Abstract
OBJECTIVES:
The overwhelming numbers of twins following assisted reproductive technology (ART) are dichorionic twins, but monochorionic twins account for around 0.9% of post ART pregnancies. The data for post ART-monochorionic pregnancy outcomes are scarce due to the rarity of this condition. Hence, we evaluated the obstetric outcomes of monochorionic and dichorionic pregnancies conceived on ART.
SETTINGS:
University teaching hospital.
STUDY DESIGN:
A case–control study of monochorionic diamniotic (MCDA) and dichorionic diamniotic (DCDA) pregnancies conceived following ART treatment. Charts of all women who conceived following ART from 2008 to 2013 were screened. Among them, the monochorionic twins diagnosed in the first trimester were included and their obstetric outcome was followed-up. For comparison, an equal number of dichorionic twin pregnancies from age and body mass index matched mothers was selected.
RESULTS:
The baseline clinical characteristics were similar between the two groups. MCDA group had a higher miscarriage rate (50%) than the DCDA group (10%), with three seconds trimester miscarriages in the MCDA group. The live birth rates were lower in the MCDA versus DCDA group (40% vs. 90%). Among triplet pregnancies with a monochorionic component, the live birth rate was only 25%.
CONCLUSIONS:
Monochorionic pregnancies following ART have poorer obstetric outcomes when compared to dichorionic pregnancies. For monochorionic pregnancies following ART, intensive antenatal surveillance at a tertiary level obstetric and neonatal center may help optimize the outcome.
KEY WORDS: Assisted reproductive technology, monochorionic twins, obstetric outcome
INTRODUCTION
Multiple pregnancy is one of the important complications following assisted reproductive technology (ART). The incidence of twins among ART pregnancies varies from 21%[1] to 43%.[2] Twin pregnancies are associated with a higher maternal and neonatal morbidity and mortality. These risks are higher in twins born out of ART when compared with twins conceived naturally.[3]
The overwhelming numbers of twins born following ART are dizygotic twins. The incidence of monozygotic twins after natural conception is approximately 0.4%[4] and following ART is around 0.9%.[5] In spontaneous conception, monochorionic twins account for 69% of monozygotic twins.[6,7,8] The true estimate of a monochorionic placentation after monozygotic twinning following ART conception is unknown, but the largest case-series puts it at 95%,[9] which is likely to be an overestimate due to misdiagnosis of dichorionic monozygotic twins as dizygotic twins. The perinatal outcome of monochorionic twins is generally poorer than dichorionic twins due to twin to twin transfusion syndrome[10,11,12] and single fetal demise.[13]
Due to paucity of data regarding pregnancy outcomes in monochorionc twins conceived following ART, we decided to retrospectively evaluate the obstetric outcome of such monochorionic pregnancies in our unit.
MATERIALS AND METHOD
We conducted a case-control study of multiple pregnancies conceived following ART treatment during 2008-2013. This study was done at the reproductive medicine unit of a tertiary care hospital.
The total number of ART conceptions during the study period was 751. The charts of all these women were screened. Among them, the monochorionic twins diagnosed in the first trimester were included in the study. Monochorionicity was diagnosed by transvaginal ultrasound using the following criteria: A single placenta, absence of a chorionic peak (twin peak or lambda sign) and an inter-twin membrane thickness of ≤2 mm.[14]
For comparison, similar numbers of dichorionic twin pregnancies following ART were selected for analysis after matching the mothers for age and body mass index (BMI).
The obstetric outcome of those patients who underwent further antenatal check-ups at our hospital and had been followed-up until delivery, were obtained from our hospital records. Those patients, who had come from other states or countries and returned to their hometown after conceiving, were followed by telephone or E-mail.
Clinical pregnancy was defined as a pregnancy diagnosed by ultrasonographic visualization of one or more gestational sacs and multiple gestational sacs were counted as one clinical pregnancy.[15] Miscarriage was defined as the spontaneous loss of a clinical pregnancy that occurs before 28 completed weeks of gestational age.[16] Preterm birth was defined as a live birth or stillbirth that takes place before 37 completed weeks of gestational age.[15] Live birth was defined as the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of the pregnancy, which, after such separation, breathes or shows any other evidence of life - e.g. beating of the heart, pulsation of the umbilical cord or definite movement of voluntary muscles - whether or not the umbilical cord has been cut or the placenta is attached.[15,17] Discordance was defined with the larger twin as the standard of growth and was calculated by the following equation: (larger weight–smaller weight)/(larger weight)[18] and a value of >20% was taken as discordant twins.[19] Neonatal mortality was defined as death of a live born baby within 28 days of birth[15] and early neonatal mortality was defined as death of a live born baby within 7 days of birth.[15]
Statistical analysis was performed using SPSS software version 17.0 (IBM statistics, New York) using the Chi-square test for categorical data and t-test for numerical data.
RESULTS
The outcome of 10 monochorionic diamniotic (MCDA) pregnancies and 10 age and BMI matched dichorionic diamniotic (DCDA) pregnancies were compared with regards to possible risk factors and outcome analysis.
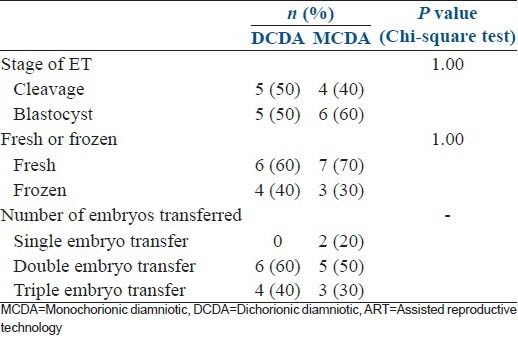
The baseline characteristics of age and BMI (which had been matched), the daily dose of gonadotrophins, total days of stimulation, total dose of gonadotrophins were similar between MCDA and DCDA pregnancies [Table 1]. Other characteristics of the cycle such as the IVF cycle attempt, indication, protocol, day of embryo transfer, stage and day of embryo transfer and number of embryos transferred were also similar between the two groups [Table 2].
Table 1.
Comparison of baseline characteristics between DCDA and MCDA pregnancies
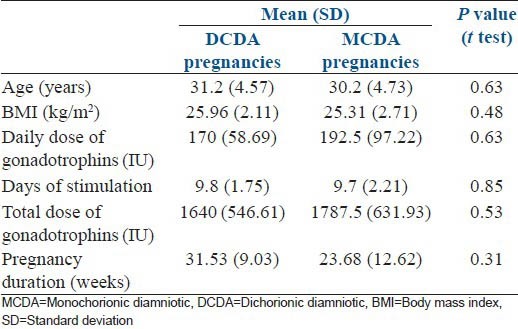
Table 2.
Baseline characteristics of the ART cycles
There were 10 MCDA pregnancies [Figure 1], which had resulted from four fresh cleavage stage transfers, three fresh blastocyst transfers and three frozen blastocyst transfers. Of these 10 MCDA pregnancies, six were twins and four were triplets (which included one MCDA twin component). Two MCDA pregnancies had resulted from a single embryo transfer.
Figure 1.
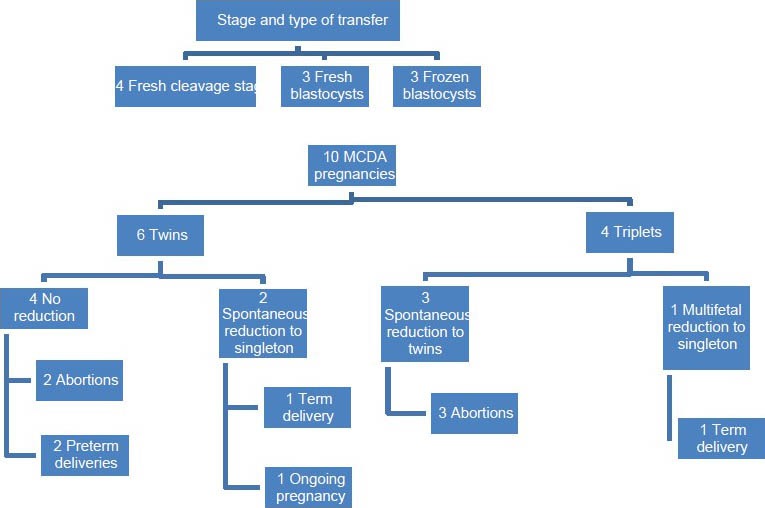
Ten monochorionic diamniotic pregnancies – An overview of the outcomes
During the course of the six twin pregnancies, two had a spontaneous reduction in the first trimester to a singleton pregnancy and four continued as twins. Of the two twins, which had spontaneously reduced to singleton pregnancies, one delivered at term (39 weeks) and the other pregnancy is still ongoing (at 30 weeks of gestation). Of the four twin pregnancies continuing as MCDA twins, there were two miscarriages (at 7 weeks and 23 weeks) and two preterm deliveries. Of the two preterm deliveries, one was a late preterm delivery at 34 weeks 6 days (discordant twins weighing 2860 g and 2220 g) and the other was an early preterm delivery at 28 weeks (discordant twins weighing 1000 g and 600 g). The latter set of preterm twins did not survive and had early neonatal deaths due to extreme prematurity.
The four triplet pregnancies which had a MCDA twin as one of the components were all followed-up to the term. Three pregnancies had a spontaneous reduction to twins in the first trimester; however, all three pregnancies miscarried (at 9 weeks, 17 weeks and 19 weeks respectively). The fourth pregnancy which was continuing as a triplet underwent a multifetal reduction of the monochorionic twin component after appropriate counseling. The pregnancy continued as a singleton pregnancy and successfully ended in a term delivery of a singleton baby at 37 weeks. Hence, among the four triplet pregnancies, only one ended in a live birth, giving a live birth rate of 25% in this group.
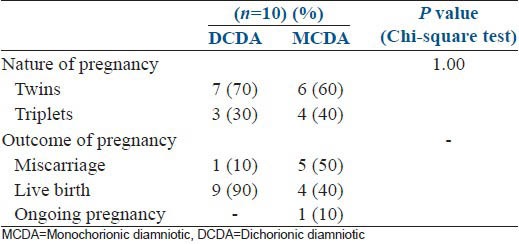
The pregnancy outcomes between the DCDA and MCDA pregnancy groups were compared. The number of twins and triplets were similar between the two groups. There was a 40% miscarriage rate in the MCDA group and a 10% miscarriage rate in the DCDA group; but, the numbers were insufficient for statistical analysis [Table 3].
Table 3.
Comparison of pregnancy outcome
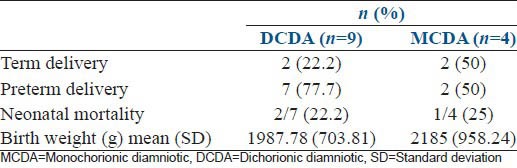
Analysis of the live birth outcome was made for four MCDA pregnancies (after excluding 5 miscarriages and 1 ongoing pregnancy) and nine DCDA pregnancies (excluding 1 miscarriage) and the results are presented in Table 4. There were 2 term and 7 preterm deliveries in the DCDA group and 2 term and 2 preterm deliveries in the MCDA group. There were two neonatal deaths among nine live births in the DCDA group and one neonatal death among four live births in the MCDA group. The mean birth weight in the DCDA group was 1987 g and in the MCDA group was 2185 g.
Table 4.
Comparison of live birth outcomes
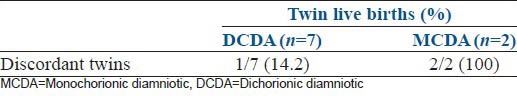
Analysis was done for the presence of discordant twin pairs among the live births [Table 5]. Of the ten MCDA pregnancies, two delivered as twins, both of which were discordant. Of the ten DCDA pregnancies, seven delivered as twins, of which one was a discordant twin.
Table 5.
Outcome of twin deliveries of DCDA and MCDA group
DISCUSSION
In our study, the incidence of monochorionic twins following ART was 1.3% (10/751). Although the multiple pregnancies following ART are mostly dichorionic twins, we specifically evaluated the outcome of monochorionic twins due to its association with a unique set of obstetrical complications.
Monochorionicity is considered more clinically relevant than monozygosity due to the evidence that DCDA monozygous twins have similar outcome as dizygous twins.[20] Placentation (monochorionicity) rather than genetics is the risk factor for the relatively poor outcome of these pregnancies[12,21] Monochorionicity is more easily diagnosed by ultrasound[14] or by a postpartum placental examination.[22] Monozygosity estimation on the other hand required DNA fingerprinting[23] of the same-sex twins or statistical methods such as Weinberg's differential rule[24] from the number of unlike-sex twins.
Monochorionic diamniotic twins occur if the monozygotic splitting occurs between 4th and 8th day after fertilization. Risk factors[5] during ART that have been suggested for monozygotic twinning include age, donor oocyte program, ovarian stimulation protocols, micromanipulation techniques such as ICSI and zona hatching, zona hardening and reduced embryonic integrity due to extended culturing to blastocyst stage in the culture media, which may undergo subtle changes. Regarding age, there are conflicting reports from literature with some studies concluding that age >35 has a higher risk of monozygotic twinning[25,26,27] and others stating that a younger age has a higher risk of monozygotic twinning.[9] In our study, the two groups were matched by age and BMI to remove the confounding effect of these two factors on the outcome. Donor oocyte program confers a two-fold increased risk, but this has been suggested to likely be a confounder due to age.[9] The role of the duration and dose of ovarian stimulation has been variously suggested to have an effect[28] or to have no effect.[29] In our study, there is no significant difference with regards to the duration or dose of ovarian stimulation in predisposing toward MCDA pregnancies. There is some evidence the risk of monozygotic twinning is increased 5-6 fold in blastocyst transfer as compared with cleavage stage transfer.[30] In our study, we did not find any significantly higher contribution of blastocyst stage transfer toward the monochorionic twinning: Four pregnancies were following cleavage stage transfers and six were following blastocyst transfers.
Monochorionic twins have a more adverse outcome than their dichorionic counterparts,[20] primarily due to twin-to-twin transfusion syndrome and single fetal demise. Twin-to-twin transfusion syndrome occurs in around 9% of MCDA twins and is an important cause of perinatal morbidity and mortality.[10,11,12] However, there were no cases of twin-to-twin transfusion syndrome among our case series, which could be due to the limited number of cases in our study. After single fetal death, the co-twin has a higher chance of intra-uterine fetal demise and neurodevelopmental morbidity in MCDA twins than in DCDA twins.[13]
In our study, there was a tendency toward a higher miscarriage rate in the MCDA group of 50% (5/10) than the DCDA group which had a miscarriage rate of 10% (1/10). Of the five miscarriages in the MCDA group, three were second trimester miscarriages (at 17, 19, and 23 weeks) which entail a higher mental and physical strain on the mother.[31] On the other hand, among the DCDA group, there were no second trimester miscarriages. There is a some data to suggest that miscarriages (especially second trimester miscarriages) are higher among MCDA pregnancies than DCDA pregnancies, and this can be extrapolated to ART pregnancies as well.[32] However, the data for the relative miscarriage risk between ART conceived MCDA and DCDA pregnancies is still nascent and more data is needed to make a definite assessment of this risk.
There were four live births and one ongoing pregnancy among the ten MCDA pregnancies giving a live birth rate of 40% (4/10) and nine live births among the ten DCDA pregnancies giving a live birth rate of 90%. Among the MCDA twins, the discordancy rate was 100% (2/2) and in the DCDA group was 14.2% (1/7).
Twins conceived following ART have a more adverse neonatal outcome than naturally conceived twins with an elevated risk of cesarean section, preterm delivery and perinatal death among ART twins.[3] There is evidence that the perinatal mortality of monochorionic pregnancies is higher than in dichorionic pregnancies among natural conceptions.[32] The same could be extrapolated to ART pregnancies as well. In our current series, the similar neonatal mortality was noted among monochorionic pregnancies and dichorionic pregnancies (25% vs. 22.2%).
The patient counseling before ART regarding multiple pregnancies is usually based on the evidence base of dichorionic twins (which are the most common type of multiple pregnancy after ART). At the stage of embryo transfer, it is important to counsel patients regarding the possibility of monochorionic twinning, which may lead to a multiple pregnancy even after a single embryo transfer. In our study, two MCDA twins had resulted after a single embryo transfer.
An early transvaginal ultrasound scan at 6 weeks of gestation is indicated to determine the number of sacs and the chorionicity, especially in the background of an unexpectedly elevated β-hCG.[33] When faced with the diagnosis of a monochorionic twin, the couples need to be counseled regarding the difference in the prognosis of this particular diagnosis. However, given the paucity of data available regarding the outcome of monochorionic twins following ART, this counseling is a challenging prospect. The evidence base regarding the outcome of monozygotic twins in ART is still evolving and the largest study evaluating the outcome of 70 ART conceived monozygotic twins concluded that the prognosis was poor, especially for single implantation monozygotic twins and for nonreduced higher order multiple pregnancies, which had monozygotic twins as a component.[34]
The other aspect with regards to triplets (and other higher order multiples) with a monochorionic twin component is the dilemma with regards to multifetal reduction. Regarding this, the limited evidence base suggests that the prognosis for the higher order multiple pregnancies is significantly improved by selective reduction of the monozygotic component of the pregnancy.[34,35,36] In our current series, of the four triplets with an MCDA component, the only pregnancy which ended in a term live birth was the pregnancy, which had underwent a multifetal pregnancy reduction from triplets to twins, reducing the MCDA component. However, further research is need before this can be extrapolated.
The low numbers in this case-control study meant that only those outcomes, which had enough numbers could be analyzed and statistical significance could not be obtained for many of the outcomes. However, considering that monochorionic twinning is a rare event, the number of cases obtainable in even a tertiary care center would be limited.
However, given the rarity of this outcome after ART, there is a need for a comprehensive database on monochorionic pregnancies after ART with record of their outcomes in order to better analyze this disorder and give a more comprehensive counseling and formulate a protocol to reduce the perinatal morbidity of these pregnancies.
CONCLUSION
To conclude, we found that monochorionic pregnancies resulting from ART have a more adverse obstetric outcome than their dichorionic counterparts. Furthermore, the subgroup of triplet with a monochorionic twin component had a poor live birth outcome. The diagnosis of a monochorionic pregnancy after ART prognosticates the need for heightened antenatal surveillance and feto-maternal medicine specialist supervision along with good neonatal care to optimize the outcome.
ACKNOWLEDGEMENT
We wish to acknowledge the help of MS. Gowri of the Department of Biostatistics, Christian Medical College, Vellore for her help with the statistical analysis of the data.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.de Mouzon J, Goossens V, Bhattacharya S, Castilla JA, Ferraretti AP, Korsak V, et al. Assisted reproductive technology in Europe, 2007: Results generated from European registers by ESHRE. Hum Reprod. 2012;27:954–66. doi: 10.1093/humrep/des023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sunderam S, Kissin DM, Crawford S, Anderson JE, Folger SG, Jamieson DJ, et al. Assisted reproductive technology surveillance – United States, 2010. MMWR Surveill Summ. 2013;62:1–24. [PubMed] [Google Scholar]
- 3.Rossi AC, D’Addario V. Neonatal outcomes of assisted and naturally conceived twins: Systematic review and meta-analysis. J Perinat Med. 2011;39:489–93. doi: 10.1515/jpm.2011.058. [DOI] [PubMed] [Google Scholar]
- 4.Derom C, Thiery E, Peeters H, Vlietinck R, Defoort P, Frijns JP. The East Flanders Prospective Twin Survey (EFPTS): An actual perception. Twin Res Hum Genet. 2013;16:58–63. doi: 10.1017/thg.2012.75. [DOI] [PubMed] [Google Scholar]
- 5.Vitthala S, Gelbaya TA, Brison DR, Fitzgerald CT, Nardo LG. The risk of monozygotic twins after assisted reproductive technology: A systematic review and meta-analysis. Hum Reprod Update. 2009;15:45–55. doi: 10.1093/humupd/dmn045. [DOI] [PubMed] [Google Scholar]
- 6.Paek B, Shields LE. Twin-to-twin transfusion syndrome: Diagnosis and treatment. Curr Womens Health Rev. 2005;1:43–7. [Google Scholar]
- 7.Benirschke K, Kim CK. Multiple pregnancy 1. N Engl J Med. 1973;288:1276–84. doi: 10.1056/NEJM197306142882406. [DOI] [PubMed] [Google Scholar]
- 8.Benirschke K, Kim CK. Multiple pregnancy 2. N Engl J Med. 1973;288:1329–36. doi: 10.1056/NEJM197306212882505. [DOI] [PubMed] [Google Scholar]
- 9.Knopman J, Krey LC, Lee J, Fino ME, Novetsky AP, Noyes N. Monozygotic twinning: An eight-year experience at a large IVF center. Fertil Steril. 2010;94:502–10. doi: 10.1016/j.fertnstert.2009.03.064. [DOI] [PubMed] [Google Scholar]
- 10.Lewi L. Monochorionic diamniotic twin pregnancies pregnancy outcome, risk stratification and lessons learnt from placental examination. Verh K Acad Geneeskd Belg. 2010;72:5–15. [PubMed] [Google Scholar]
- 11.Lewi L, Deprest J, Hecher K. The vascular anastomoses in monochorionic twin pregnancies and their clinical consequences. Am J Obstet Gynecol. 2013;208:19–30. doi: 10.1016/j.ajog.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 12.Lewi L, Gucciardo L, Van Mieghem T, de Koninck P, Beck V, Medek H, et al. Monochorionic diamniotic twin pregnancies: Natural history and risk stratification. Fetal Diagn Ther. 2010;27:121–33. doi: 10.1159/000313300. [DOI] [PubMed] [Google Scholar]
- 13.Hillman SC, Morris RK, Kilby MD. Co-twin prognosis after single fetal death: A systematic review and meta-analysis. Obstet Gynecol. 2011;118:928–40. doi: 10.1097/AOG.0b013e31822f129d. [DOI] [PubMed] [Google Scholar]
- 14.Morin L, Lim K, Bly S, Butt K, Cargill YM, Davies G, et al. Ultrasound in twin pregnancies: No.260, June 2011. Int J Gynecol Obstet. 2011;115:117–8. [Google Scholar]
- 15.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology, 2009. Hum Reprod. 2009;24:2683–7. doi: 10.1093/humrep/dep343. [DOI] [PubMed] [Google Scholar]
- 16.Doke PP, Karantaki MV, Deshpande SR. Adverse pregnancy outcomes in rural Maharashtra, India (2008-09): A retrospective cohort study. BMC Public Health. 2012;12:543. doi: 10.1186/1471-2458-12-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO. Maternal mortality ratio (per 100 000 live births) WHO. [Last cited on 2014 Feb 01]. Available from: http://www.who.int/healthinfo/statistics/indmaternalmortality/en/
- 18.Miller J, Chauhan SP, Abuhamad AZ. Discordant twins: Diagnosis, evaluation and management. Am J Obstet Gynecol. 2012;206:10–20. doi: 10.1016/j.ajog.2011.06.075. [DOI] [PubMed] [Google Scholar]
- 19.Management of Twin Pregnancies (Part 1) – 91E-CONS1-Jul2000.pdf. [Last cited on 2014 Feb 01]. Available from: http://www.sogc.org/wp-content/uploads/2013/01/91E-CONS1-Jul2000.pdf .
- 20.Dubé J, Dodds L, Armson BA. Does chorionicity or zygosity predict adverse perinatal outcomes in twins? Am J Obstet Gynecol. 2002;186:579–83. doi: 10.1067/mob.2002.121721. [DOI] [PubMed] [Google Scholar]
- 21.Lewi L, Van Schoubroeck D, Gratacós E, Witters I, Timmerman D, Deprest J. Monochorionic diamniotic twins: Complications and management options. Curr Opin Obstet Gynecol. 2003;15:177–94. doi: 10.1097/00001703-200304000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Hargitai B, Marton T, Cox PM. Best practice no 178. Examination of the human placenta. J Clin Pathol. 2004;57:785–92. doi: 10.1136/jcp.2003.014217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scheurlen W, von Stockhausen HB, Kreth HW. Diagnosis of monozygosity in multiple births by DNA fingerprinting. Monatsschr Kinderheilkd. 1991;139:30–2. [PubMed] [Google Scholar]
- 24.Weinberg W. Contributions to the physiology and pathology of multiple births in humans. Archive for the whole physiology and pathology of humans and animals. 1901;88:346–430. [Google Scholar]
- 25.Alikani M, Cekleniak NA, Walters E, Cohen J. Monozygotic twinning following assisted conception: An analysis of 81 consecutive cases. Hum Reprod. 2003;18:1937–43. doi: 10.1093/humrep/deg369. [DOI] [PubMed] [Google Scholar]
- 26.Abusheikha N, Salha O, Sharma V, Brinsden P. Monozygotic twinning and IVF/ICSI treatment: A report of 11 cases and review of literature. Hum Reprod Update. 2000;6:396–403. doi: 10.1093/humupd/6.4.396. [DOI] [PubMed] [Google Scholar]
- 27.Steinman G. Mechanisms of twinning. VI. Genetics and the etiology of monozygotic twinning in in vitro fertilization. J Reprod Med. 2003;48:583–90. [PubMed] [Google Scholar]
- 28.Schachter M, Raziel A, Friedler S, Strassburger D, Bern O, Ron-El R. Monozygotic twinning after assisted reproductive techniques: A phenomenon independent of micromanipulation. Hum Reprod. 2001;16:1264–9. doi: 10.1093/humrep/16.6.1264. [DOI] [PubMed] [Google Scholar]
- 29.Skiadas CC, Missmer SA, Benson CB, Gee RE, Racowsky C. Risk factors associated with pregnancies containing a monochorionic pair following assisted reproductive technologies. Hum Reprod. 2008;23:1366–71. doi: 10.1093/humrep/den045. [DOI] [PubMed] [Google Scholar]
- 30.Practice Committee of Society for Assisted Reproductive Technology, Practice Committee of American Society for Reproductive Medicine. Elective single-embryo transfer. Fertil Steril. 2012;97:835–42. doi: 10.1016/j.fertnstert.2011.11.050. [DOI] [PubMed] [Google Scholar]
- 31.Michels TC, Tiu AY. Second trimester pregnancy loss. Am Fam Physician. 2007;76:1341–6. [PubMed] [Google Scholar]
- 32.Al Riyami N, Al-Rusheidi A, Al-Khabori M. Perinatal outcome of monochorionic in comparison to dichorionic? Twin pregnancies. Oman Med J. 2013;28:173–7. doi: 10.5001/omj.2013.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh N, Begum AA, Malhotra N, Bahadur A, Vanamail P. Role of early serum beta human chorionic gonadotropin measurement in predicting multiple pregnancy and pregnancy wastage in an in vitro ET fertilization cycle. J Hum Reprod Sci. 2013;6:213–8. doi: 10.4103/0974-1208.121425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vela G, Luna M, Barritt J, Sandler B, Copperman AB. Monozygotic pregnancies conceived by in vitro fertilization: Understanding their prognosis. Fertil Steril. 2011;95:606–10. doi: 10.1016/j.fertnstert.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 35.De Catte L, Camus M, Foulon W. Monochorionic high-order multiple pregnancies and multifetal pregnancy reduction. Obstet Gynecol. 2002;100:561–6. doi: 10.1016/s0029-7844(02)02075-6. [DOI] [PubMed] [Google Scholar]
- 36.Li R, Chen X, Yang S, Yang R, Ma C, Liu P, et al. Retain singleton or twins? Multifetal pregnancy reduction strategies in triplet pregnancies with monochorionic twins. Eur J Obstet Gynecol Reprod Biol. 2013;167:146–8. doi: 10.1016/j.ejogrb.2012.11.018. [DOI] [PubMed] [Google Scholar]


