Abstract
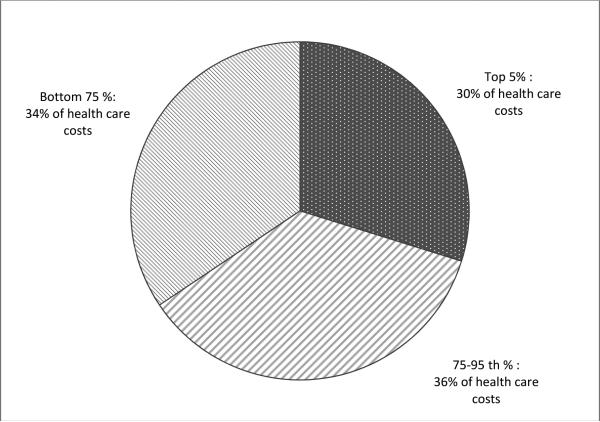
The aim of this study was to assess the economic cost of chronic pain among adolescents receiving interdisciplinary pain treatment. Information was gathered from 149 adolescents (ages 10-17) presenting for evaluation and treatment at interdisciplinary pain clinics in the United States. Parents completed a validated measure of family economic attributes, the Client Service Receipt Inventory, to report on health service use and productivity losses due to their child's chronic pain retrospectively over 12 months. Health care costs were calculated by multiplying reported utilization estimates by unit visit costs from the 2010 Medical Expenditure Panel Survey. The estimated mean and median costs per participant were $11,787 and $6,770 respectively. Costs were concentrated in a small group of participants, the top 5 % of those patients incurring the highest costs accounted for 30 % of total costs while the lower 75 % of participants accounted for only 34 % of costs. Total costs to society for adolescents with moderate to severe chronic pain were extrapolated to $19.5 billion annually in the U.S. The cost of childhood chronic pain presents a substantial economic burden to families and society. Future research should focus on predictors of increased health services use and costs in adolescents with chronic pain.
Perspective
This cost of illness study comprehensively estimates the economic costs of chronic pain in a cohort of treatment-seeking adolescents. The primary driver of costs was direct medical costs followed by productivity losses. Because of its economic impact, policy makers should invest resources in the prevention, diagnosis, and treatment of chronic pediatric pain.
Keywords: Chronic pain, adolescents, cost of illness, economic cost
Introduction
Moderate to severe chronic pain affects approximately 5 % of children and adolescents.12 As a group, children and adolescents with chronic pain seek more medical care, use more medications, miss more school and report worse quality of life relative to their peers without pain.12, 16 The societal economic costs of chronic pain are well-established for adult populations. A recent Institute of Medicine report estimated the economic burden of chronic pain to society from health care costs and lost work productivity to be over $600 billion annually.14 In contrast, the societal cost of pediatric chronic pain is not well-defined, despite recognition that pediatric chronic pain frequently occurs and is associated with economic consequences on the healthcare system and on families (e.g., parental lost work productivity). Because between 35% to 73% of children and adolescents with chronic pain are at risk for progressing into adulthood with chronic pain, it is important to consider the economic burden over a lifetime horizon.3, 5, 38
Relatively little is known about the costs of chronic pain in childhood and adolescence, although economic factors have been identified as an important outcome domain to measure in pediatric chronic pain clinical trials.20 Epidemiological studies have reported increased rates of health services use by children with chronic pain in Europe and Asia.19, 26, 37 For example, Perquin et al. (2000) found high rates of physician consultation (57%) and medication use (39%) in a community sample of children with chronic pain in the Netherlands.26 Small single-site investigations have also reported on high rates of physician consultation. Toliver-Sokol et al. (2011) found that in a sample of youth seeking care for chronic pain in an interdisciplinary U.S. pain clinic, 79.7% consulted health care providers, and 72.9% received prescribed medications for pain over the previous 6-month period. The mean number of health care visits over 6 months incurred by participants in this study were 19.63 (SD=16.87).31 While these studies confirm high rates of health care use, they do not provide estimates of costs associated with health care use.
To our knowledge, only two published studies have reported on the economic costs of pediatric chronic pain. In a small cohort of 52 youth with both inflammatory type (arthritis) and noninflammatory type chronic pain, Sleed et al. estimated the mean annual cost per adolescent with chronic pain for the United Kingdom's National Health System (NHS) at approximately $16,400 (2012 dollars). 21, 30 In another small cohort study, Ho et al. reported that children being treated with chronic pain in one interdisciplinary clinic incurred health care charges of $1,760 for outpatient visits and $7,020 for inpatient admissions over a previous 3-month period.11 These two studies were limited by their small sample sizes and inclusion of youth at a single pain clinic, which limits generalizability to other youth with pain in the US health care system.
To address these limitations in prior research, we aimed to conduct a cost of illness study with a larger, heterogeneous sample of adolescents with chronic pain being evaluated and treated at interdisciplinary pain clinics from across the United States. The goal of this study was to identify and describe the economic costs incurred by families of adolescents with idiopathic chronic pain. We sought to capture the main components of economic costs to society due to pain: (a) direct medical costs incurred by adolescents, (b) out of pocket costs incurred by parents, and (c) work productivity losses incurred by parents. We hypothesized that costs would be comparable to those incurred by youth with other chronic medical conditions. In addition, similar to findings in adults with chronic pain, we expected that a minority of patients would account for a large proportion of the total costs.28
Methods
This study was approved by the Institutional Review Board at Seattle Children's Hospital. Families were recruited as part of an ongoing randomized controlled trial investigating the efficacy of a web-based cognitive behavioral therapy program for chronic pain (clinicaltrials.gov: NC01316471).22 Participants were a convenience sample who presented for initial evaluation and treatment of chronic pain to one of eleven collaborating pediatric pain treatment centers located in the United States. All of these eleven pediatric pain treatment centers provided adolescents with coordinated and comprehensive pain evaluation and management that would meet the International Association for the Study of Pain's definition of interdisciplinary/multidisciplinary pain centers. 13 Participants received an interdisciplinary evaluation consisting of at least an evaluation by a pain physician, psychologist, and physical therapist, and also sometimes including nursing, rehabilitation medicine, social work, and psychiatry. Baseline data obtained prior to randomization to treatment conditions are included in this report.
Participants
Participants included adolescents who (a) were ages 10-17, (b) had idiopathic chronic pain of at least 3 months duration, (c) had pain occurring at least 1 time per week that interfered with daily functioning, and (d) did not have serious comorbid conditions (e.g., arthritis, cancer, diabetes). Idiopathic chronic pain was defined as chronic pain not associated with an identifiable underlying disorder that could reasonably explain their symptoms (for example we excluded participants with chronic pain due to arthritis, cancer, and sickle cell disease). Study participation required completion of web-based questionnaires in English for both adolescents and parents, and thus participants were also excluded if they (a) were non-English speaking, (b) had no Internet access, or (c) had developmental disabilities. One hundred and ninety four families were eligible for enrollment, however 45 declined, resulting in an overall enrollment rate of 77 %.
Procedure
After the adolescent's initial evaluation in the pain clinic, providers (physicians, psychologists, and nurses) at collaborating centers used a web-based system to submit referrals of potentially eligible and interested families. The study coordinator screened potential participants by phone for eligibility. Written consent was obtained from parents, and written assent from adolescents. Following receipt of consent, the study coordinator then set up password protected access for participants to the web-based program for data collection. Adolescents completed a daily pain diary for 7 days. Parents completed measures about family sociodemographics and health services use. Participants were compensated for their time with gift cards following the completed assessment.
Measures
Sociodemographic characteristics
Parents completed a background questionnaire assessing participants’ age, gender, racial and ethnic background, annual household income, caregiver educational level, and family structure. We used Rural-Urban Continuum Codes from the U.S. Department of Agriculture to determine the degree of urbanization of participant's primary residences (metropolitan versus non-metropolitan area) and Census Regions from the U.S. Census Bureau to determine which geographical area participants resided in. 32, 34
Pain characteristics
Adolescents prospectively reported daily pain intensity on an 11-point numeric rating scale (NRS) with anchors of 0 reflecting no pain and 10 reflecting worst possible pain using a 7-day online diary. Mean pain intensity over 7 days was used in analyses. Adolescents reported their primary location of pain, which were condensed to four categories (headache, abdominal, musculoskeletal, and multiple locations) for analysis.
Economic costs
Standard cost of illness methodology was conducted using a measure of economic costs, the Client Service Receipt Inventory (CSRI). 17 The CSRI is a validated research instrument that retrospectively measures health service use, social service use, out of pocket costs, informal care and lost employment.23 It has been used as a measure of economic costs in numerous studies examining resource use and costs associated with mental and physical disease.2, 15 The CSRI was adapted for adolescents with chronic pain by Sleed et al. (2005) and has subsequently been used in both adult and pediatric pain populations.7, 30
Parents completed an online version of the CSRI to collect retrospective data on economic costs incurred for their child's pain condition over the preceding 12 months. Parents were chosen as proxy reporters of their adolescents’ health care utilization, as parents have been shown to be reliable informants for this purpose. 36 Parents reported on the type and quantity of health services used. These included hospitalizations, emergency department visits, ambulatory health provider visits, medications, diagnostic testing and selected nonmedical social service provider visits. Data on hospitalizations included number of admissions and length of stay. Emergency department visit data included the number of visits. Ambulatory health provider visits included data on the type and frequency of visits. Medication data included type, quantity, and frequency of drugs used. Diagnostic test data included data on type and quantity of tests performed. Direct nonmedical costs included families’ out of pocket costs for transportation to medical appointments, special foods and supplements, special medical equipment, employing others to provide assistance for various tasks (e.g., domestic, educational), and other out of pocket costs. Parents directly recorded average annual amount spent on these items.
Productivity losses, also sometimes referred to as indirect costs, were also assessed. These losses represent a distinct aspect of disease-related costs and have two main components: productivity losses due to parents’ time off work and loss of leisure time due to providing informal care to the child with pain.
Computation of costs incurred
In order to better estimate costs, we assigned monetary values to health resources use and productivity time loss data from the CSRI.
Direct medical costs were estimated by linking health service use data obtained from the CSRI with nationally representative data on health service unit costs. National rather than regional costs were used to improve the generalizability of our findings. Unit costs for hospital admissions, emergency department, ambulatory health care visits, and diagnostic test costs were derived from the 2010 Medical Expenditure Panel Survey (MEPS). MEPS is a survey of noninstitutionalized U.S. families and individuals, and their health care providers intended to provide nationally-representative estimates of health care utilization, costs, payment sources and insurance coverage. MEPS provides data on the specific health services that American children and adolescents use and how much each of these services cost. To calculate costs for a MEPS participant receiving a medical service, we used the total expenditure variable, including costs paid by insurance, out-of-pocket, or by other sources. We did not consider costs for services that did not involve face-to-face contact with a service provider (e.g., phone consultations), or visits that resulted in zero costs. We calculated mean and median costs associated with a service for all MEPS participants aged 10-17, when at least 10 participants in this age group received the service in 2010. If fewer than 10 participants received the service, we calculated costs for all MEPS participants aged 10 - 64. All mean cost values were calculated using MEPS survey weights. Unit costs for medications were obtained using the 2010 lowest manufacturer's Average Wholesale Price per pill, minus 20% from the 2010 Red book: Pharmacy's Fundamental Reference published by Thompson Medical Economics. 27 In the United States the Average Wholesale Price is a prescription drugs term referring to the average price at which drugs are purchased at the wholesale level. Because published Average Wholesale Prices are inflated relative to actual market prices for drugs we conservatively estimated drug costs by subtracting 20% from the Average Wholesale Price, a strategy that is consistent with methodology previously used when estimating drug costs.1 Unit costs for community and social services (lawyer, home health care, tutor, and special needs coordinator) were calculated based on mean hourly earnings for these professions (to indicate charges) obtained from the U.S. Bureau of Labor Statistics. 35
To monetize productivity losses we used the human capital method, the most common approach to calculate productivity costs. Parents reported the number of days absent from work over the previous 12 months. Lost productivity to the national economy was calculated by multiplying number of lost days by the mean hourly earnings of the U.S. full-time civilian workforce obtained from the U.S. Bureau of Labor Statistics, assuming an 8 hour work day.35 When partial missed days were reported, lost productivity estimates for those days were performed. The most recent estimate was in 2011 of $22.77 per hour. We also calculated the productivity costs of lost leisure time as a result of providing informal care to a child with pain. This is time lost by parents that could otherwise have been spent on leisure activities. Consistent with previous economic studies, we valued the time spend on informal care by parents as the average hourly wage of a U.S. worker, $22.77.18
Estimating the national cost of pediatric pain
Prevalence rates for pediatric chronic pain are available from a number of epidemiological studies. Given that our sample is treatment-seeking and includes those youth with more severe pain, we chose to use the estimate from Huguet et al. who found that 5% of youth have moderate to severe pain with disability.12 Recent data from the 2012 U.S. Census puts the U.S. adolescent population at 33.1 million.33 Therefore by multiplying the 5% prevalence rate by 33.1 million we estimate that 1.7 million adolescents suffer moderate-severe chronic pain. We then multiplied the mean cost of pain in our sample by 1.7 million children to estimate national costs of adolescent chronic pain.
Statistical Analysis
To address our aim of identifying economic costs incurred by youth with chronic pain being seen in interdisciplinary pain clinics, we used a cost-of-illness approach. All reported expenditures were inflated to 2012 dollars using the 2012 medical care component of the U.S. consumer price index and 2012 U.S. dollar to U.K pound purchasing power parity conversion factor .21, 35 Descriptive analysis, including means, medians, ranges, and proportions were performed using Stata v12 (Statacorp, College Station, Texas). We examined the distribution of all health service use and economic cost variables and found the data were significantly skewed. However, while reporting on median values would better represent the distribution of our data, we instead chose to report mean values to increase interpretability. This is consistent with previous literature and facilitates comparisons to other cost-of-illness studies.
Results
Sociodemographic and clinical characteristics
Sociodemographic and clinical characteristics of the study participants are summarized in Table 1. Participants included 149 adolescents ages 10 to 17 years (M=14.2 years, SD = 1.7) and their parents. The sample was predominantly female (72.5 %) and white, non-Hispanic (78.5 %). The majority of families (55.2 %) had an annual household income above $70,000. Most families lived in counties within metropolitan areas (87.2 %), and most were residing in the West (44.5 %) and Midwest (31.1 %) regions of the United States. The sample included both families living close to and remote from pain centers, the mean distance between participants’ primary residence and their pain clinic was 87.8 (SD=172.9) , ranging from 0.4 miles to 1192 miles.
Table 1.
Descriptive sociodemographic and selected clinical characteristics of sample.
| n (%) | |
|---|---|
| Age (years)(M/SD) | 14.2 (1.7) |
| Gender | |
| Female | 108 (72.5) |
| Male | 41 (27.5) |
| Child racial background | |
| White, non-Hispanic | 117 (78.5) |
| African American | 7 (4.7) |
| Hispanic | 6 (4) |
| Othera | 17 (11.4) |
| Not reported | 2 (1.3) |
| Annual household income | |
| < $ 29,999 | 24 (16.5) |
| $ 30,000-$69,999 | 41 (28.3) |
| > $ 70,000 | 80 (55.2) |
| Caregiver educational level | |
| High school or less | 18 (12.2) |
| Vocational school/some college | 41 (27.7) |
| College/graduate/professional degree | 89 (60.1) |
| Family structure | |
| Two parent family | 112 (76.2) |
| Single parent family | 35 (23.8) |
| Location of primary residenceb | |
| Urban, metropolitan | 129 (87.2) |
| Rural, non-metropolitan | 19 (12.8) |
| Geographic region of United Statesc | |
| West | 61 (44.5) |
| Midwest | 46 (31.1) |
| Northeast | 35 (23.7) |
| South | 6 (4) |
| Distance between primary residence and pain center (miles)(M/SD) | 87.8 (172.9) |
| Average pain intensity over 7 days (M/SD) | 5.97 (1.9) |
| Primary pain location | |
| Musculoskeletal | 63 (42.3) |
| Multiple locations | 53 (35.6) |
| Abdominal | 21 (14.1) |
| Headache | 12 (8.1) |
“Other” racial category includes American Indian, Alaskan native, bi-racial or multiracial among others.
Degree of urbanization based on Rural-Urban Continuum Codes from the Department of Agriculture.
Regional divisions used by the United States Census Bureau.
Adolescents most commonly complained of musculoskeletal pain (42.3 %), followed by pain in multiple locations (35.6 %), abdominal pain (14.1 %), and headaches (8.1 %). Average pain intensity over 7 recorded days from daily diaries was in the moderate-severe range at 5.97 (SD = 1.9).
Resource utilization and costs
Using the economic cost methodology described above, we estimated the total costs over the preceding 12 months for all participants in this sample to be $1,756,282. The largest proportion of costs (68%) was towards direct medical services, with smaller amounts to direct nonmedical costs and productivity losses (see Table 2.) The mean and median costs per participant were $11,787 (SD=15,809, range $242 - $125,149) and $6,770 (interquartile range $3,462 - $13,198) respectively.
Table 2.
Total and categorical costs of medical and nonmedical expenses.
| Costs $ (% of total costs) | Costs $ (% of total costs) | |
|---|---|---|
| Total costs | 1,756,282 (100) | |
| Total direct medical costs (health care services) | 1,194,911 (68) | |
| Physician | 327,088 (18.6) | |
| Mental health | 86,160 (4.9) | |
| Physical and occupational therapy | 101,663 (5.8) | |
| Complementary and alternative medicine | 51,686 (2.9) | |
| Other providers | 3,273 (0.2) | |
| Community services | 66,345 (3.8) | |
| Diagnostic tests | 58,409 (3.3) | |
| Medications | 69,772 (4) | |
| Emergency department | 192,808 (11) | |
| Hospital inpatient costs | 237,709 (13.5) | |
| Total direct nonmedical costs (out-of-pocket costs) | 159,083 (9.1) | |
| Transportation | 75,670 (4.3) | |
| Other | 83,413 (4.8) | |
| Total productivity losses | 402,289 (22.9) | |
| Time off work | 104,692 (6) | |
| Leisure time lost | 297,597 (17) |
As hypothesized, costs between participants varied widely. As shown in Figure 1, the individuals in the top 5% in terms of costs were responsible for 30% of the total costs (mean cost of $70,928). The top 25% was responsible for 66% of all costs (mean = $33,039). In contrast, the lower 75% of participants was only responsible for 34% of the total costs (mean= $5,868).
Figure 1.
Total health care costs distribution among participants.
Direct costs
Data summarizing direct medical costs are presented in Tables 2 and 3. Direct medical costs were primarily distributed among outpatient health service costs: physician, mental health, physical and occupational therapy, complementary and alternative medicine, community services and others (36% of total costs), hospital inpatient costs (13.5%), and emergency department visits (11%) with smaller proportions attributed to medications (4%) and diagnostic testing services (3.3%).
Table 3.
Direct medical costs.
| Health Service Category | Number using Service, n (%) | Mean Unit Cost ($)* | Mean Use /SD‡ | Range | Mean Cost/SD ($)‡ | Range |
|---|---|---|---|---|---|---|
| Physiciana | 141 (95) | 225.4 | 9.6/8.2 | (0-50) | 2195.2/2222 | (0-18794.7) |
| Primary Careb | 105(70) | 181.9 | 3.8/5.6 | (0-50) | 685.5/1046.8 | (0-9667) |
| Medical Specialtyc | 124 (83) | 209.3 | 4.4/4.9 | (0-28) | 935.8/1125.0 | (0-7600.1) |
| Surgical Specialty d | 51 (34) | 399.5 | 1.4/4.2 | (0-45) | 573.8/1749.7 | (0-18794) |
| Mental Healthe | 85 (57) | 138.7 | 4.2/8.3 | (0-53) | 578.3/1151.3 | (0-7992.2) |
| Physical and Occupational therapy | 43 (29) | 140.7 | 4.8/15 | (0-111) | 682.3/2132 | (0-15824.7) |
| Complementary and Alternative Medicinef | 58 (39) | 81.5 | 4.4/10.4 | (0-78) | 346.9/831.4 | (0-7102.2) |
| Other providersg | 4 (3) | 135.7 | 0.15/1.3 | (0-15) | 22/190.1 | (0-2243.3) |
| Diagnostic servicesh | 37 (25) | 389.3 | 0.8/2.4 | (0-23) | 392/1326.2 | (0-13655.8) |
| Community servicesi | 40 (27) | 67.2 | 5.2/20.1 | (0-182) | 445.3/2481.2 | (0-25696.1) |
| Medications | 137 (92) | 2.6 | 4/2.3 | (0-8) | 468.3/1239.4 | (0-8558) |
| Emergency Department | 67 (45) | 771.2 | 1.7/3.3 | (0-30) | 1294/2542.9 | (0-23136.9) |
| Hospital inpatient costsj | 25 (17) | 3385.2 | 1.2/5 | (0-53) | 1595.4/6041.8 | (0-53136.7) |
Mean unit cost for all sub-components of health service category
Mean service use and cost calculated for entire sample.
Physician visits includes all primary care, medical specialty and surgical specialty visits.
Primary Care Visits (Pediatrician, Family Practice, and Urgent Care)
Medical Specialty Visits (Pain physician, Rheumatology, Neurology, Gastroenterology, Cardiology, Allergy/immunology, Dermatology, Physical Medicine/rehab, Hematology, Nephrology, Endocrinology/metabolism, and Pulmonary)
Surgical Specialty Visits (Orthopedics, General surgery, Gynecology, Plastic surgery, Ophthalmology, Otorhinolaryngology, and Urology)
Mental Health Visits (Psychiatry/Psychiatrist, Psychologist, and Social Worker)
Complementary and Alternative Medicine Visits (Chiropracter, Acupuncturist, Massage Therapist, Homeopath, Naturopath, and Herbalist)
Other medical provider visits ( Dentist, Podiatrist, Nursing)
Diagnostic services received (X-rays, MRI, CT, Laboratory tests, Ultrasound, and EEG)
Community visits (District Nurse, Home health care, Home tutor, Special needs coordinator, Classroom specialist, Lawyer)
Hospital inpatient costs: mean use refers to number of nights spend in hospital
The most commonly used outpatient medical visits were physician consultations; these visits accounted for slightly over half (51.5%) of all direct medical costs. Adolescents visited medical specialists more commonly than primary care physicians or surgical specialists. For the whole sample, the most frequently visited medical specialty physicians were rheumatologists, gastroenterologists, and neurologists with 33, 30, and 27 visits respectively, with substantially fewer visits to the other medical specialties. Among surgical specialists, orthopedic surgeons (41 visits) were the predominant service used, with substantially fewer visits to other surgical specialties.
Slightly over half (57%) of participants used mental health services. Of the 55 participants using psychology services, 22 had a single visit to a psychologist, with the remainder of the sample having multiple visits. Twenty-one adolescents had at least one visit to a psychiatrist.
Physical therapy and occupational therapy services were used by slightly more than a quarter of participants (29%). The majority of adolescents visiting physical and occupational therapists (75%) made multiple visits.
Slightly over a third (39%) of participants visited complementary and alternative medicine (CAM) providers. In the whole sample, visits for acupuncture (37 visits) and chiropractor services (29 visits) were the most common CAM services used. However, participants also saw a wide range of other CAM providers including homeopaths, naturopaths, herbalists, and other (total of 80 visits in the sample).
Hospital admissions and emergency department visits were common. In the sample, 25 adolescents (17%) spent at least one night in hospital over the preceding 12 months. The mean number of nights per hospital stay among adolescents that were hospitalized was 3, with a range of 1 to 53 nights. The mean number of hospitalizations per adolescent for the whole sample was 1.2 (SD=5). Hospital inpatient expenditures amounted to $237,709, representing 19.8% of all direct medical costs and 13.5% of total costs.
Sixty-seven adolescents visited the emergency department and among these sixty seven the mean number of ED visits was 3.7 per adolescent. For the whole sample the mean number of visits per adolescent was 1.7 (SD = 3.3). Emergency department costs amounted to 16.1% of direct medical costs and 11% of all costs.
Diagnostic services, including imaging studies and lab work, accounted for only 3.3% of direct medical costs, however individual tests were expensive. Computed tomography (CT) and magnetic resonance imaging (MRI) scans, at a mean cost of $2,193.82 per scan were the most expensive diagnostic tests. Six patients incurred a total of 17 CT or MRI scans.
Data on out of pocket costs by family members are summarized in Table 4. Out of pocket costs for direct nonmedical costs comprised 8.6% of total costs.
Table 4.
Direct Nonmedical Costs
| Number using service, n (%) | Mean Cost /SD ($)‡ | Range | |
|---|---|---|---|
| Employing extra help | 14 (9) | 336.8/652.1 | (0-2400) |
| Transport | 53 (35.5) | 1427.7/4083.8 | (0-24000) |
| Special equipment | 28 (18.80 | 300.1/854.9 | (0-3600) |
| Special food and supplements | 42 (28.2) | 1089.8/2179.3 | (0-12000) |
| Other | 14 (9) | 164.6/800.2 | (0-6000) |
Mean cost calculated for entire sample.
Productivity losses
Productivity losses, also referred to as indirect costs, comprised 22.9% of total costs. Data on productivity losses by families are summarized in Table 5. Adolescent pain had a significant impact on family members’ employment amounting to an average of 7 days off work per family (mean cost per family = $1,260). Lost employment was incurred by mostly mothers (53%), fathers (15.5%) or both (12.7%); however, some grandparents (5.6%), and other family members (13%) also took time off work. In addition, 3 parents stopped working entirely due to their child's pain and one parent took an extended leave of absence from work to care for the adolescent.
Table 5.
Productivity losses: time off work and leisure time lost providing informal care at home.
| Mean annual costs($)(range)‡ | ||
|---|---|---|
| Time off work: | ||
| • Families taking time off work: n (%) | 83 (56 %) | $ 1261.35(0-10792.98) |
| • Mean/SD (range) number of days off work per family per year | 7/9 (1-60) | |
| Informal care at home | ||
| • Families helping at home: n (%) | 38 (26 %) | $ 7831.5 (0-116035.9) |
| • Mean (range) number of hours helping at home per year | 343.9 (0-5096) |
Mean cost calculated for entire sample.
The primary driver of productivity losses was informal care provided to adolescents. Families reported that they provided 343 hours of additional care per year on average. Families reported helping with a wide range of routine daily activities for the child with pain, including personal care (bathing, eating, and dressing), homework, household chores, and transportation.
Estimated national cost
By multiplying the mean cost incurred by this sample ($11,787) by the estimated 1.7 million adolescents with moderate to severe chronic pain in the U.S. we found the national cost of pediatric chronic pain to be approximately $19.5 billion dollars annually.
Discussion
Our objective in this study was to comprehensively describe the economic costs related to chronic pain in a cohort of adolescents presenting to interdisciplinary pain treatment centers located in the United States. Our results show that in this cohort the mean annual cost associated with chronic pain per participant was $11,787 and the median cost was $6,770.
Our findings are consistent with previous reports of high health service use in samples of adolescents with chronic pain. 26, 30 However, direct comparison of our findings to other studies are hindered by methodological differences in economic costs computation as well as differences in health service systems and cost structure. For example, Sleed et al. (2005) measured costs in a small cohort of 52 adolescents in the United Kingdom with chronic pain also using the CSRI to capture economic costs. They found the mean annual cost of adolescents in the U.K. presenting to a chronic pain clinic at $16,400 (converted to 2012 dollars), which is higher than our estimated mean of $11,787. Despite similar methodology, direct comparison between our study and Sleed et al. is limited by differences in the UK and USA health care systems. Moreover, the small single center cohort included in the Sleed study may have been biased toward those individuals incurring the highest costs.
Ho et al. (2008) described direct health care use and indirect burden in adolescents with chronic pain presenting to one interdisciplinary pain treatment center in the United States. This sample was very similar to ours and comprised 75 adolescents (M=14.5 years, SD = 2.5) of which 68% were girls. Parents reported numerous health care visits, including primary care physician visits (mean=1.77), specialist visits (mean=2.97), physical therapy visits (mean=3.42), and mental health care visits (mean=1.12) over the three months preceding their first pain clinic visit. They also reported substantial indirect costs with a mean of 4.11 days of employment missed by parents. However, it is difficult to directly compare our findings to those of Ho et al. because of methodological differences in the economic evaluation. Unlike our comprehensive cost-of-illness approach, Ho et al. did not report on out of pocket costs, nor did they assign costs to productivity losses by parents. Furthermore, instead of reporting on direct medical service costs, this study used patient charges as a proxy for costs and found mean charges to families of $1761.06 for outpatient visits and $7020.40 for inpatient visits. Because charges may bear little resemblance to costs after factoring in discounts, using charges as proxy may result in overestimation of economic burden. 6
Similar to findings in adults with chronic pain, we also found a wide variation in costs across patients and a small subset accounting for the majority of the total costs.28 The top quartile of patients accounted for 66 % of all costs; within this subset 5% of the patients accounted for 30 % of the total costs. In contrast, the bottom two quartiles accounted for only 12.5% of costs. Future research is needed to identify biopsychosocial factors that are associated with increased costs in patients, and to begin to consider optimal methods of resource allocation for very limited pain clinic services. As reported by Peng et al (2007), there is a dramatic shortage of specialized pain facilities that provide treatment to children and adolescents and thus resource allocation is a critical issue.25
It will also be important to understand patterns of economic costs over the course of the pediatric patient's evaluation and treatment of chronic pain. Because our study focused on retrospective reports of pain evaluation and treatment primarily in the time period before and including initial consultation in a specialized pain clinic, it is not known how health service use may be altered by treatment in an interdisciplinary pain clinic. Given the relatively low rates of mental health care and physical/occupational therapy visits as compared to physician specialist visits, it seems likely that the majority of our participants were engaged in extended evaluation with multiple physicians. Future research efforts should be directed at assessing whether interdisciplinary pain care alters patterns of health service use and economic costs, and will require longitudinal designs to address these important questions.25
Findings from our study highlight the substantial costs of childhood chronic pain to the nation. In community samples, an estimated 25 to 35% of children have chronic or recurrent pain whereas the subgroup who presents for evaluation and treatment in a specialized pain clinic is much smaller.12, 16 Although reasons for referral are not empirically documented, it is likely that a myriad of factors including the severity of the pain and extent of pain-related disability as well as access to care are among the most salient reasons. Huguet and colleagues graded children and adolescents with chronic pain into four groups based on severity of their symptoms and pain related disability.12 A subgroup of 5% were assigned to grades 3 and 4 and were moderately to severely disabled by their pain and had significantly higher pain related visits to a doctor, took more medications, and were absent from school more than those in grades 1 and 2. Our study patient population, which were a treatment-seeking group of youth with chronic pain, is likely quite similar, and we therefore used the 5% prevalence rate to estimate national costs. This prevalence rate is slightly lower than recent adult reports which range from 5-15% 8, 29.
Based on published studies and reports from the Centers for Disease Control, the costs of chronic pain mirrors or exceeds those of other common childhood conditions such as asthma and attention-deficit/hyperactivity disorder (ADHD). Using an estimated prevalence rate of 5% for ADHD, a U.S. adolescent population of 33.1 million adolescents, and mean annual costs between $12,005 and $17,458 in 2005 dollars, the annual societal cost of ADHD has been reported to be 24.5 to 35.7 billion dollars (2012 dollars).4, 24 Likewise, using an estimated prevalence rate of 9% and a mean cost of $791 per child in 2003 dollars found in prior studies, the annual societal cost of asthma can be estimated at $3 billion in 2012 dollars. 4, 39 Our finding that chronic adolescent pain costs $19.5 billion annually places the societal cost for chronic pain closer to ADHD, the most costly chronic health condition identified in children and adolescents. At present, there has been far greater research attention devoted to childhood asthma and ADHD, while pediatric chronic pain has been relatively neglected in regards to research funding and public health attention. Clearly, as emphasized in the IOM report, a priority needs to be placed on the prevention, care, education, and research directed toward chronic pain.14
Our findings should be interpreted in light of several study limitations including the potential for recall bias from parents reporting on health service use and indirect costs over a 12-month retrospective period. However, objective methods of data collection, like medical record review or diary keeping, have not been found to be more accurate than retrospective recall in other health utilization studies which supports our choice of measurement approach.10 Because a centralized system of records capturing all health service data does not currently exist in the United States, retrospective methods are widely used in health services research.
Another limitation of our study is that data on the duration of chronic pain among adolescent participants was not available. Our study was also limited by the data collection at a single time point. Longitudinal cohort studies, following adolescents with chronic pain over time with repeated measures are needed to provide economic data over the course of evaluation and treatment of pediatric chronic pain. Additionally it is important to interpret the generalizability of our findings in light of our sample being predominantly Caucasian, with high socioeconomic status and educational levels, which does not accurately reflect the composition of the United States adolescent population.33 Although it is a strength that we recruited from multiple pain centers, we included a convenience sample and cannot speak to referral patterns from each center for study participation. Thus, there may be selection bias which could limit generalizability to the broader population of adolescents with chronic pain presenting to interdisciplinary pain centers.
Health care in the United States is provided by many distinct organizations, including non-profit and for-profit private companies and the state and federal governments, and is also not guaranteed for all of its citizens. In comparison, health care in European countries, Canada and Australia are publically funded and universally guaranteed. Health care reform in the U.S. will also bring about changes in health systems that may alter costs in the future. Therefore, some of our findings, especially cost data, may not be generalizable, and highlights the dynamic nature of economic cost evaluations. On the other hand, data on health service use rather than specific costs may be more similar between countries and provide a better comparison of resource use. Therefore, stakeholders in other health care systems may combine our data on resource use with their own micro-costing methods to estimate economic costs.
Given the high level of economic burden associated with pediatric chronic pain, even a modest reduction in the prevalence or severity of chronic pain will result in substantial benefits at a population level. Increased efforts to prevent and effectively treat childhood chronic pain are urgently needed. There is preliminary evidence that intensive inpatient-based pain management treatment reduces health services use, parental work absenteeism and subjective financial burden on families of children with chronic pain.9 Future research should investigate the efficacy of a full range of other, less intensive outpatient interdisciplinary pain management interventions as well as remote treatment (e.g., internet and mobile based therapies) on economic outcomes for children with pain.
Acknowledgments
This project was partially supported by National Institutes of Health R01HD065180 (TP) and the first author (CG) was supported by National Institutes of Health Ruth L. Kirschstein National Research Service Award Institutional Research Training Grant T32GM086270 (TP).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
No conflict of interest to declare
References
- 1.Anastassopoulos KP, Chow W, Tapia CI, Baik R, Ackerman SJ, Biondi D, Kim MS. Economic study on the impact of side effects in patients taking oxycodone controlled-release for noncancer pain. J Manag Care Pharm. 2012;18:615–626. doi: 10.18553/jmcp.2012.18.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beecham J, Knapp M. Costing psychiatric interventions. Gaskell; London: 1992. [Google Scholar]
- 3.Brna P, Dooley J, Gordon K, Dewan T. The prognosis of childhood headache: a 20-year follow-up. Arch Pediatr Adolesc Med. 2005;159:1157–1160. doi: 10.1001/archpedi.159.12.1157. [DOI] [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention Available at: http://www.cdc.gov/ncbddd/adhd/data.html. Accessed October 3, 2013.
- 5.Fearon P, Hotopf M. Relation between headache in childhood and physical and psychiatric symptoms in adulthood: national birth cohort study. BMJ. 2001;322:1145. doi: 10.1136/bmj.322.7295.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96:102–109. doi: 10.7326/0003-4819-96-1-102. [DOI] [PubMed] [Google Scholar]
- 7.Gannon B, Finn DP, O'Gorman D, Ruane N, McGuire BE. The cost of chronic pain: An analysis of a regional pain management service in Ireland. Pain Med. 2013 doi: 10.1111/pme.12202. [DOI] [PubMed] [Google Scholar]
- 8.Harker J, Reid KJ, Bekkering GE, Kellen E, Bala MM, Riemsma R, Worthy G, Misso K, Kleijnen J. Epidemiology of chronic pain in Denmark and Sweden. Pain Res Treat. 2012;2012:371248. doi: 10.1155/2012/371248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hechler T, Ruhe AK, Schmidt P, Hirsh J, Wager J, Dobe M, Krummenauer F, Zernikow B. Inpatient-based intensive interdisciplinary pain treatment for highly impaired children with severe chronic pain: randomized controlled trial of efficacy and economic effects. Pain. 2014;155:118–128. doi: 10.1016/j.pain.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Heinrich S, Deister A, Birker T, Hierholzer C, Weigelt I, Zeichner D, Angermeyer MC, Roick C, Konig HH. Accuracy of self-reports of mental health care utilization and calculated costs compared to hospital records. Psychiatry Res. 2011;185:261–268. doi: 10.1016/j.psychres.2010.04.053. [DOI] [PubMed] [Google Scholar]
- 11.Ho IK, Goldschneider KR, Kashikar-Zuck S, Kotagal U, Tessman C, Jones B. Health care utilization and indirect burden among families of pediatric Patients patients with chronic pain. Journal of musculoskeletal pain. 2008;16:155–164. [Google Scholar]
- 12.Huguet A, Miro J. The severity of chronic pediatric pain: an epidemiological study. J Pain. 2008;9:226–236. doi: 10.1016/j.jpain.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 13.International Association for the Study of Pain Pain Treatment Services. Available at: http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1381 Accessed May 15th, 2014.
- 14.IOM (Institute of Medicine) Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. The National Academies Press; Washington, DC: 2011. [PubMed] [Google Scholar]
- 15.King's College London Client Service Receipt Inventory. Available at: http://www.kcl.ac.uk Accessed 11 December 2013.
- 16.King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152:2729–2738. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 17.Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. Pharmacoeconomics. 2011;29:653–671. doi: 10.2165/11588380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 18.Luce BR, Manning WG, Siegel JE, Lipscomb J. Estimating Costs in Cost-Effectiveness Analysis. Oxford University Press; New York: 1996. [Google Scholar]
- 19.Masiero S, Carraro E, Sarto D, Bonaldo L, Ferraro C. Healthcare service use in adolescents with non-specific musculoskeletal pain. Acta Paediatr. 2010;99:1224–1228. doi: 10.1111/j.1651-2227.2010.01770.x. [DOI] [PubMed] [Google Scholar]
- 20.McGrath PJ, Walco GA, Turk DC, Dowrkin RH, Brown MT, Davidson K, Eccleston C, Finley GA, Goldschneider K, Haverkos L, Hertz SH, Ljungman G, Palermo T, Rappaport BA, Rhodes T, Schecter N, Scott J, Sethna N, Svensson OK, Stinson J, von Bayer CL, Walker L, Weisman S, White RE, Zajicek A, Zeltzer L. Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. J Pain. 2008;9:771–783. doi: 10.1016/j.jpain.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Officer LH, Williamson SH. MeasuringWorth “Computing ‘Real Value’ Over Time With a Conversion Between U.K. Pounds and U.S. Dollars, 1774 to Present”. Available at: www.measuringworth.com/exchange/ Accessed 20 December 2013.
- 22.Palermo T. Internet intervention for adolescents with chronic pain. Available at: http://clinicaltrials.gov/ct2/show/NCT01316471 Accessed March 10, 2014.
- 23.Patel A, Rendu A, Moran P, Leese M, Mann A, Knapp M. A comparison of two methods of collecting economic data in primary care. Fam Pract. 2005;22:323–327. doi: 10.1093/fampra/cmi027. [DOI] [PubMed] [Google Scholar]
- 24.Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. J Pediatr Psychol. 2007;32:711–727. doi: 10.1093/jpepsy/jsm022. [DOI] [PubMed] [Google Scholar]
- 25.Peng P, Stinson JN, Choiniere M, Dion D, Intrater H, Lefort S, Lynch M, Ong M, Rashiq S, Tkachuk G, Veilette Y. Dedicated multidisciplinary pain management centres for children in Canada: the current status. Can J Anaesth. 2007;54:985–991. doi: 10.1007/BF03016632. [DOI] [PubMed] [Google Scholar]
- 26.Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, van Suijlekom-Smit LW, Passchier J, van der Wouden JC. Chronic pain among children and adolescents: physician consultation and medication use. Clin J Pain. 2000;16:229–235. doi: 10.1097/00002508-200009000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Red Book: Pharmacy's Fundmental Reference. 2010 edition Thomson Reuters; Montvale,NJ: 2010. [Google Scholar]
- 28.Raftery MN, Ryan P, Normand C, Murphy AW, de la Harpe D, McGuire BE. The economic cost of chronic noncancer pain in Ireland: results from the PRIME study, part 2. J Pain. 2012;13:139–145. doi: 10.1016/j.jpain.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 29.Raftery MN, Sarma K, Murphy AW, De la Harpe D, Normand C, McGuire BE. Chronic pain in the Republic of Ireland--community prevalence, psychosocial profile and predictors of pain-related disability: results from the Prevalence, Impact and Cost of Chronic Pain (PRIME) study, part 1. Pain. 2011;152:1096–1103. doi: 10.1016/j.pain.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 30.Sleed M, Eccleston C, Beecham J, Knapp M, Jordan A. The economic impact of chronic pain in adolescence: methodological considerations and a preliminary costs-of-illness study. Pain. 2005;119:183–190. doi: 10.1016/j.pain.2005.09.028. [DOI] [PubMed] [Google Scholar]
- 31.Toliver-Sokol M, Murray CB, Wilson AC, Lewandowski A, Palermo TM. Patterns and predictors of health service utilization in adolescents with pain: comparison between a community and a clinical pain sample. J Pain. 2011;12:747–755. doi: 10.1016/j.jpain.2010.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The US. Department of Agriculture: Rural-Urban Continuum Codes. Available at: http://www.ers.usda.gov Accessed 11 December 2013.
- 33.United States Census Bureau Population Estimates. Household Population. 7/1/2012-12/1/2012. Available at: http://www.census.gov/popest/data/national/asrh/2012/2012-nat-hh.html Accessed 1 January 2014.
- 34.United States Census Bureau Geography: Census Divisions and Census Regions. Available at: http://www.census.gov Accessed 11 December 2013.
- 35.United States Department of Labor Bureau of Labor Statistics: Consumer Price Index. Available at: http://www.bls.gov/cpi/ Accessed October 3, 2013.
- 36.Ungar WJ, Davidson-Grimwood SR, Cousins M. Parents were accurate proxy reporters of urgent pediatric asthma health services: a retrospective agreement analysis. J Clin Epidemiol. 2007;60:1176–1183. doi: 10.1016/j.jclinepi.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vila M, Kramer T, Obiols JE, Garralda ME. Abdominal pain in British young people: associations, impairment and health care use. J Psychosom Res. 2012;73:437–442. doi: 10.1016/j.jpsychores.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Walker LS, Dengler-Crish CM, Rippel S, Bruehl S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain. 2010;150:568–572. doi: 10.1016/j.pain.2010.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang LY, Zhong Y, Wheeler L. Direct and indirect costs of asthma in school-age children. Prev Chronic Dis. 2005;2:A11. [PMC free article] [PubMed] [Google Scholar]