Abstract
AIM
We assess the improvement in discrimination afforded by the addition thoracic aorta calcium (TAC), aortic valve calcification (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT) and liver attenuation (LA) to Framingham risk score(FRS) + coronary artery calcium (CAC) for incident CHD/CVD in a multi ethnic cohort.
Methods and Results
A total 5745(2710 were intermediate Framingham risk, 210 CVD and 155 CHD events) 251 had adjudicated CHD, 346 had CVD events, 321 died after 9 years of follow-up. Cox proportional hazard, receiver operator curve (ROC) and net reclassification improvement (NRI) analyses.
In the whole cohort and also when the analysis was restricted to only the intermediate risk participants: CAC, TAC, AVC and MAC were all significantly associated with incident CVD/CHD/ mortality; CAC had the strongest association. When added to the FRS, CAC had the highest area under the curve (AUC) for the prediction of incident CHD/CVD; LA had the least. The addition of TAC, AVC, MAC, PAT and LA to FRS + CAC all resulted in a significant reduction in AUC for incident CHD [0.712 vs. 0.646, 0.655, 0.652, 0.648 and 0.569; all p<0.01 respectively] in participants with intermediate FRS. The addition of CAC to FRS resulted in an NRI of 0.547 for incident CHD in the intermediate risk group. The NRI when TAC, AVC, MAC, PAT and LA were added to FRS + CAC were 0.024, 0.026, 0.019, 0.012 and 0.012 respectively, for incident CHD in the intermediate risk group. Similar results were obtained for incident CVD in the intermediate risk group and also when the whole cohort was used instead of the intermediate FRS group.
Conclusion
The addition of CAC to the FRS provides superior discrimination especially in intermediate risk individuals compared with the addition of TAC, AVC, MAC, PAT or LA for incident CHD/CVD. Compared with FRS + CAC, the addition of TAC, AVC, MAC, PAT or LA individually to FRS + CAC worsens the discrimination for incident CHD/CVD. These CT risk markers are unlikely to be useful for improving cardiovascular risk prediction.
Keywords: cardiac CT derived risk factors, coronary heart disease, cardiovascular events, risk prediction
Introduction
Cardiac computed tomography (CT) imaging is an important tool for cardiovascular risk assessment in observational prospective studies (1). From a single CT image acquisition without additional contrast agents, measures of subclinical disease such as coronary artery calcium (CAC), thoracic aorta calcium (TAC), aortic valve calcification (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT), and a measure of liver attenuation (LA) can be quantified, among others. CAC, TAC, AVC, MAC, and PAT have all been associated with cardiovascular events or risk factors (2–5). Despite no clear association between LA and cardiovascular events, recent data support an association between non alcoholic fatty liver disease and Framingham risk score (FRS) (6, 7).
Current data suggest that among the top tier novel cardiovascular risk markers that have shown independent association with cardiovascular events, CAC is superior for improving discrimination over and beyond the Framingham Risk Score and the Reynolds Score (RS) (8, 9). However a closer look at these data shows that even with the addition of CAC to the FRS/RS, a significant number of individuals are still misclassified. Thus there still remains a number of high risk asymptomatic individuals especially those classified as intermediate risk by the FRS, who would be reclassified to low risk by the addition of CAC to the FRS and who would go on to have clinical cardiovascular events(10). It remains unknown whether the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel IV) guidelines due to be released soon would have a stronger recommendation for CAC screening in individuals with intermediate FRS based on recent data. Even with a stronger recommendation for CAC screening in intermediate FRS, high risk individuals with no coronary artery calcification will be considered low risk; an approach which is not optimal. This fact calls for the addition of other markers to FRS + CAC to at least minimize the reclassification of high risk to low risk in the intermediate FRS category. The cost effectiveness of the addition of CAC to the FRS to improve discrimination has also received the much needed press in recent years. The addition of another novel marker to the FRS +CAC, with small or no additional cost, further testing or radiation exposure appears attractive and hence makes TAC, AVC, MAC, PAT or LA ideal candidates.
In this report, we explore the improvement in discrimination afforded by the addition of TAC, AVC, MAC, PAT, LA and a combination to a model containing FRS +CAC for incident cardiovascular events/ coronary heart disease events/ all- cause mortality among participants in the Multi Ethnic Study of Atherosclerosis (MESA).
Methods
Study Population and Data Collection
The study design for the MESA study has been published elsewhere (11). In brief, MESA is a prospective cohort study to investigate the prevalence, correlates, and progression of subclinical CVD in persons without known CVD at baseline. The full cohort includes 6,814 women and men ages 45 to 84 years without known CVD, recruited from 6 U.S. communities (Baltimore, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; northern Manhattan, New York; and St. Paul, Minnesota). Self-reported race/ethnicity was collected to explore the possible racial differences in the development and progression of atherosclerosis. The MESA cohort was 38% white, 28% African American, 22% Hispanic, and 12% Chinese.
Demographics, medical history, and anthropometric and laboratory data for the present study were gathered during the first examination of the MESA cohort (July 2000 to August 2002). Participants with diabetes were excluded from the present analysis because it is considered a CHD risk-equivalent. Diabetes was defined as self-reported history of diabetes mellitus, diabetes medication use or fasting glucose ≥126mg/dl. Current smoking was defined as having smoked a cigarette in the last 30 days. Use of antihypertensive and other medications was based on review of prescribed medication containers. Resting blood pressure was measured three times in the seated position, and the average of the second and third readings was recorded. Hypertension was defined as a systolic blood pressure of at least 140 mm Hg, diastolic blood pressure of at least 90 mm Hg, or use of medication prescribed for hypertension. Body mass index was calculated as weight (kg) divided by height (m2). Total cholesterol and high density lipoprotein cholesterol were measured from blood samples obtained after a 12-h fast. Low-density lipoprotein cholesterol was estimated by the Friedewald equation (12). The MESA study was approved by the Institutional Review Boards of each study site, and written informed consent was obtained from all participants. The MESA study complies with the declaration of Helsinki.
Measurement of Coronary Calcium Score
Details of the MESA CT scanning and interpretation methods have been reported by Carr et al (13). Scanning centers assessed coronary calcium by chest computed tomography (CT) with either a cardiac-gated electron-beam CT scanner (Chicago, Los Angeles, and New York field centers) or a multidetector CT system (Baltimore, Forsyth County, and St. Paul field centers). Certified technologists scanned all participants twice and results were compared to phantoms of known physical calcium concentrations. A radiologist or cardiologist read all CT scans at a central reading center (Los Angeles Biomedical Research Institute at Harbor–UCLA, Torrance, California). We used the mean Agatston score for the 2 scans in all analyses. Intraobserver and interobserver agreements were excellent (κ = 0.93 and κ = 0.90, respectively).
Measurement of Extra-Coronary Calcium Score (TAC, AVC, and MAC)
Details of the MESA CT scanning and interpretation methods for quantifying extra-coronary calcium were reported previously (14). All measurements of extra-coronary calcification used a computer-based three-dimensional reconstruction program (Rapidia; Infinite Co Ltd, Seoul, Korea). Extra-coronary calcium measures were scored using the Agatston method; single lesion measurements were summed to give an overall Agatston score. Inter- and intrareader variability data for all extra-coronary calcium measurements in MESA were reported previously (14).
Measurement of Pericardial Adipose Tissue Volume
Details of the MESA cardiac CT scanning and interpretation methods for quantifying pericardial adipose tissue volume have been reported previously (4). Briefly, experienced CT analysts measured pericardial fat volume on the previously obtained images of the heart. For pericardial fat volume, slices within 15 mm above and 30 mm below the superior extent of the left main coronary artery were included. This region was selected because it includes the pericardial fat located around the proximal coronary arteries (left main coronary, left anterior descending, right coronary, and circumflex arteries). The anterior border of the volume was defined by the chest wall and the posterior border by the aorta and the bronchus. Volume analysis software (GE Health Care, Waukesha, WI) was used to discern fat from other tissues with a threshold of −190 to −30 Hounsfield units. A randomly selected quality control sample (n= 80) demonstrated an intraclass correlation coefficients of intrareader and interreader reliability were 0.99 and 0.89, respectively, for pericardial fat volume.
Measurement of Liver Attenuation
Details of the MESA cardiac CT scanning and interpretation for quantifying liver attenuation have been published previously (15). Briefly, two readers measured the scans independently blinded to the demographic data. Both scans for each participant were examined and the one with large scan span was selected for measurement of liver fat. Hepatic Hounsfield unit (HU) attenuation values were measured using regions of interest (ROI) greater than 100 mm2 in area. There were two ROIs placed in the right liver lobe anterioposteriorly and one ROI in the left liver lobe. ROIs with larger areas were used, whenever possible, to include a greater area of the liver and spleen while excluding regions of non-uniform parenchymal attenuation, including hepatic vessels. LA was calculated by taking mean HU measurement of both right liver lobe ROIs. Inter-reader and intra-reader measurements were highly correlated (0.96 and 0.99, respectively).
Ascertainment of Incident CHD and Incident CVD
Cardiovascular events were adjudicated by a MESA study committee that included cardiologists, physician-epidemiologists, and neurologists. A detailed description of the CV event adjudication process has been published (16). Here, we defined incident CHD as myocardial infarction (MI), death due to CHD, resuscitated cardiac arrest, definite or probable angina followed by coronary revascularization, and definite angina not followed by coronary revascularization. We defined incident cardiovascular event as incident CHD, stroke, stroke death, or other CVD death as defined by the MESA protocol (www.mesa.nhlbi.org).
Statistical Analysis
Diabetes mellitus is considered a CHD equivalent and hence awarded a score of greater than 20% by the current ATP III guidelines. However the FRS awards specific risk which results in some diabetics being low risk, intermediate risk and high risk. To avoid any confusion in risk assignment especially in the Net Reclassification improvement calculation, we excluded diabetics in this analysis. The cohort was divided into low (<5%), intermediate (5 %≤ × >20%) and high (≥20) risk according to their FRS at baseline (17). Descriptive data of the cohort stratified by the FRS are presented as mean ± SD for continuous variables or frequencies of participants for categorical variables. CAC, TAC, AVC, and MAC were expressed as In(CAC+1), In(TAC+1), In(AVC +1), and In(MAC +1) respectively. Cox proportional hazard analysis was used to assess the association between each of the CT risk markers and incident CHD/CVD/ death adjusting for age, gender, race/ethnicity, systolic blood pressure, total cholesterol, HDL, smoking status, BMI, triglycerides, blood pressure medication use, and HMG CoA reductase inhibitor use. These covariates were chosen based outcomes of interest in the current analysis and prior published data.
Receiver operator curve analysis (ROC) was then used to assess the predictive accuracy of the FRS, CAC, TAC, AVC, MAC, PAT and LA for incident CHD/CVD. The estimate of the probability of the outcome for each individual was assessed using the method by Pencina et al (18). The potential for further improvement afforded by the addition of TAC, AVC, MAC, PAT and LA to the FRS +CAC was also explored in ROC analysis using the method by Delong et al (19). At the time of these analyses the mean observed follow-up in the MESA cohort was 7.5 years (median 7.6 years, maximum follow-up of 9 years). The FRS calculates a 10 year risk but our duration of follow up in this study was less than 10 years. To account for the actual duration of follow-up and to avoid extrapolation, we modeled the risk for CHD and CVD events using the FRS as covariate to generate predicted probabilities for the primary outcome among those classified as low, intermediate, and high risk by FRS (base model).
The absolute event rate cut points for the primary outcome between the 3 FRS risk categories were as follows: low, <3.2%; intermediate, 3.2% to 8.6%; high, >8.6% for incident CHD; and : low, <4.3%; intermediate, 4.3% to 12.2%; high, >12.2% for incident CVD. The absolute event rate cut points were the predicted probabilities corresponding to <5%, 5 %≤ × >20% and ≥20 FRS. We then used a similar model to generate predicted probability for the primary outcome (CHD/CVD) using FRS + CAC, FRS +CAC +TAC, FRS+CAC+AVC, FRS+CAC+MAC, FRS +CAC +PAT, FRS +CAC + LA and assigned subjects to low, intermediate, or high risk using the same cut points obtained from the base model. This approach allowed us to use comparable absolute event rates for the outcomes during the period of observation rather than extrapolating beyond actual observations. The Net Reclassification Improvement (NRI) was then calculated (20) for each combination.
Calibration which measures how closely the predicted probabilities of risk using these novel markers reflect observed risk was also assessed. We calculated the survival-adapted Hosmer-Lemeshow χ2 statistic for the models (21). P <0.05 represent a significant difference between the expected and observed event rates and suggest that the model is not well calibrated. The primary analysis was done using individuals classified as intermediate risk by the FRS and the repeated in the whole cohort. A 2-tailed value of P<0.05 was considered significant. All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC).
Results
Mean (SD) age, BMI, systolic blood pressure, total cholesterol, HDL, LDL, and triglycerides were 62.1(10.2) years, 28.4(5.4) Kg/m2, 126.7(21.4) mmHg, 194.2(35.7) mg/dl, 50.9(14.8) mg/dl, 117.3(31.4) mg/dl and 132.2(89.3) mg/dl respectively for the 5745 participants with complete data included in the analysis. After a maximum follow-up of 9 years, 251 CHD and 346 CVD events occurred and 321 died. The baseline characteristics of the 5745 MESA participants stratified by FRS status appear in Table 1.
Table 1.
Demographic Characteristics of Participants in the Multi-Ethnic Study of Atherosclerosis (MESA) Stratified by Baseline Framingham Risk Score (FRS)
| Variables | Low Risk (FRS ≤5%) N = 2656 (mean ± SD) |
Intermediate Risk (FRS 5–20%) N = 2710 (mean ± SD) |
High Risk (FRS ≥ 20%) N= 379 (mean ± SD) |
|---|---|---|---|
| Age (years) | 57.4 ±9.4 | 64.9 ±9.6 | 70.6 ±7.3 |
| Female Gender (%) | 2049 (77.2) | 987 (36.4) | 58(15.3) |
| Race/ Ethnicity (%) | |||
| Caucasian | 1115(41.9) | 1102(40.6) | 143(37.7) |
| Chinese | 315(11.8) | 306(11.2) | 36(9.5) |
| African American | 710(26.7) | 702(25.9) | 108(28.5) |
| Hispanic | 516(19.4) | 600(22.1) | 92(24.3) |
| Body Mass Index(Kg/m2) | 27.9 ± 5.8 | 28.2 ± 4.9 | 28.2 ±4.3 |
| Blood Pressure(mmHg) | |||
| Systolic | 117.1± 16.6 | 131.5 ±21.2 | 145.6 ± 21.8 |
| Diastolic | 68.7 ±9.5 | 74.2 ± 9.9 | 78.4±10.4 |
| Cholesterol (mg/dl) | |||
| Total | 190.6 ± 33.7 | 197.0 ±35.5 | 211.9 ±33.9 |
| LDL | 111.3 ± 29.4 | 122.0 ± 31.0 | 137.0 ± 28.3 |
| HDL | 57.4 ± 15.3 | 47.3 ± 12.9 | 41.8 ± 9.5 |
| Triglycerides | 109.6 ± 60.6 | 140.0± 86.7 | 165.2 ± 87.3 |
| Cigarette Smoking (%) | |||
| Never | 1559(59.1) | 1218(44.9) | 111(29.3) |
| Former | 904 (34.2) | 1060(39.1) | 132(34.8) |
| Current | 174 (6.7) | 432(16.0) | 136 (35.9) |
| BP medication use (%) | 619(23.3) | 957(35.2) | 146(38.5) |
| HMG CoA reductase use (%) | 324(12.2) | 400(14.7) | 40(10.5) |
| Pericardial Fat Volume(ml) | 64.0 ±32.4 | 87.7± 42.7 | 102.9 ±46.5 |
| Liver Attenuation (HU) | 61.1 ±10.6 | 59.9± 12.3 | 59.0± 10.1 |
| In( CAC + 1) | 1.2± 2.0 | 2.6 ± 2.6 | 4.1 ±2.5 |
| In( TAC +1) | 0.7± 1.9 | 1.9± 2.8 | 3.3 ±3.2 |
| In( MVC +1) | 0.3± 1.1 | 0.5 ± 1.5 | 0.9 ±2.0 |
| In( AVC + 1) | 0.2±0.9 | 0.7 ±1.6 | 1.3 ±2.2 |
| Framingham Risk Score (%) | 2.6 ± 1.3 | 9.9 ± 3.9 | 27.3± 7.2 |
HMG CoA indicates 3-hydroxy-3-methyl-glutaryl-CoA
Associations Between CT Risk Markers and Outcomes
As shown in Table 2, CAC, TAC, AVC, MAC and PAT were significantly associated with incident CHD/CVD/ death in univariate Cox proportional hazard analyses. In multivariable Cox models, CAC, AVC, and MAC were significantly associated with incident CHD/CVD/death, whereas TAC was significantly associated with CHD and death. PAT was significantly associated with death, but not CHD/CVD, in multivariable Cox models. LA was not significantly associated with incident CHD/CVD/death in multivariable Cox models. Similar associations were seen when the analysis was restricted to participants with intermediate Framingham risk or when stratified by race/ethnicity or gender (data not shown).
Table 2.
Association between CT cardiovascular risk markers and incident cardiovascular, coronary heart events and all-cause mortality after 9 years of follow-up in Cox proportional hazard models.
| CT Risk Marker | Outcome | Univariate | Multivariable** | ||
|---|---|---|---|---|---|
| Hazard Ratio(95% CI) | P value | Hazard Ratio(95% CI) | P value | ||
| CAC | CVD | 1.43(1.37 –1.50) | <0.0001 | 1.29(1.23 – 1.35) | <0.0001 |
| CHD | 1.50(1.42 – 1.58) | <0.0001 | 1.38(1.29 – 1.47) | <0.0001 | |
| Death | 1.26(1.22 – 1.33) | <0.0001 | 1.10(1.05 – 1.16) | 0.0002 | |
| TAC | CVD | 1.19(1.15 – 123) | <0.0001 | 1.04(0.99 – 1.08) | 0.097 |
| CHD | 1.18(1.13 – 1.23) | <0.0001 | 1.06 (1.00 – 1.11) | 0.033 | |
| Death | 1.24(1.20 – 1.28) | <0.0001 | 1.08(1.04 – 1.13) | 0.0003 | |
| AVC | CVD | 1.30(1.25 – 1.37) | <0.0001 | 1.11(1.05 – 1.16) | 0.0002 |
| CHD | 1.33(1.26 – 1.40) | <0.0001 | 1.14(1.08 – 1.21) | <0.0001 | |
| Death | 1.29(1.23 – 1.35) | <0.0001 | 1.11(1.06 –1.18) | <0.0001 | |
| MAC | CVD | 1.22(1.16 – 1.28) | <0.0001 | 1.08(1.03 – 1.14) | 0.003 |
| CHD | 1.20(1.14 – 1.28) | <0.0001 | 1.09( 1.02 – 1.16) | 0.009 | |
| Death | 1.29(1.23 – 1.35) | <0.0001 | 1.13 (1.07 – 1.19) | <0.0001 | |
| PAT* | CVD | 1.38(1.28 – 1.51) | <0.0001 | 1.06(0.94 –1.21) | 0.336 |
| CHD | 1.43(1.28 – 1.57) | <0.0001 | 1.08(0.93 – 1.24) | 0.316 | |
| Death | 1.31(1.20 – 1.43) | <0.0001 | 1.19(1.04 – 1.35) | 0.009 | |
| LA* | CVD | 0.91(0.81 – 0.97) | 0.061 | 0.92(0.81 – 1.03) | 0.156 |
| CHD | 0.89(0.79 – 1.00) | 0.050 | 0.92(0.80 – 1.06) | 0.244 | |
| Death | 1.00(0.90 – 1.12) | 0.993 | 0.91(0.80 – 1.04) | 0.175 | |
For continuous risk markers, HRs are standardized per unit standard deviation change in the marker.
Multivariable models adjusted for age, gender, race/ethnicity, systolic blood pressure, total cholesterol, HDL, smoking status, BMI, triglycerides, blood pressure medication use and HMG CoA reductase inhibitor use. CAC – coronary artery calcium, TAC – Thoracic aorta calcium, AVC – Aortic valve calcium, MAC – Mitral annular calcium, PAT – pericardial adipose tissue volume, LA- liver attenuation.
Improvement in Discrimination in Intermediate risk group (ROC analysis and Clinical NRI)
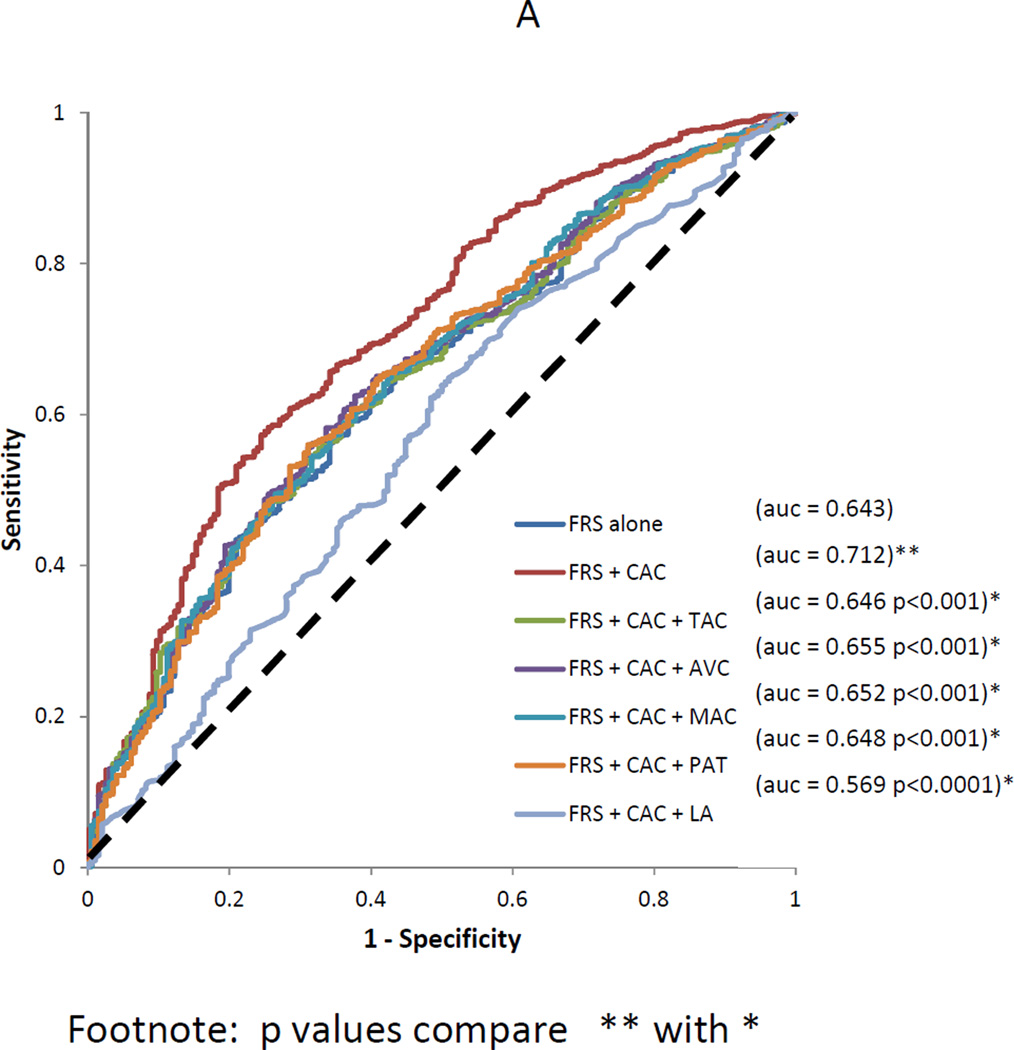
For the intermediate risk participants (N=2710, 210 CVD events and 155 CHD events), the addition of CAC to the FRS had an AUC of 0.712 for incident CHD, significantly higher than the improvement in AUC when TAC, AVC, MAC, PAT or LA is added to the FRS [0.645, 0.651, 0.643, 0.643 and 0.641 respectively]. The addition of TAC, AVC, MAC, PAT and LA individually to FRS + CAC resulted in significant reduction in AUC for incident CHD [0.712 vs. 0.646, 0.655, 0.652, 0.648 and 0.569 respectively](Figure 1A). The addition of CAC to the FRS had a clinical NRI of 0.547 for incident CHD. However, the addition of TAC, AVC, MAC, PAT and LA individually to FRS + CAC resulted in clinical NRI of 0.0236, 0.0258, 0.0187, 0.0124, and 0.0116, respectively, for incident CHD. The survival-adapted Hosmer-Lemeshow χ2 statistics was 8.42 (p=0.41) for FRS + CAC and was greater than 8.01 when TAC, AVC, MAC, PAT and LA was added to FRS + CAC (all P> 0.05) suggesting no significant lack of fit.
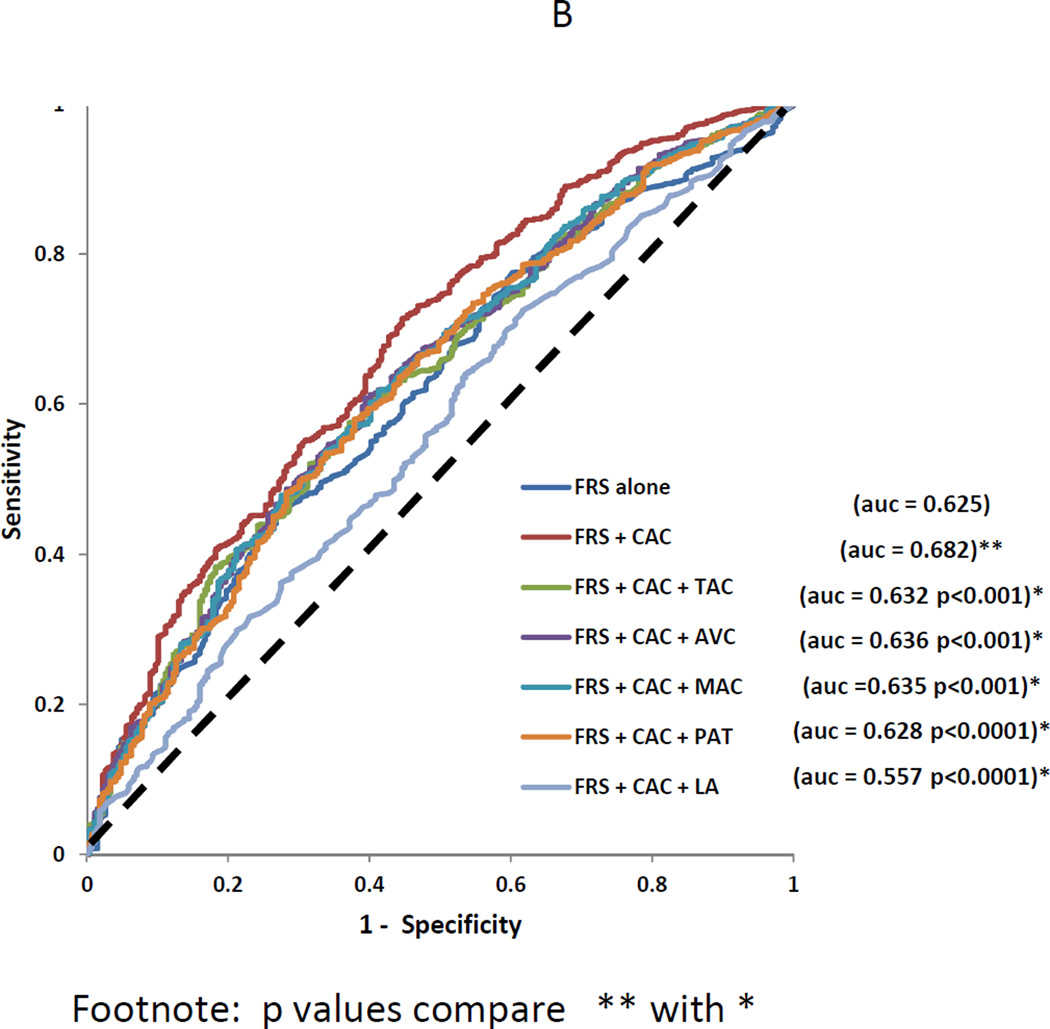
Figure 1.
A: Receiver operating characteristic curves showing the improvement of the area under the curve (AUC) after adding thoracic aorta calcium (TAC), aortic valve calcium (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT) and liver attenuation (LA) to the Framingham risk score and coronary calcium score (FRS +CAC) for incident coronary heart disease events in intermediate risk individuals in MESA.
B: Receiver operating characteristic curves showing the improvement of the area under the curve (AUC) after adding thoracic aorta calcium (TAC), aortic valve calcium (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT) and liver attenuation (LA) to the Framingham risk score and coronary calcium score (FRS +CAC) for incident cardiovascular disease events in intermediate risk individuals MESA.
The addition of TAC, AVC, MAC, PAT and LA individually to FRS + CAC resulted in a significant reduction in AUC for incident CVD [0.682 vs. 0.632, 0.636, 0.635, 0.628 and 0.557 respectively](Figure 1B). The addition of CAC to the FRS had a clinical NRI of 0.442 for incident CVD. The addition of TAC, AVC, MAC, PAT and LA individually to FRS +CAC resulted in a clinical NRI of 0.006, 0.030, 0.0130, 0.0037 and 0.0223 respectively for incident CVD. Similar results were obtained when the analysis was stratified by race/ethnicity or gender.
Improvement of Discrimination whole cohort (ROC Analysis and NRI)
The addition of CAC to the FRS resulted in significantly higher improvement in AUC compared with the addition of either TAC, AVC, MAC, PAT or LA to the FRS (data not shown). As shown in supplement Figure 1, the addition TAC, AVC, MAC, PAT and LA to FRS + CAC did not result in significant improvement in AUC for incident CHD [0.766 vs. 0.767, 0.769, 0.770, 0.766 and 0.764 respectively]. Compared with the NRI of FRS +CAC, the addition of TAC, AVC, MAC, PAT and LA individually to FRS+ CAC also resulted in very significant reductions in NRI (data not shown) for incident CHD. No significant lack of fit was also detected using the Hosmer – Lemeshow χ2 statistics.
Similarly the addition TAC, AVC, MAC, PAT and LA to FRS + CAC resulted in reductions in AUC (supplemental Figure 2) and NRI compared with FRS + CAC alone for incident (data not shown). Similar results were obtained when the analysis was stratified by race/ethnicity or gender.
Discussion
The current study shows that CAC is superior among all the currently available CT derived risk factors for improving discrimination over and beyond the FRS. Moreover, the addition of TAC, AVC, MAC, PAT or LA individually to the FRS + CAC, reduces the discriminative ability of FRS + CAC alone for incident CHD/CVD. In fact it appears that the other risk markers are so uninformative for CHD/CVD prediction compared with CAC such that their addition to CAC results in worsening of its discriminative ability. To our knowledge, this is the first study that has evaluated the improvement in discrimination afforded by the currently available cardiac CT imaging measures of subclinical disease and risk markers in a single large multi-ethnic cohort using the same statistical approach and outcomes.
The FRS is less accurate especially in individuals classified as intermediate risk by the FRS. This recognition has motivated research to identify markers that could offer greater discrimination, especially for such individuals. CAC has emerged as one of the superior markers for fine-tuning cardiovascular risk prediction in asymptomatic individuals (8, 9). However, the addition of CAC to the FRS is still not optimal and results in significant misclassification especially of high risk individuals in the intermediate Framingham risk group to low risk(8). In a recent MESA study by Yeboah et al(8), 13% of intermediate FRS participants who had CHD events were misclassified to low risk by the addition of CAC to the FRS whilst 7% of intermediate FRS participants who did not have CHD events were misclassified to high risk by the addition of CAC to the FRS. Advancements in cardiac CT imaging have resulted in the identification of other risk markers such as TAC, AVC, MAC, PAT, and LA. However, limited data exist on the independent association of these markers with CHD/CVD (3–7). In addition, the improvement in discrimination over what is provided by the FRS, the current general clinical practice tool for CV risk assessment in asymptomatic individuals, was not evaluated in most of these studies (3–5). In the present study, TAC, AVC, MAC, PAT and LA were inferior to CAC for incident CHD/CVD prediction, have worse discriminative abilities when added individually to the FRS compared with CAC and each resulted in significant reduction in discrimination when added to FRS + CAC compared with FRS+ CAC. This suggests that for CV risk prediction, CAC may be the only cardiac CT imaging risk marker worth quantifying.
CAC has shown superiority in improving CV risk prediction over and beyond the FRS when compared with novel biomarkers and imaging modalities (8,9). Even though the present study supports the use of CAC to improve CV risk prediction, especially in the intermediate Framingham risk group, further study and standardization is need to optimally incorporate CAC into primary prevention strategies. The acquisition of CAC like any screening test including biomarkers or other imaging modalities involves risks associated with the screen process. The risk associated with CAC screening include exposure to low-level radiation and incidental findings identified during the scan. Relative to each of these risks is the evolving understanding that CAC screening may require only one or two scans in midlife separated by a decade rather than numerous scans at 5 year intervals. Prior to 2009, variations in equipment and scan protocols resulted in significant variations in radiation exposure(22) resulting in subsequent professional guidelines to address these issues (23) as well as further improvements in CT scanner technology designed to reduce radiation exposure. The benefits and risks associated with incidental findings detected during CAC imaging also remains unclear (24). More research evaluating the cost-effectiveness, risk-benefit ratios, and patient preference for CAC screening in asymptomatic individuals is needed.
The strengths of the present study include the large sample size, the multi-ethnic nature of the cohort, adjudicated events, and long duration of follow-up. The limitations include the fact that the results of these CV markers were made available to the participants and their clinicians. It is plausible that some of these participants then began taking medications that may have affected the outcomes. Secondly, MESA is a prospective observational study. The CVD outcome included all strokes (hemorrhagic and non hemorrhagic) and may have affected our results. Although we adjusted for most potential confounders in our multivariable model, our results could still be influenced by residual confounding. Finally, MESA recruited participants from 4 ethnicities in the US without clinically apparent cardiovascular disease. Therefore, our results may not apply to other populations.
Conclusion
CAC, TAC, AVC, MAC were independent predictors of incident CHD/CVD in asymptomatic individuals within the MESA cohort. When added to the FRS, CAC has superior discriminative ability compared with TAC, AVC, MAC, PAT or LA. Compared with FRS +CAC, the addition of TAC, AVC, MAC, PAT or LA to the FRS and CAC resulted in significant worsening of discrimination. The present study suggests that TAC, AVC, MAC, PAT and LA may not be useful for improving cardiovascular risk prediction in multiethnic cohorts
Supplementary Material
Supplement Figure 1: Receiver operating characteristic curves showing the area under the curve (AUC) for the Framingham risk score (FRS), coronary calcium score (CAC), thoracic aorta calcium (TAC), aortic valve calcium (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT)and liver attenuation (LA) for incident coronary heart disease events in MESA.
Supplement Figure 2: Receiver operating characteristic curves showing the area under the curve (AUC) for the Framingham risk score (FRS), coronary calcium score (CAC), thoracic aorta calcium (TAC), aortic valve calcium (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT)and liver attenuation (LA) for incident cardiovascular disease events in MESA
Acknowledgements
The authors would like to thank the investigators, the staff, and the participants of the MESA study for their valuable contributions. We also thank Karen P.Klein for editing this manuscript.
Funding Sources: This research was supported by contracts N01-HC-95159 through N01-HC-95167 and a Diversity Supplement to R01HL098445 (PI: J. Jeffrey Carr) and R01 HL071739. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Footnotes
Disclosures: None.
References
- 1.Hamilton-Craig CR, Friedman D, Achenbach S. Cardiac computed tomography-evidence, limitations and clinical application. Heart Lung Circ. 2012;20:70–81. doi: 10.1016/j.hlc.2011.08.070. [DOI] [PubMed] [Google Scholar]
- 2.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Budoff MJ, Nasir K, Katz R, Takasu J, Carr JJ, Wong ND, Allison M, Lima JA, Detrano R, Blumenthal RS, Kronmal R. Thoracic aortic calcification and coronary heart disease events: the multi ethnic study of atherosclerosis (MESA) Atherosclerosis. 2011;215:196–202. doi: 10.1016/j.atherosclerosis.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ding J, Hsu FC, Harris TB, Liu Y, Kritchevsky SB, Szklo M, Ouyang P, Espeland MA, Lohman KK, Criqui MH, Allison M, Bluemke DA, Carr JJ. The association of pericardial fat with incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2009;90:499–504. doi: 10.3945/ajcn.2008.27358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benjamin EJ, Plehn JF, D’Agostino RB, Belanger AJ, Comai K, Fuller DL, Wolf PA, Levy D. Mitral annular calcification and the risk of stroke in an elderly cohort. N Engl J Med. 1992;327:374–379. doi: 10.1056/NEJM199208063270602. [DOI] [PubMed] [Google Scholar]
- 6.Ghouri N, Preiss D, Sattar N. Liver enzymes, non alcoholic fatty liver disease and incident cardiovascular disease: a narrative review and clinical perspective of prospective data. Hepatology. 2010;52:1156–1161. doi: 10.1002/hep.23789. [DOI] [PubMed] [Google Scholar]
- 7.Treeprasertsuk S, Leverage S, Adams LA, Lindur KD, St. Sauver J, Angulo P. The Framingham risk score and heart disease in non alcoholic fatty liver disease. Liver int. 2012;32:945–950. doi: 10.1111/j.1478-3231.2011.02753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeboah J, McClleland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, Carr JJ, Goff DC, Greenland P, Herrington DM. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate risk individuals. JAMA. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kavousi M, Elias-Smale S, Rutten JH, Leening MJ, Vliegenthart R, Verwoert GC, Krestin GP, Oudkerk M, de Maat MP, Leebeek FW, Mattace-Raso FU, Lindemans J, Hofman A, Steyerberg EW, van der Lugt A, van den Meiracker AH, Witteman JC. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med. 2012;156:438–444. doi: 10.7326/0003-4819-156-6-201203200-00006. [DOI] [PubMed] [Google Scholar]
- 10.Diederichsen AC, Sand NP, Norgaard B, Lambrecht J, Jensen JM, Munkholm H, Aziz A, Gerke O, Egstrup K, Larsen ML, Petersen H, Hoilund-Carlsen PF, Mickley H. Discrepancy between coronary artery calcium score and Heart score in middle aged Danes. DanRisk Study. Eur J Prev Cardiol. 2012;19:558–564. doi: 10.1177/1741826711409172. [DOI] [PubMed] [Google Scholar]
- 11.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 12.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 13.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 14.Budoff MJ, Takasu J, Katz R, Mao S, Shavelle DM, O’Brien KD, Blumenthal RS, Carr JJ, Kronmal R. Reproducibility of CT measurements of aortic valve calcification, mitral annulus calcification, and aortic wall calcification in the multi-ethnic study of atherosclerosis. Acad Radiol. 2006;13:166–172. doi: 10.1016/j.acra.2005.09.090. [DOI] [PubMed] [Google Scholar]
- 15.Zeb I, Li D, Nasir K, Katz R, Larijani VN, Budoff MJ. Computed Tomography Scans in the Evaluation of Fatty Liver Disease in a Population Based Study: The Multi-Ethnic Study of Atherosclerosis. Acad. Radiol. 2012;19:811–818. doi: 10.1016/j.acra.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima JA, Crouse JR, Herrington DM. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation. 2009;120:502–509. doi: 10.1161/CIRCULATIONAHA.109.864801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D’Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores. Results of a multiple ethnic group investigation. JAMA. 2001;286:180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 18.Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Statistics in Medicine. 2004;23:2109–2123. doi: 10.1002/sim.1802. [DOI] [PubMed] [Google Scholar]
- 19.Delong ER, Delong CM, Clarke-Pearson DL. Comparing the area under two or more correlated receiver operating characteristic curves. a non-parametric approach. Biometric. 1998;44:845–857. [PubMed] [Google Scholar]
- 20.Pencina MJ, D’Agostino RB, Vasan RS. Statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med. 2010;48:1703–1711. doi: 10.1515/CCLM.2010.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.May S, Hosmer DW. A simplified method of calculating an overall goodness-of-fit test for the Cox proportional hazards model. Lifetime Data Anal. 1998;4(2):109–120. doi: 10.1023/a:1009612305785. [DOI] [PubMed] [Google Scholar]
- 22.Kim KP, Einstein AJ, Berrington de Gonzalez A. Coronary artery calcification screening: estimated radiation dose and cancer risk. Arch intern med. 2009;169:1188–1194. doi: 10.1001/archinternmed.2009.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Voros S, Rivera JJ, Berman DS, Blankstein R, Budoff MJ, Cury RC, Desai MY, Dey D, Halliburton SS, Hecht HS, Nasir K, Santos RD, Shapiro MD, Taylor AJ, Valeti US, Young PM, Weissman G. Society for Atherosclerosis Imaging and Prevention Tomographic Imaging and Prevention Councils; Society of Cardiovascular Computed Tomography. Guideline for minimizing radiation exposure during acquisition of coronary artery calcium scans with the use of multidetector computed tomography: a report by the Society for Atherosclerosis Imaging and Prevention Tomographic Imaging and Prevention Councils in collaboration with the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2011;5:75–83. doi: 10.1016/j.jcct.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 24.George A, Movahed A. Recognition of non cardiac findings on cardiac computer tomographic examination. Rev Cardiovasc Med. 2010;11:84–91. doi: 10.3909/ricm0521. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement Figure 1: Receiver operating characteristic curves showing the area under the curve (AUC) for the Framingham risk score (FRS), coronary calcium score (CAC), thoracic aorta calcium (TAC), aortic valve calcium (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT)and liver attenuation (LA) for incident coronary heart disease events in MESA.
Supplement Figure 2: Receiver operating characteristic curves showing the area under the curve (AUC) for the Framingham risk score (FRS), coronary calcium score (CAC), thoracic aorta calcium (TAC), aortic valve calcium (AVC), mitral annular calcification (MAC), pericardial adipose tissue volume (PAT)and liver attenuation (LA) for incident cardiovascular disease events in MESA