Abstract
Background
Most persons diagnosed with HIV alter their sexual behavior in a way that reduces the risk of HIV transmission, but the durability of such behavior change is unknown.
Methods
We conducted annual anonymous cross-sectional surveys in randomly selected patients with appointments at a large, public hospital HIV Clinic in Seattle, Washington from 2005 to 2009. We used logistic regression to assess the association between time since HIV diagnosis and self-report of unprotected anal or vaginal intercourse (UAVI) with partners of negative or unknown HIV status (nonconcordant UAVI), and quantile regression to evaluate the association between time since HIV diagnosis and number of anal or vaginal sex partners.
Results
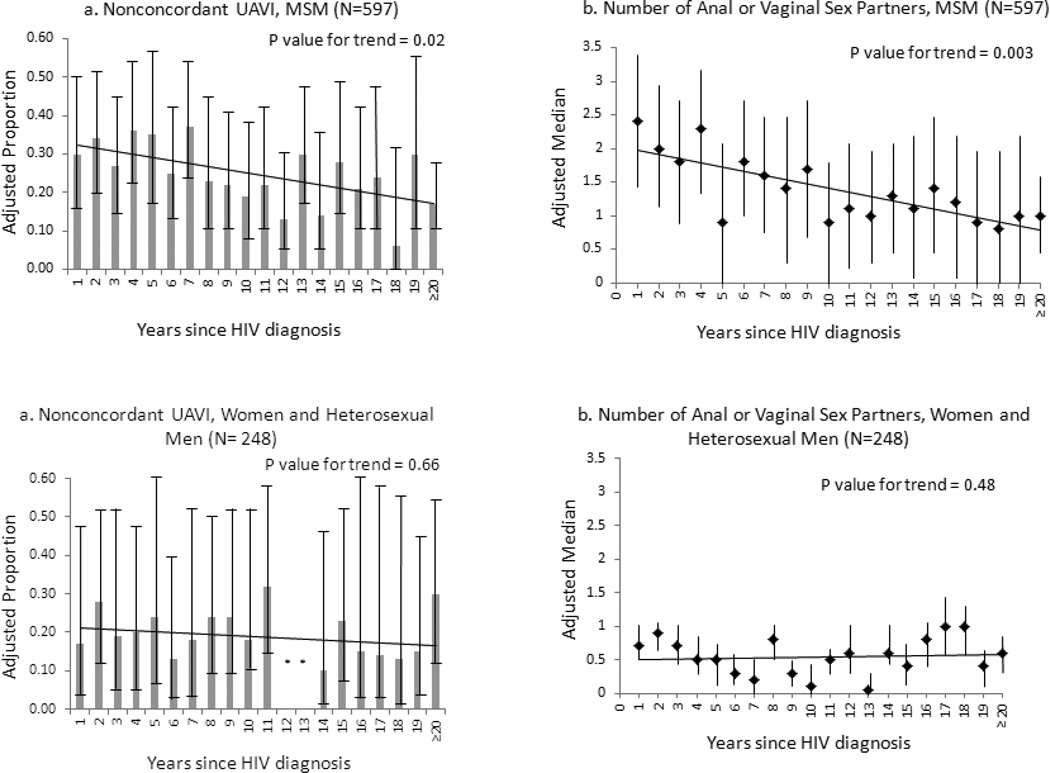
We analyzed 845 surveys collected over 5 years. MSM had been diagnosed with HIV a mean of 12 (SD 7) years and non-MSM a mean of 11 (SD 6) years. Among 597 MSM, longer time since HIV diagnosis was associated with lower age-adjusted odds of reporting nonconcordant UAVI [(OR 0.96 (95% CI: 0.92 – 0.99)] and a lower age-adjusted number of sex partners (β coefficient −0.03, p=0.007). Among 248 women and heterosexual men, time since HIV diagnosis was not significantly associated with age-adjusted odds of nonconcordant UAVI [OR 0.99 (95% CI: 0.93 – 1.04)] or number of sex partners (β coefficient −0.01, p=0.48).
Conclusions
These results indicate that HIV transmission-associated behavior is relatively stable following the first year after HIV diagnosis. Our findings suggest that behavior change in the first year after HIV diagnosis, reported in other studies, is durable.
Keywords: Sexual Behavior; HIV Infections/psychology; Homosexuality, male; Substance-Related Disorders/complications
INTRODUCTION
HIV case-finding plays a crucial role in HIV prevention, in part because most persons substantially alter their sexual behavior following the receipt of a positive HIV test result [1]. Men who have sex with men (MSM) report fewer sex partners and a reduction of unprotected anal intercourse with partners of negative or unknown HIV status in the first year following HIV diagnosis [2–4]. However, the durability of such behavior change is unclear since data on sexual behavior patterns beyond the first year after HIV diagnosis are sparse [5]. Long-term cohort studies have not consistently reported data on partner HIV status [6, 7], an aspect of sexual behavior that is now recognized to be a critical part of behavioral research related to HIV prevention [8–12]. Some investigators have suggested that factors such as safer sex fatigue may lead to increased risk behavior over time among MSM diagnosed with HIV infection [9, 13, 14]. The objective of this study was to assess whether sexual risk behaviors associated with HIV transmission increase in the time following the first year after HIV diagnosis.
MATERIALS AND METHODS
Between 2005 and 2009, we conducted annual cross-sectional surveys of patients in the Harborview Medical Center (Madison) HIV Clinic in Seattle, Washington. HMC is a public hospital and the clinic is the largest provider of HIV care in the U.S. Pacific Northwest. The survey methodology is described in detail elsewhere [15]. Briefly, we offered an anonymous, self-administered, written survey to randomly-selected English-speaking patients with clinic appointments during a two-week period in the spring of each year. The survey included questions about the date of HIV diagnosis, antiretroviral therapy (ART) use, substance abuse, number of anal or vaginal sex partners, and unprotected anal or vaginal intercourse (UAVI) by perceived HIV status of partners (positive, negative, unknown) in the past year. We separately asked questions about sex in the past year with a primary partner and the primary partner’s HIV status. In the final year of the survey, we asked participants whether they had taken the survey in the prior year. Patients received $5 for completing the survey.
The primary outcome measures for this analysis were UAVI with partners of negative or unknown HIV status (nonconcordant UAVI) and number of anal or vaginal sex partners. We stratified the population into two groups for all analyses: 1) MSM and 2) women and heterosexual men. We defined MSM as men who reported having a male sex partner in the prior year or who self-identified as gay or bisexual, and we defined heterosexual men as men who reported only having female sex partners and who did not self-identify as gay or bisexual. We excluded respondents diagnosed with HIV in the year prior to survey completion because the survey asked about sexual behavior in the past 12 months and it would not have been possible to determine if unprotected sex with discordant partners occurred before or after the respondent’s HIV diagnosis. We categorized time since HIV diagnosis by year from 1 to 19 years and grouped those diagnosed ≥ 20 years ago.
We assessed the association between time since HIV diagnosis and nonconcordant UAVI using logistic regression and between time since HIV diagnosis and number of sex partners using quantile regression. We constructed two multivariate models for each outcome measure. Both models were defined a priori. In the first model, we included age and year of survey as covariates. Because older age is associated with decreased sexual activity, we hypothesized that age would confound the relationship between risk behavior and time since HIV diagnosis. This model was of primary interest in answering our study question. In the second model, we also adjusted for ART use and substance use in order to determine whether adjustment for these additional factors would provide an explanation for the observed relationship between the age and calendar year-adjusted association between time since HIV diagnosis and the outcome measures. We analyzed substance use as methamphetamine use, heroin use, cocaine use, and for MSM, amyl nitrate use because our group previously found these factors to be associated with nonconcordant UAVI in the study population [15]. ART use was self-reported at the time of the survey. We assessed for interaction between calendar year and ART use, and included the interaction factor in the multivariate models. We used variance inflation factors to assess for collinearity between age and time since HIV diagnosis. We were not able to measure individual longitudinal changes from year to year because the responses were anonymous. The University of Washington IRB approved all study procedures.
RESULTS
Over the five year study period, we randomly selected 1782 patients with scheduled clinic appointments as potential participants. Of these, 551 (31%) did not attend their appointments and were therefore unavailable, and 18 (1%) were too ill to participate. The study staff did not approach 86 (5%) patients, the majority of whom were not offered participation because they did not speak English. Of the remaining 1127 potential participants, 119 (11%) declined to participate. Thus, the 1008 persons who completed the survey comprised 89% of those offered the survey and 57% of those randomly selected as potential participants. We excluded 69 (7%) surveys from persons diagnosed with HIV in the year prior to the survey and 61 (6%) surveys missing the date of HIV diagnosis. Of the remaining 878 respondents, 20 were excluded because they either did not indicate their gender (N=4) or were men who did not indicate their sexual orientation or the gender of their sex partners in the past year (N=16). We excluded transgendered patients due to the small size of this population (N=13). In the final year of the survey, 37 of 202 (18%) participants indicated that they had participated in the previous year.
Table 1 summarizes the characteristics of the 845 participants included in the final analysis (N=159–183 for each year of the survey). The majority (71%) were MSM. Overall, the mean age was 44 (SD ± 9) years and the mean time since HIV diagnosis was 12 (SD ± 7) years; 65% of participants were white, and 51% reported using at least one substance in the prior year. Compared to heterosexual men, women were younger (mean age 44 vs. 47 years, p=0.01) and more likely to have had education beyond high school (71% of women vs. 29% of heterosexual men, p=0.003). Otherwise, there were no significant differences in demographics, time since HIV diagnosis, ART or substance use, or behavioral outcomes between women and heterosexual men (data not shown). Age and time since HIV diagnosis were not collinear among MSM or women and heterosexual men (variance inflation factors <1.2).
TABLE 1.
Demographic, Clinical and Behavioral Characteristics of Survey Respondents, 2005–2009 (n=845)
| Variable | Men who Have Sex with Men (N=597) Mean (±SD) Median (IQR) No. (%) |
Women and Heterosexual Men (N=248) Mean (±SD) Median (IQR) No. (%) |
|---|---|---|
| Age, years | 43 (± 9) | 45 (± 10) |
| Number of anal or vaginal sex partners in the past 12 months | 1 (0 – 4) | 1 (0 – 1) |
| Time since HIV diagnosis, years | ||
| 1–4 | 123 (21) | 58 (23) |
| 5–9 | 136 (23) | 68 (27) |
| 10–14 | 143 (24) | 54 (22) |
| 15–19 | 116 (19) | 49 (20) |
| ≥ 20 | 29 (13) | 19 (8) |
| Gender | ||
| Male | 597 (100) | 108 (44) |
| Female | 0 | 140 (56) |
| Race | ||
| White | 433 (73) | 124 (50) |
| African American | 65 (11) | 81 (33) |
| Asian/Pacific Islander | 9 (2) | 1 (<1) |
| American Indian/Alaska Native | 23 (4) | 15 (6) |
| Multiple/Other | 54 (9) | 19 (8) |
| Missing | 13 (2) | 8 (3) |
| Hispanic ethnicity | 61 (12) | 14 (6) |
| Sexual identity | ||
| Gay | 504 (85) | NA |
| Bisexual Man | 73 (12) | NA |
| Heterosexual | 4 (<1) | 224 (92) |
| Lesbian or bisexual woman | NA | 19 (8) |
| Other | 13 (2) | 1 (<1) |
| Income | ||
| <$15,000 | 381 (64) | 201 (81) |
| $15,001 – 30,000 | 124 (21) | 25 (10) |
| >$30,000 | 82 (14) | 13 (5) |
| Missing | 10 (2) | 9 (4) |
| Education | ||
| <High school graduate | 61 (10) | 77 (31) |
| High school graduate | 170 (28) | 86 (35) |
| Some college | 219 (37) | 50 (20) |
| College graduate | 73 (12) | 21 (8) |
| >College | 61 (10) | 6 (2) |
| Missing | 13 (2) | 8 (3) |
| Substance use in preceding year | ||
| Methamphetamine | 154 (27) | 11 (4) |
| Amyl nitrates | 128 (22) | 2 (1) |
| Cocaine | 54 (9) | 30 (12) |
| Heroin | 53 (9) | 34 (14) |
| Taking antiretrovirals | 465 (78) | 179 (72) |
| Nonconcordant unprotected anal or vaginal intercourse | 148 (25) | 49 (20) |
NOTE. The proportions of MSM and non-MSM respondents did not differ significantly by survey year (p=0.11).
HIV Transmission-Associated Sexual Behaviors among MSM
Of 597 MSM, 375 (63%) reported having at least one anal or vaginal sex partner in the past year; 148 reported nonconcordant UAVI, comprising 25% of all MSM and 39% of sexually active MSM. In bivariate analysis, longer time since HIV diagnosis was associated with lower odds of reporting nonconcordant UAVI among MSM [OR 0.94 (95% CI: 0.91 – 0.97)]. As shown in Figure 1, longer time since HIV diagnosis remained associated with lower odds of reporting nonconcordant UAVI among MSM when age and calendar year were included as covariates [(OR 0.96 (95% CI: 0.92 – 0.99) per year up to 20 years]. With additional adjustment for substance use and ART use, length of time since HIV diagnosis was not significantly associated with the odds of reporting nonconcordant UAVI [OR 0.96 (95% CI: 0.92 – 1.00)] (Table 2). The odds of reporting nonconcordant UAVI and the number of sex partners did not differ significantly between MSM who self-identified as gay versus those self-identified as bisexual (data not shown). ART use was not significantly associated with the odds of nonconcordant UAVI in either MSM or non-MSM. The odds of reporting UAVI with HIV-positive partners was not significantly associated with time since HIV diagnosis among MSM when adjusted for age and calendar year [OR 0.99 (95% CI: 0.96 – 1.02)], and the proportion of persons reporting UAVI with HIV-positive partners did not change significantly over the survey period [37–45% per year, OR 1.02 (95% CI: 0.92 – 1.12)].
FIGURE 1.
Unprotected anal or vaginal intercourse (UAVI) with partners of negative or unknown HIV status (nonconcordant UAVI) and the median number of anal or vaginal sex partners by time since HIV diagnosis, adjusted for age and year of survey. Panels 1a and 2a show adjusted proportions of participants reporting nonconcordant UAVI by length of time since HIV diagnosis, adjusted for age, among MSM (Panel 1a) and among women and heterosexual men (Panel 2a). P-values are from logistic regression. Panels 1b and 2b show adjusted median number of anal or vaginal sex partners by length of time since HIV diagnosis, adjusted for age, among MSM (Panel 1b) and among women and heterosexual men (Panel 2b). P-values are from quantile regression.
TABLE 2.
Predictors of unprotected anal or vaginal intercourse (UAVI) with a partner of discordant or unknown HIV status (nonconcordant UAVI) in the past year and number of anal or vaginal sex partners in the past year among 845 survey respondents.
| Nonconcordant UAVI in past year |
Number of anal or vaginal sex partners in past year |
|||||
|---|---|---|---|---|---|---|
| N | No. (% each group) |
Adjusted OR (95% CI) a | Median (IQR) |
Adjusted β coefficient |
Adjusted P-value |
|
| Men who have sex with men | 597 | 148 (25) | 1 (0 – 4) | |||
| Time since HIV diagnosis (per category) b | -- | -- | 0.96 (0.92 – 1.00) | -- | −0.03 | 0.01 |
| Age (per 5 years) | -- | -- | 0.94 (0.81 – 1.10) | -- | −0.17 | <0.001 |
| Calendar year | -- | -- | 1.10 (0.86 – 1.41) | -- | 0.06 | 0.42 |
| Substance use in the past year | ||||||
| Methamphetamine | 154 | 68 (44) | 1.98 (1.10 – 3.68) | 4 (1 – 10) | 2.55 | <0.001 |
| Amyl nitrate | 128 | 54 (42) | 2.02 (1.10 – 3.71) | 4 (1 – 13) | 2.32 | <0.001 |
| Cocaine | 54 | 27 (50) | 1.35 (0.43 – 4.29) | 3 (1 – 10) | −0.10 | 0.76 |
| Heroin | 53 | 24 (45) | 1.23 (0.38 – 4.07) | 2 (0 – 12) | 3.77 | <0.001 |
| Taking antiretrovirals | 465 | 97 (21) | 0.69 (0.23 – 2.06) | 1 (0 – 3) | −0.04 | 0.90 |
| Women and heterosexual men | 248 | 49 (20) | 1 (0 – 1) | |||
| Time since HIV diagnosis (per category) b | -- | -- | 0.97 (0.90 – 1.04) | -- | −0.01 | 0.40 |
| Age (per 5 years) | -- | -- | 0.74 (0.60 – 0.90) | -- | −0.15 | 0.002 |
| Calendar year | -- | -- | 1.16 (0.91 – 1.48) | -- | 0.01 | 0.84 |
| Substance use in the past year | ||||||
| Methamphetamine | 11 | 7 (64) | 7.75 (1.50 – 40.16) | 1 (0 – 2) | 0.43 | 0.27 |
| Cocaine | 30 | 11 (37) | 1.42 (0.19 – 10.83) | 1 (0 – 1) | 0.45 | 0.29 |
| Heroin | 34 | 12 (35) | 0.82 (0.10 – 6.57) | 1 (0 – 1) | −0.54 | 0.22 |
| Taking antiretrovirals | 179 | 32 (18) | 0.90 (0.35 – 2.29) | 0 (0 – 1) | −0.36 | 0.08 |
Adjusted for factors in table and, for MSM, an interaction term of survey year with antiretroviral therapy use, which was not independently associated with either outcome in multivariate analysis (data not shown).
Per year up to 20 years (≥20 years grouped)
MSM reported a mean of 6 and a median of 1 (range 0–230) anal or vaginal sex partners in the prior year. MSM who reported nonconcordant UAVI also reported more sex partners than those who did not report nonconcordant UAVI [median 4 (IQR: 2–15) and median 1 (IQR: 0–2), respectively; p=0.009]. In bivariate analysis, longer time since HIV diagnosis was not associated with a lower number of sex partners among MSM (β coefficient 0, p=0.1), but as shown in Figure 2, longer time since HIV diagnosis was associated with a lower number of sex partners when adjusted for age and calendar year (β coefficient -0.04, p=0.003). A longer time since HIV diagnosis remained associated with a lower number of anal or vaginal sex partners among MSM when adjusted for substance use and antiretroviral use, (β coefficient −0.03, p=0.007).
HIV Transmission-Associated Sexual Behaviors among Women and Heterosexual Men
Among 248 women and heterosexual men, 123 (50%) reported having at least one anal or vaginal sex partner in the past year and 49 reported nonconcordant UAVI (20% overall, 40% of sexually active participants). The proportion of persons that reported UAVI did not differ significantly between men (18%) and women (21%; p=0.5). In contrast to MSM, the association between length of time since HIV diagnosis and the odds of reporting nonconcordant UAVI was not statistically significant in bivariate analysis [OR 0.99 (95% CI: 0.94 – 1.05)] or when adjusted for age and calendar year [OR 0.99 (95% CI: 0.93 – 1.04)]. Additional adjustment for substance use and ART use did not alter these results [OR 0.97 (95% CI: 0.90 – 1.04)]. Women and heterosexual men reported a mean and median of 1 (range 0–60) sex partner in the prior year. The length of time since HIV diagnosis was statistically significantly associated with a lower number of sex partners in bivariate analysis (β coefficient −0.05, p<0.001). However, longer time since HIV diagnosis was not independently associated with a lower number of sex partners among women and heterosexual men when age and calendar year were included as covariates (β coefficient −0.01, p=0.48) nor when ART and substance use were additionally included (β coefficient −0.01, p=0.40).
DISCUSSION
We found no association between transmission-associated sexual risk behavior and time since HIV diagnosis among patients attending an HIV clinic more than one year following their initial positive HIV test. Although previous reports have suggested that safer sex fatigue may contribute to increased sexual risk behavior among MSM diagnosed with HIV [9, 13, 14], our findings do not support this, and instead suggest that sexual risk behavior remains relatively stable among MSM in the period starting one year after HIV diagnosis. Adjustment for age, and ART and substance use did not alter this finding.
Our findings complement prior reports, which, taken together, suggest a pattern of evolving sexual behavior following HIV diagnosis. Most people rapidly and profoundly decrease behaviors likely to transmit HIV infection in the period immediately following diagnosis. Over the course of the first year following diagnosis, most resume sexual activity, and a minority engage in nonconcordant UAVI [2–4]. This new level of HIV transmission-associated risk behavior may then reach equilibrium within the first year, and although risk behaviors continue to wax and wane over time [16], these changes are relatively small. Our findings are consistent with those from a cross-sectional survey of black and Latino MSM in Los Angeles, New York City, and Philadelphia, which found that the prevalence of nonconcordant unprotected anal intercourse did not differ by length of time since HIV diagnosis [17], and with observations from a cohort study of MSM living with HIV/AIDS in San Francisco demonstrating sustained reductions in nonconcordant unprotected anal intercourse over the 12 years following HIV diagnosis [18]. Although the latter study found that the total number of anal sex partners increased transiently over the study period, the number of nonconcordant partners with whom the participants reported unprotected anal sex decreased in the year following HIV diagnosis and remained stable in subsequent years. Furthermore, we found no evidence to suggest that ART use is associated with behavioral disinhibition. As in previous studies [17, 19, 20], ART use was not associated with a greater likelihood of reporting nonconcordant UAVI or more sex partners.
This analysis was limited by methodologic factors that could affect the validity and generalizability of our results. We inferred natural history from serial cross-sectional data, which may not be valid. Since the survey was anonymous, we could not measure changes in individual sexual behavior over time. Some persons completed our survey during more than one year, meaning our data were correlated, but we were not able to account for this in the analysis. We did not capture data on behavioral changes in the first year after HIV diagnosis, and thus cannot directly determine whether our survey participants changed their sexual behavior in response to being diagnosed with HIV, nor can we compare our results directly with those of cohort studies of behavior during the first year after HIV diagnosis. Finally, our findings may not be generalizable. We analyzed data from a single clinical site in Seattle, WA, not all randomly selected persons completed our survey, and our exclusion of non-English speakers likely caused us to undersample Latino and foreign-born blacks.
In summary, these results indicate that HIV transmission-associated behavior is relatively stable following the first year after HIV diagnosis. Our findings suggest that behavior change in the first year after HIV diagnosis, reported in other studies, is durable.
Acknowledgments
The authors thank Mark Fleming for administering the survey and entering data, Carol Glenn for recruiting survey participants, Dr. Joanne Stekler for reviewing a draft of the manuscript, and Dr. James Hughes for providing statistical advice.
Sources of Funding and Conflicts of Interest: This work was supported by the Public Health – Seattle & King County HIV/STD Program; the National Institutes of Health [JCD was supported by T32 AI-07140 from NIAID and 5K23MH090923 from NIMH]; and the University of Washington Center for AIDS Research (CFAR), an NIH funded program (P30 AI027757), which is supported by the following NIH Institutes and Centers (NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA). Dr. Golden has received donated test kits from Genprobe and azithromycin from Pfizer for research, and Dr. Harrington has received payment for lectures on HIV to the American Academy of Family Practice and the Academy of Physician Assistants.
Footnotes
These findings were presented in part at the 18th meeting of the International Society for STD Research/ British Association for Sexual Health & HIV; London, UK; 2009.
References
- 1.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–453. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 2.Colfax GN, Buchbinder SP, Cornelisse PG, Vittinghoff E, Mayer K, Celum C. Sexual risk behaviors and implications for secondary HIV transmission during and after HIV seroconversion. AIDS. 2002;16:1529–1535. doi: 10.1097/00002030-200207260-00010. [DOI] [PubMed] [Google Scholar]
- 3.Gorbach PM, Weiss RE, Jeffries R, et al. Behaviors of recently HIV-infected men who have sex with men in the year postdiagnosis: effects of drug use and partner types. J Acquir Immune Defic Syndr. 2011;56:176–182. doi: 10.1097/QAI.0b013e3181ff9750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gorbach PM, Drumright LN, Daar ES, Little SJ. Transmission behaviors of recently HIV-infected men who have sex with men. J Acquir Immune Defic Syndr. 2006;42:80–85. doi: 10.1097/01.qai.0000196665.78497.f1. [DOI] [PubMed] [Google Scholar]
- 5.Eaton LA, Kalichman SC. Changes in transmission risk behaviors across stages of HIV disease among people living with HIV. J Assoc Nurses AIDS Care. 2009;20:39–49. doi: 10.1016/j.jana.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DiFranceisco W, Ostrow D, Adib S, Chmiel J, Hoffmann R. Predictors of long-term maintenance of safer sex and lapse/relapse: a nine-year follow-up of the Chicago CCS/MACS Cohort. AIDS and Behavior. 1999;3:325–334. [Google Scholar]
- 7.Wolf K, Young J, Rickenbach M, et al. Prevalence of unsafe sexual behavior among HIV-infected individuals: the Swiss HIV Cohort Study. J Acquir Immune Defic Syndr. 2003;33:494–499. doi: 10.1097/00126334-200308010-00010. (1999) [DOI] [PubMed] [Google Scholar]
- 8.Golden MR, Brewer DD, Kurth A, Holmes KK, Handsfield HH. Importance of sex partner HIV status in HIV risk assessment among men who have sex with men. J Acquir Immune Defic Syndr. 2004;36:734–742. doi: 10.1097/00126334-200406010-00011. [DOI] [PubMed] [Google Scholar]
- 9.Cox J, Beauchemin J, Allard R. HIV status of sexual partners is more important than antiretroviral treatment related perceptions for risk taking by HIV positive MSM in Montreal, Canada. Sex Transm Infect. 2004;80:518–523. doi: 10.1136/sti.2004.011288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golden MR, Stekler J, Hughes JP, Wood RW. HIV serosorting in men who have sex with men: is it safe? J Acquir Immune Defic Syndr. 2008;49:212–218. doi: 10.1097/QAI.0b013e31818455e8. [DOI] [PubMed] [Google Scholar]
- 11.Wilson DP, Regan DG, Heymer KJ, Jin F, Prestage GP, Grulich AE. Serosorting may increase the risk of HIV acquisition among men who have sex with men. Sex Transm Dis. 2010;37:13–17. doi: 10.1097/OLQ.0b013e3181b35549. [DOI] [PubMed] [Google Scholar]
- 12.Eaton LA, Kalichman SC, Cherry C. Sexual partner selection and HIV risk reduction among Black and White men who have sex with men. Am J Public Health. 2010;100:503–509. doi: 10.2105/AJPH.2008.155903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stolte IG, de Wit JB, Kolader M, Fennema H, Coutinho RA, Dukers NH. Association between 'safer sex fatigue' and rectal gonorrhea is mediated by unsafe sex with casual partners among HIV-positive homosexual men. Sex Transm Dis. 2006;33:201–208. doi: 10.1097/01.olq.0000194596.78637.8e. [DOI] [PubMed] [Google Scholar]
- 14.Ostrow DG, Silverberg MJ, Cook RL, et al. Prospective study of attitudinal and relationship predictors of sexual risk in the multicenter AIDS cohort study. AIDS Behav. 2008;12:127–138. doi: 10.1007/s10461-007-9223-x. [DOI] [PubMed] [Google Scholar]
- 15.Golden MR, Wood RW, Buskin SE, Fleming M, Harrington RD. Ongoing risk behavior among persons with HIV in medical care. AIDS Behav. 2007;11:726–735. doi: 10.1007/s10461-007-9244-5. [DOI] [PubMed] [Google Scholar]
- 16.Aidala AA, Lee G, Garbers S, Chiasson MA. Sexual behaviors and sexual risk in a prospective cohort of HIV-positive men and women in New York City, 1994–2002: implications for prevention. AIDS Educ Prev. 2006;18:12–32. doi: 10.1521/aeap.2006.18.1.12. [DOI] [PubMed] [Google Scholar]
- 17.Marks G, Millett GA, Bingham T, et al. Understanding differences in HIV sexual transmission among Latino and black men who have sex with men: The Brothers y Hermanos Study. AIDS Behav. 2009;13:682–690. doi: 10.1007/s10461-008-9380-6. [DOI] [PubMed] [Google Scholar]
- 18.Vallabhaneni S, Loeb L, Bragg L, et al. Program and abstracts of the 18th Conference on Retroviruses and Opportunistic Infections. Boston, MA: 2011. Seroadaptive tactics adopted by HIV+ MSM can contribute to profound and sustained reductions in HIV transmission risk following HIV diagnosis [abstract 1038] [Google Scholar]
- 19.Crepaz N, Hart TA, Marks G. Highly active antiretroviral therapy and sexual risk behavior: a meta-analytic review. JAMA. 2004;292:224–236. doi: 10.1001/jama.292.2.224. [DOI] [PubMed] [Google Scholar]
- 20.Crepaz N, Marks G, Liau A, et al. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. AIDS. 2009;23:1617–1629. doi: 10.1097/QAD.0b013e32832effae. [DOI] [PubMed] [Google Scholar]