Abstract
Previous studies showed a beneficial effect of motor re-training in task-specific hand dystonia. Here we examined whether re-training needs to specifically focus on the task affected by dystonia. 21 patients with writer's cramp were randomly assigned to two types of re-training: One group of patients trained drawing and writing movements using a pen attached to the bottom of a finger splint. The second group used therapeutic putty to train finger movements without exercises of drawing and writing movements. Training lasted for eight weeks. Before re-training, affected hand and forearm were immobilized for four weeks to facilitate the responsiveness to re-training. Dystonia was assessed during handwriting using the Writer's Cramp Rating Scale. While no clinical improvement was observed immediately after immobilization, eight weeks of re-training improved task-specific dystonia relative to baseline (p=0.005). Both training modalities were equally effective. More severely affected patients benefited most. There was no correlation between disease duration and the individual treatment response. Re-training also improved hand function as indexed by the Arm Dystonia Disability Scale (p=0.008). Kinematic handwriting analysis showed that re-training lowered vertical force level and enhanced the fluency of handwriting. We conclude that re-training does not need to specifically focus on the task affected by dystonia to be clinically effective.
Keywords: Focal hand dystonia, writer's cramp, kinematic analysis, training, writing, immobilization
Introduction
Writer's cramp is a task-specific dystonia affecting handwriting.1 Standard treatment involves botulinum toxin (BTX) injections into affected muscles, but may cause disabling weakness, and only 50% of patients remain on long-term treatment. 2, 3 Task-specific hand dystonia is associated with abnormal patterns of activity at multiple levels within the sensorimotor system 1, 4-7 An abnormal homuncular organization of sensory finger representation in the primary somatosensory cortex indicates cortical disorganization.6, 8 Based on these findings, novel therapeutical approaches intend to normalize sensorimotor integration.9 Sensory 10, 11 and motor 12, 13 re-training has been shown to produce a sustained improvement of writer's cramp. Sensorimotor retuning also improved task-specific dystonia in musician's cramp.14
The present study addressed the question whether motor re-training needs to specifically target the movements that are affected by dystonia to induce clinical improvement. Patients with writer's cramp were randomly assigned to two types of motor training. The first group trained writing movements using a pen attached to the bottom of a finger splint (task specific training). The second group trained finger movements using therapeutic putty, but without writing exercises (non-task specific training). We expected task specific training to be more effective in improving dystonia than non-task specific training with putty.
A four-week period of immobilization of the affected limb was found to be beneficial in patients with musician's cramp9, 15. Therefore, to further enhance the effect of re-training, we immobilized the affected forearm and hand for four weeks before patients started with their training program. We reasoned that a prolonged period of inactivity would attenuate malfunctional representations of handwriting movements, and thus, help to re-establish normal movement representations with training.
Methods
26 (12 females) patients with writer's cramp volunteered for the study (Table 1). Mean age was 49.8 ± 12.2 years (range: 27-71 years). Seven patients had simple and 19 patients dystonic writer's cramp.16 Mean disease duration was 11.5 ± 7.4 years (range: 2-25 years). BTX injections were stopped three months before enrollment in the study and patients were included when the BTX effect had disappeared. 21 age-matched healthy individuals served as controls (9 females). Mean age was 49.14 ± 13.35 years (range: 27-68 years). Controls performed the standardized writing and drawing task without receiving immobilization or training. All participants gave written informed consent before the study. The study had the approval of the local ethics committee.
Table 1.
Clinical data of patients with writer's cramp
| Patient ID | Age (ys) | Symptom Duration (ys) | Type of Writer's Cramp | Total ADDS score (%) | Total WCRS score |
|---|---|---|---|---|---|
| 205 | 52 | 3 | Simple | 64.57 | 13 |
| 109 | 27 | 5 | Simple | 72.86 | 15 |
| 212 | 71 | 5 | Simple | 77.14 | 16 |
| 117 | 76 | 12 | Simple | 77.14 | 5 |
| 221 | 52 | 11 | Simple | 72.86 | 13 |
| 123 | 34 | 8 | Simple | 55.71 | 11 |
| 224 | 45 | 2 | Simple | 68.57 | 2 |
| 101 | 52 | 18 | Dystonic | 68.57 | 14 |
| 202 | 63 | 25 | Dystonic | 34.29 | 20 |
| 203 | 62 | 3 | Dystonic | 70,00 | 3 |
| 104 | 49 | 15 | Dystonic | 17.14 | 18 |
| 106 | 64 | 7 | Dystonic | 64.29 | 10 |
| 207 | 35 | 3 | Dystonic | 51.42 | 10 |
| 208 | 52 | 8 | Dystonic | 68,57 | 20 |
| 110 | 29 | 15 | Dystonie | 60.00 | 9 |
| 211 | 52 | 5 | Dystonic | 60.00 | 6 |
| 213 | 59 | 15 | Dystonic | 8.57 | 17 |
| 114 | 47 | 3 | Dystonic | 42.86 | 10 |
| 115 | 60 | 18 | Dystonic | 51.42 | 13 |
| 116 | 46 | 15 | Dystonic | 60.00 | 15 |
| 218 | 38 | 7 | Dystonic | 47.14 | 6 |
| 119 | 54 | 25 | Dystonic | 24.43 | 3 |
| 220 | 52 | 20 | Dystonic | 64.29 | 17 |
| 122 | 47 | 25 | Dystonic | 64.29 | 1 |
| 225 | 39 | 17 | Dystonic | 30.00 | 17 |
| 126 | 39 | 10 | Dystonic | 55.71 | 20 |
| Mean | 48.81 | 11.76 | 55.07 | 11.81 | |
| SD | 11.06 | 7.50 | 18.58 | 5.91 |
ADDS = Arm Dystonia Disability Scale, WCRS = Writer's Cramp Rating Scale The first number of the patient's ID refers to the group they were randomized to. Patients with an ID that starts with 1 were randomized into the first group with task specific training, whereas the ID starting with a 2 refers to the second group with non task specific training using therapeutic putty. Patients marked in italics did not complete the study and were not included in the statistical analysis.
Immobilization of the affected limb
The wrist and finger joints were continuously immobilized using a plastic splint as described by Priori et al.15 (CAMP Handgelenksorthese-Halbzirkel, No. 8709, Basko Healthcare, Hamburg, Germany). Patients were allowed to take the splint off for 30 minutes per day for cleaning and stretching exercises. To control the compliance, a temperature log was fixed inside the splint (Kooltrak GmbH, Geisenheim, Germany) and measured local temperature every 30 min over the entire period of immobilization.
Task-specific re-training with finger splints
All patients participated in a daily training program lasting eight weeks. In the first two weeks, re-training included exercises with therapeutic putty (TheraputtyR, Sammons Preston Rolyan, Cedarburg, Wisconsin, USA) only to build up strength in the hand and forearm after immobilization, and task specific training exclusively with splints. Training with therapeutic putty was performed daily for 20 minutes in the first, and 10 minutes in the second week and did not involve finger training.
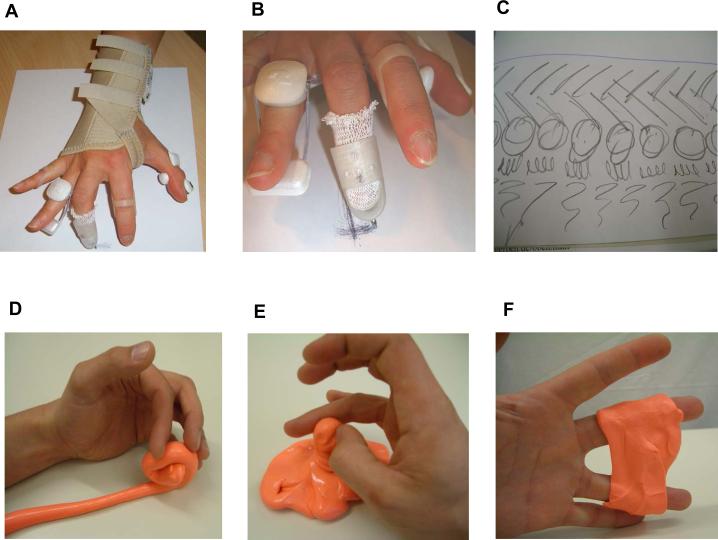
Task-specific training consisted of drawing and writing exercises (Fig.1B,C). Finger movements were trained with stax finger splints (Dj. Orthopedics, LLC; Vista, CA, USA) with a pen attached on the bottom of these splints as described previously (Fig.1A).12 The co-contracting fingers were splinted with finger splints using RolyanR finger splints (Sammons Preston Rolyan, Cedarburg, Wisconsin, USA) to enable finger movements without dystonic co-contractions. (Fig.1A). To ensure that practice time did not exceed 35 minutes in the first two weeks, finger training was limited to three minutes per finger in the first and five minutes in the second week. In the third week, exercise time for each finger was increased to10 minutes. In the fourth week, finger exercises were reduced to five minutes because patients performed additional drawing and writing exercises and trained those for 10 minutes in the third and 20 minutes in the fourth week. Writing and drawing exercises were performed with a modified pen that had a large diameter. This rendered the pen easy to grasp and minimized co-contractions. Together, patients practiced daily 35 minutes in the first and second week, 60 minutes in the third, and 50 minutes for the remaining five weeks. Patients recorded all exercises using a diary.
Figure 1.
Panels A-C illustrate task specific re-training. Panel A shows how the hand was restrained with splints during task specific training.. Panel B illustrates drawing exercises performed with the middle finger using a pen that was attached to a plastic splint at the tip of the finger. Some writing exercises are shown in panel C. Panel D-F show exercises with therapeutic putty during non-task specific training. Patients trained flexion (D), rotational (E), and abduction-adduction finger movements (F).
Non-task specific re-training with therapeutic putty
Patients practiced finger movements with therapeutic putty. They formed a snail like figure to perform flexion movements (Fig.1D). Rotational finger movements were trained by turning a bump in clockwise and counterclockwise direction (Fig. 1E ). Patients exercised abduction, adduction and extension movements of each finger against the resistance of the putty (Fig.1F). Daily training sessions lasted for 30 minutes in the first and 45 minutes in the remaining seven weeks.
The therapeutic effect of immobilization and re-training was prospectively assessed using standardized clinical rating scales and analysis of movement kinematics during handwriting and drawing. Patients were examined at baseline (week 0), after immobilization (week 4), and twice during training (week 8 and 12).
Clinical assessment of writer's cramp
Dystonia was assessed while participants continuously wrote the sentence “Die Wellen schlagen hoch” (“The waves are surging high”) ten times and videotaped. A blinded rater assessed the severity of dystonia using the writer's cramp rating scale (WCRS).17 The WCRS served as primary outcome measure because this scale quantifies hand dystonia during writing .17 The higher the total WCRS score the more severe are dystonic symptoms during handwriting.17
The Arm Dystonia Disability Scale (ADDS) provided a secondary outcome measure to assess how dystonia interfered with manual activities during daily life.18 The ADDS contains seven items which estimates the impairment of manual skills. A score of 100% indicates normal motor function. The final score presents the percentage of normal manual activity. The lower the ADDS score the stronger is the functional impairment.18
Kinematic handwriting analysis
To examine how re-training impacts on motor control during handwriting, we performed a stroke-based kinematic analysis of the written trace obtained during the standardized handwriting described above.19-21 Since dystonic symptoms tend to increase with prolonged handwriting, the word “Wellen” of the first and last three of the ten sentences were analyzed separately. The word “Wellen” consisted of a letter sequence that facilitates a smooth and fluent writing style.22-24 The writing movements can easily be segmented in subsequent vertical up- or down-strokes of the pencil which represent the modules of skilled writing.
Participants also performed a drawing task in which they were required to quickly draw superimposed circles for three seconds.
Kinematic recordings and analysis
Drawing and writing movements were recorded using an inking digitizing pen and a pressure-sensitive digitizing tablet (WACOM Intuos A4 oversize, Wacom Europe GmbH, Neuss, Germany). The position of the pen-tip was stored on a personal computer with a sample frequency of 166 Hz and analysed using CS-Software (MedCom, Germany). The spatial resolution was 0.05 mm; the accuracy was 0.025 mm in the horizontal and vertical direction. The recorded data were smoothed by non-parametric regression methods. 25
Mean vertical force level during writing and the number of inversion (NIV) per up- and down-stroke were used to assess changes in performance during continuous writing. The number of inversion (NIV) per stroke equals the number of velocity peaks during a single stroke and reflects the degree of automaticity 13, 20, 23, 26. The axial force measured was multiplied by the sine of the writing angle (defined as angle between the tablet and the axis of the pencil) in order to calculate the vertical force exerted with the pen on the tablet.20, 24, 26 Mean stroke frequency and mean coefficient of variation (CV) of vertical peak velocity were defined as kinematic measures of interest for the analysis of circle drawing.24
Statistical Analysis
Separate two-factorial repeated measures ANOVAs were computed for each clinical score and kinematic measure of interest to assess the effect of immobilization and training. The time of measurement (4 levels: measurement at baseline [week 0], after immobilization [week 4] during and after training [week 8 and 12]) and type of training (2 levels: task specific vs. non-task specific training) were treated as within-subjects factor. If necessary, the Greenhouse-Geisser method was used to correct for nonsphericity. Depending on a significant main effect of time, post-hoc two-tailed t-tests were performed to assess time-dependent changes relative to baseline. Since the mean NIV was not normally distributed, non-parametric test statistics (Friedman test and Whitney Mann test) were used to analyze changes in NIV during the course of the study. In the patient group, we performed a linear regression analysis to test whether the relative change in the WCRS score correlated with the total WCRS score at baseline. Two-tailed unpaired t-tests were performed to explore differences between groups. A p-value of 0.05 or less was considered significant.
Results
21 of the 26 patients completed the study. Patients 110 and 117 dropped out of the study because they could not cope with the long period of immobilization. Patients 205 and 220 discontinued participating in the study due to job-related reasons. Patient 203 developed an acute carpal tunnel syndrome after immobilization that required surgical therapy. Consequently, patients with a neurophysiologically confirmed carpal tunnel syndrome were excluded. 10 patients carried out task specific finger training, while 11 patients trained with therapeutic putty. Table 1 gives the baseline WCRS and ADDS scores of all patients. There was no correlation among individual ADDS scores, WCRS scores, and age of patients.
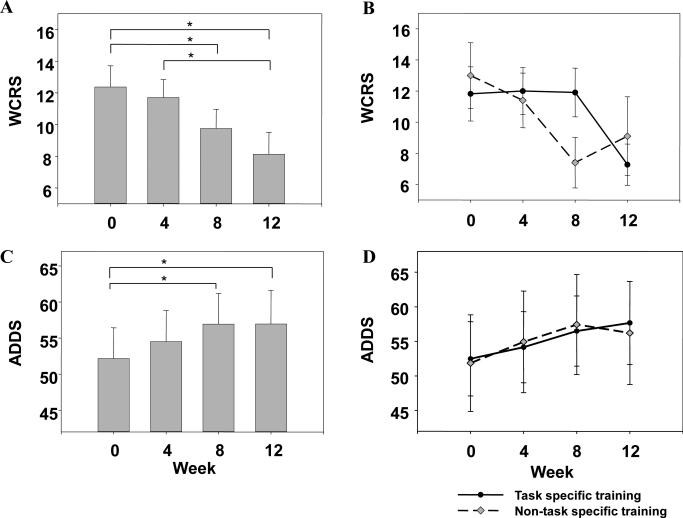
Eight weeks of re-training improved writer's cramp as indexed by a decrease in the mean WCRS ( time of measurement: F [2.4; 48.1] = 3.80; p = 0.023; Fig.2a). Both types of retraining were equally effective although patients who performed training with putty tended to improve more quickly (Fig.2b, 6). Because ANOVA showed no main effect of type of training and no interaction between type of training and time of measurement (p > 0.2), the results of both groups were pooled together for further analysis (Fig.2a). Post-hoc t-tests showed no overall change in WCRS immediately after immobilization (p > 0.6), while there was a consistent reduction in mean WCRS score after eight weeks (week 8 vs. week 0: T(20) = 2.67; p = 0.015) and twelve weeks (week 12 vs. week 0: T(20) = 3.17; p = 0.005; week 12 vs. week 4: T(20) = 2.67; p = 0.015).
Figure 2.
The top left panel (a) gives the mean WCRS score at baseline (week 0), after immobilization (week 4), and motor re-training (week 8 and 12) of the 21 patients with writer's cramp who completed the study. The upper right panel (b) shows the results for each group separately. The black circles represent the first group with task specific training, the grey diamond group 2 who trained with therapeutic putty. The lower left panel (c) shows the mean ADDS score in % at baseline (week 0), after immobilization (week 4) and motor training (week 8 and 12). Data of patients performed task specific finger training with splints and non-task specific training with therapeutic putty are pooled together. The right lower panel (d) gives the results of each groups (black circle = task specific training; grey diamond = non-task specific training). Error bars equal onefold standard error of the mean. The asterisk indicates significant differences at p < 0.05.
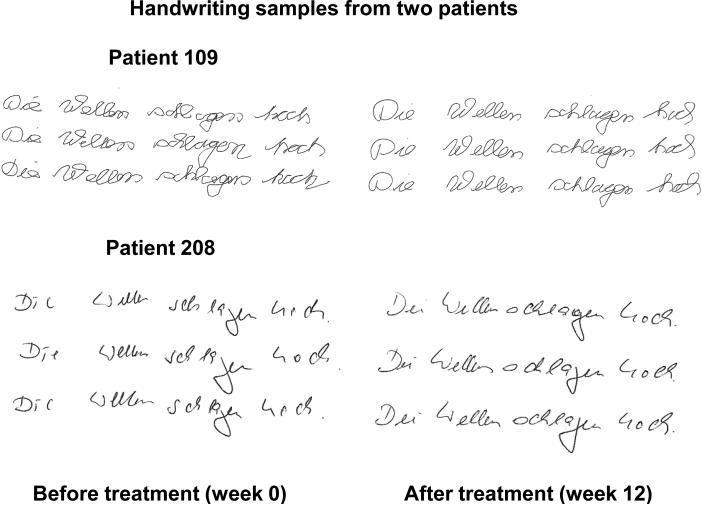
Figure 6.
Handwriting samples of two patients with writer's cramp at baseline (left panel) and after four weeks of immobilization followed by eight weeks of motor re-training (right panel). Patient 109 (upper panel) performed a specific finger training with splints. Patient 208 (lower panel) received a general occupational finger and hand training with therapeutical putty. In both patients, the written trace became more regular and the curvatures of the letters were smoother after treatment.
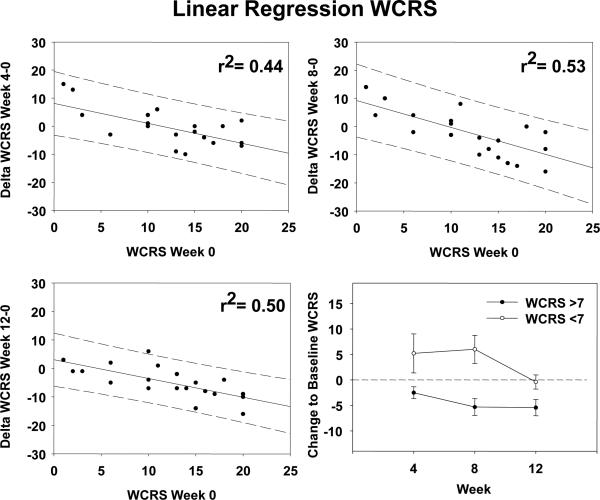
The severity of dystonic symptoms at baseline correlated with the clinical improvement. The higher the WCRS score at baseline the stronger was the relative reduction in the WCRS after week 4 (r2 = 0.44; p < 0.001), week 8 (r2 = 0.53; p < 0.001) and week 12 (r2 = 0.50; p < 0.001). To explore the relationship between disease severity and treatment response, we stratified patients into two groups depending on the initial WCRS score: five patients had mild dystonia with WCRS scores < 7 at baseline, whereas 16 more severly affected patients showed WCRS scores > 7 (Fig. 3). In mildly affected patients, dystonia transiently worsened immediately after immobilization and returned to baseline levels during subsequent training. Disease duration and age were not correlated with the decrease in the WCRS score.
Figure 3.
Regression analysis. The graphs plot the total WCRS score of each patient at baseline (x-axis) against the relative change in WCRS (y-axis) at week 4 (left upper panel), week 8 (right upper panel) and week 12 (left lower panel). The continuous line presents the optimal fit of the data to a simple linear model. The area between the hatched lines represents the 95% confidence interval of the regression line. The higher the WCRS score at baseline the more pronounced the relative decrease in WCRS score. The r2 value refers to the simple regression analysis. The right lower panel gives the relative change in WCRS score depending on the severity of dystonia at baseline. Open circles represent the relative changes in WCRS scores of the five mildly affected patients (WCRS score of < 7), while closed circles give the relative changes in WCRS scores of 16 more severely affected patients(WCRS score > 7). Error bars equal onefold standard error of the mean.
Paralleling the beneficial effects on task-specific dystonia, the mean ADDS score increased during the course of the study reflecting an improvement in overall arm function (Fig.2 b,d). Both types of training produced a comparable increase in mean ADDS score (Fig.2d). Accordingly, repeated-measures ANOVA disclosed a main effect of time of measurement (F [2.4; 47.0] = 4.86; p = 0.009), but no main effect of type of training, and no interaction between the two factors (p > 0.2). Post-hoc t-tests showed an increase in mean ADDS score at week 8 (T(20) = -2.67; p = 0.015) and week 12 (T(20) = -2.92; p = 0.008) relative to baseline.
At baseline, drawing and writing movements were less fluent and regular in patients with writerś cramp than in healthy controls. During circle drawing, mean stroke frequency (T[40] = -6.87; p < 0.001) was decreased. The mean CV of peak vertical velocity (T[40] = 3.44; p = 0.0014) and mean NIV per stroke (Z = -4.66; p < 0.001) were increased in dystonic patients relative to healthy controls. During continuous writing, mean stroke frequency of the word “Wellen”was slower during the first (T[40] = -3.94; p = 0.0003) and last three sentences (T[40] = -3.78; p = 0.001). Patients also exerted a higher vertical writing force level than controls during the first (T[40]=-2.84; p=0.0071) and last three sentences (T[40]=3.1; p=0.0031). In addition, the mean NIV was increased relative to controls during the first (Z = -2.65; p = 0.008) and last three sentences (Z = -2.89; p = 0.004).
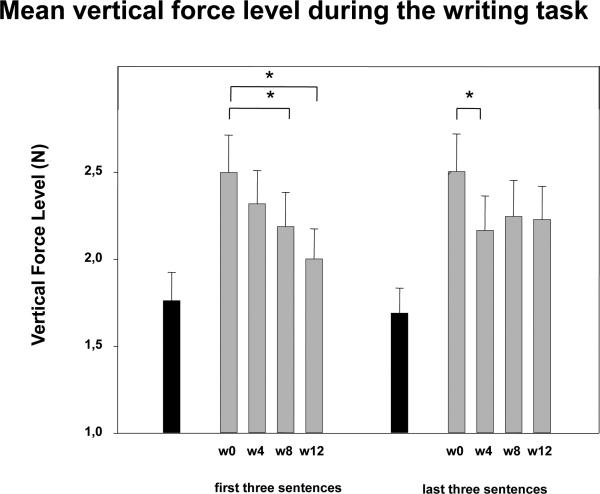
After re-training, patients exerted less vertical force on the digitizing tablet during writing compared to pre-interventional baseline (Fig.4). ANOVA showed a main effect of time of measurement for the mean vertical force level during the first (F [2.239; 89.55] = 4.96; p = 0.007) and last three sentences (F [1.94; 79.59] = 3.38; p = 0.04). For the last three sentences, the decrease in vertical force level after the end of immobilization (week 0 versus week 4: T[20]= 2.69; p=0.014) remained stable during training. For the first three sentences, re-training led to a further reduction in mean vertical writing force (week 0 versus week 12: T(20) = 3.30; p = 0.0036; week 4 versus week 12: T(20) = 2.41; p = 0.026; week 8 versus week 12: T(20) = 2.35; p = 0.029).
Figure 4.
Mean vertical force level during a standardized writing task. The task required the participants to write the sentence “Die Wellen schlagen hoch” (The waves are surging high). Participants had to continuously write ten sentences without a break. The columns reflect the mean vertical force level that was applied by the participants during the first three (left panel) and last three sentences (right panel) of the task. In 21 patients (grey columns), vertical force level was measured at baseline (week 0), after immobilization (week 4), after four and eight weeks of re-training (week 8 and 12). The black columns give the mean vertical force level of 21 healthy controls. The asterisk indicates a significant decrease in vertical force level relative to baseline in the patient group (p < 0.05). Error bars equal onefold standard error of the mean.
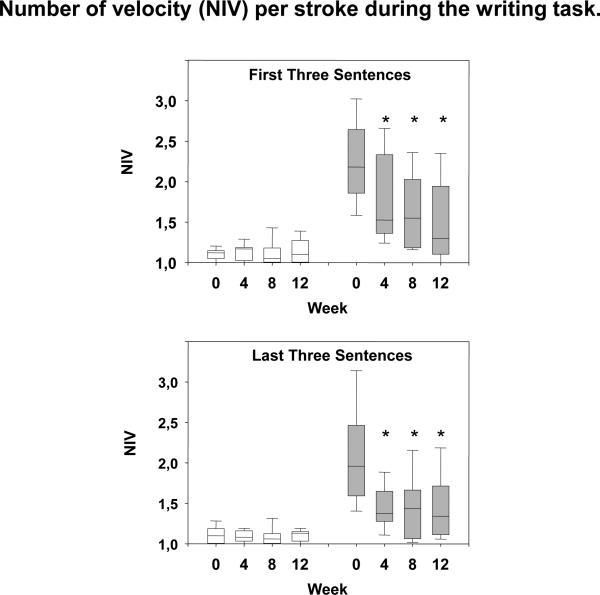
Measurements of mean NIV showed an overall improvement in automaticity of writing movements with motor re-training (Fig. 5). Accordingly, non-parametric Friedman repeated measures analysis of variance on ranks showed a change in mean NIV over time (Chi-Square: 9,754; p = 0.021) for the word “Wellen” in the last three sentences. Subgroup analyses showed that the overall decrease in NIV was caused by a beneficial effect of training in those patients with abnormally increased NIVs at baseline. When statistical analysis was restricted to the eight patients who had shown an abnormal increase in mean NIV at baseline, the change in NIV during the course of the study was significant, both for the first (Chi-Square: 20,55; p < 0.001) and last three sentences (Chi-Square: 12,27; p = 0.007) of the writing task. This was caused by a progressive decrease in mean NIV from week 0 to 12 (Fig. 4). Patients with increased NIVs at baseline showed a significant decrease in mean NIV after 4, 8, and 12 weeks relative to baseline (post-hoc Wilcoxon rank sum tests: Z ≥ 2.19; P ≤ 0.028). In contrast, the 13 patients with initially normal NIV showed no consistent changes in NIV during the course of the study (p > 0.5; Fig. 5).
Figure 5.
Box plot of the number of velocity (NIV) per stroke during a standardized writing task. Participants continuously wrote ten sentences (for details see Figure 3). The upper panel illustrates the NIV during the first three sentences while the lower panel displays the NIV during the last three sentences of the task. The white boxes give the data of 13 patients with a normal NIV value (NIV < 1.4) at baseline. The grey boxes gives the data of eight patients who showed an increase in NIV (NIV > 1.4) at baseline. In the latter group, immobilization and re-training consistently reduced the NIV per stroke, especially during the first three sentences of the task. The asterisk indicates a significant decrease in NIV relative to baseline (Wilcoxon rank sum test; p < 0.05). The bars give the 5% and 95% percentile of the group data.
Discussion
An eight week period of daily motor training improved task-specific dystonia, global hand function, and movement kinematics in patients with writer's cramp. Contrary to our prediction, non-task specific re-training with therapeutic putty was as effective as task specific re-training of finger movements with splints. This implies that re-training does not need to specifically focus on the task affected by dystonia to be clinically efficient. The task-specific and non-task specific re-training program required the training of finger movements, and this may be the critical feature that mediates therapeutic efficacy. Therapeutic putty is generally available and re-training can be applied by any occupational therapist. In contrast, task-specific re-training is demanding (e.g. adjustment of individual finger splints) and requires an occupational therapist. Because of its general availability and simplicity, re-training with therapeutic putty is an interesting option for the future treatment of task-specific hand dystonias.
Paralleling the clinical outcome, the two types of re-training had comparable effects on movement kinematics during handwriting and drawing. During the course of the study, training resulted in a relative reduction of vertical force level and improved automaticity as indexed by a decrease in NIV. The individual decrease in vertical force level correlated with clinical improvement, suggesting that this measure may provide a good kinematic marker for clinical improvement.19, 26 Immobilization and motor re-training had distinct effects on the vertical force exerted on the tablet during writing. During the last three sentences, a decrease in mean vertical force level was already present after immobilization. In contrast, mean vertical force during the first three sentences was not altered by immobilization but decreased during the course of motor re-training. While immobilization appears to attenuate the abnormal increase in vertical writing force during prolonged writing, motor re-training seems to counteract the gradual build-up of dystonia during the beginning of writing and thus, prevent an increase in vertical writing force during the first three sentences.
In this study, re-training was preceded by four weeks immobilization of the affected limb to minimize manual activity and dystonic symptoms for a prolonged period prior to retraining. The rationale for applying immobilization prior to re-training has been outlined in the introduction. As a result of immobilization, the baseline state of the sensorimotor system was matched across patients when they started with re-training. However, we wish to emphasize that this study was not designed to reexamine the therapeutical efficacy of immobilization15 as there was no study arm without immobilization. The study design was also not suited to explore whether and how a preceding period of immobilization primes the subsequent response to re-training. A major problem was the prolonged period of immobilization massively interfered with the patient's professional activities and caused many patients to refrain from participating in the first place. In a recent study, ten patients performed a similar task-specific re-training of independent finger movements without immobilization.12 In that study, re-training led to a mean increase in ADDS that was similar to the increase in patients who performed re-training after immobilization in the present study. Therefore, four weeks of immobilization may not substantially boost the efficacy of subsequent re-training. However, this issue has to be specifically addressed in a separate study.
Table 2.
Kinematics of writing and circle drawing of 21 patients.
| Kinematic Measures | week 0 | week 4 | week 8 | week 12 | p-value |
|---|---|---|---|---|---|
| Circle drawing task | |||||
| Frequency (Hz) | 3.01 ± 0.97 | 3.24 ± 0.80 | 3.08 ± 0.78 | 3.27 ± 0.80 | >0.1 |
| CV of vertical peak velocity | 0.18 ± 0.08 | 0.21 ± 0.11 | 0.15 ± 0.07 | 0.16 ± 0.06 | > 0.1 |
| Continuous handwriting task (first three sentences) | |||||
| Force level (N) | 2.50 ± 0.98 | 2.32 ± 0.88 | 2.19 ± 0.90 | 2.00 ± 0.79 | 0.004 |
| NIV | 1.54 ± 0.66 | 1.38 ± 0.50 | 1.33 ± 0.42 | 1.29 ± 0.39 | 0.024 |
| Continuous handwriting task (last three sentences) | |||||
| Force level (N) | 2,50 ± 0.99 | 2.17 ± 0.90 | 2.25 ± 0.95 | 2,23 ± 0.87 | 0.055 |
| NIV | 1.49 ± 0.63 | 1.22 ± 0.26 | 1.24 ± 0.34 | 1.24 ± 0.33 | 0.050 |
As the type of re-training had no specific effect on the kinematic changes, the data of the 10 patients who performed task-specific training using splints and the 11 patients who trained with therapeutic putty are pooled together. Handwriting and drawing was recorded at baseline (week 0), after immobilization (week 4), after four weeks or eight weeks of motor re-training (week 8 and week 12). Values are expressed as mean ± onefold standard deviation (SD). The p-values given in the right column of the table refers to the pair-wise comparison of the kinematic data at week 0 and week 12. NIV = number of inversion in velocity. CV = coefficient of variation of vertical peak velocity.
Acknowledgments
We greatly appreciate the patients and normal volunteers for participating in this study. We would like to thank Dirk Dressler, MD, Department of Neurology at the University of Rostock, Alexander Munchau, MD, Department of Neurology at the University of Hamburg, Lars Timmermann, MD and Markus Butz, PhD, Department of Neurology, University of Düsseldorf for referring patients to us.
This work has been supported by the Deutsche Forschungsgemeinschaft to G. Deuschl and H. Siebner (grant DE 438/7-1 and 7-2). H.R. Siebner was supported by a structural grant sponsored by the Federal Ministry of Education and Research to Neuro-ImageNord (grant 01 GO 0511).
Footnotes
Disclosure: The authors report no conflict of interest. The corresponding author had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Hallett M. Pathophysiology of writer's cramp. Hum Mov Sci. 2006;25(4-5):454–463. doi: 10.1016/j.humov.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Kruisdijk JJ, Koelman JH, Ongerboer de Visser BW, de Haan RJ, Speelman JD. Botulinum toxin for writer's cramp: a randomised, placebo-controlled trial and 1-year follow-up. J Neurol Neurosurg Psychiatry. 2007;78(3):264–270. doi: 10.1136/jnnp.2005.083170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Das CP, Dressler D, Hallett M. Botulinum toxin therapy of writer's cramp. Eur J Neurol. 2006;13(Suppl 1):55–59. doi: 10.1111/j.1468-1331.2006.01446.x. [DOI] [PubMed] [Google Scholar]
- 4.Hallett M. The neurophysiology of dystonia. Arch Neurol. 1998;55(5):601–603. doi: 10.1001/archneur.55.5.601. [DOI] [PubMed] [Google Scholar]
- 5.Berardelli A, Rothwell JC, Hallett M, Thompson PD, Manfredi M, Marsden CD. The pathophysiology of primary dystonia. Brain. 1998;121(Pt 7):1195–1212. doi: 10.1093/brain/121.7.1195. [DOI] [PubMed] [Google Scholar]
- 6.Meunier S, Lehericy S, Garnero L, Vidailhet M. Dystonia: lessons from brain mapping. Neuroscientist. 2003;9(1):76–81. doi: 10.1177/1073858402239593. [DOI] [PubMed] [Google Scholar]
- 7.Peller M, Zeuner KE, Munchau A, et al. The basal ganglia are hyperactive during the discrimination of tactile stimuli in writer's cramp. Brain. 2006;129(Pt 10):2697–2708. doi: 10.1093/brain/awl181. [DOI] [PubMed] [Google Scholar]
- 8.Meunier S, Garnero L, Ducorps A, et al. Human brain mapping in dystonia reveals both endophenotypic traits and adaptive reorganization. Ann Neurol. 2001;50(4):521–527. doi: 10.1002/ana.1234. [DOI] [PubMed] [Google Scholar]
- 9.Pesenti A, Barbieri S, Priori A. Limb immobilization for occupational dystonia: a possible alternative treatment for selected patients. Adv Neurol. 2004;94:247–254. [PubMed] [Google Scholar]
- 10.Zeuner KE, Bara-Jimenez W, Noguchi PS, Goldstein SR, Dambrosia JM, Hallett M. Sensory training for patients with focal hand dystonia. Ann Neurol. 2002;51(5):593–598. doi: 10.1002/ana.10174. [DOI] [PubMed] [Google Scholar]
- 11.Zeuner KE, Hallett M. Sensory training as treatment for focal hand dystonia: a 1-year follow-up. Mov Disord. 2003;18(9):1044–1047. doi: 10.1002/mds.10490. [DOI] [PubMed] [Google Scholar]
- 12.Zeuner KE, Shill HA, Sohn YH, et al. Motor training as treatment in focal hand dystonia. Mov Disord. 2005;20(3):335–341. doi: 10.1002/mds.20314. [DOI] [PubMed] [Google Scholar]
- 13.Schenk T, Bauer B, Steidle B, Marquardt C. Does training improve writer's cramp? An evaluation of a behavioral treatment approach using kinematic analysis. J Hand Ther. 2004;17(3):349–363. doi: 10.1197/j.jht.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Candia V, Wienbruch C, Elbert T, Rockstroh B, Ray W. Effective behavioral treatment of focal hand dystonia in musicians alters somatosensory cortical organization. Proc Natl Acad Sci U S A. 2003;100(13):7942–7946. doi: 10.1073/pnas.1231193100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Priori A, Pesenti A, Cappellari A, Scarlato G, Barbieri S. Limb immobilization for the treatment of focal occupational dystonia. Neurology. 2001;57(3):405–409. doi: 10.1212/wnl.57.3.405. [DOI] [PubMed] [Google Scholar]
- 16.Sheehy MP, Marsden CD. Writers' cramp-a focal dystonia. Brain. 1982;105(Pt 3):461–480. doi: 10.1093/brain/105.3.461. [DOI] [PubMed] [Google Scholar]
- 17.Wissel J, Kabus C, Wenzel R, et al. Botulinum toxin in writer's cramp: objective response evaluation in 31 patients. J Neurol Neurosurg Psychiatry. 1996;61(2):172–175. doi: 10.1136/jnnp.61.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fahn S. Assessment of the primary dystonias. In: Munsat T, editor. The quantification of neurologic deficit. Butterworths; Boston: 1989. pp. 241–270. [Google Scholar]
- 19.Siebner HR, Auer C, Ceballos-Baumann A, Conrad B. Has repetitive transcranial magnetic stimulation of the primary motor hand area a therapeutic application in writer's cramp? Electroencephalogr Clin Neurophysiol Suppl. 1999;51:265–275. [PubMed] [Google Scholar]
- 20.Mai N, Marquardt C. Schreibtraining in der neurologischen Rehabilitation. 2 nd edition ed. Borgmann Publishing; Dortmund: 1999. [Google Scholar]
- 21.Schenk T, Walther EU, Mai N. Closed- and open-loop handwriting performance in patients with multiple sclerosis. Eur J Neurol. 2000;7(3):269–279. doi: 10.1046/j.1468-1331.2000.00068.x. [DOI] [PubMed] [Google Scholar]
- 22.Teulings HL, Contreras-Vidal JL, Stelmach GE, Adler CH. Adaptation of handwriting size under distorted visual feedback in patients with Parkinson's disease and elderly and young controls. J Neurol Neurosurg Psychiatry. 2002;72(3):315–324. doi: 10.1136/jnnp.72.3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siebner HR, Limmer C, Peinemann A, Bartenstein P, Drzezga A, Conrad B. Brain correlates of fast and slow handwriting in humans: a PET- performance correlation analysis. Eur J Neurosci. 2001;14(4):726–736. doi: 10.1046/j.0953-816x.2001.01694.x. [DOI] [PubMed] [Google Scholar]
- 24.Zeuner KE, Peller M, Knutzen A, et al. How to assess motor impairment in writer's cramp. Mov Disord. 2007;22(8):1102–1109. doi: 10.1002/mds.21294. [DOI] [PubMed] [Google Scholar]
- 25.Marquardt C, Mai N. A computational procedure for movement analysis in handwriting. J Neurosci Methods. 1994;52(1):39–45. doi: 10.1016/0165-0270(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 26.Siebner HR, Tormos JM, Ceballos-Baumann AO, et al. Low-frequency repetitive transcranial magnetic stimulation of the motor cortex in writer's cramp. Neurology. 1999;52(3):529–537. doi: 10.1212/wnl.52.3.529. [DOI] [PubMed] [Google Scholar]