 130.Yan C, Boyd DD. Regulation of matrix metalloproteinase gene expression. J Cell Physiol. 2007;211(1):19–26. doi: 10.1002/jcp.20948. [DOI] [PubMed] [Google Scholar]
- 131.Segal A, Wong DT. Salivary diagnostics: Enhancing disease detection and making medicine better. Eur J Dent Educ. 2008;12(Suppl 1):22–9. doi: 10.1111/j.1600-0579.2007.00477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Buduneli N, Kinane DF. Host-derived diagnostic markers related to soft tissue destruction and bone degradation in periodontitis. J Clin Periodontol. 2011;38(Suppl 11):85–105. doi: 10.1111/j.1600-051X.2010.01670.x. [DOI] [PubMed] [Google Scholar]


