Abstract
Objective
To examine the contributions of frequency, consistency, and comprehensiveness of dietary self-monitoring to long-term weight change.
Design and Methods
Participants included 220 obese women (mean±SD, age=59.3±6.1 years; BMI=36.8±4.9 kg/m2) who achieved a mean loss of -10.39±5.28% from baseline during 6 months of behavioral treatment and regained 2.30±7.28% during a 12-month extended-care period. The contributions of cumulative frequency (total number of food records) of self-monitoring, consistency across time (number of weeks with ≥3 records), and comprehensiveness of information recorded were examined as predictors of weight regain in a hierarchical linear regression analysis The mediating role of adherence to daily caloric intake goals was tested using a bootstrapping analysis.
Results
The association between high total frequency of self-monitoring and reduced weight regain was moderated by weekly consistency of self-monitoring, p=.004; increased frequency produced beneficial effects on weight change only when coupled with high consistency (>3 days/week). There was no impact of comprehensiveness on weight change, p>.05. The favorable effect of high frequency/high consistency self-monitoring on weight change was partially mediated by participants’ success in meeting daily caloric intake goals (p< .001).
Conclusion
The combination of high frequency plus high consistency of dietary self-monitoring improves long-term success in weight management.
Keywords: obesity treatment, weight maintenance, behavior modifications, behavioral strategies, dietary adherence
Introduction
Self-monitoring is considered the “cornerstone” of behavioral weight-loss treatment. Written recording of key aspects of dietary intake, physical activity and body weight allows an individual to track progress toward achieving negative energy balance and weight loss and to make adjustments in eating and exercise behaviors as needed.1–3 Further, adherence to self-monitoring mediates the association between intervention provision and weight loss.4,6 Numerous studies have shown that self-monitoring is positively related to weight loss during the initial phase of weight loss treatment;1,7,8 however, few studies have investigated which components (e.g., frequency, consistency, and comprehensiveness) of self-monitoring impact weight loss. Moreover, the impact of these components during the weight maintenance period following weight loss remains unknown.
Boutelle and Kirschenbaum found that individuals lost more weight when they self monitored more frequently (i.e., on a greater number of days) and on weeks where food records were the most complete (i.e., recording “every” vs. “any” of the foods eaten during a day),9 whereas Helsel, Jakicic, and Otto demonstrated that the frequency of recording was more important than the detail of recording in the facilitation of short-term weight loss.10 Research on comprehensiveness of record keeping that accounted for food name, type, time, quantity, and fat grams recorded demonstrated that individuals lost more weight on weeks that they were the most comprehensive compared to weeks when they were the least comprehensive.7 The impact of consistent record keeping (i.e., number of weeks completing a minimum number of records) on initial weight loss, beyond simple frequency over time, has not been investigated.
Less is known about the association of self-monitoring with changes in weight following treatment, especially regarding the relative importance of factors such as frequency, consistency, and comprehensiveness of self-monitoring. Current recommendations are for individuals to continue self-monitoring their behavior following initial lifestyle intervention,11 as sustained dietary self-monitoring has been associated with maintaining weight losses long-term.12 However, the impact of specific components of self-monitoring on maintenance of lost weight is unknown. Given adherence to self-monitoring tends to decline over time,13 it is useful clinically to investigate whether certain facets of self-monitoring are more important to provide specific recommendations for self-monitoring throughout the maintenance period.
Current Study
The current study first aimed to investigate the contributions of frequency, consistency, and comprehensiveness of self-monitoring records on weight change during a 12-month extended-care maintenance period following a six-month weight loss intervention. It was hypothesized that frequency of self-monitoring would be the biggest predictor of maintenance of lost weight. This study also aimed to determine whether the association between self-monitoring and percent weight regain was mediated by meeting daily caloric intake goals. It was hypothesized that meeting daily calorie goals would mediate the relationship between self-monitoring and percent weight regain.
Method and Procedures
Participants
Participants were 234 women living in medically underserved rural counties who took part in the Treatment of Obesity in Underserved Rural Settings (TOURS) trial14 (recruitment, intervention, and assessments conducted June 2003 through May 2008). Participants were 50– 75 years old (mean ± SD age = 59.3 ±6.1 years), with BMIs between 30 and 50 kg/m2 (BMI at baseline = 36.8 ± 4.9 kg/m2). Potential participants were excluded if their medical history, clinical examination, or laboratory results revealed underlying diseases likely to limit five-year life expectancy and/or increase risk of intervention (e.g., history of cardiovascular disease, current or planned pregnancy, musculo-skeletal conditions that limited walking, etc.), or if they experienced weight loss ≥ 4.5 kg in the six months prior to the study. In terms of race and ethnicity, 77.7% of participants self-reported that they identified as Caucasian, 18.2% as African American, 2.3% as Hispanic, and 1.9% as Asian, Native American, or Pacific Islander. Further details on the inclusion/exclusion criteria, recruitment and screening procedures, and attrition have been published previously.14
Measures
Height and Weight
Height was measured without shoes for each participant to the nearest 0.1 cm using a stadiometer. Weight was measured without shoes, in one layer of indoor clothing, to the nearest 0.1 kg using a calibrated and certified balance beam scale. Weights and heights were used to calculate each participant's BMI.
Dietary Self-Monitoring Records
During the extended-care program, participants were provided with paper self-monitoring forms and instructed to complete records at least three days each week (one weekend day and two weekdays), including the type, amount, caloric content, and time of consumption for all foods and drinks consumed. This self-monitoring recommendation was consistent with procedures of the Diet Modification Trial in the Women's Health Initiative study,15 and participants were encouraged to self-monitor more frequently if they found it useful. Participants were asked to return these records to the interventionist in person or by mail (via postage-paid envelopes).
Lifestyle Intervention
Data for the current study were collected as part of a randomized controlled trial approved by the Institutional Review Board of the University of Florida. The TOURS trial consisted of a six-month, group-based lifestyle intervention for obesity followed by one of three 12-month extended-care conditions delivered bimonthly in person, via telephone, or via mail. During the extended-care period, all participants were encouraged to adhere to the reduced calorie, low-fat diet and physical activity recommendations provided within the initial intervention. Participants in the in-person group continued meeting bi-monthly in interventionist-led group-based sessions, while participants in the telephone group had bi-monthly contact with an interventionist via individual telephone calls. Interventionists in both groups used formal problem-solving techniques16 to address barriers to healthy eating/activity experienced by participants. Participants in the mail group received bi-monthly psychoeducational newsletters providing information about nutrition, exercise, problem solving, and healthy lifestyle behaviors to promote weight maintenance. For additional details regarding design and method of the TOURS trial, see Perri et al.14
Statistical Analyses
Data preparation
To assess the effects of frequency, consistency, and comprehensiveness on weight change during the extended-care program (months 7 – 18), the following definitions were used to code and analyze the data:
Frequency
Frequency of food records was defined as the total number of food records that a participant submitted during the extended-care program.
Consistency
Consistency was defined as the number of weeks within the extended-care period in which a participant completed ≥ 3 daily food records per week.
Comprehensiveness
Each food record was coded using the following point system: participants received one point for each of the variables (time, food name, amount, and calories; range 0-4 per meal) at breakfast, lunch and dinner. Snacks were excluded from the current analyses, as participants were encouraged to limit snacks outside of structured mealtimes. Comprehensiveness was calculated by dividing actual number of points received by the total possible points a participant could have received and multiplying by 100. Due to the large volume of records, the extended-care program was divided into quartiles and records from the middle month of each quartile (i.e., months 8, 11, 14, and 17) were coded for comprehensiveness by the first author (NDP). Comprehensiveness scores from this 16-week subset of data were averaged and used to calculate a total comprehensiveness score for each participant. The fourth author (KEM) re-coded a randomly selected subset of these records; inter-rater reliability was calculated from agreement between these scores and the scores by NDP.
Meeting caloric intake goals
Participants were asked to report their daily calorie goal (established by the group interventionist) and the number of days each week that they met this goal.
Analyses
An ANOVA was used to assess whether there were differences between participants who returned at the end of the TOURS trial (and thus were included in the current analyses) and those who did not. The primary aim assessing the impact of each self-monitoring component of self-monitoring on weight change during months 7-18 was analyzed using a hierarchical linear regression. The previously established impact of extended-care condition (i.e., in-person, telephone, or mail) on percent weight regain during months 7 through 1814 led us to include this variable in the model first as covariate. TOURS trial results demonstrated that participants randomized to the treatment conditions delivered in-person and via telephone experienced similar weight regain;14 therefore, we collapsed these two conditions and compared them to the mail-only condition. Total frequency of self-monitoring was entered next, as previous research has most strongly associated this factor with weight loss and maintenance. Weekly consistency and comprehensiveness variables were entered into the model in step three and four, respectively, to assess their impact above and beyond total frequency. Finally, interactions between variables were investigated.
For the second aim, bootstrapping17 was conducted to assess the indirect effect of meeting daily caloric intake goals on the association of self-monitoring and percent weight regain. Two thousand bootstrapping estimations were used to build an empirical approximation of the sampling distribution of ab (indirect effect), and this sampling distribution was subsequently used to construct a confidence interval for the indirect effect. Percent weight change was entered as the dependent variable, components of self-monitoring were entered as the predictor variables, and percent adherence to daily caloric intake goals was entered as a proposed mediator. Data were analyzed in PASW Statistics v.18.018 and SAS® v. 9.3.19
Results
The 220 women who returned for assessment at the end of the TOURS trial were not significantly different than those who did not return (n = 14) with respect to baseline weight, p = .353, or body weight changes from baseline to month 6, p = .772. An ANOVA revealed group differences between the completers and non-completers for total frequency of self-monitoring, F (1, 233) = 8.88, p = .003, such that women who did not complete the study submitted significantly fewer food records than women who completed the study. A significant difference was also found for weekly consistency of self-monitoring, F (1, 233) = 9.60, p = .002; women who did not complete the study submitted food records less consistently than women who completed the study. Finally, a marginally significant difference was found for completers and non-completers for comprehensiveness of self-monitoring, F (1, 233) = 3.48, p = .063, such that women who completed the study were more comprehensive in their record keeping compared to non-completers.
Due to these differences, we completed the following analyses two ways: both within an intent-to-treat paradigm using multiple imputation (n=234), and using completers only (n=220). The pattern of results from both sets of analyses was identical; thus, for ease of reporting interactions we present the completers-only analysis.
Preliminary analyses
The average total frequency, weekly consistency, and comprehensiveness of self-monitoring records over time is represented in Table 1. During months 7 through 18 of the study, 23 women (10.5%) did not submit any food records, 89 women (40.5%) submitted records for 1-25% of the days, 61 women (27.7%) submitted records for 26-50% of the days, 20 women (9.1%) of the sample submitted records for 51-75% of the days, and 27 women (12.3%) submitted records for 76-100% of the days. The number of participants who submitted food records decreased over time, from 195 participants during month 7 to 91 participants during month 18. Frequency of self-monitoring decreased from month 7 to month 18, such that the mean (±SD) number of records submitted per week decreased from 3.62 ± 0.15 at month 7 to 1.46 ± 0.15 at month 18, t(219) = 13.76, p < .001.
Table 1.
| Variable | Month 7-9 | Months 10-12 | Months 13-15 | Months 16-18 | ||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| Frequency (# of records) | 13.78 | 8.76 | 9.71 | 9.24 | 7.58 | 8.87 | 6.77 | 8.90 |
| Consistency (# of weeks ≥ 3 records) | 2.64 | 1.38 | 1.92 | 1.67 | 1.50 | 1.62 | 1.30 | 1.64 |
| Comprehensiveness* (% completed) | 86.21 | 13.40 | 84.42 | 15.39 | 85.05 | 15.51 | 83.73 | 18.22 |
comprehensiveness was assessed only at month 8, 11, 14, and 17
In terms of weekly consistency, 101 women (45.9%) were consistent at least 50% of the extended-care period, while 119 women (54.1%) were consistent less than 50% of the time. The percentage of participants who self-monitored consistently at least three days per week decreased from 70.7% ± 4.7 at month 7 to 29.8% ± 1.5 at month 18. Further, the mean (±SD) number of weeks per month in which participants submitted three or more records decreased from 2.83 ± 1.36 at month 7 to 1.19 ± 1.69 at month 18, t(219) =-13.34, p < .001.
The average comprehensiveness score of records that contained self-monitoring information was 84.0% ± 15.03 (range = 29.4% to 100%) during the extended-care year; for participants who did not turn in records, it was assumed that records were not completed (i.e., comprehensiveness of 0%). There was a small non-significant decline in comprehensiveness of self-monitoring over time (see Table 1). During months 7 - 18, 100% of records specified the food/drink name, 98.4% included the calories in each food, and 97.6% calculated total calories for the day, 81.8% noted amount of food/drink consumed, and 68.3% of records identified time of consumption. The intra-class correlation for agreement between raters was α = .997.
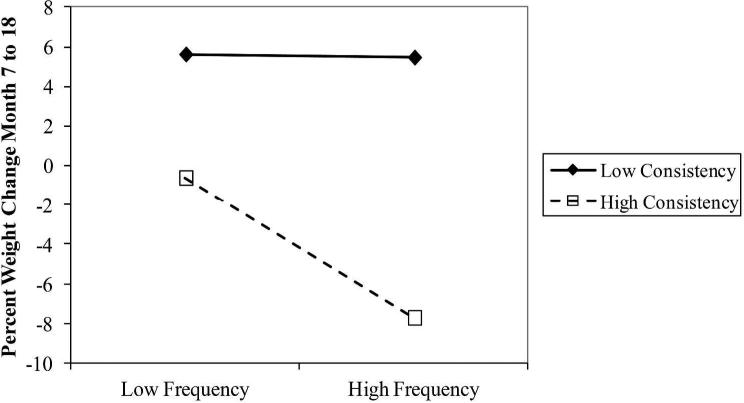
The impact of frequency, consistency, and comprehensiveness on weight change
From baseline to month 6, participants experienced a mean (±SD) weight change of -10.39 ± 5.28%. During the extended-care period (months 7 - 18), participants experienced a mean weight change of 2.30 ± 7.28%. Table 2 provides the regression coefficients and model effects for the final model. After entering extended-care condition, total frequency, weekly consistency, comprehensiveness, and interactions between these factors were entered into the model, comprehensiveness and interactions between comprehensiveness and other model factors were removed from the model due to poor fit (regression coefficient ps >.05). A three way interaction between Phase 2 assignment, frequency, and consistency was not significant, p > .05, and was removed from the model. There was a significant interaction observed between consistency and frequency, p = .004 (Table 2), such that increased frequency of self-monitoring had little impact for individuals who were not as consistent with their self-monitoring, but resulted in less weight regain in participants who self-monitored consistently (see Figure 1). Further, results demonstrated that the women who self-monitored consistently (50% or more of the extended-care year) lost weight ( -.98 ± 6.67%), while less consistent participants gained weight (5.1 ± 6.59%), t(218) = 6.78, p < .001.
Table 2.
| % Weight Change | R2 | F | df | β | t | P |
|---|---|---|---|---|---|---|
| Block 1 | .044 | 10.06 | 1,218 | |||
| Extended-Care Condition | −3.22 | −3.172 | 0.002 | |||
| Block 2 | .210 | 28.77 | 2,217 | |||
| Extended-Care Condition | −1.87 | −1.973 | .050 | |||
| Frequency | −0.03 | −6.74 | < .0001 | |||
| Block 3 | .212 | 19.38 | 3,216 | |||
| Extended-Care Condition | −1.79 | −1.881 | .061 | |||
| Frequency | −0.02 | −2.216 | .028 | |||
| Consistency | −0.05 | −0.83 | .407 | |||
| Block 4 | .242 | 17.15 | 4,215 | |||
| Extended-Care Condition | −2.21 | −2.337 | .020 | |||
| Frequency | 0.01 | 0.326 | .745 | |||
| Consistency | −0.16 | −2.328 | .021 | |||
| FrequencyxConsistency | 0.00 | −2.905 | .004 |
Figure 1.
The impact of frequency and consistency on weight percent weight regain from month 7 to month 18.
Mediation by achievement of daily caloric intake goal
The total effect of the interaction between total frequency and weekly consistency of self-monitoring on percent weight change (total effect = -.0014, p < .001) decreased, but remained significant, when the percent adherence to daily caloric intake goals was included in the model as a mediator (direct effect of the interaction term = -.0001, t(219) = -2.12, p = .035). The total indirect effect (i.e., the difference between the total and direct effects) of the frequency by consistency interaction on weight change through adherence to caloric intake goals was significant, z = -4.3475, p < .0001, with a point estimate of -.0007 and a 95% bias-corrected and accelerated20 bootstrap confidence interval of -.0012 to -.0004. Thus, adherence to daily caloric intake goals partially mediated the moderation of frequency of self-monitoring by consistency and percent weight change.
Discussion
The current study investigated the patterns of frequency, consistency, and comprehensiveness of self-monitoring records and their contributions to weight change during a one-year extended-care period following initial lifestyle intervention. Findings demonstrate reductions in adherence to self-monitoring throughout the extended-care period; both total frequency and weekly consistency decreased from month 7 to 18. This pattern is in line with previous findings demonstrating that self-monitoring of eating and exercise behaviors and other adherence factors (e.g., attendance, adherence to fat gram goals and exercise goals) decline as the intervention intensity is reduced.13,21
Although the number of participants who submitted food records decreased over time, the mean scores for comprehensiveness of food records submitted remained fairly stable. Thus, the women who continued to submit food records remained fairly comprehensive with their self-monitoring. As comprehensiveness declined, it is possible that overall self-monitoring declined or ceased.
Participants who self-monitored both frequently and consistently maintained their weight changes more effectively compared to participants who failed to monitor as often or as consistently. Moreover, while individuals who were consistent (i.e., ≥ 3 records per week) at least 50% of the extended-care period lost a small amount of weight, those who were not consistent at least 50% of this time regained about 5% from their month 6 assessment weight. Results also revealed that comprehensiveness did not provide any added benefit above and beyond the variance explained by total frequency, weekly consistency, and the interaction between frequency and consistency. While this finding differs from the results of two previous studies that found an impact of comprehensiveness on initial weight loss,7,9 it provides additional support that frequency of recording was more important than the detail of recording in the facilitation of short-term weight loss in adults.10 The impact of the interaction between frequency and consistency was partially mediated by adherence to caloric intake goals. Thus, consistent and frequent self-monitoring appears to facilitate the maintenance of lost weight by helping participants to adhere to daily caloric intake goals.22
Limitations and Strengths
The current study has several limitations. Given that the TOURS trial included only women aged 50-75 living in rural areas,14 results may not be generalizable to men, younger adults, or persons living in non-rural areas. Further, 14 participants failed to return at the final 18-month assessment visit and were excluded from analysis; however, the main regression model was run with multiply imputed data and the pattern of results was identical. Finally, this study did not prospectively randomize participants to differing frequencies/consistencies of self-monitoring per week. Thus, increased frequency in the context of high consistency may not lead to better results alone, but may be related to another factor, such as treatment engagement or motivation.
The current study also exhibits important strengths. While the association between frequency of self-monitoring and weight loss has been well established and at least two studies have demonstrated that comprehensiveness of self-monitoring records may be important for initial weight loss,7,9 to our knowledge no studies have investigated the impact of consistency of self-monitoring on weight loss. Additionally, we are aware of no studies that have investigated how frequency, consistency, and comprehensiveness impact weight change during an extended-care period following initial weight loss. This study is the first to demonstrate that total frequency of self-monitoring during this time may only be important in the context of weekly consistency.
Clinical Significance and Future Directions
The current study supports the clinical recommendation11 of continued self-monitoring for maintenance of lost weight. Specifically, encouraging individuals to frequently and consistently self-monitor, even if this means sacrificing completeness (e.g., the “something is better than nothing” approach), appears to be particularly important. Consistent and frequent self-monitoring appears to facilitate weight maintenance by helping participants adhere to daily caloric intake goals. Self-regulatory theorists, including Kirschenbaum and others23,24 have suggested that a certain preoccupation or “healthy obsession” with target weight control behaviors (e.g., self-monitoring and close scrutiny of one's food intake) can be adaptive. Therefore, for participants already highly committed to self-monitoring frequently and consistently, continuing to nurture the mindset that this self-regulatory behavior is critical to their weight control efforts may improve overall self-monitoring adherence and maintenance of lost weight.
These results also support a continual-care model in which obesity is characterized as a chronic disorder that requires long-term treatment.25,26 Long-term continued care necessitates the identification of the key components of treatment to reduce overall patient burden. For patients experiencing difficulty maintaining self-monitoring behaviors, encouragement to maintain frequent and consistent records without focusing on comprehensive logging of details may be warranted to promote adherence to both self-monitoring and daily caloric intake goals. Recent technological advances may assist in this realm. The availability of electronic calorie records accessed via the Internet or smartphone apps may increase ease and reduce time required for self-monitoring. Results from studies investigating electronic record keeping compared to traditional pen-and-paper methods have been mixed;1 however, a recent randomized trial of two personal digital assistant (PDA) diary-based interventions compared to a traditional paper diary condition demonstrated superior adherence for the PDA records.27 Research with time/date stamped self-monitoring records has demonstrated that many participants do not adhere to instructions for record completion and some may falsify the time and date of diary entries.13 Thus, future studies are needed to assess the impact of frequency, consistency, and completeness of electronic self-monitoring records on weight loss and maintenance.
Summary and Conclusions
Results of the present study revealed that during the year following lifestyle treatment, higher total frequency of self-monitoring was significantly associated with lower percent weight change within individuals who self-monitored consistently, but had little impact on weight change for those who did not self-monitor consistently. This association was partially mediated by adherence to daily caloric intake goals. There was no effect for comprehensiveness beyond the impact of frequency and consistency. Thus, encouraging consistent and frequent self-monitoring of dietary intake past the initial weight loss period may serve as a beneficial strategy for reducing the weight regain commonly observed during the maintenance period. These findings can be utilized to improve the long-term management of obesity in adults seeking lifestyle intervention.
What is already known about this subject:
Dietary self-monitoring is a key component associated with weight loss during behavioral treatment of obesity.
Current recommendations encourage individuals to continue self-monitoring their dietary intake following initial lifestyle intervention, but there is limited knowledge regarding the impact of frequency, consistency, and comprehensiveness of self-monitoring on maintenance of lost weight.
What this study adds:
Increased frequency of self-monitoring, when coupled with high consistency, produced beneficial effects on weight change during the extended-care period.
Comprehensiveness of dietary self-monitoring had no impact on weight change during the weight maintenance period.
Meeting daily caloric intake goals partially mediated the impact of frequency and consistency on weight change.
Acknowledgements
NDP and MGP designed the study. NDP and VAM were involved in data collection. NPD coded self-monitoring data; KEM re-coded a subset of this data to assess inter-rater agreement. NDP and KRM analyzed the data. NDP, KRM, LMN, KEM, VAM, and MGP were involved in writing the paper and had final approval of the submitted and published versions. This research was supported by grant R18HL73326 from the National Heart, Lung, and Blood Institute.
Footnotes
Conflicts of Interest Statement
The authors declare no conflicts of interest.
References
- 1.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: A systematic review of they literature. J Am Diet Assoc. 2011;111:92–102. doi: 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanfer FH. Self-monitoring: Methodological limitations and clinical applications. J Consult Clin Psychol. 1970;35:148–152. [Google Scholar]
- 3.Wadden TA, Osei S. The treatment of obesity: An overview. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. Guilford Press; New York: 2002. pp. 229–248. [Google Scholar]
- 4.Wang J, Sereika SM, Chasens ER, Ewing LJ, Matthews JT, Burke LE. Effect of adherence to self-monitoring of diet and physical activity on weight loss in a technology-supported behavioral intervention. Patient Prefer Adherence. 2012;6:221–226. doi: 10.2147/PPA.S28889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and its relationship to adherence to self-monitoring and weight loss in a 16-week internet behavioral weight loss intervention. J Nutr Educ Behav. 2010;42:161–167. doi: 10.1016/j.jneb.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Turk MW, Elci OU, Wang J, et al. Self-monitoring as a mediator of weight loss in the SMART randomized clinical trial. Int J Behav Med. 2012;20:556–561. doi: 10.1007/s12529-012-9259-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behav Ther. 1993;24:377–394. [Google Scholar]
- 8.Streit KJ, Stevens NH, Stevens VJ, Rossner J. Food records: a predictor and modifier of weight change in a long-term weight loss program. J Am Diet Assoc. 1991;91:213–216. [PubMed] [Google Scholar]
- 9.Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obes Res. 1998;6:219–224. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- 10.Helsel DL, Jakicic JM, Otto AD. Comparison of techniques for self-monitoring eating and exercise behaviors on weight loss in a correspondence-based intervention. J Am Diet Assoc. 2007;107:1807–1810. doi: 10.1016/j.jada.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 11.Jensen MD, Ryan DH, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults. Obesity. 2013 epub ahead of print. [Google Scholar]
- 12.McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? J Consult Clin Psychol. 1999;67:177–185. doi: 10.1037//0022-006x.67.2.177. [DOI] [PubMed] [Google Scholar]
- 13.Burke LE, Sereika SM, Music E, Warziski M, Styn MA, Stone A. Using instrumented paper diaries to document self-monitoring patterns in weight loss. Contemp Clin Trials. 2008;29:182–193. doi: 10.1016/j.cct.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perri MG, Limacher MC, Durning PE, et al. Extended-care programs for weight management in rural communities: The Treatment of Obesity in Underserved Rural Settings (TOURS) randomized trial. Arch Intern Med. 2008;168:2347–2354. doi: 10.1001/archinte.168.21.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tinker LF, Burrows ER, Henry H, Patterson R, Rupp J, Van Horn L. The Women's Health Initiative: overview of the nutrition components. In: Krummel D, Kris-Etherton P, editors. Nutrition in Women's Health. Aspen; Gaithersburg, MD: 1996. pp. 510–542. [Google Scholar]
- 16.D'Zurilla TJ, Nezu AM. Problem-solving therapy: A social competence approach to clinical intervention. 2nd edn. Springer; New York: 1999. [Google Scholar]
- 17.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 18.SPSS Inc. PASW Statistics for Windows, Version 18.0. SPSS Inc.; Chicago: 2009. [Google Scholar]
- 19.SAS Institute Inc. SAS Version 9.3. SAS Institute Inc.; Cary, NC: 2011. [Google Scholar]
- 20.Efron B. Better bootstrap confidence intervals. J Am Stat Assoc. 1987;82:171–185. [Google Scholar]
- 21.Acharya SD, Elci OU, Sereika SM, Music E, Styn MA, Turk MW, et al. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient Prefer Adherence. 2009;3:151–160. doi: 10.2147/ppa.s5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sperduto WA, Thompson HS, O'Brein RM. The effect of target behavior monitoring on weight loss and completion rate in a behavior modification program for weight reduction. Addict Behav. 1986;11:337–340. doi: 10.1016/0306-4603(86)90060-2. [DOI] [PubMed] [Google Scholar]
- 23.Kirschenbaum DS. Weight-loss camps in the U.S. and the immersion-to-lifestyle change model. Childhood Obesity. 2010;6:318–323. [Google Scholar]
- 24.Geirut KJ, Pecora KM, Kirschenbaum DS. Highly successful weight control by formerly obese adolescents: A qualitative test of the Healthy Obsession Model. Childhood Obesity. 2012;8:455–465. doi: 10.1089/chi.2012.0101. [DOI] [PubMed] [Google Scholar]
- 25.Boutelle KN, Kirschenbaum DS, Baker RC, Ellen M. How can obese weight controllers minimize weight gain during the high risk holiday season? By self-monitoring very consistently. Health Psycho. 1999;18:364–368. doi: 10.1037//0278-6133.18.4.364. [DOI] [PubMed] [Google Scholar]
- 26.Latner JD, Stunkard AJ, Wilson GT, Jackson ML, Zelitch DS, Labouvie E. Effective long-term treatment of obesity: a continuing care model. Int J Obes Relat Metab Disord. 2000;24:893–898. doi: 10.1038/sj.ijo.0801249. [DOI] [PubMed] [Google Scholar]
- 27.Burke LE, Conry MB, Sereika SM, et al. The effect of electronic self-monitoring on weight loss and dietary intake: A randomized behavioral weight loss trial. Obesity. 2011;19:338–344. doi: 10.1038/oby.2010.208. [DOI] [PMC free article] [PubMed] [Google Scholar]