Abstract
Background
This Stage II trial builds on a Stage I trial comparing the single-gender Women’s Recovery Group (WRG) to mixed-gender Group Drug Counseling (GDC) that demonstrated preliminary support for the WRG in treating women with substance use disorders. The Stage II trial aims were to (1) investigate effectiveness of the WRG relative to GDC in a sample of women heterogeneous with respect to substance of abuse and co-occurring psychiatric disorders, and (2) demonstrate the feasibility of implementing WRG in an open-enrollment group format at two sites.
Method
In this randomized clinical trial, participants were included if they were substance dependent and had used substances within the past 60 days (n = 158). Women were randomized to WRG (n = 52) or GDC (n = 48); men were assigned to GDC (n = 58). Substance use outcomes were assessed at months 1–6 and 9.
Results
Women in both the WRG and GDC had reductions in mean number of substance use days during treatment (12.7 vs 13.7 day reductions for WRG and GDC, respectively) and 6 months post-treatment (10.3 vs 12.7 day reductions); however, there were no significant differences between groups.
Conclusions
The WRG demonstrated comparable effectiveness to standard mixed-gender treatment (i.e., GDC) and is feasibly delivered in an open-group format typical of community treatment. It provides a manual-based group therapy with women-focused content that can be implemented in a variety of clinical settings for women who are heterogeneous with respect to their substance of abuse, other co-occurring psychiatric disorders, and life-stage.
Keywords: Substance use disorders, Gender differences, Women, Treatment Outcomes, Group Therapy
1. INTRODUCTION
Substance use disorders (SUDs) are a growing health problem among women in the United States (Substance Abuse and Mental Health Services Administration (SAMHSA), 2009). For example, since the late 1980’s there has been a narrowing of the gender gap in the male to female prevalence ratio of alcohol use disorders in the U.S., and levels of abstaining have decreased in women in birth cohorts born after versus before World War II, while these rates remained stable in men (Grucza et al., 2008). Gender-specific SUD treatment approaches for women are informed by research highlighting the importance of co-occurring psychiatric disorders, histories of trauma, and relationships with children and significant others that are important in women’s recovery (Greenfield and Pirard, 2009). Nevertheless, there are few therapies developed for women with SUDs, and fewer empirical studies on the relative effectiveness of these therapies versus standard treatments for this population (Greenfield et al., 2007a; Tang et al., 2012), or in comparison with mixed-gender SUD treatment (Bride, 2001; Greenfield et al., 2007a; Kaskutas et al., 2005; Orwin et al., 2001). Those that do exist were designed for specific subpopulations of women with SUDs, such as pregnant women (Reynolds et al., 1995), methadone maintained mothers (Luthar and Suchman, 2000), women with co-occurring post-traumatic stress (Hien et al., 2004; Najavits et al., 1998), women in correctional settings (Messina et al., 2010), among others (Greenfield et al., 2007a; Kelly et al., 2000; Linehan et al., 1999). However, women in community treatment programs often use multiple substances, have various co-occurring psychiatric disorders, are of different ages and may or may not be pregnant or parenting (Greenfield et al., 2007a; SAMHSA, 2012). Although SUD treatment is most frequently offered in groups (Hodgins et al., 1997; Kominars and Dornheim, 2004; Morgan-Lopez and Fals-Stewart, 2006; Stinchfield et al., 1994), there has been no manual-based, empirically-tested group therapy designed for this heterogeneous population of treatment-seeking women with SUDs.
Based on this treatment gap, we used the Stage Model of Behavioral Therapies research (Rounsaville et al., 2001) to develop and test the Women’s Recovery Group (WRG). As defined by Rounsaville and colleagues (2001), Stage I consists of manual writing and pilot and feasibility testing, and Stage II involves randomized controlled trials to investigate the efficacy of a manualized treatment that has shown promise in pilot testing. Therefore, in a Stage I behavioral therapy development trial, we developed and tested the effectiveness of the WRG compared with a standard mixed-gender group therapy (Greenfield et al., 2007b). The WRG is a manual-based group therapy for women heterogeneous with respect to their substance dependence, co-occurring psychiatric disorders, trauma history, and age and stage of life. The WRG is a 12-session, structured relapse-prevention group therapy that utilizes a cognitive behavioral approach and includes gender-specific content and single-gender group composition. Individual session content was derived from research on gender-specific substance abuse antecedents, consequences, and treatment outcomes (Greenfield et al., 2007a; Grella, 2008; Hernandez-Avila et al., 2004; Piazza et al., 1989). The content areas translated into 14 specific session topics (e.g., violence and abuse, partners and recovery, caretaking and recovery, co-occurring disorders, women’s reproductive health, effects of drugs on women’s health, disclosure) that could be flexibly implemented in any order for a 12-week sequence of groups.
In the Stage I trial (45), women were randomized to WRG (n =16) or a mixed-gender control condition, Group Drug Counseling (GDC, n = 7; Crits-Christoph et al., 1999; Daley et al., 2002). No significant differences in outcomes emerged between WRG and GDC during the 12 week group sequence. However, in the 6 months post-treatment, WRG participants showed a pattern of continued reductions in substance use while GDC participants did not (Greenfield et al., 2007b).
While these results were promising, the Stage I trial utilized a small, relatively homogeneous pilot sample and a Stage II trial was warranted to test the WRG in a larger, more diverse sample. Moreover, the WRG and GDC groups in the Stage I trial were conducted in semi-open format (i.e., enrollment continued until a maximum of 6–8 subjects were entered per group and then enrollment was closed until the end of the sequence). The design of the Stage I trial was essential for treatment development and testing (Carroll and Onken, 2005). However, most group treatment is delivered in open enrollment (or “rolling”) group format in which patients can enter at any time in the group sequence and exit the group after 12 weeks are completed (Morgan-Lopez and Fals-Stewart, 2006; Washton, 2005) rather than starting and ending with a cohort of other participants. Because the WRG is intended to be a manual-based treatment ready for dissemination into clinical practice if demonstrated to be effective (Greenfield et al., 2014), the Stage II trial was designed to be implemented in an open group format at two clinical sites. The aim of this clinical trial was to investigate the effectiveness of the WRG relative to GDC in reducing days of use of any substance from baseline in a sample of women heterogeneous with regard to drugs of abuse, co-occurring disorders, trauma histories, and age and stage of life, as well as to demonstrate the feasibility of implementing the WRG in open-enrollment group format.
2. METHODS
2.1. Participant Recruitment
Participants were recruited through treatment programs and private practices, websites, and advertisements (for detailed recruitment information see Greenfield et al., 2014). Inclusion criteria were: 1) current DSM-IV diagnosis of substance dependence for at least one substance besides nicotine; 2) age 18 years or older; 3) use of substances within the past 60 days; 4) available during the follow-up period; 5) interested in group treatment; 6) gave consent for study personnel to communicate with their treatment providers; 7) providing two individuals who could assist in locating the participant; 8) ability to attend group weekly; and 9) signed informed consent. Exclusion criteria were: 1) current medical conditions that would prevent regular group attendance; 2) mental retardation or organic mental disorder; 3) diagnosis of certain Axis I psychiatric disorders (e.g., psychotic disorders) more likely to respond to another form of treatment; 4) residential treatment in which substance use is monitored and restricted during the treatment period; 5) current need for medical detoxification (however, these participants could enter the study after detoxification); 6) current use of intravenous drugs; or 7) active engagement in self-destructive behaviors or other behaviors that would interfere with group participation (e.g., violence toward others).
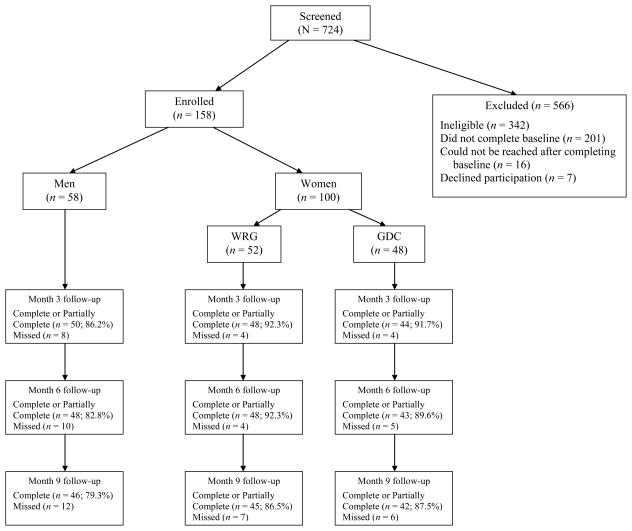
Overall, 342 participants were deemed ineligible based on our criteria (see Figure 1). One hundred fifty-eight participants (100 women and 58 men) were enrolled in the study.
Figure 1.
CONSORT diagram of study participation
2.2. Procedure
The study was conducted in outpatient clinics at an academic teaching hospital (McLean Hospital, Belmont, MA) and a community treatment program (Stanley Street Treatment and Resources, or SSTAR, Fall River, MA). Eighty-three participants were enrolled at McLean, and 75 at SSTAR. The protocol was listed in clinicaltrials.gov (Identifier: NCT01318538), approved by the McLean Hospital Institutional Review Board, and written informed consent was obtained from all participants.
Participants who met prescreen inclusion criteria completed baseline assessments. Eligible women were randomly assigned either to the experimental (WRG; n = 52) or control condition (GDC; n = 48), and all men (n = 58) were assigned to GDC. Participants could attend other outpatient treatment (e.g., individual psychotherapy, pharmacotherapy, self-help meetings, etc.) except other clinician-led SUD group therapy during their 12 weeks in study groups.
2.3. Treatments
2.3.1. The Women’s Recovery Group (WRG)
The WRG is an empirically-supported (Greenfield et al., 2007b) group therapy consisting of twelve 90-minute sessions that include a brief check-in, review of the previous week’s skill practice, topic presentation, open discussion among participants of the session topic and other recovery-related subjects, review of take-home messages and upcoming week’s skill practice, and check-out. The WRG is a relapse-prevention group therapy, based on a cognitive behavioral approach. The WRG provides education about gender-specific topics in addiction and recovery. It also provides, a safe and supportive atmosphere for open discussion of these topics to help women identify triggers to relapse and obstacles to recovery that are frequently encountered by women with SUDs, as well as skill practices to assist women in formulating strategies for relapse prevention and recovery. A central principle underlying the WRG is that the all-women group composition and the women-focused content combine to enhance outcomes for the participants. The WRG emphasizes commonalities rather than differences among participants, the need for self-care, and focuses on relapse prevention (e.g., developing skills to stay abstinent from substances) and repair work (e.g., finding balance, repairing relationships, overcoming shame and stigma) in recovery. See Greenfield et al. (2007b) for specific details and content areas of the WRG.
2.3.2. Control Group: Group Drug Counseling (GDC)
GDC (Daley et al., 2002) is a 12-session, evidence-supported group therapy (Crits-Christoph et al., 1999). GDC consists of 90-minute sessions that include the following: a check-in on substance use and craving, education and discussion on a substance-related topic, check-out, and group recitation of the serenity prayer. GDC is designed to educate patients about addiction and recovery, facilitate abstinence, encourage participation in self-help groups, and teach new mechanisms to cope with substance-related problems. GDC has a mixed-gender composition and session topics do not explicitly cover gender-specific issues.
2.4. Therapists
Eight therapists, who were all female in order to eliminate any therapist-patient gender matching effects (Fiorentine and Hillhouse, 1999; Sterling et al., 1998), were trained and randomly assigned to lead either WRG or GDC. Study therapists were required to have a master’s degree in an area that included training in psychopathology, at least two years of experience with SUD treatment, and one year of group therapy experience. Study therapists worked within the two treatment settings and were randomly assigned to provide either GDC or WRG. Group sessions were videotaped and therapists were supervised weekly by their respective supervisors (SFG for WRG; JR for GDC). Two independent raters completed adherence scales for a random selection of 20% of WRG and 10% of GDC sessions. For both groups, the extensiveness to which the therapist engaged in a behavior during the session was rated with a 5-point Likert scale (0 = not at all; 4 = extensively).
2.5. Assessments
Participants completed assessments at baseline, and follow-up assessments were conducted monthly during treatment (Months 1–3) and three months after treatment (Months 4–6), and at six months post-treatment (Month 9). Participants were compensated either $25 or $50 for participation in each research assessment, depending on the visit length.
Substance use was assessed using the Addiction Severity Index-Lite (ASI-L; McLellan et al., 1992b) and the Timeline Follow-Back (TLFB; Sobell et al., 1992). The ASI is a multidimensional assessment of substance-related problems which yields composite scores for alcohol use, drug use, psychiatric status, medical status, legal status, family/social relationships, and employment status. Composite scores range from 0 to 1, with higher scores indicating more significant problems. The TLFB uses a calendar method to calculate: days of alcohol use, days of any drug use including alcohol, days of drug use excluding alcohol, days of primary substance use, heavy drinking days, and drinks per drinking day. Urine toxicology screens were obtained at group sessions and monthly assessments to validate self-reported drug use.
The Composite International Diagnostic Interview (CIDI; World Health Organization, 1997) and the Diagnostic Interview for Personality Disorders (DIPD-IV; Zanarini et al., 1996) were administered at baseline to assess additional Axis I and Axis II psychological disorders. Use of other treatment services were assessed using the Treatment Services Review (TSR; McLellan et al., 1992a) and the Monthly Self-Help Questionnaire (MSHQ; Weiss et al., 1996). Participants were asked to report on their experiences in the “past 30 days” for the TSR and in the “last month” for the MSHQ.
2.6. Power and Statistical Analysis
The study was powered for the primary analysis concerning treatment group differences in the degree of improvement in the number of days of any substance use and in the Addiction Severity Index (ASI) composite scores. Specifically, with a total of 100 women (50 in each treatment group), the study was adequately powered to detect a minimum 5 day benefit in the number of days of any substance use (power = 83%) and a 0.2 benefit in the ASI drug and alcohol composite scores (power = 94%).
All analyses focus on comparison between women enrolled in WRG and women enrolled in GDC; men were excluded from these analyses. Background characteristics of participants were compared by treatment group (and study site), using chi-square tests for categorical variables and independent t-tests for continuous variables. Our primary substance use outcomes were the number of days of any substance use and the ASI drug and alcohol composite scores. Secondary outcomes included number of days of alcohol use, number of days of drug use, number of heavy drinking days, and number of drinks per drinking day.
In longitudinal regression analyses, changes in outcomes were compared between treatment groups; quantitative outcomes (e.g., ASI composite scores) were analyzed using linear mixed effect models, discrete outcomes (e.g., number of days of any substance use) were analyzed using loglinear (negative binomial) regression models with estimation via generalized estimating equations (GEE). These analyses focused on the changes from baseline (month 0) during the treatment phase (months 1–3), and two post-treatment phases (months 4–6, and months 7–9). The models included the effects of treatment group, phase (3 levels), and the treatment group by phase interaction. Comparison of treatment groups in terms of changes in outcomes were based on the test of interaction. The regression models accounted for the correlation among repeated measures of the outcomes over time and also adjusted for study site. We used an intent-to-treat outcome analysis, which includes all available data from all randomized participants.
For ease of interpretation, results of these analyses are presented in terms of mean changes from baseline to the end of the treatment and the two post-treatment follow-up phases, respectively; the formal comparison of these changes is based on the test for treatment group by phase interaction (see Table 3). Results from the linear mixed model analyses are presented in terms of absolute changes in the mean outcome from baseline; results from the loglinear regression model analyses are presented in terms of relative changes (percent change).
Table 3.
Reduction from baseline in mean of primary outcomes (95% confidence interval) during treatment phase (months 1–3), 3 months post-treatment (months 4–6), and 6 months post-treatment (months 7–9) phases.
| In-Treatment | 3 month post-treatment | 6 month post-treatment | ||||||
|---|---|---|---|---|---|---|---|---|
| WRG | GDC | WRG | GDC | WRG | GDC | χ2 | p-value | |
| Percent reduction in number of days of any substance use | 76.5% (65.7, 83.9) | 76.5% (63.0, 85.0) | 68.4% (56.8, 76.9) | 73.3% (58.1, 83.0) | 62.2% (43.1, 74.9) | 70.8% (56.1, 80.5) | 0.92 | 0.821 |
| ASI Alcohol | 0.27 (0.22, 0.33) | 0.33 (0.28, 0.39) | 0.28 (0.22, 0.34) | 0.36 (0.30, 0.43) | 0.30 (0.21, 0.39) | 0.35 (0.26, 0.44) | 4.08 | 0.253 |
| ASI Drug | 0.03 (0.02, 0.05) | 0.03 (0.01, 0.05) | 0.03 (0.01, 0.05) | 0.03 (0.01, 0.05) | 0.02 (−0.02, 0.05) | 0.04 (0.0, 0.07) | 1.57 | 0.667 |
Note: 3-df chi-square test for comparison between treatment groups.
3. RESULTS
3.1. Baseline Statistics
Demographic, substance use, psychiatric diagnoses, and other clinical data for the women randomized to treatment are represented in Table 1. There were no significant baseline differences between women randomized to WRG and GDC in sociodemographic characteristics, Axis I or Axis II diagnoses, days in a controlled environment, or ASI alcohol and drug composite scores. However, there were statistically significant differences between women in WRG and GDC with regard to two of the substance use variables: number of heavy drinking days and drinks per drinking day. Specifically, GDC women reported more heaving drinking days and more drinks per drinking day than WRG women (see Table 1). There were several statistically significant baseline differences in clinical characteristics of women participants between the two study sites (see Table 2). At baseline, the following additional treatment services were reported: 61% utilized individual psychotherapy; 67% attended at least one self-help group (e.g., AA) in the past month; 4% attended a visit with a substance abuse counselor; 17% used naltrexone; and 14% used acamprosate. There were no baseline group differences in additional treatment services use. Examination of group differences at end of treatment and 6 months post-treatment revealed only that naltrexone was used more by women in GDC (n = 9, 22.0%) compared to women in WRG (n = 2, 4.4%), (Fisher’s exact p < 0.05); however, the number of women using naltrexone in both groups was very low.
Table 1.
Baseline sociodemographic, substance use, and clinical characteristics of women by group assignment
| Treatment Group Assignment | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Variable | Total (N = 100) | WRG (n = 52) | GDC (n = 48) | |||
|
|
||||||
| N | (%) | N | % | N | % | |
| Race | ||||||
| White | 95 | 95.0 | 48 | 92.3 | 47 | 97.9 |
| African American | 4 | 4.0 | 3 | 5.8 | 1 | 2.1 |
| Asian | 1 | 1.0 | 1 | 1.9 | 0 | 0.0 |
| Ethnicity | ||||||
| Non-Hispanic | 99 | 99.0 | 52 | 100.0 | 47 | 97.9 |
| Marital Status | ||||||
| Married | 32 | 32.0 | 19 | 36.5 | 13 | 27.1 |
| Divorced/Separated | 35 | 35.0 | 17 | 32.7 | 18 | 37.5 |
| Never Married | 25 | 25.0 | 12 | 23.1 | 13 | 27.1 |
| Unmarried & living with partner | 6 | 6.0 | 4 | 7.7 | 2 | 4.2 |
| Widowed | 2 | 2.0 | 0 | 0.0 | 2 | 4.2 |
| Education | ||||||
| Did not graduate high school | 7 | 7.0 | 4 | 7.7 | 3 | 6.3 |
| Graduated high school | 14 | 14.0 | 7 | 13.5 | 7 | 14.6 |
| Some College | 22 | 22.0 | 11 | 21.2 | 11 | 22.9 |
| Graduated from college | 33 | 33.0 | 18 | 34.6 | 15 | 31.3 |
| Postgraduate | 24 | 24.0 | 12 | 23.1 | 12 | 25.0 |
| Household Income | ||||||
| $0 – $20,000 | 30 | 30.0 | 17 | 32.7 | 13 | 27.1 |
| $20,001 – $50,000 | 22 | 22.0 | 9 | 17.3 | 13 | 27.1 |
| $50,001 – $100,000 | 22 | 22.0 | 11 | 21.2 | 11 | 22.9 |
| More than $100,000 | 26 | 26.0 | 15 | 28.8 | 11 | 22.9 |
| Current Psychiatric Diagnoses | ||||||
| Major Depressive Disorder | 61 | 61.0 | 30 | 57.7 | 31 | 64.6 |
| Generalized Anxiety Disorder | 22 | 22.0 | 11 | 21.2 | 11 | 22.9 |
| Post-traumatic Stress Disorder | 20 | 20.0 | 9 | 17.3 | 11 | 22.9 |
| Any Axis I | 75 | 75.0 | 37 | 71.2 | 38 | 79.2 |
| Any Axis II | 17 | 17.0 | 9 | 17.3 | 8 | 16.7 |
| Substance Use Diagnoses | ||||||
| Alcohol current | 88 | 88.0 | 43 | 82.7 | 45 | 93.8 |
| Alcohol lifetime | 91 | 91.0 | 45 | 86.5 | 46 | 95.8 |
| Cocaine current | 15 | 15.0 | 8 | 15.4 | 7 | 14.6 |
| Cocaine lifetime | 31 | 31.0 | 17 | 32.7 | 14 | 29.2 |
| Cannabis current | 9 | 9.0 | 3 | 5.8 | 6 | 12.5 |
| Cannabis lifetime | 15 | 15.0 | 7 | 13.5 | 8 | 16.7 |
| Opioids current | 17 | 17.0 | 7 | 13.5 | 10 | 20.8 |
| Opioids lifetime | 25 | 25.0 | 13 | 25.0 | 12 | 25.0 |
| Sedatives current | 9 | 9.0 | 5 | 9.6 | 4 | 8.3 |
| Sedatives lifetime | 10 | 10.0 | 5 | 9.6 | 5 | 10.4 |
|
|
||||||
| Mean | SD | Mean | SD | Mean | SD | |
|
|
||||||
| Age (years) | 47 | 12.5 | 45.7 | 12.6 | 49.3 | 12.2 |
| Substance use days (past 30 days) | ||||||
| Alcohol use days | 14.1 | 10.2 | 12.7 | 9.9 | 15.5 | 10.4 |
| Days of any substance use (including alcohol) | 17.1 | 9.6 | 16.5 | 9.3 | 17.8 | 10.0 |
| Drug use days (excluding alcohol) | 4.4 | 9.1 | 4.8 | 9.2 | 4.0 | 9.1 |
| Primary Substance use days | 14.7 | 10.2 | 13.4 | 9.9 | 16.1 | 10.4 |
| Heavy Drinking days* | 12.0 | 10.4 | 9.8 | 9.7 | 14.3 | 10.7 |
| Drinks per drinking day** | 8.6 | 5.9 | 7.0 | 5.0 | 10.2 | 6.3 |
| Controlled environment days† | 0.38 | 1.6 | 0.38 | 1.6 | 0.38 | 1.6 |
| Addiction Severity Index Composite Scores | ||||||
| Alcohol | 0.52 | 0.31 | 0.47 | 0.33 | 0.59 | 0.28 |
| Drug | 0.07 | 0.11 | 0.07 | 0.11 | 0.06 | 0.12 |
| Medical | 0.19 | 0.27 | 0.18 | 0.24 | 0.21 | 0.31 |
| Psychiatric | 0.23 | 0.19 | 0.25 | 0.20 | 0.20 | 0.17 |
| Legal | 0.10 | 0.70 | 0.04 | 0.11 | 0.18 | 1.01 |
| Family | 0.27 | 0.43 | 0.29 | 0.55 | 0.25 | 0.24 |
| Employment | 0.42 | 0.26 | 0.42 | 0.24 | 0.42 | 0.28 |
Significant difference between WRG and GDC women, p < .05
Significant difference between WRG and GDC women, p < .01
Days in which participant was in a controlled environment (i.e. detox) where substances were unavailable
Table 2.
Baseline sociodemographic, substance use, and clinical characteristics of women by site
| Site | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Variable | Total (N = 100) | McLean (n = 54) | SSTAR (n = 46) | |||
|
|
||||||
| N | (%) | N | % | N | % | |
| Race | ||||||
| White | 95 | 95.0 | 53 | 98.1 | 42 | 91.3 |
| African American | 4 | 4.0 | 1 | 1.9 | 3 | 6.5 |
| Asian | 1 | 1.0 | 0 | 0.0 | 1 | 2.2 |
| Ethnicity | ||||||
| Non-Hispanic | 99 | 99.0 | 54 | 100.0 | 45 | 97.8 |
| Marital Status** | ||||||
| Married | 32 | 32.0 | 23 | 42.6 | 9 | 19.6 |
| Divorced/Separated | 35 | 35.0 | 13 | 24.1 | 22 | 47.8 |
| Never Married | 25 | 25.0 | 13 | 24.1 | 12 | 26.1 |
| Unmarried & living with partner | 6 | 6.0 | 3 | 5.6 | 3 | 6.5 |
| Widowed | 2 | 2.0 | 2 | 3.7 | 0 | 0.0 |
| Education*** | ||||||
| Did not graduate from high school | 7 | 7.0 | 0 | 0.0 | 7 | 15.2 |
| Graduated from high school | 14 | 14.0 | 3 | 5.6 | 11 | 23.9 |
| Some College | 22 | 22.0 | 10 | 18.5 | 12 | 26.1 |
| Graduated from college | 33 | 33.0 | 21 | 38.9 | 12 | 26.1 |
| Postgraduate | 24 | 24.0 | 20 | 37.0 | 4 | 8.7 |
| Household Income*** | ||||||
| $0 – $20,000 | 30 | 30.0 | 8 | 14.8 | 22 | 47.8 |
| $20,001 – $50,000 | 22 | 22.0 | 8 | 14.8 | 14 | 30.4 |
| $50,001 – $100,000 | 22 | 22.0 | 14 | 25.9 | 8 | 17.4 |
| More than $100,000 | 26 | 26.0 | 24 | 44.4 | 2 | 4.3 |
| Current Psychiatric Diagnoses | ||||||
| Major Depressive Disorder | 61 | 61.0 | 35 | 64.8 | 26 | 56.5 |
| Generalized Anxiety Disorder | 22 | 22.0 | 15 | 27.8 | 7 | 15.2 |
| Post-traumatic Stress Disorder | 20 | 20.0 | 8 | 14.8 | 12 | 26.1 |
| Any Axis I | 75 | 75.0 | 42 | 77.8 | 33 | 71.7 |
| Any Axis II* | 17 | 17.0 | 5 | 9.3 | 12 | 26.1 |
| Substance Use Diagnoses | ||||||
| Alcohol current* | 88 | 88.0 | 51 | 94.4 | 37 | 80.4 |
| Alcohol lifetime* | 91 | 91.0 | 52 | 96.3 | 39 | 84.8 |
| Cocaine current* | 15 | 15.0 | 2 | 3.7 | 13 | 28.3 |
| Cocaine lifetime** | 31 | 31.0 | 10 | 18.5 | 21 | 45.7 |
| Cannabis current | 9 | 9.0 | 3 | 5.6 | 6 | 13.0 |
| Cannabis lifetime | 15 | 15.0 | 7 | 13.0 | 8 | 17.4 |
| Opioids current | 17 | 17.0 | 7 | 13.0 | 10 | 21.7 |
| Opioids lifetime | 25 | 25.0 | 11 | 20.4 | 14 | 30.4 |
| Sedatives current | 9 | 9.0 | 6 | 11.1 | 3 | 6.5 |
| Sedatives lifetime | 10 | 10.0 | 6 | 11.1 | 4 | 8.7 |
|
|
||||||
| Mean | SD | Mean | SD | Mean | SD | |
|
|
||||||
| Age (years)* | 47 | 12.5 | 50.4 | 13.2 | 43.9 | 10.6 |
| Substance use (past 30 days) | ||||||
| Alcohol use days*** | 14.1 | 10.2 | 17.5 | 8.8 | 10.0 | 10.3 |
| Days of any substance use (including alcohol)* | 17.1 | 9.6 | 19.2 | 8.0 | 14.7 | 10.8 |
| Drug use days (excluding alcohol) | 4.4 | 9.1 | 2.7 | 7.4 | 6.3 | 10.5 |
| Primary Substance use days** | 14.7 | 10.2 | 17.3 | 9.2 | 11.7 | 10.7 |
| Heavy Drinking days** | 12.0 | 10.4 | 14.9 | 9.6 | 8.5 | 10.4 |
| Drinks per drinking day | 8.6 | 5.9 | 7.7 | 4.5 | 9.8 | 7.3 |
| Controlled environment days† | 0.38 | 1.6 | 0.50 | 1.7 | 0.24 | 1.5 |
| Addiction Severity Index Composite Scores | ||||||
| Alcohol*** | 0.52 | 0.31 | 0.65 | 0.24 | 0.38 | 0.33 |
| Drug | 0.07 | 0.11 | 0.05 | 0.09 | 0.08 | 0.13 |
| Medical | 0.19 | 0.27 | 0.16 | 0.26 | 0.23 | 0.29 |
| Psychiatric*** | 0.23 | 0.19 | 0.30 | 0.18 | 0.14 | 0.16 |
| Legal | 0.10 | 0.70 | 0.16 | 0.95 | 0.04 | 0.12 |
| Family | 0.27 | 0.43 | 0.34 | 0.54 | 0.20 | 0.24 |
| Employment* | 0.42 | 0.26 | 0.37 | 0.23 | 0.48 | 0.28 |
Significant difference between McLean and SSTAR women, p < .05 level
Significant difference between McLean and SSTAR women, p < .01 level
Significant difference between McLean and SSTAR women, p < .001 level
Days in which participant was in a controlled environment (i.e. detox) where substances were unavailable
3.2. Substance Use Outcomes
3.2.1. Primary Outcomes
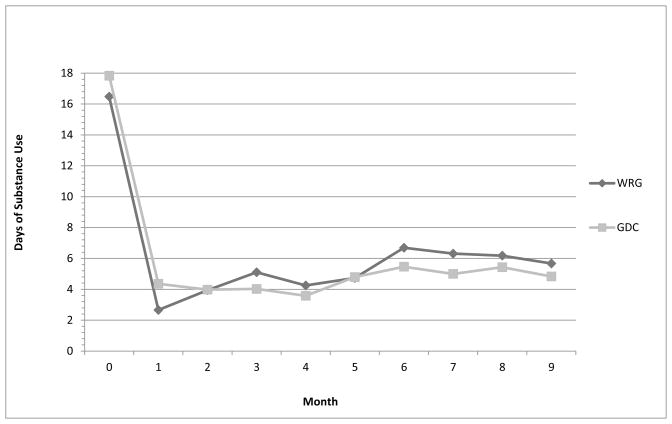
We found no significant differences between the WRG and GDC groups in terms of their reduction in mean days of any substance use, and reductions in mean ASI alcohol and drug composite scores (see Table 3). Overall, mean days of substance use decreased significantly from baseline during the in-treatment phase for both groups, with a 76.5% reduction in both groups (WRG versus GDC rate ratio = 1.00; 95% CI: 0.55, 1.80); these reductions correspond to 12.7 (χ2=56.4, d=1, p<0.0001) and 13.7 (χ2=39.3, df=1, p<0.0001) day reductions for the WRG and GDC groups, respectively (See Figure 2). For both groups, mean days of any substance use also decreased significantly from baseline during the two post-treatment phases. Specifically, there were 68.4% and 73.3% reductions during the 3 month post-treatment phase for the WRG and GDC groups, respectively (rate ratio = 0.85; 95% CI: 0.49, 1.47); these reductions correspond to 11.3 (χ2=51.6, df=1, p<0.0001) and 13.2 (χ2=33.0, df=1, p<0.0001) day reductions for the WRG and GDC groups, respectively. Similarly, there were 62.2% and 70.8% reductions during the 6 month post-treatment phase for the WRG and GDC groups, respectively (rate ratio = 0.77; 95% CI: 0.43, 1.37); these reductions correspond to 10.3 (χ2=21.8, df=1, p<0.0001) and 12.7 (χ2=35.2, df=1, p<0.0001) day reductions.
Figure 2.
Time Plot of Mean Days of Any Substance Use
For both treatment groups, the mean ASI alcohol composite scores also declined (improved) during the in-treatment phase and the two post-treatment phases. During the in-treatment phase, the mean ASI alcohol composite declined by 0.27 (χ2=107.3, df=1, p<0.0001) and 0.33 (χ2=143.5, df=1, p<0.0001) for the WRG and GDC groups, respectively (WRG versus GDC difference = −0.057; 95% CI: −0.134, 0.020). During the 6 month post-treatment phase, the mean ASI alcohol composite declined by 0.30 (χ2=46.0, df=1, p<0.0001) and 0.35 (χ2=58.5, df=1, p<0.0001) for the WRG and GDC groups, respectively (difference = −0.054; 95% CI: −0.180, 0.072). For both treatment groups, there were very modest declines of 0.03 (χ2=16.2, df=1, p<0.0001; χ2=13.7, df=1, p<0.0005, for WRG and GDC groups, respectively) in the mean ASI drug composite scores during the in-treatment phase (see Table 3; difference = 0.0; 95% CI: −0.022, 0.025); the declines were not significant during the 6 month post-treatment phase (χ2=0.8, df=1, p>0.3; χ2=3.8, df=1, p>0.05, for WRG and GDC groups, respectively).
3.2.2. Secondary Outcomes
We found no significant differences between the WRG and GDC groups in terms of their reduction in mean number of alcohol use days and mean number of drug use days during the in-treatment and post-treatment phases. In addition, no significant differences between WRG and GDC groups were found in heavy drinking days or drinks per drinking day.
Overall, women in both the WRG and GDC groups had significant (p<0.0001) reductions in mean number of alcohol use days during treatment (9.9 and 12.4 day reductions for WRG and GDC, respectively) and at 6 months post-treatment (8.3 and 12.2 day reductions). Similarly, women in both the WRG and GDC groups had significant (p<0.05) reductions in mean number of drug use days during treatment (3.0 and 1.5 day reductions for WRG and GDC, respectively); however, at 6 months post-treatment, the reductions were significant for WRG (2.8 day reduction; p<0.05) but not for GDC (1.6 day reduction; p>0.1). In addition, women in both the WRG and GDC groups had significant (p<0.0001) reductions in mean number of heavy drinking days during treatment (8.6 and 12.1 day reductions for WRG and GDC, respectively) and at 6 months post-treatment (8.0 and 11.8 day reductions). Finally, women in both the WRG and GDC groups had significant (p<0.05) reductions in mean number of drinks per drinking day only during the in-treatment phase (2.0 and 2.9 reductions for WRG and GDC, respectively).
3.2.3. Quality Assurance
We compared participants’ self-report of substance use to urine toxicology screens. Of the self-reported weekly and monthly data, 78.1% were concordant with urine screens, 19.8% were cases of reported substance use that was not detected by urine screen, and 2.1% were considered discordant (i.e., a positive urine screen when no use was self-reported). Thus, 97.9% of all self-reports were either consistent with urine screens or reported use undetected by urine screens.
3.3. Therapist Adherence
Percent agreement between the independent raters for each item of the two scales was calculated to assess inter-rater reliability. For WRG, percent agreement scores ranged from 66–100%, with an average agreement score of 86%. For GDC, percent agreement scores ranged from 61–100%, with an average agreement score of 81%. An overall mean score for each scale was calculated to assess therapist adherence. The mean for WRG therapist adherence was 3.8 (SD=0.13) and the mean for GDC therapist adherence was 3.6 (SD=0.28).
3.4. Group Stability and Attendance
We also compared treatment attendance rates and the stability of group membership across WRG and GDC women. Treatment attendance was calculated by summing the number of treatment sessions attended; there were no differences between WRG (M=7.64, SD=1.36) and GDC (M=7.69, SD=1.36). Treatment group stability was calculated using the Percentage of Group Change Index (Morgan-Lopez and Fals-Stewart, 2008) which captures change in group membership composition from session-to-session separately for each individual within each group (specific to the calendar period that each person was in the group). The value can range from 0 (i.e., the exact same membership from one session to the next) to 1 (i.e., complete turnover in membership). The average values across all sessions were taken to get an overall sense of the amount of turnover each person experienced in the group during the period in calendar time they were in treatment. There were no significant differences between WRG (M=.386, SD=.07) and GDC (M=.356, SD=.07) in the proportion of members that “turned over” from session-to-session.
4. DISCUSSION
In this Stage II trial, women in both the WRG and the GDC conditions had significant reductions of approximately 75% fewer days of substance use during the 12-week group treatment and these reductions were sustained during the 6-month post-treatment follow-up period. This study provides evidence that women with alcohol and drug dependence, with or without co-occurring other psychiatric disorders, can have significant reductions in their substance use through treatment in weekly outpatient group therapy and maintain these reductions 6 months after treatment ends.
This Stage II trial of the WRG did not replicate the findings of the Stage I trial that demonstrated sustained reductions in days of substance use for the WRG but not for GDC (Greenfield et al., 2007b). However, the Stage II trial demonstrated that the WRG is comparable to standard mixed-gender GDC treatment even when implemented in an open enrollment group format that is typical of community treatment settings. The theoretical model of WRG posits the synergism between women-focused group session content and the all-women group composition (Greenfield et al., 2007b). Our qualitative studies of the Stage I WRG (Greenfield et al., 2013a, 2013b) demonstrated that women participants in WRG found the support of other women in the group to be an essential component of the WRG (Greenfield et al., 2013a), and we documented a greater number of supportive statements made in WRG than GDC (Greenfield et al., 2013b). Although in this Stage II trial there were no differences between WRG and GDC in average number of participants per group session, treatment attendance, and turn-over, similar to other open enrollment group therapy studies, the Stage II trial of WRG was challenged to provide a robust and stable group attendance (average group ≤ 3 participants for both WRG and GDC; Greenfield et al., 2014). It is possible that differences between the Stage I and Stage II trial results may in part be due to fewer average participants per group and lower stability of attendance in the Stage II trial. The smaller average group size and lack of participant stability in the Stage II versus Stage I trials may have affected the WRG women’s experience of mutual support that is a major effective component of the WRG (Greenfield et al., 2013a). Even with this change, outcomes of the WRG implemented in the open enrollment group format were comparable to GDC.
The Stage II trial demonstrates that the WRG was comparable to mixed-gender GDC in an open-enrollment format delivered in two community-based clinical settings (Greenfield et al., 2014). Our sample differs in certain demographic characteristics typical of some women seeking treatment in the community (SAMHSA, 2012), insofar as our participants were predominately white, attained higher educational status, and were more affluent. However, it is important to note that this is the first empirically supported group therapy for women with substance use disorders who have a range of other co-occurring psychiatric disorders, with or without trauma histories, who are at diverse stages of life with respect to age, parenting and marital status (Greenfield et al., 2007a). These clinical and demographic characteristics are also typical characteristics of women seeking treatment in the community (SAMHSA, 2012). Group therapy in outpatient community settings can provide cost-effective treatment for women with SUDs (Weiss et al., 2004). The results of this study provide evidence that the manual-driven WRG can be replicated and disseminated as a single-gender group therapy for women in substance abuse treatment programs. It is notable that therapists delivering both treatments were provided weekly supervision and were highly adherent to each treatment model. Consideration of enhancing provider training and supervision in routine practice may be warranted to deliver adherent and effective group behavioral treatments (Carroll et al., 2010).
Qualitative studies of women with SUDs indicate that women often prefer all-women’s treatment (Kauffman et al., 1995; Nelson-Zlupko et al., 1996) and patient preference has been demonstrated to be strongly correlated with clinical outcomes in a range of treatments (Swift and Callahan, 2009). In this study, we did not assess women’s preference for single-gender treatment pre-randomization. In fact, the study was advertised as an “investigational group therapy” with no mention of single-gender treatment so that preference for single-gender treatment would not be a factor in subject recruitment or study inclusion. However, we administered a group overview questionnaire at the end of treatment to assess satisfaction. Women were asked about the helpfulness of having only women in the group and covering women-specific issues on a scale of 0 to 4 (0 = “not at all helpful”; 4 = “extremely helpful”). Women in the WRG reported scores between “extremely helpful” and “very helpful” with regard to having a single-gender group composition (M = 3.3, SD = 0.8) and covering gender-specific issues in the group (M = 3.4, SD = 0.8). They also rated the coverage in the WRG of women’s issues and substance abuse issues as equally important.
The WRG provides education, discussion of relapse prevention, and skills practices to help women identify the way in which clinically significant issues for women with SUDs such as domestic violence and abuse, reproductive health, and family and partner concerns play a role in relapse risk and to problem-solve managing these risks in the course of recovery. The WRG provides an effective single-gender, women-focused group therapy component of treatment that can be delivered in the context of mixed-gender outpatient, partial, or residential treatment. The WRG increases the therapeutic options for women with SUDs; it is a replicable, manual-based group therapy for women with women-focused content that can be implemented in an open-enrollment format in a variety of clinical settings for women who are heterogeneous with respect to their substance of abuse, other co-occurring psychiatric disorders, and life-stage.
Acknowledgments
Role of funding source
Support for this study was provided by the National Institute on Drug Abuse grants R01 DA015434, K24 DA019855, and U10 DA015831 to McLean Hospital. NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Contributors
All authors had substantial contributions to the conception and design, or the analysis and interpretation of data; made substantial contributions to drafting the article or reviewing for critical content; and all authors have approved the final manuscript.
Conflict of interest
Dr. Bailey provides the following disclosures: Dr. Bailey’s institution has received grant support from NIDA, Titan Pharmaceuticals, Inc., Alkermes, Inc., BioDelivery Sciences International, Inc. and Orexo. Dr. Bailey has received travel support from Titan Pharmaceuticals, Inc. and is on the advisory boards of Braeburn Pharmaceuticals, BioDelivery Sciences International, Inc. and Camurus AB. All other authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bride BE. Single-gender treatment of substance abuse: Effect on treatment retention and completion. Soc Work Res. 2001;25:223–232. [Google Scholar]
- Carroll KM, Martino S, Rounsaville BJ. No train, no gain? Clin Psychol. 2010;17:36–40. [Google Scholar]
- Carroll KM, Onken LS. Behavioral therapies for drug abuse. Am J Psychiatry. 2005;162:1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, Muenz LR, Thase ME, Weiss RD, Gastfriend DR, Woody GE, Barber JP, Butler SF, Daley D, Salloum I, Bishop S, Najavits LM, Lis J, Mercer D, Griffin ML, Moras K, Beck AT. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry. 1999;56:493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Daley DC, Mercer D, Carpenter G. Group Drug Counseling for Cocaine Dependence. United States Department of Health and Human Services (USDHHS); Rockville, MD: 2002. [Google Scholar]
- Fiorentine R, Hillhouse MP. Drug treatment effectiveness and client-counselor empathy. J Drug Issues. 1999;29:59–74. [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln MF, Hien D, Miele GM. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007a;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Crisafulli MA, Kaufman JS, Freid CM, Bailey GL, Connery HS, Rapoza M, Rodolico J. Implementing substance abuse group therapy clinical trials in real-world settings: challenges and strategies for participant recruitment and therapist training in the Women’s Recovery Group Study. Am J Addict. 2014;23:197–204. doi: 10.1111/j.1521-0391.2014.12099.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Cummings AM, Kuper LE, Wigderson SB, Koro-Ljungberg M. A qualitative analysis of women’s experiences in single-gender versus mixed-gender substance abuse group therapy. Subst Use Misuse. 2013a;48:772–782. doi: 10.3109/10826084.2013.787100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Kuper LE, Cummings AM, Robbins MS, Gallop RJ. Group process in the single-gender women’s recovery group compared with mixed-gender group drug counseling. J Groups Addict Recover. 2013b;8:270–293. doi: 10.1080/1556035X.2013.836867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Pirard S. Gender-specific treatment for women with substance use disorders. In: Brady KT, Back SE, Greenfield SF, editors. Women and Addiction: A Comprehensive Handbook. Guilford Press; New York, NY: 2009. [Google Scholar]
- Greenfield SF, Trucco EM, McHugh RK, Lincoln MF, Gallop R. The Women’s Recovery Group Study: a Stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug Alcohol Depend. 2007b;90:39–47. doi: 10.1016/j.drugalcdep.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE. From generic to gender-responsive treatment: changes in social policies, treatment services, and outcomes of women in substance abuse treatment. J Psychoactive Drugs Suppl. 2008;5:327–343. doi: 10.1080/02791072.2008.10400661. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Bucholz KK, Rice JP, Bierut LJ. Secular trends in the lifetime prevalence of alcohol dependence in the United States: a re-evaluation. Alcohol Clin Exp Res. 2008;32:763–770. doi: 10.1111/j.1530-0277.2008.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opioid-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Depend. 2004;74:265–272. doi: 10.1016/j.drugalcdep.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, El-Guebaly N, Addington J. Treatment of substance abusers: single or mixed gender programs? Addiction. 1997;92:805–812. [PubMed] [Google Scholar]
- Kaskutas LA, Zhang L, French MT, Witbrodt J. Women’s programs versus mixed-gender day treatment: results from a randomized study. Addiction. 2005;100:60–69. doi: 10.1111/j.1360-0443.2005.00914.x. [DOI] [PubMed] [Google Scholar]
- Kauffman E, Dore MM, Nelson-Zlupko L. The role of women’s therapy groups in the treatment of chemical dependence. Am J Orthopsychiatry. 1995;65:355–363. doi: 10.1037/h0079657. [DOI] [PubMed] [Google Scholar]
- Kelly AB, Halford WK, Young RM. Maritally distressed women with alcohol problems: the impact of a short-term alcohol-focused intervention on drinking behaviour and marital satisfaction. Addiction. 2000;95:1537–1549. doi: 10.1046/j.1360-0443.2000.951015378.x. [DOI] [PubMed] [Google Scholar]
- Kominars K, Dornheim L. Group approaches in substance abuse treatment. In: DeLucia-Waack JL, Gerrity DA, Kalodner CR, Riva MT, editors. Handbook of Group Counseling and Psychotherapy. Sage Publications Ltd; Thousand Oaks, CA: 2004. pp. 563–675. [Google Scholar]
- Linehan MM, Schmidt H, III, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE. Relational psychotherapy mothers’ group: a developmentally informed intervention for at-risk mothers. Dev Psychopathol. 2000;12:235–253. doi: 10.1017/s0954579400002078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, O’Brien CP. A new measure of substance abuse treatment. Initial studies of the treatment services review. J Nerv Ment Dis. 1992a;180:101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992b;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Messina N, Grella CE, Cartier J, Torres S. A randomized experimental study of gender-responsive substance abuse treatment for women in prison. J Subst Abuse Treat. 2010;38:97–107. doi: 10.1016/j.jsat.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan-Lopez AA, Fals-Stewart W. Analytic complexities associated with group therapy in substance abuse treatment research: problems, recommendations, and future directions. Exp Clin Psychopharmacol. 2006;14:265–273. doi: 10.1037/1064-1297.14.2.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan-Lopez AA, Fals-Stewart W. Analyzing data from open enrollment groups: current considerations and future directions. J Subst Abuse Treat. 2008;35:36–40. doi: 10.1016/j.jsat.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits L, Weiss R, Shaw S, Muenz L. “Seeking safety:” outcome of a new cognitive-behavioral psychotherapy for women with postttraumatic stress disorder and substance dependence. J Trauma Stress. 1998;11:437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Nelson-Zlupko L, Dore M, Kauffman E, Kaltenbach K. Women in recovery: their perceptions of treatment effectiveness. J Subst Abuse Treat. 1996;13:51–59. doi: 10.1016/0740-5472(95)02061-6. [DOI] [PubMed] [Google Scholar]
- Orwin RG, Francisco L, Bernichon T. Effectiveness Of Women’s Substance Abuse Treatment Programs: A Meta-Analysis. Center for Substance Abuse Treatment. Substance Abuse and Mental Health Services Administration; Arlington, Virginia: 2001. [Google Scholar]
- Piazza NJ, Vrbka JL, Yeager RD. Telescoping of alcoholism in women alcoholics. Int J Addict. 1989;24:19–28. doi: 10.3109/10826088909047272. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Coombs DW, Lowe JB, Peterson PL, Gayoso E. Evaluation of a self-help program to reduce alcohol consumption among pregnant women. Int J Addict. 1995;30:427–443. doi: 10.3109/10826089509048735. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: getting started and moving on from stage I. Clin Psychol. 2001;8:133–142. [Google Scholar]
- Sobell LC, Sobell MB, Litten RZ, Allen JP. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Humana Press; Totowa, NJ: 1992. Timeline Follow-Back: A Technique For Assessing Self-Reported Alcohol Consumption; pp. 41–72. [Google Scholar]
- Sterling RC, Gottheil E, Weinstein SP, Serota R. Therapist/patient race and sex matching: treatment retention and 9-month follow-up outcome. Addiction. 1998;93:1043–1050. doi: 10.1046/j.1360-0443.1998.93710439.x. [DOI] [PubMed] [Google Scholar]
- Stinchfield R, Owen PL, Winters KC. Group therapy for substance abuse: a reveiw of the empirical research. In: Fuhriman A, Burlingame GM, editors. Handbook of Group Psychotherapy: An Empirical and Clinical Synthesis. John Wiley & Sons; New York: 1994. pp. 458–488. [Google Scholar]
- SAMHSA. Addressing the Specific Needs of Women. Treatment Improvement Protocol (TIP) Series, No. 51. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. [Google Scholar]
- SAMHSA. Treatment Episode Data Set (TEDS): 2000–2010. National Admissions to Substance Abuse Treatment Services. Center for Behavioral Health Statistics and Quality; Rockville, MD: 2012. DASIS Series S-61, HHS Publication No (SMA) 12-4701. [Google Scholar]
- Swift JK, Callahan JL. The impact of client treatment preferences on outcome: a meta-analysis. J Clin Psychol. 2009;65:368–381. doi: 10.1002/jclp.20553. [DOI] [PubMed] [Google Scholar]
- Tang Z, Claus RE, Orwin RG, Kissin WB, Arieira C. Measurement of gender-sensitive treatment for women in mixed-gender substance abuse treatment programs. Drug Alcohol Depend. 2012;123:160–166. doi: 10.1016/j.drugalcdep.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washton AM. Group therapy with outpatients. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, editors. Substance Abuse: A Comprehensive Textbook. 4. Lippincott Williams & Wilkins; 2005. pp. 671–679. [Google Scholar]
- Weiss RD, Griffin ML, Najavits LM, Hufford C, Kogan J, Thompson HJ, Albeck JH, Bishop S, Daley DC, Mercer D, Siqueland L. Self-help activities in cocaine dependent patients entering treatment: results from the NIDA collaborative cocaine treatment study. Drug Alcohol Depend. 1996;43:79–86. doi: 10.1016/s0376-8716(96)01292-6. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Jaffee WB, de Menil VP, Cogley CB. Group therapy for substance use disorders: what do we know? Harv Rev Psychiatry. 2004;12:339–350. doi: 10.1080/10673220490905723. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (CIDI): Core Version 2.1. World Health Organization; Geneva, Switzerland: 1997. [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) McLean Hospital; Belmont, MA: 1996. [Google Scholar]