Abstract
Background
Replacement of β-cells with the use of isolated islet allotransplantation (IT) is an emerging therapy for type 1 diabetics with hypoglycemia unawareness. The current standard protocol calls for a 36–72-hour culture period beforeIT. We examined 13 clinical islet preparations with ≥2 purity fractions to determine the effect of culture on viability.
Methods
After standard islet isolation and purification, pure islet fractions were placed at 37°C with 5% CO2 for 12-24 hours and subsequently moved to 22°C,whereas less pure fractions were cultured at 22°C for the entire duration. Culture density was targeted at a range of 100-200 islet equivalents (IEQ)/cm2 adjusted for purity. Islets were assessed for purity (dithizone staining), quantity (pellet volume and DNA), and viability (oxygen consumption rate normalized to DNA content[OCR/DNA] and membrane integrity).
Results
Results indicated that purity was overestimated, especially in less pure fractions. This was evidenced by significantly larger observed pellet sizes than expected and tissue amount as quantified with the use of a dsDNA assay when available. Less pure fractions showed significantly lower OCR/DNA and membrane integrity compared with pure. The difference in viability between the 2 purity fractions may be due to a variety of reasons, including hypoxia, nutrient deficiency, toxic metabolite accumulation, and/or proteolytic enzymes released by acinar tissue impurities that are not neutralized by human serum albumin.
Conclusions
Current clinical islet culture protocols should be examined further, especially for less pure fractions, to ensure the maintenance of viability beforetransplantation. Even though relatively small, the difference in viability is important because the amount of dead or dying tissue introduced into recipients may be dramatically increased, especially with less pure preparations.
Introduction
Despite the recent progress made in the field of human clinical allograft islet transplantation (IT) for the treatment of type 1 diabetes, the majority of recipients do not become fully insulin independent after a single transplantation [1). Factors associated with lower purity, such as competition for oxygen and other nutrients between islet and nonislet tissue during in vitroculture and after transplantation, may have a major impact on the success of IT. The standard method to estimate the purity fraction of islets is by staining with dithizone (DTZ) and examining by light microscopy, which is operator dependent and can lead to overestimation of purity[2,3]. Not accounting for this overestimation (ie, appropriately adjusting the culture surface density) can be detrimental to the viability and function of the islets, which in turn may reducethe chance of insulin independence in the recipient [2-7]. There is a need for standardization and optimization of purity measurements and culture methods to minimize or eliminate this chance. The present study was designed to retrospectively examine IT preparations by various methods of cell quantification and to evaluate the effect of purity on islet viability after culture with the use of oxygen consumption rate normalized to DNA content (OCR/DNA) and membrane integrity stains.
Methods
We retrospectively examined all human clinical islet allograft preparationswith at least 2 purity fractions (n = 13) after 36-72 hours of the standard culture method of IT[8].After routinehuman islet isolation and purification, pure islet fractions (≥70% purity estimated by DTZ staining) were placed in an incubator at 37°C with 5% CO2 for 12-24 hours and subsequently moved to 22°C. Less pure (30%-69%purity) fractions were cultured at 22°C with 5% CO2 for the entire duration. Culture density per T-175 flask was targeted at a range of 100-200 islet equivalents (IEQ)/cm2 adjusted for purity (ie, 50-100 IE/cm2 fora 50% pure preparation). CMRL-1066 media volume was 30mL per T-175 flask, with 20mL being replaced after 12-24 hours of culture[9]. After the culture period, islets were assessed for purity, quantity, and viability.
Purity was estimated by removing 2 samples of 100-200 μL each from the well mixed and presumed homogeneoustissue suspension and adding DTZ. Samples were examined under a light microscope, and the percent of red-stained cells was estimated as the purity [2,3,7].
Islet quantity was measured by 3 methods and estimated by 1 method(1) A standard IEQcountwas based on the DTZ samples, in which islets ≥50 μm in diameter were stratified into groups of 50-μm increments and normalized to a150-μm diameter size. (2) A dsDNA fluorescent dye kit (Quant-it PicogreendsDNA kit; Molecular Probes, Eugene, Oregon) was used to measure the quantity of DNA in each purity fraction; the total quantity of DNA measured was converted to IEQ by assuming 1 IEQ = 10.4 ng DNA [2] and corrected for purity as measured by DTZ to be compared with the IEQ counts. (3) For measuring the observed pellet volume, ithe tissue was aspirated into a 10-mL glass pipette and allowed to settle for 3-5 minutes, and the cell volume (mL) was then visually observed. (4) The IEQ measured by method (1) was then used to estimate the expected pellet volume to be compared with the observed pellet volume; the expected pellet volume (mL) based on the IEQ counts was determined by using the volume of an IEQ which, being by definition a sphere with a diameter of 150 μm, is 1.77 × 106 μm3; for example, accounting for a ~10%void fraction, or the extracellular space between islets, a pellet size of 2 mL would be expected to contain ~1 × 106IEQ of 100% pure islets, and 4 mL would be expected to contain ~1 × 106IEQ of 50% pure islets.
Islet viability was assessed by 2 methods. The first method was by membrane integrity staining with the use of anIT release assay (viability must be ≥70%). Briefly, an aliquot of islets (80-100 IEQ) were spun down and resuspended in 460 μL Dulbecco phosphate-buffered saline solution (DPBS), 10 μL 0.46 μmol/L fluorescinediacetate(Sigma no F7378;inclusion dye in which viable cells appear as bright green fluorescent), and 10 μL 14.34μmol/L propidium iodide (Sigma no P4170;exclusion dye which enters ruptured cell membranes with a red/orange fluorescence). The cells were then washed with DPBS and viewed under a fluorescent microscope. Percentage viability was estimated as the area of green cells (live) to total tissue [2,3]. The second method of assessing islet viability was by measuring the OCR/DNA as detailed elsewhere [2,7,10] with the use of a real-time in vitroassay that has been validated as a quality assay in various animal models and the human autograft model[11-13].
Statistical Techniques
All statistical analyses were performed with the use of the SAS statistical software package, version 9.3 (SAS Institute, Cary, North Carolina) or GraphpadPrism, version 5.03 (GraphpadSoftware, La Jolla, California). Values are reported as mean ± SD. Statistical significance was tested by a paired Student t test and corresponded to P<.05.
Results
The islet puritywas typically grossly overestimated in all fractions based on the comparison between observed and expected pellet volumes, especially in the less pure fractions. This was demonstrated by the significantly larger observed pellet volumesrelative to the volumes expected from the counts (P = .01 for pure; P = .0001 for less pure; Fig 1a and b). The overestimation of purity was also evidenced by the significant difference between the actual IEQ counts and the IEQ estimated from the dsDNA assay when available (P = .003 for pure; P = .0001 for less pure; Fig 1c and d). Less pure fractions showed a significantly lower viability than pure fractions after culture as measured by both OCR/DNA and membrane integrity stains (Fig 1e and f). Mean ± SD OCR/DNA was 125 ± 28nmol O2/min•mgDNA for pure fractionsand 99 ± 19 for less pure fractions (P = .009). Based on membrane integrity, percentage viability was 92 ± 5% for pure fractionsand 86 ± 4%for less pure fractions (P = .003).
Fig 1.
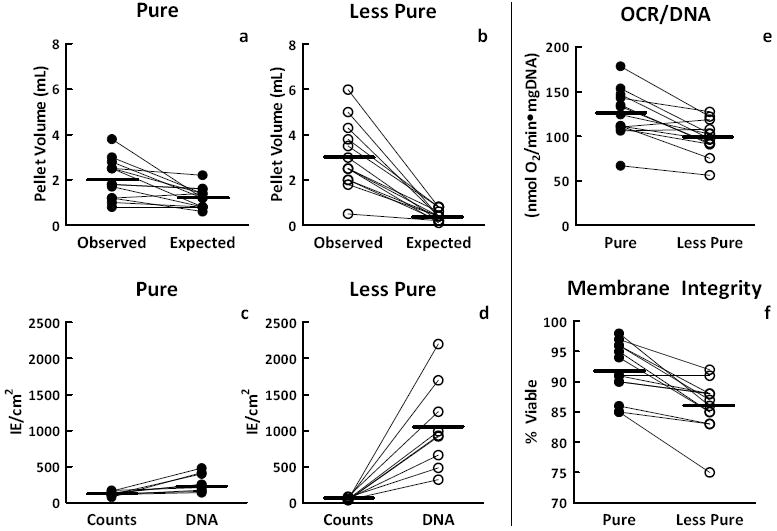
Observed values plotted against theoretical expected valuesfor (a, b) pellet volume, (c,d) islet density (islet equivalents [IE]/cm2) in culture flasks as measured by counts and DNA, and (e,f) islet preparation viability for separate purity fractions as measured by oxygen consumption rate normalized to DNA content (OCR/DNA) and membrane integrity staining for 13 clinical islet preparations.
Discussion
Among the major factors favoring successful IT, the islet yield, the purity of preparations, and the viability of the islets post-culture are critical for transplant outcome. Purity has been traditionally measured by visual estimation of preparations stained with DTZ, and this test gave 20%-30% erroneously higher values on average compared with more rigorous assessments of islet preparation fractions, such as electron microscopy or laser scanning cytometry[4,5,7]. Street et al reported that when comparing islet purity assessed by DTZ staining with results with the use of immunostaining to quantify total endocrine cellular composition, the DTZ-based purity assessment gave significantly higher results than those indicated by the endocrine immunostaining [6]. Furthermore, it is known that individual estimates from DTZ staining are subject to considerable observer variability [6,14,15].
The results from this study indicate that the purity by DTZ staining is typically grossly overestimated in all fractions and especially in less pure ones. This was evidenced by observing significantly larger settled tissue volumes and estimated IEQ from DNA quantities than what was expected based on the counts. This overestimation could be the cause of lower viability in the less pure preparations after culture. The cells may have been exposed to hypoxia and/or nutrient deficiency, because the culture density would be much higher than desired [16]. Another possible cause of the difference in viability may be toxic metabolite accumulation and/or proteolytic enzymes released by the acinar tissue impurities that are not neutralized by human serum albumin [17].In addition, there may be a preferential loss of viability in nonislet tissue, which would explain the lower viability in less pure fractions.
In conclusion, current clinical islet purity measurements and culture protocols should be examined and further refined to ensure the maintenance of viability after culture and beforetransplantation. Even though relatively small, the difference in viability observed with purity is important because the amount of total and thus dead tissue introduced in recipients may be dramatically increased, especially with less pure preparations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Collaborative Islet Transplant Registry. [May 3, 2013];CITR Sixth Annual Report. 2009 Available at: https://web.emmes.com/study/isl/reports/CITR%206th%20Annual%20Data%20Report%20120109.pdf.
- 2.Colton CK, Papas KK, Pisania A, et al. Characterization of islet preparations. In: Halberstadt C, Emerich DF, et al., editors. Cell transplantation from laboratory to clinic. New York: Elsevier; 2007. pp. 35–132. [Google Scholar]
- 3.Boyd V, Cholewa OM, Papas KK. Limitations in the use of fluorescein diacetate/propidium iodide (FDA/PI) and cell permeable nucleic acid stains for viability measurements of isolated islets of langerhans. Curr Trends Biotechnol Pharm. 2008;2:66–84. [PMC free article] [PubMed] [Google Scholar]
- 4.Pisania A, Weir GC, O’Neil JJ, et al. Quantitative analysis of cell composition and purity of human pancreatic islet preparations. Lab Invest. 2010;90:1661–75. doi: 10.1038/labinvest.2010.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ichii H, Inverardi L, Pileggi A, et al. A novel method for the assessment of cellular composition and beta-cell viability in human islet preparations. J Transplant. 2005;5:1635–45. doi: 10.1111/j.1600-6143.2005.00913.x. [DOI] [PubMed] [Google Scholar]
- 6.Street CN, Lakey JRT, Shapiro AMJ, et al. Islet graft assessment in the Edmonton protocol. Implications for predicting long-term clinical outcome. Diabetes. 2004;53:3107–14. doi: 10.2337/diabetes.53.12.3107. [DOI] [PubMed] [Google Scholar]
- 7.Papas KK, Suszynski TM, Colton CK. Islet assessment for transplantation. CurrOpin Organ Transplant. 2009;14:674–82. doi: 10.1097/MOT.0b013e328332a489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shapiro AMJ, Ricordi C, Hering BJ, Auchincloss H, Lindblad R, et al. International trial of the Edmonton protocol for islet transplantation. N Engl J Med. 2006;355:1318–30. doi: 10.1056/NEJMoa061267. [DOI] [PubMed] [Google Scholar]
- 9.Clinical Islet Transplantation Study. [May 3, 2013];Purified human pancreatic islets master production batch record. Available at: http://www.isletstudy.org/CITDocs/SOP%203101,%20B01,%20MPBR%20v05,%20October%2028,%202010.pdf.
- 10.Papas KK, Pisania A, Wu H, Weir GC, Colton CK. A stirred microchamber for oxygen consumption rate measurements with pancreatic islets. BiotechnolBioeng. 2007;98:1071–82. doi: 10.1002/bit.21486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papas KK, Colton CK, Nelson RA, Rozak PR, Avgoustiniatos ES, Scott WE, 3rd, et al. Human islet oxygen consumption rate and DNA measurements predict diabetes reversal in nude mice. Am J Transplant. 2007;7:707–13. doi: 10.1111/j.1600-6143.2006.01655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papas KK, Colton CK, Qipo A, et al. Prediction of marginal mass required for successful islet transplantation. J Invest Surg. 2010;23:28–34. doi: 10.3109/08941930903410825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Papas KK, Bellin MD, Sutherland DE, et al. Clinical islet auto-transplant outcome is highly correlated with viable isle dose as measured by oxygen consumption rate. CellR4. 2013;1:108. [Google Scholar]
- 14.Ricordi C, Gray DW, Hering BJ, et al. Islet isolation assessment in man and large animals. ActaDiabetol. 1990;27:185–95. doi: 10.1007/BF02581331. [DOI] [PubMed] [Google Scholar]
- 15.Ricordi C. Quantitative and qualitative standards for islet isolation assessment in humans and large mammals. Pancreas. 1991;6:242–4. doi: 10.1097/00006676-199103000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Papas KK, Avgoustiniatos ES, Tempelman LA, et al. High-density culture of human islets on top of silicone rubber membranes. Transplant Proc. 2005;37:3412–4. doi: 10.1016/j.transproceed.2005.09.086. [DOI] [PubMed] [Google Scholar]
- 17.Avgoustiniatos ES, Scott WEIII, Suszynski TM, et al. Supplements in human islet culture: human serum albumin is inferior to fetal bovine serum. Cell Transplant. 2012;21:2805–14. doi: 10.3727/096368912X653138. [DOI] [PubMed] [Google Scholar]


