Abstract
Bladder carcinoma is the most frequent tumor of the urinary tract and accounts 7% of all malignancies in men and 2% of all malignancies in women. This retrospective study was carried out to assess the diagnostic utility of F18-fludeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) in the imaging evaluation of bladder carcinoma. Seventy-seven consecutive patients diagnosed to have carcinoma urinary bladder referred for F18-FDG PET/CT were included in this study. Thirty-four patients were for initial staging after transurethral biopsy and remaining 43 patients were for restaging. All patients also underwent CT scan of the abdomen and pelvis. PET/CT findings were correlated with diagnostic CT scan and histopathological findings. In 30 of the 34 patients for initial staging, both PET/CT and CT confirmed the primary lesion in the bladder. Histopathology report was available in 23 patients. Lymph nodes FDG uptake reported to be metastatic in 10/23 patients while CT detected lymph node metastasis in 12 patients. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy have been calculated to be 87.5%, 80%, 70%, 92%, 82% for PET/CT and 66%, 57%, 50%, 72%, 60% for CT respectively. PET/CT detected metastatic disease in 8 patients whereas CT detected in 4 patients. Of the 43 patients for restaging, local recurrence was detected in 24 patients on both PET/CT and CT. Histopathology report was available in 17 patients. Sensitivity, specificity, PPV, NPV and accuracy were 85%, 60%, 60%, 85%, 70% for PET/CT and 80%, 50%, 40%, 85%, 58% for CT respectively. Nineteen patients were detected to have metastatic disease by PET/CT, whereas CT detected metastases in 11 patients. F-18 FDG PET/CT is a very useful modality in pre-operative staging and monitoring after surgery, chemotherapy or radiotherapy of patients with carcinoma urinary bladder.
Keywords: Bladder carcinoma, fludeoxyglucose positron emission tomography/computed tomography, restaging, staging
Introduction
Urinary bladder carcinoma represents second most common malignancy of the genitourinary tract and constitutes 7% of all malignancies in men and 2% of all malignancies in women.[1] Transitional cell carcinoma (TCC) is the most common tumor histology. Approximately 70% of TCCs present as a superficial lesion while 10-20% of these progress to muscle invasive lesion. Nearly 20-25% of newly diagnosed bladder cancers are muscle invasive and 5-10% are metastatic at initial presentation.[2] Urine cytology and cystoscopy with biopsy are the mainstay of diagnostic modalities. Conventional imaging evaluation includes ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI). However, CT and MRI are not reliable in evaluating the extent of local or regional disease.[3,4] CT and MRI encounter difficulties because tumor involvement is not necessarily reflected by changes in shape or texture of an affected lymph node (LN). Lymph nodes not exceeding 1 cm in diameter are difficult to detect and the importance of these small LNs on CT or MRI is uncertain. Furthermore, the presence of enlarged regional LNs does not always indicate metastasis; rather, such nodes may be reactive. Nearly 50% of the high-grade tumors may have occult metastatic disease at initial diagnosis and gross metastases within 2 years of diagnosis despite prompt treatment.[3] CT and MRI have accuracies as low as 55% and 60%, respectively.[4,5,6] Novel imaging methods are needed to detect occult metastatic disease. Prognosis depends upon the depth of tumor penetration into the bladder wall, with 5-year survival of 85% for superficial disease and 55% for invasive disease. Metastatic disease is associated with very poor prognosis.[7] Treatment depends on the disease stage. For low-grade, superficial tumors treatment of the lesion is complete endoscopic resection with or without additional intravesical chemotherapy. For non-metastatic invasive bladder cancer the standard treatment is radical cystectomy with urinary diversion.[8,9] Treatment of metastatic disease includes chemotherapy and palliative radiation therapy. Fludeoxyglucose (FDG) positron emission tomography (PET) is a molecular imaging technique that assesses regional glucose metabolism. It is widely used because most cancers exhibit increased glucose utilization compared with normal tissues.[10] Metabolic changes detectable by PET precede morphologic changes detectable by anatomic imaging methods, leading to greater sensitivity of PET. Combined PET/CT provides spatially co-registered functional and anatomic images, resulting in increased sensitivity and specificity by comparison with PET alone for many different tumor types.[11]
Preliminary assessment of FDG PET in patients with bladder cancer revealed that FDG PET could detect distant metastatic lesions and was useful in differentiating viable recurrent tumor from radiation-induced alterations.[12] However, detection of the primary bladder tumor was difficult due to intense accumulation of excreted FDG in urine. Interventions such as bladder irrigation, forced diuresis with furosemide, or both, may contribute significantly to overcome this problem.[13] This study was performed to evaluate the diagnostic utility of FDG PET/CT in the imaging evaluation of patients with primary and metastatic bladder carcinoma.
Materials and Methods
Patient population
Seventy-seven consecutive patients (72 male; 5 female) of histopathologically confirmed carcinoma urinary bladder (high grade TCC in 50 patients, low grade in 23, adenocarcinoma in 2 and 1 each of Squamous cell carcinoma and sarcomatoid carcinoma) subjected to F-18 FDG PET/CT from April 2009 to June 2011 were included in this study. Average age of the patients was 60 years (age range 30-88 years). All patients had been previously submitted to transurethral biopsy or primary tumor resection or cystectomy.
Patients were analyzed in 2 groups: One group included the patients for initial staging after transurethral biopsy (34 patients) and another group of 43 patients for restaging (after 3 times transurethral resection 21, chemotherapy 5, radiotherapy 3, radical cystectomy 5, combined chemotherapy and radiotherapy 6 and combined radical cystectomy, chemotherapy and radiotherapy 3 patients respectively). All patients underwent conventional staging procedures including CT scan of the abdomen and pelvis. PET/CT findings were correlated with diagnostic CT scan and histopathological findings.
PET/CT protocol
Patients were instructed to fast for at least 6 h prior to PET investigation. An intravenous injection of 370-555 MBq (10-15 mCi) of 18F-FDG was given. Blood glucose was measured before injection of the tracer to ensure glucose blood levels below 150 mg/dL.
PET/CT images were acquired from the base of the skull to the mid-thighs 60 min after the intravenous injection of F18-FDG using dedicated PET/CT scanner present (Discovery STE-16, GE Healthcare, Milwaukee, U.S.A). Breath holding CT transmission images were acquired (140 kVp, 80 mA, Pitch: 1.375, slice thickness: 1.25 mm) after administration of intravenous and oral contrast. The PET emission scan was obtained in 3-D mode from the mid-thigh and ending at the base of the skull in 5-8 bed positions with an acquisition time of 2 min for each bed position, immediately after acquisition of the CT scan. An additional single bed position acquisition was also acquired for the head if there was suspicion of brain metastases. In 63 patients delayed pelvic image was acquired 1 h after the intravenous injection of furosemide (40 mg), oral hydration and repeated bladder evacuation. The data was reconstructed by iterative reconstruction with CT-derived attenuation correction using the ordered subsets expectation maximization algorithm. PET, CT and fused PET/CT images were displayed on Advantage workstation (GE Healthcare).
Data analysis
All PET/CT images were interpreted by two experienced nuclear medicine physicians. Focal accumulation of FDG above background (liver, non-working muscle) was considered as a positive finding. In addition to qualitative evaluation of the images, the maximum standardized uptake values (SUVmax) were also recorded for selected lesions, using software provided by the vendor. The combined metabolic information of PET and structural information of CT were used for image interpretation. Discordant metabolic-structural findings were further analyzed. Available correlative imaging studies at the time of PET/CT interpretation included contrast-enhanced CT studies of the abdomen and pelvis in all patients and bone scintigraphy in 18 patients. All these studies were obtained within 3 months of the PET scans. Confirmation of the findings was done by histopathology in 40 patients and by follow-up PET/CT scan in 10 patients. A lesion was considered true positive (TP) on imaging if the same lesion was confirmed on histology, false positive (FP) on imaging when histology was negative, false negative (FN) if histology of lesion revealed malignant involvement with no positive imaging findings and true negative when both imaging and histology were negative. Sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) of both PET/CT and CT were calculated.
Results
In Group I (patients investigated for initial staging, n = 34), both PET/CT and CT detected primary lesion in the bladder in 30 patients. FDG uptake (SUVmax) in primary lesions varied from 5.7-30.4. Final histopathology report was available in 23/34 patient.
Of the 23 patients with available histopathological data, PET/CT detected local LNs involvement in 10/23 patients (local nodes in 2 patients, iliac nodes in 4 patients, extra pelvic in 1 patient, local, iliac and extrapelvic in 1 patient and iliac and extrapelvic in 2 patients). PET/CT was TP in 7/10 patients, FP in 3/10, true negative in 12/13 patients and FN in 1/13 patients. CT detected LN metastasis in 12 patients (TP - 6/12 and FP - 6/12. Eight patients were true negative and 3 were FN. PET/CT upstaged one patient and down staged 4 patients compared with CT. However, this modality misdiagnosed 4 patients [Figure 1]. Sensitivity, specificity, PPV, NPV and accuracy for PET/CT have been calculated to be 87.5%, 80%, 70%, 92%, 82% and for CT 66%, 57%, 50%, 72%, 60% respectively.
Figure 1.
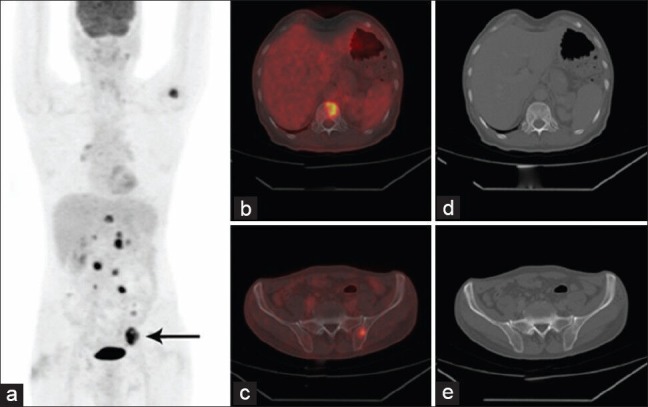
F-18 fludeoxyglucose (FDG) Whole body positron emission tomography/computed tomography image of a patient referred for staging of the urinary bladder carcinoma (a) Maximum intensity projection image showing intense FDG uptake in left external iliac lymph nodes (arrow) along with other lesion, axial fused images showing intense FDG avid foci in the vertebra (b) and left ilium (c) respectively while the corresponding axial CT images (d and e) show no definite changes
PET/CT detected single or multiple metastases in 8 patients (local spread in 3, lungs in 4, liver in 2 and bone in 2 patients respectively) whereas CT detected metastatic disease in 4 patients. Bone scan done in 7 was found to be negative for skeletal metastases in all patients. In 4 patients both PET/CT and CT were normal, two of them did not develop any abnormality on follow-up.
Amongst the 43 Group II patients for restaging, both PET/CT and CT were found to be positive in 24 patients and negative in 19 patients. The FDG uptake (SUVmax) in this group varied from 5.2 to 30.8. Histopathology report was available in 17 patients. PET/CT detected local LNs in 10 patients (local nodes in 1 patient, iliac nodes in patient, extrapelvic nodes in 3 patients, local, iliac and extra pelvic nodes in 3 patient and iliac and extrapelvic in remaining 2 patients). The FDG uptake (SUVmax) in LN metastases this group varied from 3.5 to 13.5. Lymph nodes metastatic involvement on PET/CT was TP in 6/10 patients, FP in 4/10, TN in 6/7 and FN in 1/7 patients respectively. CT was TP in 4, FP in 6, TN in 6 and FN in 1 patient respectively. Sensitivity, specificity, PPV, NPV and accuracy for PET/CT was 85%, 60%, 60%, 85%, 70% and for CT was 80%, 50%, 40%, 85%, 58% respectively.
PET/CT also detected single or multiple metastases in 19 patients (local spread 11, lungs 7, liver 4, muscle 5, adrenal 2, kidney 2, brain 2 and bone 10 patients respectively) whereas CT detected metastatic disease in 11 patients. Bone scan was done in 18 patients was found to be positive in 8 patients. Extensive metastases were found in multiple organs so histopathological confirmation was not done in 11 patients. Of these 11 patients, 7 patients showed PET e/o metabolic response after chemotherapy in follow-up scans proving metastatic nature of the disease. Remaining 4 patient's a progressive disease was proven by other imaging modality. In one patient suspected metastasis to colon on imaging was later confirmed to be due to collagenous colitis.
Forced diuresis coupled with oral hydration showed marked reduction of urinary tract activity to near-background level in 49 out of 63 bladder preserved patients [Figure 2].
Figure 2.
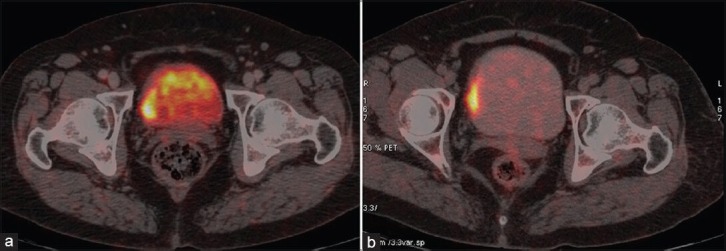
F-18 fludeoxyglucose positron emission tomography/computed tomography fused images of a patient (a) prior to furosemide injection and (b) after furosemide demonstrating better delineation of tumor uptake in the later image
Discussion
Assessment of local disease as well as evaluation of recurrence and distant spread has immense importance in planning the optimal therapy in patients with carcinoma urinary bladder. PET imaging has been effectively used in a variety of cancer for primary staging and restaging of disease after therapy. This retrospective study validated the utility of FDG-PET/CT in initial staging and restaging of bladder carcinoma. CT is the most widely used technique for preoperative node, metastases (NM) staging in bladder carcinoma. The reported accuracy of CT in detecting LN involvement ranges from 70% to 90%, with false-negative rates of 25-40% respectively.[4,9]
Bladder carcinomas are FDG-avid. We have found a SUVmax in the range of 5.7-30.4 for the primary tumor and 3.5-13.8 in LN metastases. In an earlier rat bladder tumor model, a high tumor-to-blood FDG uptake ratio of 22 was noted.[14] In our study, regarding primary tumor detection both PET/CT and CT are equally good and detected 88% tumors which were proved histopathologically. Underestimation of tumor spread by CT can be improved by using PET/CT. PET/CT improved detection of metastatic LN in 5 patients (1 patient upstaged and 4 patients down staged) in initial staging group and 2 patients (upstaged) in restaging group.
Metastatic disease was detected by PET/CT in 8 patients whereas CT detected in 4 patients when the patients were subjected to pre-operative staging (initial staging). In the restaging group 19 patients were found to have metastatic disease by PET/CT but CT was found to positive in 11 patients. The metastatic sites detected by PET/CT in the present study included the liver, kidney, adrenal, mediastinum, lungs, brain and bone. Rare metastatic involvement of skeletal muscle and penile muscle was found in 4 and 2 patients respectively. Local spread to the adjacent structures was found to the ureter in 6 patients, 5 patients in prostate, 2 patients each to the seminal vesicle and rectum. In 7 patients follow-up imaging confirmed metastatic nature, however in other cases follow-up imaging or histopathology report was not found. Overall, in both groups of patients, PET/CT diagnostic information was valuable in detecting, localizing and characterizing the extent of metastatic disease.
Among the additional imaging modalities bone scan was negative for 7 patients but PET/CT detected metastases in 2 other patients in initial staging group. In restaging group 18 patients underwent bone scan and was positive in 8 patients whereas PET/CT detected bony lesions in 10 patients. PET/CT positivity of more lesions represents early marrow deposits of metastatic tumor. Incorporation of metabolic information in the diagnostic imaging assessment can affect clinical management significantly. In this study, the complementary information provided by the PET/CT affected the clinical management in 5 patients in initial staging group and 6 patients in the restaging group by altering the management strategy between curative or palliative options.
FDG undergoes glomerular filtration similar to glucose, but it is not reabsorbed through the tubules and it is largely excreted in the urine, producing high activity in the urinary tract.[15] Hence, a major limitation of the use of FDG-PET for staging an abdominal malignancy is the urinary elimination and the non-specific and variable intestinal uptake of the radiotracer, which may mimic focal hyper metabolism and thus lead to a false-positive diagnosis. Delayed imaging after forced diuresis using furosemide and repeated micturition improves lesion detection by reducing the urinary activity. In our study, beneficial effect was found in 49 (77%) out of 63 bladder preserved patients. This finding is in keeping with the improved accuracy of FDG PET imaging in abdomino-pelvic malignancies when it was combined with forced diuresis documented by Kamel et al.[13] Correlation of morphological images from CT data with PET data from combined PET/CT studies increases the diagnostic utility.
Compared with CT improvements is seen in PET/CT, with respect to sensitivity (initial staging group 66% vs. 87%; restaging group 80% vs. 85%) specificity (initial staging group 57% vs. 80%; restaging group 50% vs. 60%), PPV (initial staging group 50% vs. 70%; restaging group 40% vs. 60%), NPV (initial staging group 72% vs. 92%; restaging group 85% vs. 85%) and accuracy (initial staging group 60% vs. 82%; restaging group 58% vs. 70%). From a clinical point of view, if PET shows a hypermetabolic nodular lesion and CT does not indicate the reasons for false positivity of PET (e.g., urinary stasis in ureter, invasion of the ureter by the primary tumor, bladder diverticulum), the high positive likelihood of malignant LN involvement seems to justify a PET-induced change in the therapeutic strategy. In this situation, PET/CT improves the diagnostic accuracy. Seven of the 40 patients found to have FP LN on PET/CT may be due to reactive changes following recent biopsy.
Other studies used different tracers apart from FDG. In a study by Letocha et al. investigated whether PET with L-methyl-11C-methionine as a tracer could be used for the evaluation of therapy response in 44 patients with varying stages of the urinary bladder TCC treated with chemotherapy.[16] In that study PET was poor diagnostic accuracy and the technique could not monitor the therapeutic effect of chemotherapy. Better result was found with C-11 choline, which is not excreted into urine, overcoming a significant limitation of FDG.[17,18] However, role of non FDG PET tracers in the imaging evaluation of patients with bladder carcinoma is yet to be fully established.
Study limitations
Being a retrospective study there may be evaluation bias. Moreover, clinical information and follow-up data of all the patients could not be retrieved. Histopathology report was found only in 40 patients and follow-up imaging data was available in 10 patients. Metastatic lesions were not confirmed histopathologically. It was not sure that the particular LNs showing FDG PET/CT positivity actually harbors metastatic disease. Histological findings were found as LN group not as an individual node.
Conclusion
Our findings add to the current literature, suggesting that FDG PET/CT scanning may contribute significantly to the imaging evaluation of patients with carcinoma urinary bladder compared with CT both in pre-operative and restaging settings especially in detection of lymph nodal and distant metastatic disease. More prospective data is required on a larger series of patients to determine the exact diagnostic performance, impact of FDG PET/CT and its cost-effectiveness in patients with carcinoma urinary bladder.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, et al. Cancer statistics, 2005. CA Cancer J Clin. 2005;55:10–30. doi: 10.3322/canjclin.55.1.10. [DOI] [PubMed] [Google Scholar]
- 2.Messeing EM. Urothelial tumour of bladder. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walse Urology. 9th ed. Philadelphia: Saunders Elsevier; 2007. pp. 2407–46. [Google Scholar]
- 3.Droller MJ. Bladder cancer: State-of-the-art care. CA Cancer J Clin. 1998;48:269–84. doi: 10.3322/canjclin.48.5.269. [DOI] [PubMed] [Google Scholar]
- 4.Paik ML, Scolieri MJ, Brown SL, Spirnak JP, Resnick MI. Limitations of computerized tomography in staging invasive bladder cancer before radical cystectomy. J Urol. 2000;163:1693–6. [PubMed] [Google Scholar]
- 5.Lantz EJ, Hattery RR. Diagnostic imaging of urothelial cancer. Urol Clin North Am. 1984;11:567–83. [PubMed] [Google Scholar]
- 6.Buy JN, Moss AA, Guinet C, Ghossain MA, Malbec L, Arrive L, et al. MR staging of bladder carcinoma: Correlation with pathologic findings. Radiology. 1988;169:695–700. doi: 10.1148/radiology.169.3.3186994. [DOI] [PubMed] [Google Scholar]
- 7.Frank IN, Graham S, Jr, Nabors WL. Urologic and male genital cancers. In: Holleb AI, Fink DJ, Murphy GP, editors. Clinical Oncology. Atlanta: American Cancer Society; 1991. pp. 272–4. [Google Scholar]
- 8.Greenlee RT, Murray T, Bolden S, Wingo PA. Cancer statistics, 2000. CA Cancer J Clin. 2000;50:7–33. doi: 10.3322/canjclin.50.1.7. [DOI] [PubMed] [Google Scholar]
- 9.Herr HW. Uncertainty, stage and outcome of invasive bladder cancer. J Urol. 1994;152:401–2. doi: 10.1016/s0022-5347(17)32748-9. [DOI] [PubMed] [Google Scholar]
- 10.Kelloff GJ, Hoffman JM, Johnson B, Scher HI, Siegel BA, Cheng EY, et al. Progress and promise of FDG-PET imaging for cancer patient management and oncologic drug development. Clin Cancer Res. 2005;11:2785–808. doi: 10.1158/1078-0432.CCR-04-2626. [DOI] [PubMed] [Google Scholar]
- 11.von Schulthess GK, Steinert HC, Hany TF. Integrated PET/CT: Current applications and future directions. Radiology. 2006;238:405–22. doi: 10.1148/radiol.2382041977. [DOI] [PubMed] [Google Scholar]
- 12.Kosuda S, Kison PV, Greenough R, Grossman HB, Wahl RL. Preliminary assessment of fluorine-18 fluorodeoxyglucose positron emission tomography in patients with bladder cancer. Eur J Nucl Med. 1997;24:615–20. doi: 10.1007/BF00841398. [DOI] [PubMed] [Google Scholar]
- 13.Kamel EM, Jichlinski P, Prior JO, Meuwly JY, Delaloye JF, Vaucher L, et al. Forced diuresis improves the diagnostic accuracy of 18F-FDG PET in abdominopelvic malignancies. J Nucl Med. 2006;47:1803–7. [PubMed] [Google Scholar]
- 14.Harney JV, Wahl RL, Liebert M, Kuhl DE, Hutchins GD, Wedemeyer G, et al. Uptake of 2-deoxy, 2-(18F) fluoro-D-glucose in bladder cancer: Animal localization and initial patient positron emission tomography. J Urol. 1991;145:279–83. doi: 10.1016/s0022-5347(17)38314-3. [DOI] [PubMed] [Google Scholar]
- 15.Gallagher BM, Fowler JS, Gutterson NI, MacGregor RR, Wan CN, Wolf AP. Metabolic trapping as a principle of oradiopharmaceutical design: Some factors resposible for the biodistribution of [18F] 2-deoxy-2-fluoro-D-glucose. J Nucl Med. 1978;19:1154–61. [PubMed] [Google Scholar]
- 16.Letocha H, Ahlström H, Malmström PU, Westlin JE, Fasth KJ, Nilsson S. Positron emission tomography with L-methyl-11C-methionine in the monitoring of therapy response in muscle-invasive transitional cell carcinoma of the urinary bladder. Br J Urol. 1994;74:767–74. doi: 10.1111/j.1464-410x.1994.tb07123.x. [DOI] [PubMed] [Google Scholar]
- 17.de Jong IJ, Pruim J, Elsinga PH, Jongen MM, Mensink HJ, Vaalburg W. Visualisation of bladder cancer using (11) C-choline PET: First clinical experience. Eur J Nucl Med Mol Imaging. 2002;29:1283–8. doi: 10.1007/s00259-002-0881-7. [DOI] [PubMed] [Google Scholar]
- 18.Yoshida S, Nakagomi K, Goto S, Futatsubashi M, Torizuka T. C-choline positron emission tomography in bladder cancer: Report of four cases. Int J Urol. 2006;13:829–31. doi: 10.1111/j.1442-2042.2006.01416.x. [DOI] [PubMed] [Google Scholar]


