Abstract
Introduction
Condom-associated erection problems (CAEP) are reported by a substantial number of young men and are associated with inconsistent and/or incomplete condom use. The underlying mechanisms of CAEP are not well understood and research examining the possibility that men who report CAEP differ from other men in their sexual responsivity is lacking.
Aim
This study used psychophysiological methods to examine whether men who report CAEP have a higher threshold for sexual arousal, a stronger need for tactile stimulation, and/or more easily lose their sexual arousal due to neutral distractors or performance-related demands.
Methods
A total of 142 young, heterosexual men (53% reporting CAEP) were presented with four 3-minute erotic film clips. Three film clips were combined with one of the following manipulations: 1) distraction, 2) performance demand, or 3) vibrotactile stimulation. One erotic film clip was presented with no further instructions or manipulations.
Main Outcome Measures
Average penile circumference changes during the first, second, and third minute (Time) of the erotic film stimuli (Condition) were submitted to a mixed-model ANOVA with Condition and Time as within-subjects factors and Group (CAEP/No-CAEP) as between-subjects factor.
Results
Significant main effects of Condition and Time and a significant interaction of Group×Time were found. No significant interactions involving Condition were found. Men who reported CAEP had smaller erectile responses during the first minute, regardless of film condition, than men who reported no CAEP (F(1,141)=8.64, p<.005).
Conclusion
The findings suggest that men with and without CAEP differ in the ease with which they become sexually aroused. Men reporting CAEP needed more time and/or more intense stimulation to become aroused. To our knowledge, this study is the first to use psychophysiological methods to assess sexual responsivity in men who report CAEP.
Keywords: Condom-associated erection problems, condoms for penile vaginal intercourse, sexual arousal, condoms, psychophysiology
Introduction
A growing number of studies indicate that condom use problems and errors are common, even among self-identified “consistent condom users” [1–7]. One of the problems associated with condom use that is increasingly receiving research attention involves the loss of arousal and erection during and/or after condom application. An early study found that loss of erection during condom application or condom use was commonly mentioned by men attending STI clinics [8]. Following this research, Warner et al. found that 12% of young adult men in their sample reported loss of erection either before or after the condom was put on their penis [6]. A review of the literature from 1995 to 2011 examined studies reporting on CAEP during application separately from CAEP occurring during intercourse [9]. Prevalence estimates of problems with erection during condom application ranged from 14.3% to 28.1% of participants reporting on condom use. CAEP during intercourse was reported by 9.9% to 20.2% of participants [9].
The loss of erection during and/or after condom application is associated with inconsistent and incomplete use of male condoms, and therefore it is a cause of concern from a public health perspective [9, 10]. For example, Graham and colleagues found that 37% of young men attending a public STI clinic reported at least one of these types of CAEP, and these problems were associated with significantly higher frequencies of unprotected vaginal intercourse and lower rates of consistent condom use [4]. Men with erection loss also were more likely to report removing condoms before intercourse was over, more problems with ‘fit or feel’ of condoms, and lower self-efficacy to use condoms correctly.
Even though the phenomenon of CAEP is now well-documented, the underlying mechanisms are not well understood [9]. Although interpersonal (e.g., communication), intrapersonal (e.g., condom application skills), and situational (e.g., drug or alcohol use) factors may all contribute to CAEP, the current study focused on the possibility that men who experience CAEP differ from other men in their sexual responsivity. More specifically, the current study, using psychophysiological methods, explored whether men who report CAEP have a higher threshold for sexual arousal, a stronger need for tactile stimulation, and/or more easily lose their sexual arousal due to external distractors or performance-related demands or concerns.
Psychophysiological studies have convincingly shown that attention is vital to acquiring and maintaining high levels of sexual arousal [11, 12]. Distracting participants from sexual stimuli (e.g., having participants perform competing tasks; [13]) is one of the most effective ways to reduce sexual arousal. Sources of distraction, however, can also be related to sexual activity itself, for example when one is pre-occupied with or worries about one’s sexual performance.
In the current study, the relevance of distraction and performance pressure was evaluated by comparing men who do and those who do not experience CAEP in their sensitivity to sexually ‘neutral’ distractors (i.e., solving simple arithmetic equations) or with sexual performance-related distractions (e.g., due to feeling pressured to obtain or maintain an erection). In addition, the study examined whether men who experience CAEP have a higher threshold for sexual arousal and/or a stronger need for sexual stimulation, by comparing men who experience CAEP with men who do not report CAEP in their responses to erotic film clips with content that varied in intensity, by increasing the explicitness of the depicted behaviors over time (e.g., petting and manual stimulation of the genitals, oral sex, and penile-vaginal intercourse). We also explored whether men who report CAEP have a stronger need for tactile stimulation by including a condition in which sexual film was combined with vibration applied to the penis. The current study focused on young men who are not in a long-term relationship because 1) these men tend to be at higher risk for acquiring and transmitting STDs/HIV and 2) CAEP in long(er) term relationships may involve additional or other causes (e.g., ones more intrinsic to the relationship).
Aims
The current study aimed to answer the following questions: Do men with CAEP, as compared to men without CAEP, 1) more easily lose erections due to external distractors and performance-related concerns?; 2) have a stronger need for tactile stimulation?; and 3) have a higher threshold for sexual arousal?
Methods
Participants
A total of 142 heterosexual men participated in this study. Participants were recruited through the use of flyers and newspaper and online advertisements (e.g., Facebook, Craigslist, online university forums) and from an associated questionnaire study [14]. Eligibility criteria included self-identifying as heterosexual, being 18–29 years of age, not being in a committed relationship, and having used condoms for penile-vaginal intercourse within the past 90 days. Men were excluded if they were participating in a safe sex or condom use program, if they were in treatment for sexual problems, or if they experienced erectile problems at a clinical level (as established using the IIEF, see below). Additionally, men were excluded if they had been in a sexually exclusive (monogamous) relationship for at least one month. For the purposes of this study, men reporting condom-associated erection problems were oversampled using targeted advertising. The study reported in this paper was part of a larger project, involving additional sessions and procedures, the findings of which will be presented elsewhere. All participants provided informed consent and received $50 for their participation. All study protocols and procedures were approved by the university’s Institutional Review Board.
Questionnaires
Participants were asked to complete an online questionnaire consisting of demographic questions and questions about general and sexual health, sexual orientation, relationship status, as well as frequency of various types of sexual activity. In addition, participants completed the International Index of Erectile Function (IIEF [15]) and a modified version of the Condom Use Errors/Problems Survey (CUES, [16]).
The International Index of Erectile Function (IIEF) is a widely used measure of male sexual function, which assesses erectile function, orgasmic function, sexual desire, intercourse satisfaction and overall sexual satisfaction. Men who scored at the clinical level in terms of erectile functioning (scores below 26; [15]) were excluded.
As part of the Condom Use Errors/Problems Survey (CUES), two types of condom-associated erection problems were assessed: CAEP occurring during application of the condom (CAEP-Application) and CAEP occurring during penile-vaginal intercourse while using a condom (CAEP-PVI). CAEP-Application was assessed by the question: “How often over the past 90 days did you lose or start to lose your erection while putting the condom on before vaginal intercourse?” CAEP-PVI was assessed by the question: “In the past 90 days, how often did you lose or start to lose your erection while wearing a condom during vaginal intercourse?” Response options for both questions were: never, occasionally, less than half the time, most of the time, always. CAEP was coded as “yes” when men answered at least “occasionally” to one or both of the two questions.
Genital response
Genital responses were monitored using a RigiScan device (Timm Medical Technologies; for a discussion of its validity and reliability, see [17]). The RigiScan device has two tension loops. The current study included the measurement of penile sensitivity as well of erections during condom application (the findings of which will be reported elsewhere) and for this reason only one loop was used, placed on the base of the penis1. Participants, who were tested individually, put the RigiScan in place themselves, in private. During the study, a problem with the Rigiscan was discovered, and although this problem was fixed by the manufacturer, it may have affected the rigidity readings of a subset of participants. As penile circumference readings were not affected by this problem, erectile response will be reported in terms of penile circumference change. New disposable loops were used for each participant.
Stimuli and tasks
Film stimuli
Participants were presented with a series of four erotic film clips. One was combined with distraction, one with performance demand, and one with vibration. The fourth video was presented without additional stimuli or manipulations. All excerpts were taken from commercially available films, were 3 minutes in duration, and depicted heterosexual petting (e.g., kissing, manual stimulation of genitals, 1st minute), oral sex (2nd minute), and penile-vaginal intercourse (3rd minute). Prior to the first erotic film presentation, participants were presented with a 15-minute neutral film clip to determine baseline levels. Also, neutral film excerpts (from nature documentaries about marine life) were used for 3-minute return-to-baseline intervals between erotic stimuli [cf., 18]).
Vibrotactile stimulation
One of the erotic video conditions was combined with vibrotactile stimulation. Vibrotactile stimulation was administered by means of a commercially available ring-shaped vibrator, with a frequency of approximately 50Hz [19].
Neutral distraction
A second erotic video clip was combined with neutral distraction. For this purpose, arithmetic (e.g., basic addition, subtractions, multiplications, and divisions) were displayed for 10 seconds in a corner of the screen. Participants were asked to solve the equation while continuing to watch the film, and to write down the answer on an answer sheet [19].
Performance demand
A third erotic film excerpt was associated with performance demand. Participants were asked, through instructions that were presented on the monitor, to try and obtain an erection as quickly as possible during the following film presentation [13, 20].
To ensure that possible differences in responding between groups or conditions would not in some way be caused by the order of presentation of the films and manipulations, the order of the film, film and distraction, and film and performance demand conditions were randomized. For this purpose, participants within each of the two groups (CAEP, non-CAEP) were randomly assigned to one of three orders. The combined film and vibrotactile stimulation condition was always presented after this series of three conditions.
Main Outcome Measures
Erectile responses were calculated using the difference between mean penile circumferences recorded during the first, second, and third minutes of the sexual stimuli minus the average circumference recorded during the last minute of the first neutral film and subjected to a mixed-model ANOVA using IBM SPSS Statistics 20 for Mac OS X. The Greenhouse-Geisser epsilon procedure was applied to correct for the violation of the sphericity assumption [21].
Results
Sample Characteristics
The mean age of the participants was 20.8 years (SD=1.9). The majority were White (72%), with 9% of the participants being Asian, 5% African American/Black, and the remainder having selected other races. Hispanic ethnicity was reported by 3% of the men. The mean number of times the participants had had penile vaginal intercourse in the 90-day recall period was 16.7 (SD = 22.6). The mean number of times men used condoms during the same period was 11.5 (SD = 17.5). The majority (61.2%) had more than one female sex partner in the past 90 days.
The oversampling of men with condom-associated erection problems (CAEP) was successful: A total of 53% of the participants reported CAEP during application and/or CAEP during PVI. Comparisons between the no-CAEP group and the CAEP group revealed no differences in age (no-CAEP: M=20.6, CAEP: M=21.0, p>.2). The groups significantly differed in IIEF scores for erectile function. Men reporting no CAEP (M=29.4) had higher erectile function scores compared to the men reporting CAEP (M=27.5), t(106)= 5.72, p<.001. However, IIEF erectile function scores of both groups were well within the “no dysfunction” range (scores between 25–30).
Erectile Responses
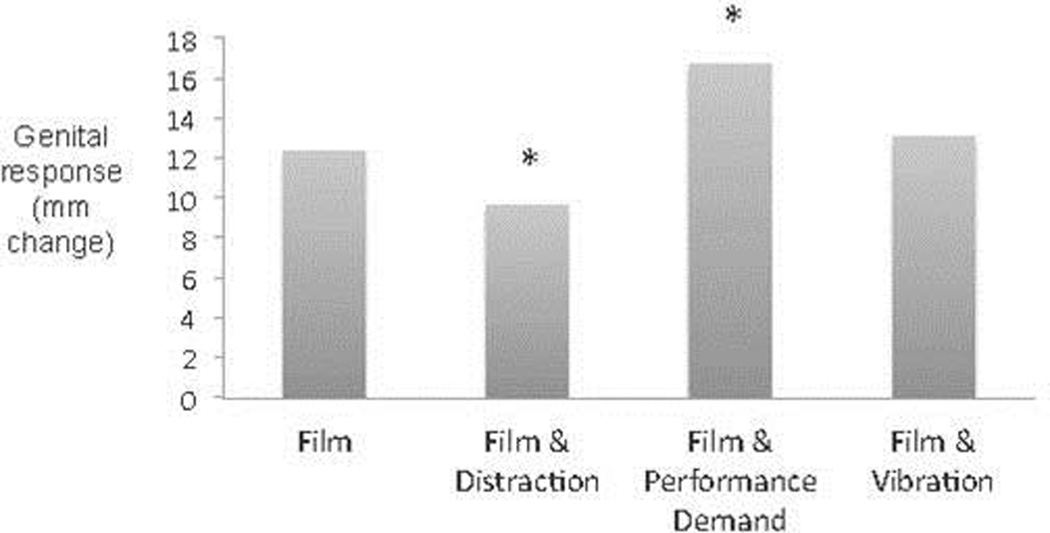
A mixed-model ANOVA with Condition (4: Film, Film & Distraction, Film & Performance Demand, Film & Vibration) and Time (3: First minute, Second Minute, Third Minute) as within-subjects factors and Group (2: CAEP, No-CAEP) as between-subjects factor revealed significant main effects of Condition (F(3,282)=28.67, p<.001) and Time (F(2,282)=361.45, p<.001). Follow-up tests on the effect of Time revealed that genital responses increased over time during the sexual film presentations (Minute 1: Mean = 5.5 mm, Minute 2: Mean = 15.3 mm, Minute 3: Mean = 18.0 mm). Follow-up tests on the effect of Condition revealed that responses to Film & Distraction were significantly smaller than responses to all other conditions (ps<.001, see Figure 1). In addition, Film & Performance Demand resulted in significantly larger responses than all other conditions (all ps<.001). Responses to Film and Film & Vibration did not differ significantly from each other.
Figure 1.
Erectile responses (in mm change from baseline) to four erotic film conditions. *Significantly different (p<.001) from the three other conditions.
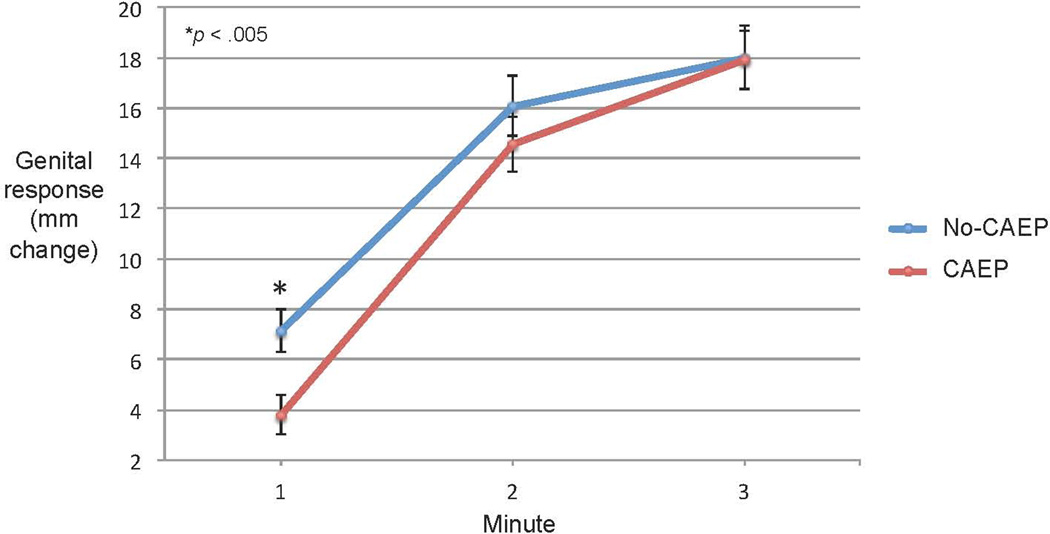
In addition to the two main effects, a significant interaction of Group × Time (F(2,282)=5.63, p<.02) was found. Follow-up tests showed that the CAEP group had significantly smaller erectile responses during the first minute of the film presentations than no-CAEP group (F(1,141)=8.64, p<.005, see Figure 2). No significant differences were found for the second and third minute.
Figure 2.
Erectile responses (in mm change from baseline) during the first, second, and third minute of film conditions (CAEP = Condom-Associated Erectile Problems).
Conclusion
To our knowledge, the present study is the first to compare, using psychophysiological methods, erectile responses of men who do and do not report condom-associated erection problems (CAEP). The primary goal of the study was to examine whether men who report CAEP have a higher threshold for sexual arousal, a stronger need for tactile stimulation, and/or more easily lose their sexual arousal due to external distractors or performance-related concerns. The findings indicate that men reporting CAEP were not more sensitive to experimentally manipulated distraction or performance demand than men not reporting CAEP. Also, the findings suggest that they do not necessarily have a stronger need for tactile stimulation (as responses to vibration were not different between groups). However, the results clearly suggest that men who do and do not report CAEP differ in the ease with which they become sexually aroused, with men reporting CAEP needing more time, or stronger stimulation, to become aroused. At this point it is unclear whether it is the duration or the intensity (or nature) of the presented sexual stimuli that contributed most to the difference, as the first minute of all film clips depicted petting and foreplay (e.g., manual stimulation of the genitals), not more intense forms of sexual stimulation (e.g., oral sex, intercourse). Thus, the findings suggest that men reporting CAEP may need longer stimulation, stronger stimulation, or a combination of the two, in order to become sexually aroused.
Although the experimental manipulations did not lead to any group differences in responses during the sexually-neutral distraction or performance-related conditions, the possibility should be considered that distraction or performance-related processes do contribute to the experience of CAEP, but only in the presence of a sexual partner or within the context of distractions that are more relevant to sex (e.g., condom application, concerns of sexual performance). It is possible that the arithmetic tasks used for the distraction condition do not sufficiently mimic the distraction of condom application. This interpretation is consistent with findings reported by Sanders et al., which indicate that a scale measuring condom distraction/worry (i.e., worrying that condoms will interfere with erections/arousal and/or finding condoms distracting) was significantly associated with CAEP during condom application and with CAEP during intercourse while using a condom [14].
Some other limitations of this study should be acknowledged. The study sample was limited to heterosexual men who were not in a stable relationship. Future studies could expand this work by examining CAEP in homosexual and bisexual men and men who are in a committed relationship. Also, our findings were based on penile circumference, not rigidity. However, the aim of the study was to compare men who do with men who do not report CAEP in their sensitivity to distraction, performance pressure, and other variables, and therefore a focus on response patterns (instead of levels) seems justified. Penile circumference and rigidity are partly independent, neurophysiologically, but they are strongly correlated. For example, one study found a correlation of r=. 87 between circumference and rigidity at the base of the penis [22]. Furthermore, future studies could examine whether men who report CAEP, although by definition being about erection loss, experience lower subjective sexual arousal.
The findings of this study contribute to our basic understanding of situational, or context-specific (in this case, associated with condom use), erectile problems in non-clinical samples of young men. In addition, our findings suggest some clear avenues for intervention for men who experience CAEP. Interventions, particularly condom-focused STI/HIV prevention programs, could address the fact that late condom application, early removal, or more generally, inconsistent use of condoms is more likely when men are worrying about or experiencing arousal or erection loss. More specifically, intervention programs should incorporate a stronger focus on educating men who report CAEP to take more time to become aroused and/or receive the stimulation that is most likely to help them obtain and maintain an erection, especially when using condoms.
Acknowledgments
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number R21 HD060447, E. Janssen and S.A. Sanders (PIs). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Penile responses as measured at the base of the penis are the most commonly analyzed and reported in studies using the RigiScan.
References
- 1.Crosby RA, Sanders SA, Yarber WL, Graham CA, Dodge B. Condom use errors and problems among college men. Sex Transm Dis. 2002;29:552–557. doi: 10.1097/00007435-200209000-00010. (2002). [DOI] [PubMed] [Google Scholar]
- 2.Fishbein M, Pequegnat W. Evaluating AIDS prevention interventions using behavioral and biological outcome measures. Sexually transmitted diseases. 2000;27(2):101–110. doi: 10.1097/00007435-200002000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Graham CA, Crosby RA, Sanders SA, Yarber WL. Assessment of condom use in men and women. Annual review of sex research. 2005;16(1):20–52. [PubMed] [Google Scholar]
- 4.Graham CA, Crosby RA, Yarber WL, Sanders SA, McBride KR, Milhausen RR, Arno JN. Erection loss in association with condom use among young men attending a public STI clinic: Potential correlates and implications for risk behaviour. Sexual Health. 2006;3(4):255–260. doi: 10.1071/sh06026. [DOI] [PubMed] [Google Scholar]
- 5.Sanders SA, Graham CA, Yarber WL, Crosby RA. Condom use errors and problems among young women who put condoms on their male partners. J Am Med Womens Assoc. 2003;58:95–98. [PubMed] [Google Scholar]
- 6.Warner L, Clay-Warner J, Boles J, Williamson J. Assessing condom use practices: implications for evalutating method and user effectiveness. Sex Transm Dis. 1998;25(6):273–277. doi: 10.1097/00007435-199807000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Yarber WL, Graham CA, Sanders SA, Crosby RA. Correlates of condom breakage and slippage among university undergraduates. Int J STD AIDS. 2004;15:467–472. doi: 10.1258/0956462041211207. [DOI] [PubMed] [Google Scholar]
- 8.Richters J, Hendry O, Kippax S. When safe sex isn’t safe. Cult Health Sex. 2003;5:37–52. [Google Scholar]
- 9.Sanders SA, Yarber WL, Kaufman EL, Crosby RA, Graham CA, Milhausen RR. Condom use errors and problems: a global view. Sex Health. 2012;9:81–95. doi: 10.1071/SH11095. [DOI] [PubMed] [Google Scholar]
- 10.Adam BD, Husbands W, Murray J, Maxwell J. AIDS Optimism, condom fatigue, or self-esteem? Explaining unsafe sex among gay and bisexual men. J Sex Res. 2005;42:2238–2248. doi: 10.1080/00224490509552278. [DOI] [PubMed] [Google Scholar]
- 11.Barlow DH. Causes of sexual dysfunction: the role of anxiety and cognitive interference. J Cons Clin Psych. 1986;54(2):140. doi: 10.1037//0022-006x.54.2.140. [DOI] [PubMed] [Google Scholar]
- 12.Janssen E. Sexual arousal in men: A review and conceptual analysis. Hormones Beh. 2011;59:708–716. doi: 10.1016/j.yhbeh.2011.03.004. (2011). [DOI] [PubMed] [Google Scholar]
- 13.Janssen E. Psychophysiological measures of sexual response. In: Wiederman MW, Whitley BE, editors. Handbook for conducting research on human sexuality. Mahwah, NJ: Erlbaum; 2002. pp. 139–171. [Google Scholar]
- 14.Sanders SA, Hill BJ, Crosby RA, Janssen E. Correlates of condom-associated erection problems in young, heterosexual men: Condom fit, self-efficacy, perceptions, and motivations. AIDS Behav. 2013;ePrint:1–7. doi: 10.1007/s10461-013-0422-3. (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 16.Crosby RA, Graham CA, Milhausen RR, Sanders SA, Yarber WL. Correct condom use self-efficacy scale. In: Fisher TD, Davis CM, Yarber WL, Davis SL, editors. Handbook of sexuality-related measures. London: Routledge; 2010. pp. 160–161. [Google Scholar]
- 17.Janssen E, Prause N, Greer J. The sexual response. In: Cacioppo JT, Tassinary LG, Berntson GG, editors. Handbook of psychophysiology. New York: Cambridge University Press; 2007. pp. 245–266. [Google Scholar]
- 18.Janssen E, Goodrich D, Petrocelli J, Bancroft J. Psychophysiological response patterns and risky sexual behavior in heterosexual and homosexual men. Arch Sex Behav. 2009;38:538–550. doi: 10.1007/s10508-008-9432-z. [DOI] [PubMed] [Google Scholar]
- 19.Janssen E, Everaerd W, van Lunsen RH, Oerlemans S. Visual stimulation facilitates penile responses to vibration in men with and without erectile disorder. J Consult Clin Psychol. 1994;62:1222–1228. doi: 10.1037//0022-006x.62.6.1222. [DOI] [PubMed] [Google Scholar]
- 20.Heiman JR, Rowland DL. Affective and physiological sexual response patterns: the effects of instructions on sexually functional and dysfunctional men. J Psychosom Res. 1983;27(2):105–116. doi: 10.1016/0022-3999(83)90086-7. [DOI] [PubMed] [Google Scholar]
- 21.Vasey MW, Thayer JF. The continuing problem of false positives in repeated measures ANOVA in psychophysiology: A multivariate solution. Psychophysiology. 1987;24:479–486. doi: 10.1111/j.1469-8986.1987.tb00324.x. [DOI] [PubMed] [Google Scholar]
- 22.Levine LA, Carroll RA. Nocturnal penile tumescence and rigidity in men without complaints of erectile dysfunction using a new quantitative analysis software. J Urology. 1994;152:1103–1107. doi: 10.1016/s0022-5347(17)32514-4. [DOI] [PubMed] [Google Scholar]