Abstract
Objective
To determine the relationship between persistence or change in leisure-time physical activity habits and waist gain among young adults.
Design and Methods
Population-based cohort study among 3383 Finnish twin individuals (1578 men) from five birth cohorts (1975–1979), who answered questionnaires at mean ages of 24.4 y (SD 0.9) and 33.9 y (SD 1.2), with reported self-measured waist circumference. Persistence or change in leisure-time physical activity habits was defined based on thirds of activity metabolic equivalent h/day during follow-up (mean 9.5 y; SD 0.7).
Results
Decreased activity was linked to greater waist gain compared to increased activity (3.6 cm, P<0.001 for men; 3.1 cm, P<0.001 for women). Among same-sex activity discordant twin pairs, twins who decreased activity gained an average 2.8 cm (95%CI 0.4 to 5.1, P=0.009) more waist than their co-twins who increased activity (n=85 pairs); among MZ twin pairs (n=43), the difference was 4.2 cm (95%CI 1.2 to 7.2, P=0.008).
Conclusions
Among young adults, an increase in leisure-time physical activity or staying active during a decade of follow-up was associated with less waist gain, but any decrease in activity level, regardless baseline activity, led to waist gain that was similar to that associated with being persistently inactive.
Keywords: Physical activity, waist circumference, twins, longitudinal studies
Introduction
Prevalence of general and abdominal obesity are high, and increasing both among children and adults, although there are some encouraging signs that the increase is slowing (1–4). Abdominal obesity is a major cardio-metabolic risk factor (5,6), and waist circumference measure is considered to be a valid marker of abdominal obesity (6,7), correlating better than body mass index (BMI) with intra-abdominal fat (6,8).
According to longitudinal studies long-term physical activity is related to smaller waist circumference (9,10) and less abdominal fat (11). However, constant physical activity may be insufficient to prevent age-related waist gain, because waist circumference seems to grow with time despite regular physical activity (10,12). Intervention studies have identified significantly reduced waist circumference after increased physical activity, even without substantial weight loss (13–15). Only a few longitudinal studies have examined the relationship between changed physical activity habits and concordant change in waist circumference, showing that increased physical activity was associated with a lower waist gain (12,16–18). However, longitudinal studies have not focused on early adulthood, when age-related weight and waist gain already seem to escalate (19,20), and many other changes in life occur (i.e. work and family related commitments); thus, young adulthood is a critical but largely unexplored period from the obesity epidemic viewpoint.
Along with environmental effects, genetics plays a role in the development of obesity (21,22) and exercise participation (23). Genetic predispositions can lead to genetic selection bias in studies of the relationship between physical activity and the development of obesity and chronic diseases, by favoring some individuals to attain high physical activity levels or appropriate body composition. The studies of monozygotic (MZ) and dizygotic (DZ) twin pairs make possible to standardize for childhood family environment and fully (MZ pairs) or partially (DZ pairs) for genetic background. Therefore, co-twin control studies are better in revealing the causal relations between physical activity and health outcomes than observational follow-up studies of nonrelated individuals. Of note, while routine daily activity has decreased in modern society, the role of leisure-time physical activity in modifying total energy expenditure has particularly been emphasized (24,25). The purpose of this study was to determine how the persistence or change in leisure-time physical activity during early adulthood is associated with waist gain.
Materials and Methods
Data collection
This study is part of the FinnTwin16 twin cohort study (26) investigating the role of genetic and environmental factors as determinants of different health behaviors, disease risk factors and chronic disease. Virtually all twins born in 1975–1979 were identified from the Finnish population register for FinnTwin16. The follow-up cohort includes about 5500 individuals and almost 2700 twin pairs. Data collection for this follow-up study started in 1991, and participants were sent the first questionnaire within two months of their 16th birthday. Later, questionnaires were mailed when participants were 17 and 18.5 years old. The 4th wave questionnaire was collected on 2000–2002, when the participants were on average 24.5 years old. The 5th wave of data collection was done in 2010–2012 when the participants were a mean age of 34.0 years.
Waves 4 and 5 were used for the present study. Wave 4, the baseline for this report, was done using a postal paper questionnaire, and wave 5, the follow-up was conducted using a web-based questionnaire, both including questions related to health, body composition and leisure-time physical activity. The response rates for the overall cohort were 84.5% and 71.9% for waves 4 and 5, respectively, with 77.9% of those replying at wave 4 also replying at wave 5.
The study was conducted according to ethical standards and the Declaration of Helsinki, and approved by the ethical committee of the Central Finland Hospital district. Participants gave their informed consent.
Participants
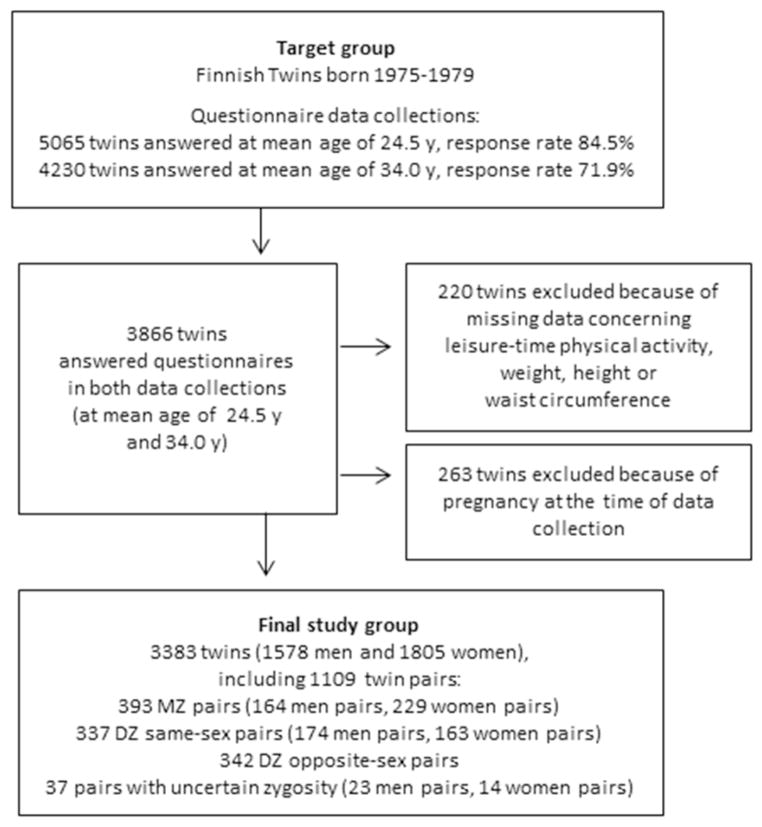
Altogether 3866 twin individuals from five consecutive birth cohorts (1975–1979) answered both questionnaires (baseline and follow-up). We included in this study all participants who answered at both collections the questions related to leisure-time physical activity, weight and height, and measured their waist circumference. All who had responded affirmative to being pregnant at the time of data collection were excluded from this study (n=263). After exclusions, the final study group consisted of 1578 men and 1805 women (total N=3383, including 1109 twin pairs of which 393 were known to be MZ pairs and 679 DZ pairs) (Figure 1). Determination of zygosity was based on accurate and validated questionnaire method (27).
Figure 1.
Flow chart of participants and data collection.
Measurement of waist circumference
Self-measurement of waist circumference was done using a supplied tape measure at both data collections; in wave 5, it was included in the mailed invitation letter that contained the access code to the Internet survey. The instructions with an illustration for measuring waist circumference were included in the questionnaire. Waist circumference was measured while standing, at either the narrowest part of the waist, or if that was not found, the midpoint between the lowest part of the ribs and top of the hip bone. The intra-class correlation between self-measured and healthcare professional-measured waist circumference (n=24) is 0.97 (P<0.001) (9). A change in waist circumference was calculated as the difference between follow-up and baseline data collection.
Assessment of leisure-time physical activity
The assessment of leisure-time physical activity was based on a series of questions covering leisure-time physical activity and physical activity during journeys to and from work. These questions were identical at waves 4 and 5. Validity information of physical activity questions is available in detail elsewhere (9). The questionnaire included three structured questions about leisure-time physical activity. First, average monthly frequency of activity with seven response alternatives: 1) not at all, 2) less than once a month, 3) 1–2 times a month, 4) about once a week, 5) 2–3 times a week, 6) 4–5 times a week, 7) about every day. Second, average duration of one session of activity with four response alternatives: 1) under 30min, 2) 30min - under 1h, 3) 1h - under 2h, 4) 2h or more. Third, intensity of activity based on the following question: Is your physical activity during leisure-time about as strenuous on average as: 1) walking, 2) alternately walking and jogging, 3) jogging, 4) running. Physical activity during journeys to and from work was included to leisure-time physical activity, and it was assessed with a question about the average time used for walking, bicycling, jogging, skiing or/and roller-skating in one day for work journeys with five response alternatives: 1) under 15min, 2) 15min - under 30min, 3) 30min - under 1h, 4) 1h or more, 5) I do not work or study. The frequency for this commuting activity was set at five times a week and intensity as corresponding to walking. A leisure-time physical activity MET (metabolic equivalent) index was calculated by assigning a multiple of the resting metabolic rate (intensity×duration×frequency). It was expressed as a sum score of leisure time physical activity MET hours per day as described earlier (28) with modifications to account for the slightly different response alternatives of the related questions in the present questionnaires.
Persistence or change in leisure-time physical activity habits was evaluated by dividing participants into sex-specific thirds using tertiles computed from the leisure-time physical activity MET index at baseline and follow-up (Table 1). The participants in the first thirds were categorized as inactive, in the second as moderately active, and in the third as active. Persistence or change in leisure-time physical activity habits was based on remaining in the same category during the follow-up or changing to another category (nine groups in total).
Table 1.
Characteristics of participants at baseline and at follow-up by sex and leisure-time physical activity categoriesa
| Men (N=1578) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Baseline |
Follow-up |
|||||||
| Inactive (n=488) | Moderately active (n=521) | Active (n=569) | P c | Inactive (n=525) | Moderately active (n=527) | Active (n=526) | P c | |
| LTPA MET hours per dayb | MET<2.3 | 2.3≤MET<6.8 | MET≥6.8 | MET<2.2 | 2.2≤MET<5.4 | MET≥5.4 | ||
|
|
|
|||||||
| Age, mean (SD), y | 24.4 (0.9) | 24.4 (0.9) | 24.4 (1.0) | - | 34.0 (1.2) | 33.8 (1.1) | 33.8 (1.2) | *† |
| Weight, mean (SD), kg | 77.7 (13.7) | 76.1 (11.8) | 77.1 (10.2) | - | 85.1 (14.8) | 82.6 (13.9) | 81.8 (11.6) | *† |
| Height, mean (SD), cm | 179.3 (6.6) | 179.3 (6.3) | 179.9 (6.7) | - | 179.5 (6.6) | 179.2 (6.3) | 179.9 (6.9) | - |
| BMI, mean (SD), kg/m2 | 24.1 (3.7) | 23.6 (3.1) | 23.8 (2.6) | - | 26.4 (4.1) | 25.7 (3.8) | 25.2 (3.1) | *†‡ |
| Waist circumference, mean (SD), cm | 87.3 (11.1) | 85.2 (9.1) | 83.7 (7.1) | *†‡ | 95.2 (12.0) | 92.1 (10.3) | 89.7 (9.0) | *†‡ |
| P | P | |||||||
| Work-related physical activity, n (%) | <0.001 | 0.005 | ||||||
| Sedentary | 185 (38.1) | 254 (49.0) | 273 (48.1) | 208 (39.7) | 267 (50.7) | 258 (49.0) | ||
| Standing or walking at work | 72 (14.8) | 100 (19.3) | 117 (20.7) | 100 (19.1) | 92 (17.5) | 110 (20.9) | ||
| Light manual work | 114 (23.5) | 94 (18.1) | 102 (18.0) | 115 (21.9) | 93 (17.6) | 95 (18.1) | ||
| Heavy manual work | 73 (15.0) | 44 (8.5) | 59 (10.4) | 74 (14.1) | 57 (10.8) | 45 (8.6) | ||
| Not working or studying | 42 (8.6) | 26 (5.0) | 15 (2.7) | 27 (5.2) | 18 (3.4) | 18 (3.4) | ||
| Educational level, n (%) | <0.001 | |||||||
| Primary | 21 (4.0) | 19 (3.6) | 11 (2.1) | |||||
| Secondary | 303 (57.8) | 224 (42.5) | 245 (46.6) | |||||
| Tertiary | 200 (38.2) | 284 (53.9) | 270 (51.3) | |||||
| Children, [n (%)] | <0.001 | 0.02 | ||||||
| Yes | 74 (15.2) | 47 (9.0) | 38(6.7) | 315 (60.2) | 295 (56.0) | 272 (51.7) | ||
| No | 412 (84.8) | 474 (91.0) | 531 (93.3) | 208 (39.8) | 232 (44.0) | 254 (48.3) | ||
| Chronic diseases, n (%) | 0.39 | 0.02 | ||||||
| Yes | 62 (12.2) | 52 (10.1) | 64 (11.4) | 98 (18.7) | 73 (13.9) | 67 (12.8) | ||
| No | 421 (87.2) | 464 (89.9) | 497 (88.6) | 426 (81.3) | 453 (86.1) | 457 (87.2) | ||
| Smoking status, n (%) | <0.001 | <0.001 | ||||||
| Current (daily) smoker | 219 (44.9) | 146 (28.0) | 95 (16.7) | 153 (29.1) | 86 (16.3) | 75 (14.3) | ||
| Occasional smoker | 64 (13.1) | 83 (15.9) | 102 (17.9) | 70 (13.3) | 74 (14.1) | 50 (9.5) | ||
| Quitters | 55 (11.3) | 82 (15.7) | 89 (15.6) | 121 (23.0) | 120 (22.8) | 115 (21.9) | ||
| Never smoked | 150 (30.7) | 210 (40.3) | 283 (49.7) | 181 (34.5) | 246 (46.8) | 286 (54.4) | ||
| Alcohol use, n (%) | 0.03 | 0.003 | ||||||
| Daily | 21 (4.3) | 10 (1.9) | 8 (1.4) | 44 (8.4) | 24 (4.6) | 17 (3.2) | ||
| 1–2 times/week | 281 (57.7) | 311 (59.8) | 319 (56.2) | 318 (60.7) | 316 (60.0) | 294 (55.9) | ||
| 1–2 times/month | 120 (24.6) | 123 (23.7) | 168 (29.5) | 95 (18.1) | 117 (22.2) | 126 (24.0) | ||
| Less than once a month | 42 (8.6) | 39 (7.5) | 42 (7.4) | 41 (7.8) | 41 (7.8) | 53 (10.1) | ||
| Never | 23 (4.7) | 37 (7.1) | 31 (5.4) | 26 (5.0) | 29 (5.5) | 36 (6.8) | ||
| Women (N=1805) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Baseline |
Follow-up |
|||||||
| Inactive (n=562) | Moderately active (n=635) | Active (n=608) | P c | Inactive (n=591) | Moderately active (n=611) | Active (n=603) | P c | |
| LTPA MET hours per dayb | MET<2.5 | 2.5≤MET<5.5 | MET≥5.5 | MET<2.0 | 2.0≤MET<5.0 | MET≥5.0 | ||
|
|
|
|||||||
| Age, mean (SD), y | 24.3 (0.9) | 24.3 (0.9) | 24.3 (0.9) | - | 33.9 (1.3) | 33.9 (1.2) | 33.9 (1.2) | - |
| Weight, mean (SD), kg | 61.8 (12.0) | 61.5 (10.0) | 59.9 (7.9) | †‡ | 67.4 (14.8) | 66.2 (13.2) | 63.9 (10.3) | †‡ |
| Height, mean (SD), cm | 165.4 (5.8) | 165.8 (5.4) | 166.6 (5.9) | †‡ | 165.6 (5.8) | 165.8 (5.8) | 166.4 (5.6) | † |
| BMI, mean (SD), kg/m2 | 22.5 (4.0) | 22.3 (3.3) | 21.6 (2.5) | †‡ | 24.6 (5.2) | 24.1 (4.6) | 23.0 (3.4) | †‡ |
| Waist circumference, mean (SD), cm | 76.1 (10.2) | 74.9 (8.6) | 72.4 (7.0) | *†‡ | 83.0 (13.2) | 80.7 (11.1) | 77.9 (9.5) | *†‡ |
| P | P | |||||||
| Work-related physical activity, n (%) | <0.001 | <0.001 | ||||||
| Sedentary | 222 (39.6) | 294 (46.3) | 289 (47.5) | 238 (40.3) | 228 (37.3) | 261 (43.4) | ||
| Standing or walking at work | 83 (14.8) | 128 (20.2) | 131 (21.5) | 84 (14.2) | 143 (23.4) | 131 (21.8) | ||
| Light manual work | 114 (20.4) | 126 (19.9) | 127 (20.9) | 131 (22.2) | 143 (23.4) | 140 (23.3) | ||
| Heavy manual work | 23 (4.1) | 15 (2.4) | 18 (3.1) | 13 (2.2) | 7 (1.1) | 16 (2.7) | ||
| Not working or studying | 118 (21.1) | 71 (11.2) | 43 (7.1) | 124 (21.0) | 90 (14.7) | 54 (9.0) | ||
| Educational level, n (%) | 0.002 | |||||||
| Primary | 20 (3.4) | 5 (0.8) | 14 (2.3) | |||||
| Secondary | 242 (40.9) | 263 (43.0) | 213 (35.3) | |||||
| Tertiary | 329 (55.7) | 343 (56.1) | 376 (62.4) | |||||
| Children, n (%) | <0.001 | <0.001 | ||||||
| Yes | 121 (21.5) | 84 (13.2) | 41 (6.7) | 431 (72.9) | 372 (61.0) | 326 (54.1) | ||
| No | 441 (78.5) | 551 (86.8) | 567 (93.3) | 160 (27.1) | 238 (39.0) | 277 (45.9) | ||
| Chronic diseases, n (%) | 0.25 | 0.46 | ||||||
| Yes | 74 (13.3) | 69 (11.0) | 62 (10.2) | 104 (17.6) | 107 (17.5) | 92 (15.3) | ||
| No | 484 (86.7) | 557 (89.0) | 543 (89.8) | 486 (82.4) | 503 (82.5) | 511 (84.7) | ||
| Smoking status, n (%) | <0.001 | 0.05 | ||||||
| Current (daily) smoker | 173 (30.8) | 144 (22.7) | 100 (16.4) | 109 (18.4) | 105 (17.2) | 70 (11.6) | ||
| Occasional smoker | 90 (16.0) | 78 (12.3) | 97 (16.0) | 52 (8.8) | 47 (7.7) | 59 (9.8) | ||
| Quitters | 80 (14.2) | 97 (15.3) | 69 (11.3) | 120 (20.3) | 126 (20.7) | 125 (20.7) | ||
| Never smoked | 219 (39.0) | 316 (49.8) | 342 (56.2) | 310 (52.5) | 332 (54.4) | 349 (57.9) | ||
| Alcohol use, n (%) | 0.92 | 0.007 | ||||||
| Daily | 3 (0.5) | 1 (0.2) | 3 (0.5) | 14 (2.4) | 3 (0.5) | 2 (0.3) | ||
| 1–2 times/week | 238 (42.3) | 259 (40.7) | 254 (41.8) | 220 (37.2) | 259 (42.4) | 248 (41.1) | ||
| 1–2 times/month | 201 (35.8) | 242 (38.1) | 221 (36.4) | 175 (29.5) | 192 (31.4) | 178 (29.5) | ||
| Less than once a month | 91 (16.2) | 96 (15.1) | 101 (16.6) | 145 (24.5) | 116 (19.0) | 135 (22.4) | ||
| Never | 29 (5.2) | 37 (5.8) | 28 (4.6) | 38 (6.4) | 41 (6.7) | 40 (6.6) | ||
Abbreviations: LTPA, leisure-time physical activity; MET, metabolic equivalent; SD, standard deviation; BMI, body mass index
Physical activity category by LTPA MET h/day: lowest tertile: inactive; middle tertile: moderately active; highest tertile: active
Leisure-time physical activity and physical activity during journeys to and from work
Continuous variables; significant differences (P<0.05) between activity groups are coded:
inactive vs. moderately active,
inactive vs. active,
moderately active vs. active
Assessment of confounding factors
Baseline BMI (kg/m2), calculated from self-reported height and weight (29), as well age at follow-up and the number of children at follow-up were used as continuous variables in adjusted analysis. Work-related physical activity at follow-up was assessed with the question about how strenuous work or studies are physically, see classification in table 1. The question was slightly modified from Kujala et al. (30). Educational level was defined as a highest level reached at follow-up. This question about education completed was re-categorized as follows: 1) primary and compulsory education (nine years), 2) secondary vocational and academic (up to 12 years), 3) tertiary education (>12 years, i.e. university and polytechnics) (31). Chronic diseases were reported as having/not having chronic disease or handicap interfering daily activities (32). Alcohol use at follow-up was assessed by asking the frequency of drinking any alcohol (32), and responses were classified into five categories (see table 1). Smoking status was defined as 1) current smoker, 2) occasional smoker, 3) quitter, 4) never smoked, according to structured question (32).
Statistical analysis
Data were analyzed using Stata 12.0 (Stata Corp., College Station, TX, USA) and SPSS Statistics 20.0 (IBM Corp., Armonk, NY, USA). All individual–based analyses were done separately for men and women and carried out by taking into account clustered observations of twins within pairs. The differences in characteristics of the participants between leisure-time physical activity categories (inactive, moderately active, active) were analyzed with the adjusted Wald test for continuous variables and Pearson’s χ2 test for categorical variables.
The F-test (analysis of variance) with the clustered option for twin pairs was used to compare differences in waist gain during follow-up among nine different leisure-time physical activity groups (persistently inactive vs. other groups).
To further confirm the role of decreased or increased leisure-time physical activity in waist gain, we re-categorized all same sex (MZ and DZ) twin pairs as well only MZ twin pairs in which one twin was more active than the co-twin. With these categories, we performed pairwise comparison of waist gain between 1) those who decreased activity (any change from higher third to a lower one) and who increased activity (any change from a lower third to a higher one); 2) the persistently inactive and those who changed from inactive to moderately active or active; and 3) the persistently active and those who changed from active to moderately active or inactive. Normally distributed data were analyzed with two-sided paired-sample t-tests and non-normally distributed data with the Wilcoxon signed-rank test. The same re-categorizing and comparison were done also at the individual level. In all analyses the level of statistical significance was set at P <0.05.
Results
Characteristics of participants
Over an almost 10- year follow-up (mean 9.5 y; SD 0.7, median 10.0 y), the mean waist circumference increased 7.0 cm (SD 8.1) for men and 6.1 cm (SD 8.2) for women. BMI increased during the follow-up 1.9 kg/m2 (SD 2.4) for men and 1.8 kg/m2 (SD 2.8) for women. Characteristics of the study participants stratified by leisure-time physical activity level (active, moderately active, inactive) and sex at baseline and follow-up are shown in Table 1. Waist circumference differed significantly among activity groups in both men and women at baseline and follow-up. Inactive men had an average greater body weight than moderately active or active men, and BMI differed among all groups at follow-up, but not at baseline. Active women had lower mean body weight and BMI than moderately active and inactive women both at baseline and follow-up. Active and moderately active men appeared to be slightly more educated than inactive men, and the latter more often had work with a high occupational loading. In women, those who were not working or studying were more often inactive than those who were working. Both men and women who had children were less often physically active than those without children. Participants with chronic diseases were distributed equally across all leisure-time groups, except that inactive men more often had chronic diseases than others at follow-up. Less active people were more often current smokers and daily alcohol users, especially among men.
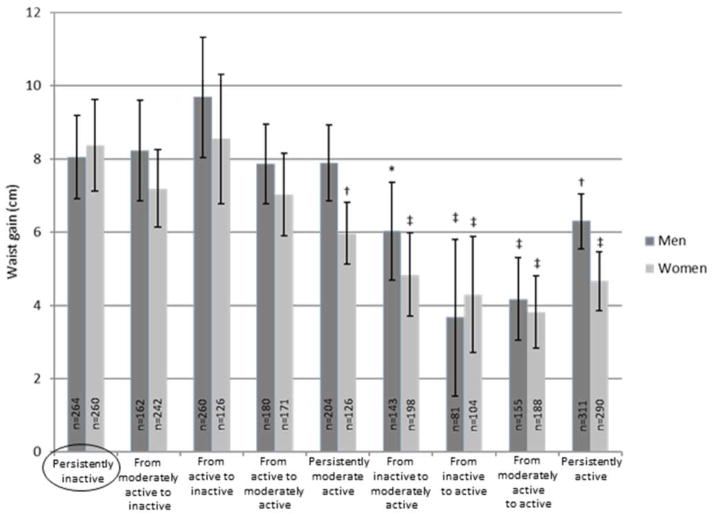
Association between persistence or change in leisure-time physical activity and waist gain in individual based analysis
Waist circumference increased in both sexes in all leisure-time physical activity groups (persistence or change) (mean waist gain from 3.7 to 9.7 cm by group) during the follow-up (Figure 2, Table 2). When comparing the waist gain of persistently inactive people to all other groups (Figure 2, Table 2), persistently active men or men who increased activity during follow-up gained less waist than the persistently inactive respondents did (P<0.05). Men who decreased activity or stayed only moderately active got waist similar to that associated with being persistently inactive. Women, who stayed at least moderately active or increased activity during follow-up, gained less waist than persistently inactive women (P<0.01). Women who decreased activity level during the follow-up got waist as those who stayed persistently inactive. Further, the highest mean waist gain occurred in men and women who changed from active to inactive during the follow-up. Adjusting for potential confounders, such as age, baseline waist circumference and BMI, work-related physical activity, educational level, number of children, chronic diseases, smoking status and alcohol use, did not change the results substantially (Table 2).
Figure 2.
Persistence or change in leisure-time physical activity and waist gain (cm, mean and 95%CI) during follow-up. Significant differences are coded (persistently inactive as a reference group): * P<0.05, † P<0.01, ‡ P<0.001.
Table 2.
Differences in waist gain during follow-up by sex and adjusted for potential cofounders. Model with each potential confounder added individually to a model with waist gain as the dependent variable and physical activity as the independent variable.
| Persistence or change
in leisure-time physical activity |
Waist gaina | No covariates in the model |
Waist gain adjusted for: |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y)c | Baseline WC (cm)c |
Baseline BMI (kg m−2)c |
Work- related physical activityd |
Educational leveld |
Childr enc |
Chronic diseasesd |
Smoking statusd |
Alcoh ol used |
||||
|
| ||||||||||||
| N (%) | Mean (95%CI), cm | |||||||||||
|
Pb
|
||||||||||||
| MEN | ||||||||||||
| 1. Persistently inactive | 264 (16.7) | 8.1 (6.9 to 9.2) | Reference group | |||||||||
| 2. From moderately active to inactive | 162 (10.3) | 8.2 (6.9 to 9.6) | 0.85 | 0.87 | 0.91 | 0.84 | 0.92 | 0.70 | 0.70 | 0.83 | 0.82 | 0.85 |
| 3. From active to inactive | 99 (6.3) | 9.7 (8.0 to 11.3) | 0.11 | 0.12 | 0.14 | 0.11 | 0.11 | 0.09 | 0.23 | 0.14 | 0.14 | 0.14 |
| 4. From active to moderately active | 180 (11.4) | 7.9 (6.8 to 9.0) | 0.82 | 0.78 | 0.49 | 0.83 | 0.72 | 0.88 | 0.69 | 0.85 | 0.92 | 0.97 |
| 5. Persistently moderate active | 204 (12.9) | 7.9 (6.9 to 8.9) | 0.84 | 0.79 | 0.62 | 0.85 | 0.73 | 0.82 | 0.55 | 0.85 | 0.86 | 0.93 |
| 6. From inactive to moderately active | 143 (9.1) | 6.0 (4.7 to 7.4) | 0.03 | 0.02 | 0.02 | 0.03 | 0.02 | 0.04 | 0.04 | 0.03 | 0.02 | 0.04 |
| 7. From inactive to active | 81 (5.1) | 3.7 (1.5 to 5.8) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.01 | <0.001 | <0.001 | <0.001 |
| 8. From moderately active to active | 155 (9.8) | 4.2 (3.1 to 5.3) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 9. Persistently active | 290 (18.4) | 6.3 (5.6 to 7.1) | 0.01 | 0.01 | 0.003 | 0.01 | 0.01 | 0.04 | 0.02 | 0.02 | 0.02 | 0.03 |
| WOMEN | ||||||||||||
| 1. Persistently inactive | 260 (14.4) | 8.4 (7.1 to 9.6) | Reference group | |||||||||
| 2. From moderately active to inactive | 205 (11.4) | 7.2 (6.1 to 8.3) | 0.16 | 0.15 | 0.14 | 0.16 | 0.15 | 0.23 | 0.74 | 0.17 | 0.19 | 0.16 |
| 3. From active to inactive | 126 (7.0) | 8.5 (6.8 to 10.3) | 0.88 | 0.90 | 0.94 | 0.86 | 0.86 | 0.73 | 0.91 | 0.79 | 0.82 | 0.73 |
| 4. From active to moderately active | 171 (9.5) | 7.0 (5.9 to 8.2) | 0.11 | 0.11 | 0.06 | 0.12 | 0.12 | 0.19 | 0.65 | 0.14 | 0.14 | 0.15 |
| 5. Persistently moderate active | 242 (13.4) | 6.0 (5.1 to 6.8) | 0.002 | 0.002 | 0.001 | 0.002 | 0.002 | 0.003 | 0.17 | 0.002 | 0.002 | 0.003 |
| 6. From inactive to moderately active | 198 (11.0) | 4.8 (3.7 to 6.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.01 | <0.001 | <0.001 | <0.001 |
| 7. From inactive to active | 104 (5.8) | 4.3 (2.7 to 5.9) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.02 | <0.001 | <0.001 | <0.001 |
| 8. From moderately active to active | 188 (10.4) | 3.8 (2.8 to 4.8) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 9. Persistently active | 311 (17.2) | 4.7 (3.9 to 5.5) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.009 | <0.001 | <0.001 | <0.001 |
Abbreviations: WC, waist circumference; BMI, body mass index; CI, confidence interval
Overall observed change in waist circumference between baseline and follow-up
P value for difference in waist gain during follow-up compared to persistently inactive
used as continuous variable
used as categorical variable
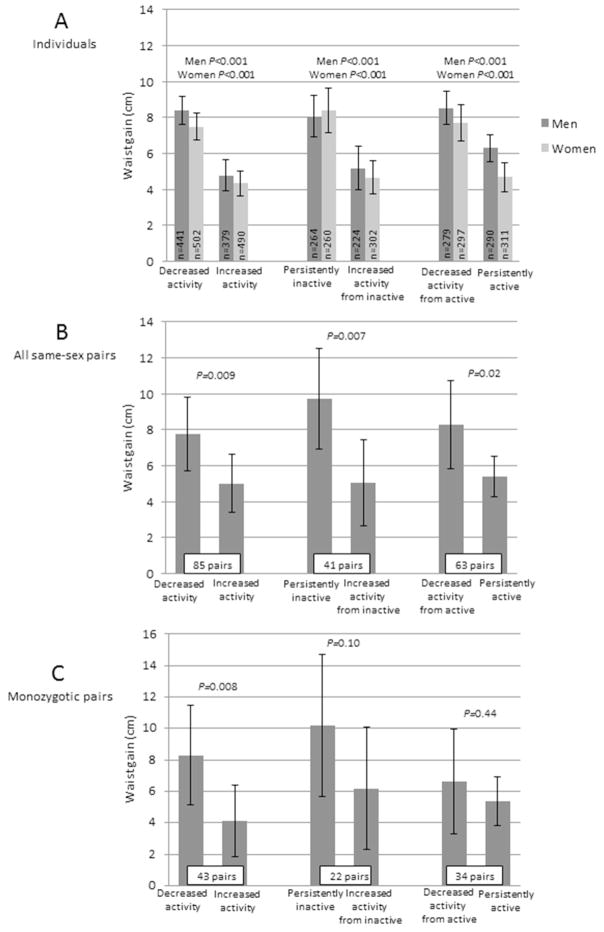
When comparing waist gain of all participants who decreased leisure-time physical activity (men 8.4 cm; 95%CI 7.6 to 9.2, women 7.5 cm; 95%CI 6.7 to 8.2) to those who increased activity during follow-up (men 4.8 cm; 95%CI 3.9 to 5.6, women 4.3 cm; 95%CI 3.6 to 5.0), the difference was statistically significant (P<0.001) (Figure 3a). The persistently inactive (men 8.1 cm; 95%CI 6.9 to 9.2, women 8.4 cm; 95%CI 7.1 to 9.6) gained more circumference than those, who were inactive at baseline but increased activity (men 5.2 cm; 95%CI 4.0 to 6.4, women 4.7 cm; 95%CI 3.7 to 5.6) during follow-up. Persistently active respondents (men 6.3 cm; 95%CI 5.6 to 7.1, women 4.7 cm; 95%CI 3.9 to 5.5) gained significantly less circumference than those who were active at baseline but decreased activity (men 8.5 cm; 95%CI 7.6 to 9.4, women 7.7 cm; 95%CI 6.7 to 8.7) during follow-up.
Figure 3.
Differences in waist gain (cm, mean and 95%CI) during follow-up (decreased activity: changed from upper third to a lower one; increased activity: changed from a lower third to upper one). A. Sex-specific differences among individuals taking into account clustered observation of twin pairs. B. Pairwise difference among leisure-time physical activity discordant same sex twin pairs. C. Pairwise differences among leisure-time physical activity discordant monozygotic twin pairs.
Pairwise analysis among physical activity discordant twin pairs
Among leisure-time physical activity discordant twin pairs, twins who decreased physical activity during the follow-up gained an average 2.8 cm (95%CI 0.4 to 5.1, P=0.009) more waist than their co-twins who increased physical activity (n=85 pairs); among MZ twin pairs (n=43), the difference was 4.2 cm (95%CI 1.2 to 7.2, P=0.008) (Figure 3b and c, Table 3). These pairwise differences remained statistically significant when each waist measure was first divided by the corresponding BMI value (P=0.027 for all pairs, 0.027 for MZ pairs). When comparing persistently inactive twins to their co-twins who were inactive at baseline but increased activity during follow-up, the mean difference in waist gain was 4.7 cm (95%CI 1.3 to 8.0) for all 41 pairs (P=0.007) and 4.0 cm (95%CI, −0.8 to 8.8) for 22 MZ pairs (P=0.10). Although the difference in waist gain between those who were active at baseline but decreased activity during follow-up and those who were persistently active was not significant among MZ twin pairs (n=43) (1.2 cm; 95%CI −1.9 to 4.4, P=0.44), it was among all same-sex twin pairs (n=85)(2.9 cm; 95%CI 0.5 to 5.3, P=0.02).
Table 3.
Pairwise differences in waist gain during follow-up between leisure-time physical activity discordant twin pairs.
| All same sex twin pairs | Waist gain during follow-up |
Monozygotic twin pairs | Waist gain during follow-up |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Twin 1 | Twin 2 | Twin 1 | Twin 2 | |||||||
|
|
|
|||||||||
| Pairs, N | Mean (SD), cm | Mean (SD), cm | Mean difference (95%CI) | P | Pairs, N | Mean (SD), cm | Mean (SD), cm | Mean difference (95%CI) | P | |
| Decreased activity (twin 1) vs. increased activity (twin 2) | 85 (men=31) | 7.7 (9.5) | 5.0 (7.5) | 2.8 (0.4 to 5.1) | 0.009 | 43 (men=16) | 8.3 (10.3) | 4.2 (7.3) | 4.2 (1.2 to 7.2) | 0.008 |
| Persistently inactive (twin 1) vs. from inactive to moderately active or active (twin 2) | 41 (men=16) | 9.7 (8.8) | 5.1 (7.6) | 4.7 (1.3 to 8.0) | 0.007 | 22 (men=9) | 10.2 (10.1) | 6.2 (8.8) | 4.0 (−0.8 to 8.8) | 0.10 |
| From active to moderately active or inactive (twin 1) vs. persistently active (twin 2) | 63 (men=30) | 8.3 (9.8) | 5.4 (4.5) | 2.9 (0.5 to 5.3) | 0.02 | 34 (men=15) | 6.6 (9.5) | 5.4 (4.4) | 1.2 (−1.9 to 4.4) | 0.44 |
Abbreviations: SD, standard deviation; CI, confidence interval
Discussion
In this twin cohort study of young adults, an increase in leisure-time physical activity (shifting from a lower third to a higher one) or staying active was associated with less waist gain over the almost 10-year follow-up period. Any decrease in leisure-time physical activity during the follow-up, regardless of starting category, led to a waist gain similar to that of persistently inactive respondents.
Earlier studies among young adults have reported rather similar age-related mean waist circumference growth during follow-up (10) as well as among middle-aged and older populations (12,16). In particular our results stress the associations between changes in physical activity and waist gain. Although similar associations have been observed previously (12, 16–18), prior studies did not focus on early adulthood, a period when age-related weight and waist gain already seem to escalate (19,20), even as many other changes in lifestyle and health occur. Earlier follow-up studies have also often focused on the relationship between prolonged physical activity habits and weight and waist gain (9,10). What is important to note from the current findings is that decreasing physical activity regardless of baseline activity level is related to increased waist gain. This may have an influence on the results of those studies which only look at the predictive value of baseline physical activity on follow-up waist or obesity. In our study 52% of men and 57% of women changed their leisure-time physical activity habits according to our criteria. More research is needed on to determine how to prevent increased waist gain among those who must decrease physical activity for various reasons.
Our results did not substantially change after adjusting the effect of physical activity change on waist gain for potential confounders such as baseline waist circumference, BMI, work-related physical activity, educational level, number of children, chronic diseases, smoking status or alcohol use. We could not adjust our results for energy intake; however, our earlier study in older twins showed that although the physically active were leaner, their daily energy intake was higher than that of their inactive co-twins (33).
As genetics plays a role in exercise participation (23) and development of obesity (21,22), it may be easier for some individuals to achieve high levels of physical activity and appropriate body composition. This may lead to selection bias in observational follow-up studies of nonrelated individuals, and make it difficult to assess the true extent of the causal relation between physical activity and health outcomes. With pairwise analysis among all same-sex twin pairs and MZ twin pairs, we could consider genetic background and childhood environment, including differences in, for example, social class and education, family structure and parenting practice. Pairwise analysis confirmed the importance of maintaining or increasing leisure-time physical activity and the risk of decreasing activity for waist gain, and gave evidence for causal relation between physical activity and reduced waist gain. As expected, the relatively small number of physical activity discordant MZ pairs reduced the power to detect possible differences in some comparisons.
We focused particularly on leisure-time physical activity instead of total daily activity because modifying total daily energy expenditure through leisure-time physical activity is emphasized currently while physical activity related to daily routines (e.g. work and household) has decreased (24,25). We decided to use age-specific thirds when participants were divided to physical activity classes (inactive, moderately active, active), since average physical activity level seems to change with time in population. Use of age-specific cut-offs leads to better statistical power. In our study sample the number of participants, who were active at baseline and then even increased their level of physical activity at follow-up, remained low. Consequently, analysis concerning this interesting target group was not carried out. Both assessment of leisure-time physical activity and waist circumference measurement were self-reported, which can lead to reporting bias, but made large observational data collection possible. Because we had two follow-up points, it is not possible to determine when changes in leisure-time physical activity occurred, or interpret causality. However, our pairwise analyses among monozygotic physical activity discordant twin pairs gave evidence for causal relation between physical activity and reduced waist gain. We focused particularly on waist gain instead of BMI because abdominal obesity is an independent risk factor for all-cause mortality (34) and cardio-metabolic diseases (35–37). Furthermore, when the waist circumference was divided by the corresponding BMI value, the change in this ratio differed significantly between the twins who decreased physical activity compared to their co-twins who increased physical activity, supporting the importance of waist measurement as an indicator of the effect of physical activity. Compared to the general population the BMI values of our twins are similar level or slightly lower (38) meaning that the generalizability of the results is good.
In conclusion, regardless of physical activity level, waist circumference increased during young adulthood. To attenuate this waist gain, increased leisure-time physical activity or staying active seemed to be essential for both sexes. In contrast, despite the starting level, any decrease in leisure-time physical activity led to waist gain that was similar to that associated with being persistently inactive. These findings deliver an important public health message to promote high leisure-time physical activity habits from early adulthood onward to prevent age-related abdominal obesity. Physical activity level seems often to decrease during early adulthood, and thus our results highlight also the need to establish how increased waist gain can be attenuated among those people.
‘What is already known about this subject?’
Abdominal obesity is an alarming health problem, and leisure-time physical activity has the potential to prevent age-related waist gain.
Physical activity is related to smaller waist circumference and less abdominal fat. However, constant physical activity may be insufficient to prevent age-related waist gain.
‘What this study adds?’
Changes in an easily measured waist circumference, which correlates well with many cardio-metabolic risk factors, are associated with the changes in leisure-time physical activity habits already in early adulthood.
Our pairwise analyses among monozygotic physical activity discordant twin pairs (comparing twins who decreased activity to their co-twins who increased activity), controlled for segregating genes. This gives evidence for causal relation between physical activity and reduced waist gain.
Acknowledgments
We thank Markku Kauppinen for expert advice concerning statistical data analysis. Data collection in FinnTwin16 has been made possible by the Academy of Finland (grants 100499, 205585, 118555, and 141054 to JK), the National Institute of Alcohol Abuse and Alcoholism (grants AA-12502, AA-00145, and AA-09203 to Richard J Rose), and the Finnish Ministry of Education and Culture (UK). Analyses have been supported by Juho Vainio Foundation (MR), Finnish Ministry of Education and Culture (UK), META-PREDICT (within the European Union Seventh Framework Programme, HEALTH-F2-2012-277936 to UK), and Academy of Finland (grants 265240, and 263278 to JK).
Footnotes
Competing interests: the authors have no competing interests.
Study conception and design: MR, KHP, JK, UMK; Acquisition of data: MR, KHP, JK, UMK; Statistical analysis: MR; Interpretation of data: MR, JK, UMK; Drafting the manuscript: MR, UMK; Critical revision of the manuscript and final approval of the version to be published: MR, KHP, JK, UMK.
References
- 1.Li C, Ford ES, Mokdad AH, Cook S. Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics. 2006;118:e1390–1398. doi: 10.1542/peds.2006-1062. [DOI] [PubMed] [Google Scholar]
- 2.Lahti-Koski M, Harald K, Männistö S, Laatikainen T, Jousilahti P. Fifteen-year changes in body mass index and waist circumference in Finnish adults. Eur J Cardiovasc Prev Rehabil. 2007;14:398–404. doi: 10.1097/HJR.0b013e32800fef1f. [DOI] [PubMed] [Google Scholar]
- 3.Lilja M, Eliasson M, Stegmayr B, Olsson T, Söderberg S. Trends in obesity and its distribution: Data from the Northern Sweden MONICA Survey, 1986–2004. Obesity (Silver Spring) 2008;16:1120–1128. doi: 10.1038/oby.2008.8. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 5.Dixon JB. The effect of obesity on health outcomes. Mol Cell Endocrinol. 2010;316:104–108. doi: 10.1016/j.mce.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: A Consensus Statement from Shaping America’s Health: Association for weight management and obesity prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Diabetes Care. 2007;30:1647–1652. doi: 10.2337/dc07-9921. [DOI] [PubMed] [Google Scholar]
- 7.Rankinen T, Kim SY, Perusse L, Despres JP, Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int J Obes Relat Metab Disord. 1999;23:801–809. doi: 10.1038/sj.ijo.0800929. [DOI] [PubMed] [Google Scholar]
- 8.Molarius A, Seidell JC. Selection of anthropometric indicators for classification of abdominal fatness - a critical review. Int J Obes Relat Metab Disord. 1998;22:719–727. doi: 10.1038/sj.ijo.0800660. [DOI] [PubMed] [Google Scholar]
- 9.Waller K, Kaprio J, Kujala UM. Associations between long-term physical activity, waist circumference and weight gain: A 30-year longitudinal twin study. Int J Obes (Lond) 2008;32:353–361. doi: 10.1038/sj.ijo.0803692. [DOI] [PubMed] [Google Scholar]
- 10.Hankinson AL, Daviglus ML, Bouchard C, Carnethon M, Lewis CE, Schreiner PJ, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304:2603–2610. doi: 10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leskinen T, Sipilä S, Alen M, Cheng S, Pietiläinen KH, Usenius JP, et al. Leisure-time physical activity and high-risk fat: A longitudinal population-based twin study. Int J Obes (Lond) 2009;33:1211–1218. doi: 10.1038/ijo.2009.170. [DOI] [PubMed] [Google Scholar]
- 12.May AM, Bueno-de-Mesquita HB, Boshuizen H, Spijkerman AM, Peeters PH, Verschuren WM. Effect of change in physical activity on body fatness over a 10-y period in the Doetinchem Cohort Study. Am J Clin Nutr. 2010;92:491–499. doi: 10.3945/ajcn.2010.29404. [DOI] [PubMed] [Google Scholar]
- 13.Ross R, Janssen I, Dawson J, Kungl AM, Kuk JL, Wong SL, et al. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res. 2004;12:789–798. doi: 10.1038/oby.2004.95. [DOI] [PubMed] [Google Scholar]
- 14.Eriksson MK, Franks PW, Eliasson M. A 3-year randomized trial of lifestyle intervention for cardiovascular risk reduction in the primary care setting: The Swedish Björknas Study. PLoS One. 2009;4:e5195. doi: 10.1371/journal.pone.0005195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ross R, Bradshaw AJ. The future of obesity reduction: Beyond weight loss. Nat Rev Endocrinol. 2009;5:319–325. doi: 10.1038/nrendo.2009.78. [DOI] [PubMed] [Google Scholar]
- 16.Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willet W, et al. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am J Clin Nutr. 2003;78:719–727. doi: 10.1093/ajcn/78.4.719. [DOI] [PubMed] [Google Scholar]
- 17.Sternfeld B, Wang H, Quesenberry CP, Jr, Abrams B, Everson-Rose SA, Greendale GA, et al. Physical activity and changes in weight and waist circumference in midlife women: Findings from the Study of Women’s Health Across the Nation. Am J Epidemiol. 2004;160:912–922. doi: 10.1093/aje/kwh299. [DOI] [PubMed] [Google Scholar]
- 18.Davidson LE, Tucker L, Peterson T. Physical activity changes predict abdominal fat change in midlife women. J Phys Act Health. 2010;7:316–322. doi: 10.1123/jpah.7.3.316. [DOI] [PubMed] [Google Scholar]
- 19.Sheehan TJ, DuBrava S, DeChello LM, Fang Z. Rates of weight change for black and white americans over a twenty year period. Int J Obes Relat Metab Disord. 2003;27:498–504. doi: 10.1038/sj.ijo.0802263. [DOI] [PubMed] [Google Scholar]
- 20.Droyvold WB, Nilsen TI, Kruger O, Holmen TL, Krokstad S, Midthjell K, et al. Change in height, weight and body mass index: Longitudinal data from the HUNT Study in Norway. Int J Obes (Lond) 2006;30:935–939. doi: 10.1038/sj.ijo.0803178. [DOI] [PubMed] [Google Scholar]
- 21.Schousboe K, Visscher PM, Erbas B, Kyvik KO, Hopper JL, Henriksen JE, et al. Twin study of genetic and environmental influences on adult body size, shape, and composition. Int J Obes Relat Metab Disord. 2004;28:39–48. doi: 10.1038/sj.ijo.0802524. [DOI] [PubMed] [Google Scholar]
- 22.Segal NL, Feng R, McGuire SA, Allison DB, Miller S. Genetic and environmental contributions to body mass index: Comparative analysis of monozygotic twins, dizygotic twins and same-age unrelated siblings. Int J Obes (Lond) 2009;33:37–41. doi: 10.1038/ijo.2008.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stubbe JH, Boomsma DI, Vink JM, Cornes BK, Martin NG, Skytthe A, et al. Genetic influences on exercise participation in 37,051 twin pairs from seven countries. PLoS One. 2006;1:e22. doi: 10.1371/journal.pone.0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borodulin K, Laatikainen T, Juolevi A, Jousilahti P. Thirty-year trends of physical activity in relation to age, calendar time and birth cohort in Finnish adults. Eur J Public Health. 2008;18:339–344. doi: 10.1093/eurpub/ckm092. [DOI] [PubMed] [Google Scholar]
- 25.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 26.Kaprio J. Twin studies in Finland 2006. Twin Res Hum Genet. 2006;9:772–777. doi: 10.1375/183242706779462778. [DOI] [PubMed] [Google Scholar]
- 27.Sarna S, Kaprio J, Sistonen P, Koskenvuo M. Diagnosis of twin zygosity by mailed questionnaire. Hum Hered. 1978;28:241–254. doi: 10.1159/000152964. [DOI] [PubMed] [Google Scholar]
- 28.Kujala UM, Kaprio J, Sarna S, Koskenvuo M. Relationship of leisure-time physical activity and mortality: The Finnish twin cohort. JAMA. 1998;279:440–444. doi: 10.1001/jama.279.6.440. [DOI] [PubMed] [Google Scholar]
- 29.Mustelin L, Silventoinen K, Pietiläinen K, Rissanen A, Kaprio J. Physical activity reduces the influence of genetic effects on BMI and waist circumference: a study in young adult twins. Int J Obesity. 2009;33:29–36. doi: 10.1038/ijo.2008.258. [DOI] [PubMed] [Google Scholar]
- 30.Kujala UM, Kaprio J, Koskenvuo M. Modifiable risk factors as predictors of all-cause mortality: the roles of genetics and childhood environment. Am J Epidemiol. 2002;156:985–993. doi: 10.1093/aje/kwf151. [DOI] [PubMed] [Google Scholar]
- 31.Latvala A, Dick DM, Tuulio-Henriksson A, Suvisaari J, Viken RJ, Rose RJ, et al. Genetic correlation and gene-environment interaction between alcohol problems and educational level in young adulthood. J Stud Alcohol Drugs. 2011;72:210–220. doi: 10.15288/jsad.2011.72.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aarnio M, Kujala UM, Kaprio J. Associations of health-related behaviors, school type and health status to physical activity patterns in 16 year old boys and girls. Scand J Soc Med. 1997;25:156–167. doi: 10.1177/140349489702500303. [DOI] [PubMed] [Google Scholar]
- 33.Rintala M, Lyytikainen A, Leskinen T, Alen M, Pietiläinen KH, Kaprio J, et al. Leisure-time physical activity and nutrition: A twin study. Public Health Nutr. 2011;14:846–852. doi: 10.1017/S136898001000090X. [DOI] [PubMed] [Google Scholar]
- 34.Jacobs EJ, Newton CC, Wang Y, Patel AV, McCullough ML, Campbell PT, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170:1293–1301. doi: 10.1001/archinternmed.2010.201. [DOI] [PubMed] [Google Scholar]
- 35.Rexrode KM, Carey VJ, Hennekens CH, Walters EE, Colditz GA, Stampfer MJ, et al. Abdominal adiposity and coronary heart disease in women. JAMA. 1998;280:1843–1848. doi: 10.1001/jama.280.21.1843. [DOI] [PubMed] [Google Scholar]
- 36.Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–384. doi: 10.1093/ajcn/79.3.379. [DOI] [PubMed] [Google Scholar]
- 37.Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr. 2005;81:555–563. doi: 10.1093/ajcn/81.3.555. [DOI] [PubMed] [Google Scholar]
- 38.Peltonen N, Harald K, Männistö S, Saarikoski L, Peltomäki P, Lund L, et al. The National FINRISK 2007 Study. B34. Publications of the National Public Health Institute; Helsinki: 2008. [Google Scholar]