Abstract
Uretero-ileal anastomotic stricture is a potentially serious late complication after ileal conduit formation, with a reported incidence of 3–9%. The standard management technique is open surgical revision of the anastomosis with reimplantation of the affected ureter. This is technically challenging and has potential significant morbidity for the patient. Advances in endourological techniques now offer a variety of less-invasive treatment options, like balloon dilatation or laser ureterotomy followed by stent insertion. What happens when such open and minimally invasive techniques fail? Recently, using a combined antegrade and retrograde approach, we inserted a novel, semi-permanent, dual-expansion thermo-expandable metallic alloy stent across a recurrent ileal-ureteric stricture. We describe the technique and potential advantages of this minimally invasive method. This minimally invasive treatment option is of interest, as in contrast to other stents, it does not require routine change, and is resistant to corrosion and urothelial ingrowth, hence ensuring ease of exchange or removal if required.
Abbreviations: PCNL, percutaneous nephrolithotomy
Keywords: Stricture, Anastomosis, Ileum conduit, Stent, Memokath
1. Introduction
Uretero-ileal anastomotic stricture is a potentially serious complication after ileal conduit formation, with a reported incidence of 3–9% [1–3]. The standard treatment for uretero-ileal strictures in ileal conduits is open revision with reimplantation of the ureter [4,5]. Endourological approaches offer minimally invasive options with potentially less patient morbidity [6]. Dilatation of strictures with semi-rigid serial dilators, balloon dilatation, Acucise® cutting balloon (Applied Medical Resources Corp., Laguna Hills, CA) endoureterotomy or laser ureterotomy are examples, but they are associated with a high stricture recurrence rate [5,7–10].
In patients at high medical risk, and those who have had failed revisions, but also in those who have failed minimally invasive procedures, placing a conventional ureteric JJ stent remains an option. However, these patients have to undergo 3–6 monthly stent exchanges, and JJ stents are also often poorly tolerated and have significant morbidity [11].
The Memokath® 051 (PNN Medical, Copenhagen, Denmark) stent has recently been shown to be an attractive long-term and cost-effective minimally invasive option for both benign and malignant ureteric strictures [12]. It is resistant to urothelial ingrowth and corrosion [13–16], and therefore seems to be a good option for treating such strictures, although its use in uretero-ileal anastomotic strictures has not been reported to date.
2. Technique
Under general anaesthesia, the patient is placed supine as for percutaneous nephrolithotomy (PCNL), with a 10–15° tilt of the ipsilateral trunk. Percutaneous renal access is obtained by standard PCNL techniques, and a nephrostogram taken to confirm the position and length of the stricture (Fig. 1). A guidewire is inserted via the percutaneous tract through the stricture and externalised through the conduit using the flexible cystoscope, leaving a ‘through and through wire’.
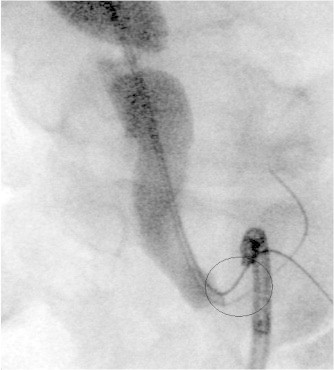
Figure 1.

Nephrostogram to visualize the position of the stricture marked with a circle.
This wire is exchanged for a stiffer wire, over which the anastomotic stricture is then balloon-dilated. A second guidewire is inserted through the stricture serving as a ‘safety wire’ (Fig. 2). The first ‘working wire’ is then used to guide the insertion system for the Memokath. If needed, slight traction on both ends can increase the rigidity and allow for increased radial force to pass the stricture with endoscopic instruments and devices. By flushing the thermolabile stent with hot sterile water, both ends expand, anchoring the stent proximally and distally of the stricture. A contrast-medium view confirms the position of the stent (Fig. 3). The dual-expansion version of the Memokath was used to reduce the risk of proximal migration of the stent into the dilated ureter above the stricture.
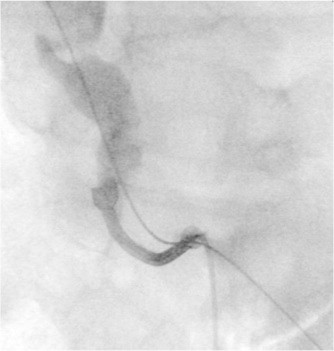
Figure 2.
Two wires passing through the stricture. The flexible cystoscope is placed inside the ileal conduit at the distal end of the stricture. Note the awkward, acute angle at the anastomotic stricture.
Figure 3.
Both ends of the stent are expanded and a subsequent contrast-medium study using a ureteric catheter confirms the good position of stent.
3. Discussion
Permanent or at least long-term stent placement seems to be an attractive option in such patients, where other endourological approaches, such as dilatation of the strictures with semi-rigid serial dilators, balloon dilatation, cutting balloon endoureterotomy or ureterotomy, have failed, and where open revision is technically complicated or would put the patient at risk. Several metallic stents have been introduced for this purpose.
The metallic ureteric Resonance® stent (Cook Urological, Spencer IN, USA), can remain in situ for 12 months before needing an exchange. This stent was recently investigated for treating uretero-ileal anastomotic strictures, but the results were inconsistent and a high migration rate was reported [4,17].
Other metallic stents, like the self-expanding mesh stents, have shown encouraging short-term but disappointing long-term success rates. The main drawback is their often heavy urothelial in- and over-growth, leading to obstruction and making repositioning or removal impossible [18,19].
A newer stent, the Memokath 051, was recently shown to be an attractive long-term and cost-effective minimally invasive management option for both benign and malignant ureteric strictures, and a durable minimally invasive alternative to JJ stents or reconstructive surgery [12]. This stent is composed of a thermo-expandable nickel-titanium alloy; it has a shaft diameter of 10.5 F and its fluted ends expands to 20 F. The stent is available in various lengths, from 30 to 200 mm. Its spiral structure, which can adapt to the curves of the ureter, prevents ischaemic lesions of the ureter by avoiding outward pressure. At the same time the tight coils prevent urothelial in-growth, and its titanium component makes it resistant to corrosion and allows exchange if necessary [13–16].
The patient reported here had undergone cystectomy for a non-oncological indication. However, tumour as a reason for anastomotic strictures in ileal conduits is a possibility, albeit mostly after tumour cystectomy [20]. We excluded a malignancy by endoscopic inspection of the stricture and a ‘conduit-gram’.
The use of the Memokath 051® in uretero-ileal anastomotic strictures has not been reported to date, and is challenging due to the difficult access to the stricture. An often awkward access angle can be overcome by using the described technique of a ‘through-and-through’ guidewire, which allows the system to be straightened when pulled. This will allow the stent to be inserted using the usual standard technique.
We used the dual-expansion version of the stent to reduce the risk of proximal migration of the stent, as the ureter above the stricture was significantly dilated. Once the stent was in the desired position, 60 °C warm sterile water was instilled and the full expansion of both ends could be visualized in real time by image-intensifier screening. A final contrast-medium study confirmed the correct stent position and decompression of the upper urinary tract.
Conflict of Interest
The authors have no conflict of interest to declare.
References
- 1.Hetet J.F., Rigaud J., Karam G., Glémain P., Le Normand L., Bouchot O. Complications of Bricker ileal conduit urinary diversion: analysis of a series of 246 patients. Prog Urol. 2005;15:23–29. [PubMed] [Google Scholar]
- 2.Schmidt J.D., Hawtrey C.E., Flocks R.H., Culp D.A. Complications, results and problems of ileal conduit diversions. J Urol. 1973;109:210–216. doi: 10.1016/s0022-5347(17)60390-2. [DOI] [PubMed] [Google Scholar]
- 3.Weijerman P.C., Schurmans J.R., Hop W.C., Schroder F.H., Bosch J.L. Morbidity and quality of life in patients with orthotopic and heterotopic continent urinary diversion. Urology. 1998;51:51–56. doi: 10.1016/s0090-4295(97)00461-5. [DOI] [PubMed] [Google Scholar]
- 4.Liatsikos E., Kallidonis P., Kyriazis I., Constantinidis C., Hendlin K., Stolzenburg J.U. Ureteral obstruction: is the full metallic double-pigtail stent the way to go? Eur Urol. 2010;57:480–486. doi: 10.1016/j.eururo.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 5.Meretyk S., Clayman R.V., Kavoussi L.R., Kramolowsky E.V., Picus D.D. Endourological treatment of ureteroenteric anastomotic strictures: long-term followup. J Urol. 1991;145:723–777. doi: 10.1016/s0022-5347(17)38435-5. [DOI] [PubMed] [Google Scholar]
- 6.Buchholz N.E.I., Howairis M., Bach C., Moraitis K., Masood J. From stone cutting to high-technology methods. The changing face of stone surgery. Arab J Urol. 2011;9:25–27. doi: 10.1016/j.aju.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin D.W., Bush W.H., Mayo M.E. Endourological treatment of ureteroenteric strictures: efficacy of Acucise endoureterotomy. J Urol. 1999;162:696–698. doi: 10.1097/00005392-199909010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Kwak S., Leef J.A., Rosenblum J.D. Percutaneous balloon catheter dilatation of benign ureteral strictures: effect of multiple dilatation procedures on long-term patency. AJR Am J Roentgenol. 1995;165:97–100. doi: 10.2214/ajr.165.1.7785643. [DOI] [PubMed] [Google Scholar]
- 9.Cornud F., Chretien Y., Helenon O., Casanova J.M., Correas J.M., Bonnel D. Percutaneous incision of stenotic uroenteric anastomoses with a cutting balloon catheter: long-term results. Radiology. 2000;214:358–362. doi: 10.1148/radiology.214.2.r00fe03358. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro M.J., Banner M.P., Amendola M.A., Gordon R.L., Pollack H.M., Wein A.J. Balloon catheter dilation of ureteroenteric strictures: long-term results. Radiology. 1988;168:385–387. doi: 10.1148/radiology.168.2.3393656. [DOI] [PubMed] [Google Scholar]
- 11.Maan Z., Patel D., Moraitis K., El-Husseiny T., Papatsoris A.G., Buchholz N.P. Comparison of stent-related symptoms between conventional Double-J stents and a new-generation thermoexpandable segmental metallic stent: a validated-questionnaire-based study. J Endourol. 2010;24:589–593. doi: 10.1089/end.2009.0318. [DOI] [PubMed] [Google Scholar]
- 12.Papatsoris A.G., Buchholz N. A novel thermo-expandable ureteral metal stent for the minimally invasive management of ureteral strictures. J Endourol. 2010;24:487–491. doi: 10.1089/end.2009.0138. [DOI] [PubMed] [Google Scholar]
- 13.Klarskov P., Nordling J., Nielsen J.B. Experience with Memokath 051 ureteral stent. Scand J Urol Nephrol. 2005;39:169–172. doi: 10.1080/00365590510007720. [DOI] [PubMed] [Google Scholar]
- 14.Kulkarni R., Bellamy E. Nickel-titanium shape memory alloy Memokath 051 ureteral stent for managing long-term ureteral obstruction: 4-year experience. J Urol. 2001;166:1750–1754. [PubMed] [Google Scholar]
- 15.Kulkarni R.P., Bellamy E.A. A new thermo-expandable shape-memory nickel-titanium alloy stent for the management of ureteric strictures. BJU Int. 1999;83:755–759. doi: 10.1046/j.1464-410x.1999.00054.x. [DOI] [PubMed] [Google Scholar]
- 16.Staios D., Shergill I., Thwaini A., Junaid I., Buchholz N.P. The Memokath stent. Expert Rev Med Dev. 2007;4:99–101. doi: 10.1586/17434440.4.2.99. [DOI] [PubMed] [Google Scholar]
- 17.Garg T., Guralnick M.L., Langenstroer P., See W.A., Hieb R.A., Rilling W.S. Resonance metallic ureteral stents do not successfully treat ureteroenteric strictures. J Endourol. 2009;23:1199–1201. doi: 10.1089/end.2008.0454. [DOI] [PubMed] [Google Scholar]
- 18.Hekimoglu B., Men S., Pinar A., Ozmen E., Soylu S.O., Conkbayir I. Urothelial hyperplasia complicating use of metal stents in malignant ureteral obstruction. Eur Radiol. 1996;6:675–681. doi: 10.1007/BF00187672. [DOI] [PubMed] [Google Scholar]
- 19.Pollak J.S., Rosenblatt M.M., Egglin T.K., Dickey K.W., Glickman M. Treatment of ureteral obstructions with the Wallstent endoprosthesis: preliminary results. J Vasc Interv Radiol. 1995;6:417–425. doi: 10.1016/s1051-0443(95)72833-0. [DOI] [PubMed] [Google Scholar]
- 20.Yossepowitch O., Dalbagni G., Golijanin D. Orthotopic urinary diversion after cystectomy for bladder cancer implications for cancer control and patterns of disease recurrence. J Urol. 2003;169:177–181. doi: 10.1016/S0022-5347(05)64062-1. [DOI] [PubMed] [Google Scholar]


