Abstract
Recently there has been increased interest in emotional and physical tolerance risk factors for mood and anxiety disorders. Three tolerance risk factors that have been shown to be related are anxiety sensitivity (AS), distress tolerance (DT), and discomfort intolerance (DI). Although previous research has demonstrated these constructs are malleable, no research has investigated the effects of an AS intervention on DT or DI. Further, no studies have investigated whether changes in DT or DI play a role in mood and anxiety symptom amelioration due to an AS intervention. Participants (N=104), who were selected for elevated levels of AS, completed a single-session computer-assisted AS intervention or a control intervention and follow-up assessments at 1-week and 1-month post intervention. Results revealed that the intervention reduced AS and increased DT, but did not affect DI at the 1-week follow-up. Mediation analyses revealed that changes in AS and DT both mediated changes in symptoms (depression, anxiety, worry) due to the intervention at 1-month follow-up, however, when AS and DT were considered in the same model only the effect via AS remained significant. These results have important implications for the nature of the relationships between AS, DT, and DI as well as the specific mechanistic pathways through which an AS intervention ameliorates symptoms.
Keywords: anxiety sensitivity, distress tolerance, discomfort intolerance, anxiety, depression, worry
Anxiety and depressive disorders are prevalent and disabling conditions that commonly co-occur (Kessler et al., 2003). Given the implications for etiological models, prevention, and treatment, there has been a great deal of research on the identification of common and distinct risk factors for anxiety and depressive disorders (Beekman et al., 2000; Beesdo, Pine, Lieb, & Wittchen, 2010; de Graaf, Bijl, Smit, Vollebergh, & Spijker, 2002; Kendler, Gardner, Gatz, & Pedersen, 2007; Moffitt et al., 2010). Although a number of studies have identified negative emotionality as a robust risk factor for the development of these conditions (Beesdo et al., 2010; Kendler, Kuhn, & Prescott, 2004; Moffitt et al., 2010), recent research has begun to investigate constructs reflective of individual differences in the ability to tolerate negative emotional states rather than variables reflective of the frequency/intensity of the negative emotional states themselves (see Leyro, Zvolensky, & Bernstein, 2010 for a review).
Although a number of affect tolerance constructs have been discussed in the literature, anxiety sensitivity (AS), distress tolerance (DT), and, to a lesser extent, discomfort intolerance (DI) have received considerable research attention within the context of anxiety and depression. AS, or the fear of anxiety-related sensations, has been associated with greater anxiety and worry symptoms (Keough et al., 2010; Macatee et al., 2013; Norr et al., 2013; Viana & Rabian, 2008) as well as depressive symptoms (Cox, Enns, Freeman, & Walker, 2001; Cox, Taylor, & Enns, 1999; Tull & Gratz, 2008). Further, elevated AS confers risk for the development of depressive symptoms (Grant, Beck, & Davila, 2007) and anxiety disorders (Schmidt, Zvolensky, & Maner, 2006). DT is defined as an individual difference variable reflecting the capacity to tolerate aversive emotional states (Simons & Gaher, 2005). Low DT has also been associated with greater anxiety and worry symptoms (Huang, Szabó, & Han, 2009; Keough, Riccardi, Timpano, Mitchell, & Schmidt, 2010; Starr & Davila, 2012; Timpano, Buckner, Richey, Murphy, & Schmidt, 2009) and depressive symptoms in non-clinical samples (Anestis, Gratz, Bagge, & Tull, 2012; Buckner, Keough, & Schmidt, 2007; Dennhardt & Murphy, 2011; Ellis, Fischer, & Beevers, 2010; Gorka, Ali, & Daughters, 2012). In addition, low DT has been shown to prospectively predict increases in worry symptoms (Macatee, Capron, Guthrie, Schmidt, & Cougle, 2013) and has been associated with greater anxiety and depressive symptoms at post-treatment (McHugh et al., 2014; Williams, Thompson, & Andrews, 2013). DI, a construct reflective of individual differences in difficulties tolerating uncomfortable physical sensations, has been linked to anxiety and depressive symptoms, though its relationship to depressive symptoms appears to be less robust given that high DI has only been shown to predict changes in anxiety, but not depressive, symptoms over time (Schmidt, Richey, & Fitzpatrick, 2006). Research on DI has revealed high DI to be most strongly associated with panic-relevant symptoms and outcomes (e.g., fear reactivity to a CO2 challenge; Bon-Miller, Zvolensky, & Bernstein, 2009; Schmidt, Richey, et al., 2006; Schmidt, Richey, Cromer, & Buckner, 2007). To summarize, extant data suggests that DT, AS and DI are associated with anxiety and depressive pathology, though the relationships amongst the affect tolerance constructs themselves, and their relative importance to anxiety and depressive symptoms, has remained relatively unexplored.
AS, DT, and DI have been conceptualized as theoretically-related, but distinct, constructs (Leyro, Zvolensky, & Bernstein, 2010; Zvolensky, Vujanovic, Bernstein, & Leyro, 2010), though little empirical work has been conducted to explicitly test the proposed theoretical associations between these constructs. Bernstein, Zvolensky, Vujanovic, and Moos (2009) conducted an exploratory factor analysis in a healthy sample and found AS and DT to be related to one another as distinct lower-order factors of a higher-order affect tolerance factor, whereas DI was unrelated to AS and DT at the lower and higher-order levels. Mitchell, Riccardi, Keough, Timpano, and Schmidt (2013) found a similar latent structure amongst these variables in non-clinical and clinical samples, though they found AS to be a lower-order factor of DT rather than a distinct but hierarchically adjacent lower-order factor. Though the results of these studies differ on the nature of the relationship between AS and DT, they converge on the dissociation between emotional tolerance (i.e., AS and DT) and physical tolerance (i.e., DI).
The differential importance of these tolerance variables to anxiety and depressive symptoms has rarely been examined in the literature. Available data suggest that AS and DT may contribute both independently and synergistically to worry symptoms (Allan, Macatee, Norr, & Schmidt, in press; Keough et al., 2010; Norr et al., 2013) whereas for depressive symptoms evidence is less consistent for the non-redundant role of DT (Capron, Norr, Macatee, & Schmidt, 2013; Starr & Davila, 2012). There are no studies known to the authors that examine the unique contribution of DI to the prediction of anxiety or depressive symptoms. Taken together, existing data suggest that both AS and DT are uniquely associated with worry symptoms, whereas for depressive symptoms AS appears to play a more important role. Further, little is known about the unique role of DI in anxiety or depressive symptoms, extant research suggesting that it tends to be more narrowly related to panic-relevant variables (Bonn-Miller et al., 2009; Schmidt, Richey, Cromer, & Buckner, 2007).
In a recent paper aimed at developing a translational research framework, Zvolensky, Schmidt, Bernstein, and Keough (2006) stressed the importance of examining prevention and intervention protocols to determine the malleability of risk factors for mood and anxiety symptoms. A growing number of studies have effectively developed AS intervention protocols, including single day workshops (Gardenswartz & Craske, 2001), three-session CBT interventions (Watt et al., 2006a; Watt et al., 2006b), six-week exercise protocols (Broman-Fulks & Storey, 2008), and psychoeducation programs (Feldner, Zvolensky, Babson, Leen-Feldner, & Schmidt, 2008). Schmidt, Eggleston, et al. (2007) examined the effects of a brief (one-session) AS intervention including elements of psychoeducation, cognitive restructuring, and interoceptive exposure in a sample of 404 young adults (M age = 19.3, SD = 3.9). They found significant mean reductions in post-intervention AS. Keough and Schmidt (2012) replicated the findings of Schmidt, Eggleston, et al. (2007), finding post-intervention AS reductions. They also found that reductions in AS were maintained at follow-up one month later.
Although few interventions have been designed to explicitly target DT, several studies have examined the impact of exposure, cognitive-behavioral, acceptance, and mindfulness based intervention protocols on DT. In general, these interventions have led to significant increases in DT (e.g., Borovalova, Gratz, Daughters, Hunt, & Lejuez, 2012; McHugh et al., 2014; Williams et al., 2013; but see Kapson, Leddy, & Haaga, 2012 for an exception). In the largest such study,McHugh et al. (2014) examined the effects of cognitive-behavioral therapy (CBT) on a self-report measure of DT composed of items derived via factor analyses from several affect tolerance measures in a sample of 469 participants (M age = 34 years, SD = 14) in a partial hospital setting (i.e., treatment in a managed care facility lasting on average 8.2 days, SD = 3.2). They found significant changes in DT as well as associations between changes in DT and reductions in mood and anxiety symptoms. Of note, several aspects of their treatment overlapped with aspects of AS interventions (i.e., psychoeducation, challenging negative automatic thoughts).
In contrast to the recent focus of intervention effects on DT, relatively few studies have examined intervention effects on DI. To our knowledge, only a single study examined whether it was possible to reduce levels of DI using a mindfulness-based intervention. Lotan, Tanay, and Bernstein (2013) examined the effect of 4 weekly 60-minute mindfulness training sessions compared to a no-treatment control condition in a community sample of 53 adults (M age = 25.2, SD = 4.3). Whereas reductions in DT were found, there was no improvement in DI, leading Lotan et al. to speculate that the orthogonal nature of DT and DI and/or the lack of malleability of DI may have accounted for this. Together, these findings suggest that similar intervention protocols may be useful in reducing both AS and DT, but not DI.
Interventions focused on transdiagnostic risk factors offer an efficient means to potentially impact multiple disorders. To our knowledge, only three studies have considered whether reductions in risk factors such as AS, DT, and DI mediate the relation between risk factor interventions and reductions in mood and anxiety. Smits, Powers, Cho, and Telch (2004) found that AS mediated the relationship between CBT and reductions in panic symptoms in a sample of 103 individuals diagnosed with panic disorder. Schmidt, Capron, Raines, and Allan (in press) examined the effects of a computerized intervention targeting a lower-order dimension of AS (i.e., AS cognitive concerns) in a sample of 108 community participants and whether this intervention influenced worry and depressive symptoms as well as suicidality and suicidal ideation. They found that the targeted dimension of AS (i.e., AS cognitive concerns) at month 1 mediated the effects of the intervention on month 1 worry, depression, suicidality, and suicidal ideation. Finally, Olthuis and colleagues (in press) found that reductions in AS mediated the effects of a telephone-delivered CBT intervention. Although other studies have also found that interventions targeting AS and DT lead to reductions in psychopathology (e.g., Mitchell, Capron, Raines, & Schmidt, 2014; Schmidt, Eggleston, et al., 2007; Williams et al., 2013), no other studies have examined whether the effects of these interventions on psychopathology are mediated by risk factor reductions. Further, no studies have examined whether a reduction in mood and anxiety symptoms occurs via multiple risk factors. It would be useful to determine whether an AS, DT, or DI intervention reduces mood and anxiety symptoms via more than just AS, DT, or DI, respectively, as this would help highlight potential targets to increase the efficacy of the intervention.
There are several gaps in the literature that the current study is designed to address. Whereas interventions have successfully impacted AS and DT separately as well as together in a composite (e.g., Schmidt, Eggleston, et al., 2007; McHugh et al., 2014), no study has examined the effects of an AS intervention on both AS and DT. Although AS interventions such as the one employed in the current study are specifically designed to target AS, aspects of the intervention, including the use of psychoeducation and interoceptive exposure, may influence other affect tolerance constructs. The findings of McHugh et al. (2014) that CBT led to reductions in a measure of DT composed of items assessing AS, DT, and frustration tolerance is suggestive that an AS intervention could influence affect tolerance more generally. However, this effect may not generalize to physical tolerance, as one study targeting DT and DI found reductions in DT, but not in DI (Lotan et al., 2013). Gaining a better understanding of the mechanisms through which an AS intervention reduces symptoms of anxiety, worry, and depression is important as we do not want to misattribute the full potency of the intervention to be due to changes in AS if there are other mechanisms in play. Therefore, one aim of the current study was to examine the effects of an AS intervention on related risk factors, including DT and DI. The effects of the current intervention on AS have already been reported (Keough & Schmidt, 2012), and have demonstrated that this intervention reduces AS. We hypothesized that the intervention would also impact DT, but not DI. This would provide strong empirical evidence that AS and DT are in fact more closely related to each other than to DI (Berstein et al., 2009; Mitchell et al., 2013), and support claims that there is a distinction between emotional and physical tolerances (Leyro et al., 2010). Additionally, this would provide support for AS being conceptualized as a subfactor of DT (Mitchell et al., 2013) rather than being parallel lower order factors of a broader tolerance factor (Bernstein et al., 2009). If AS is a lower order facet of DT, than an efficacious AS circumscribed intervention should also impact DT, but if AS and DT have a parallel relationship a circumscribed AS intervention would not necessarily impact DT. A further aim of the current study was to examine the impact of the current intervention on mood and anxiety symptoms and the mechanisms for this reduction. The current study seeks to improve upon the methods employed by McHugh and colleagues (2014) by examining the unique contributions of AS, DT, and DI as mediators rather than a composite tolerance variable. The current study also seeks to improve upon the methods used by Schmidt and colleagues (in press) by temporally separating the assessment of the mediators and symptom variables. Based on past findings that AS and DT interventions have reduced mood and anxiety symptoms (e.g., McHugh et al., 2014; Mitchell et al., 2014; Williams et al., 2013) and one study demonstrating that reductions in worry and depression were mediated by reductions in AS cognitive concerns (Schmidt et al. in press), we hypothesized that the intervention would decrease mood and anxiety symptoms and that it would do so through reductions in both AS and DT but not DI.
Method
Participants
Participants, selected for elevated AS, consisted of 104 college students from a large university in the Southern United States. Participants were primarily female (83.7%) with an average age of 18.9 years (SD = 1.42). The racial/ethnic breakdown of the sample was: 81.7% Caucasian, 8.7% African American, 4.8% Asian, and 4.8% Other (e.g., bi-racial); with 11.5% of the sample identifying as Hispanic. Forty-five percent of participants met criteria for at least one psychiatric disorder (see Keough & Schmidt, 2012 for more details).
Self-report Measures
Anxiety Sensitivity. Anxiety Sensitivity Index-3 (ASI-3)
The ASI-3 is a 18-item self-report measure that is used to measure fear of anxiety related sensations (Taylor et al., 2007). Adapted from the original ASI (Reiss, Peterson, Gursky, & McNally, 1986), the ASI-3 was designed to provide a more stable assessment of the three most commonly replicated anxiety sensitivity subfactors (cognitive, social, and physical concerns). In the present study, the ASI-3 demonstrated good to excellent internal consistency at pre-intervention (α = .88) and week 1 (α = .93). The original ASI was used in the current study only for the selection of eligible participants.
Anxiety Symptoms. Beck Anxiety Inventory (BAI)
The BAI is a 21-item questionnaire that measures the experience of anxiety symptoms (Beck, Brown, Epstein, & Steer, 1988). In the present study, the BAI demonstrated excellent internal consistency at pre-intervention (α = .90) and month 1 (α = .92).
Depression Symptoms. Beck Depression Inventory-2 (BDI-2)
The BDI-2 is a 21-item measure of depressive symptoms (Beck, Steer, & Brown, 1996). In the present study, the BDI-2 demonstrated excellent internal consistency at pre-intervention (α = .92) and month 1 (α = .95).
Discomfort Intolerance. Discomfort Intolerance Scale (DIS)
The DIS is a 5-item questionnaire that was used to measure tolerance of physical discomfort (Schmidt, Richey, et al., 2006). In the present study, the DIS demonstrated acceptable internal consistency at pre-intervention (α = .68) and week 1 (α = .64) considering the DIS contains less than 10 items (Devellis, 2003).
Distress Tolerance. Distress Tolerance Scale (DTS)
The DTS is a 15-item measure that was used to measure individual differences in the ability to experience and withstand negative psychological states (Simons & Gaher, 2005). Lower scores on the DTS are indicative of increased problems with tolerating negative psychological states. A self-report rather than behavioral measure of DT was chosen because of extant data indicating discordance amongst measurement methods for affect tolerance constructs (McHugh et al., 2011). Thus, a self-report measure was chosen to maintain consistency with the AS and DI measures. In the present study, the DTS demonstrated excellent internal consistency at pre-intervention (α = .90) and week 1 (α = .93).
Worry. Penn State Worry Questionnaire (PSWQ)
The PSWQ is a 16-item scale measuring symptoms related to pathological worry (Meyer, Miller, Metzger, & Borkovec, 1990). In the present study, the PSWQ demonstrated excellent internal consistency at pre-intervention (α = .94) and month 1 (α = .93).
Procedure
Participants who scored at least 1.5 SD above the mean on the ASI (ASI ≥ 20) were recruited from the undergraduate psychology research pool. The selection mean and standard deviation were derived from the full research pool sample. Trained doctoral students in clinical psychology served as study therapists to administer the study protocol. Eligible participants completed pre-intervention measures and were randomly assigned to an active computer-assisted AS reduction protocol or a computer-assisted control condition (52 participants per condition). Participants in the active condition were guided through the Anxiety Sensitivity Education and Reduction Training (ASERT) program by a study therapist. ASERT consisted of psychoeducation on the nature of symptoms arising from stress and anxiety as well as a brief interoceptive exposure. Participants in the control condition were guided through the Physical Health /Education Training (PHET) program, which consisted of information about habits for a healthy lifestyle (e.g., diet and exercise). The intervention component of both conditions lasted for approximately 50 minutes and was completed in a single session. Self-report questionnaires were administered during laboratory visits one week and one month following the intervention appointment to assess changes in relevant tolerance and symptom variables. All participants were retained at the one week follow-up, and all but one participant (active condition) were retained at the one month follow-up Participants were provided course credit for their participation. All study procedures were approved by the university’s Institutional Review Board. For a more detailed description of the intervention and study design please see Keough and Schmidt (2012).
Data Analytic Plan
Descriptive statistics were first computed for all variables. Outliers were examined and corrected if they were +/− 3 SD from the mean. Following this, skew and kurtosis values were examined for problematic values and transformations were conducted if necessary. Scores were considered significantly skewed or kurtotic if skew over standard error of skew exceeded 1.98 (Tabachnick & Fidell, 2007). Although it is now generally agreed that a significant indirect path, from the independent variable to the dependent variable through the mediator is the only requirement necessary to demonstrate mediation (Preacher & Hayes, 2008; Zhao, Lynch Jr., & Chen, 2010), direct effects of the intervention (1 = PHET [control]; 2 = ASERT [active]) on the potential mediator variables (i.e., ASI-3, DIS, and DTS scores) at week 1, controlling for baseline levels, as well as the outcome variables (i.e., PSWQ, BAI, and BDI-2 scores) at month 1, controlling for baseline levels, were first examined in a series of regression analyses conducted in SPSS version 18.1.
Finally, mediation analysis was conducted in Mplus version 5.1 (Muthen & Muthen, 1998–2011). Mediation models were conducted using maximum likelihood estimation with bootstrapped (5000 samples) asymmetric confidence intervals (CIs) for indirect effects. Overall model fit was assessed using the likelihood ratio test, based on the χ2 value with a nonsignificant value indicating good model fit. The comparative fit index (CFI) and root mean square error of approximation (RMSEA), which are considered approximate fit indices, were also provided. CFI values greater than .95 indicate good fit. RMSEA values less than .05 indicate good fit and values less than .08 indicate adequate fit (Hu & Bentler, 1999; MacCallum, Browne, & Sugawara, 1996). Mediation was examined for the effects of each mediator on all outcome variables separately. Following this, all significant mediation pathways were examined in a single multiple mediation model (Preacher & Hayes, 2008) to determine the unique effects of each mediator on each outcome variable. In all mediation models, pre-intervention scores of each variable were used as covariates on all concordant follow-up scores. Mediation results are reported in unstandardized values by convention.
Results
Descriptive Statistics
The analyses were conducted on participants with elevated ASI, randomized at the intervention session. There was very little missing data (i.e., one missing value for pre-intervention ASI-3, month 1 BAI, and month 1 BDI-2 scores, and two missing values for month 1 PSWQ scores) and there were no significant differences on variables used in the current study for those who did and did not have missing data. Because there were so few participants with missing data, listwise deletion was used for the regression analyses. Full information maximum likelihood was used to handle missing data in the mediation analysis. Results of the mediation analyses were not substantively different when the analyses were conducted excluding participants with any missing data. Means and correlations for all variables are included in Table 1. Outliers were examined across groups at pre-intervention and within groups (i.e., PHET and ASERT) at post-intervention (i.e., week 1 for ASI-3, DIS, and DTS scores and month 1 for PSWQ, BAI, and BDI-2 scores). There was one value greater than 3 SD for pre-intervention BAI and BDI-2 scores. There were two values greater than 3 SD for week 1 ASI-3 scores and one value each in the month 1 BAI and BDI-2 scores in the ASERT condition. All outliers were brought in to 3 SD above the mean. Following this procedure, several variables were significantly positively skewed, including ASI-3, BAI, and BDI-2 scores at pre-intervention and follow-up (i.e., week 1 for ASI-3 and month 1 for BAI and BDI-2). Based on their distributions, square root transformations were deemed appropriate to reduce the effects of skew. Following these corrections, all variables were within acceptable ranges for skew and kurtosis. Analyses of variance models for pre-intervention scores revealed no significant mean differences between PHET and ASERT across all variables.
Table 1.
Descriptive Statistics for Potential Mediators and Anxiety and Depression at Pre-Intervention, Week 1, and Month 1 Follow-up
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Pre-Int ASI-3 | -- | |||||||||||
| 2. | Pre-Int DIS | .30* | -- | ||||||||||
| 3. | Pre-Int DTS | −.58* | −.24* | -- | |||||||||
| 4. | Pre-Int PSWQ | .52* | .32* | −.65* | -- | ||||||||
| 5. | Pre-Int BAI | .55* | .26* | −.58* | .54* | -- | |||||||
| 6. | Pre-Int BDI-2 | .57* | .17 | −.57* | .57* | .62* | -- | ||||||
| 7. | W1 ASI-3 | .72* | .22* | −.45* | .36* | .33* | .47* | -- | |||||
| 8. | W1 DIS | .29* | .77* | −.24* | .29* | .25* | .17 | .27* | -- | ||||
| 9. | W1 DTS | −.50* | −.27* | .77* | −.55* | −.44* | −.53* | −.63* | −.31* | -- | |||
| 10. | M1 PSWQ | .59* | .28* | −.67* | .83* | .49* | .61* | .58* | .24* | −.66* | -- | ||
| 11. | M1 BAI | .60* | .18 | −.47* | .40* | .55* | .53* | .66* | .23* | −.54* | .52* | -- | |
| 12. | M1 BDI-2 | .61* | .20* | −.53* | .54* | .49* | .78* | .57* | .24* | −.55* | .63* | .63* | -- |
| PHET Mean | 27.96 | 13.67 | 44.08 | 54.92 | 14.60 | 12.00 | 25.27 | 14.19 | 45.54 | 54.08 | 12.22 | 10.84 | |
| PHET SD | 12.26 | 5.37 | 11.69 | 13.56 | 9.11 | 9.69 | 12.83 | 4.87 | 12.80 | 14.20 | 10.35 | 11.13 | |
| ASERT Mean | 27.88 | 13.87 | 44.19 | 57.77 | 15.63 | 10.83 | 15.12 | 13.63 | 50.87 | 51.41 | 7.83 | 8.02 | |
| ASERT SD | 12.37 | 5.14 | 11.81 | 12.31 | 10.26 | 8.71 | 10.70 | 5.25 | 13.13 | 14.16 | 7.06 | 9.04 | |
Note. N = 101-104 across variables. Pre-Int = Pre-Intervention. W1 = Week 1. M1 = Month 1. ASI-3 = Anxiety Sensitivity Index-3. DIS = Discomfort Intolerance Scale. DTS = Distress Tolerance Scale. PSWQ = Penn State Worry Questionnaire. BAI = Beck Anxiety Index. BDI-2 = Beck Depression Inventory-2.
p < .05.
Direct Effects of Intervention Condition on Mediators and Anxiety and Depression
Results from the regression analyses conducted on the mediator and outcome variables are provided in Table 2. For the mediator variables, direct effects were found for the intervention on week 1 ASI-3 scores (β = −.41, p < .001) and on week 1 DTS scores (β = .20, p < .001). There was no significant effect of the intervention on week 1 DIS scores (β = −.07, p = .27). For the outcome variables, direct effects were found for the intervention on month 1 PSWQ scores (β = −.16, p < .01) and month 1 BAI scores (β = −.25, p < .01). However, there was only a marginally significant direct effect of the intervention on month 1 BDI-2 scores (β = −.10, p < .10).
Table 2.
Regression Analyses of Mediator and Outcome Variables
| Predictors | Follow-Up Variable | |
|---|---|---|
| ASI-3 | ||
| β | ||
| Intervention Condition | −.41 *** | |
| Pre-Intervention ASI-3 | .71 *** | |
| DIS | ||
| Intervention Condition | −.07 | |
| Pre-Intervention DIS | .77 *** | |
| DTS | ||
| Intervention Condition | .20 *** | |
| Pre-Intervention DTS | .77 *** | |
| PSWQ | ||
| Intervention Condition | −.16 ** | |
| Pre-Intervention PSWQ | .84 *** | |
| BAI | ||
| Intervention Condition | −.25 ** | |
| Pre-Intervention BAI | .56 *** | |
| BDI-2 | ||
| Intervention Condition | −.10 | |
| Pre-Intervention BDI-2 | .78 *** | |
Note. ASI-3 = Anxiety Sensitivity Index-3. DIS = Discomfort Intolerance Scale. DTS = Distress Tolerance Scale. PSWQ = Penn State Worry Questionnaire. BAI = Beck Anxiety Inventory. BDI-2 = Beck Depression Inventory-2.
p < .001,
p < .01.
Mediation Effects on Anxiety and Depression
Given these findings, independent mediation models were conducted including ASI-3 scores and DTS scores as mediators. DIS scores were not included as there was not a significant direct effect of intervention condition on DIS scores.1 BDI-2 scores were included as the direct effect was marginal and current practice in mediation analysis does not require a direct effect on the dependent variable to test for mediation effects (e.g., Zhao et al., 2010). The mediation model including the effect of the intervention on month 1 PSWQ, BAI, and BDI-2 scores mediated through week 1 ASI-3 scores provided good fit to the data (χ2 = 13.65, p = .32, CFI = 1.00, RMSEA = .04). Unstandardized model parameters with confidence intervals are provided in Table 3. In this model, there was a significant indirect effect from intervention condition through week 1 ASI-3 scores to month 1 PSWQ scores (B = −3.56, 95% CI [−5.58, −2.02]). There was also a significant indirect effect from intervention condition to month 1 BAI scores (B = −.60, 95% CI [−.88, −.41]) and to month 1 BDI-2 scores (B = −.37, 95% CI [−.68, −.10]) via week 1 ASI-3 scores. Across all mediation pathways, the effect of the intervention condition on month 1 scores was no longer significant (no longer marginally significant for BDI-2 scores).
Table 3.
Mediation Model through Anxiety Sensitivity Index-3 Scores at Week 1: Intervention Condition on Penn State Worry Questionnaire, Beck Anxiety Inventory, and Beck Depression Inventory-2 Scores at Month 1
| Month 1 PSWQ | Month 1 BAI | Month 1 BDI-2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Indirect | 95% CI | Indirect | 95% CI | Indirect | 95% CI | ||||
| Lower | Upper | Lower | Upper | Lower | Upper | ||||
| Pre-Int Score | .80 | .66 | .93 | .40 | .23 | .56 | .78 | .58 | .96 |
| Condition | −.42 | −3.40 | 2.69 | −.04 | −.46 | .38 | .03 | −.53 | .51 |
| ASI-3 Score | 3.08 | 1.88 | 4.21 | .52 | .38 | .69 | .32 | .07 | .53 |
| Indirect Effect | −3.56 | −5.58 | −2.02 | −.60 | −.88 | −.41 | −.37 | −.68 | −.10 |
Note. PSWQ = Penn State Worry Questionnaire. BAI = Beck Anxiety Inventory. BDI-2 = Beck Depression Inventory-2. ASI-3 = Anxiety Sensitivity Index-3. Pre-Int Score = Concordant pre-intervention score. CI = Confidence interval. Significant effects are in bold.
The mediation model including the effect of the intervention on month 1 PSWQ, BAI, and BDI-2 scores mediated through week 1 DTS scores provided good fit to the data (χ2 = 14.76, p = .26, CFI = .99, RMSEA = .05). Unstandardized model parameters with confidence intervals are provided in Table 4. In this model, there were significant indirect effects from intervention condition through week 1 DTS scores to month 1 PSWQ scores (B = −1.20, 95% CI [−2.85, −.22]), month 1 BAI scores (B = −.19, 95% CI [−.34, −.08]) and month 1 BDI-2 scores (B = −.13, 95% CI [−.31, −.02]). Across the mediation pathways to month 1 PSWQ and BDI-2 scores, the effect of the intervention condition on month 1 scores was no longer significant. The effect of the intervention on month 1 BAI scores remained significant (B = −.49, 95% CI [−.90, −.06]).
Table 4.
Mediation Model through Distress Tolerance Scale Scores at Week 1: Intervention Condition on Penn State Worry Questionnaire, Beck Anxiety Inventory, and Beck Depression Inventory-2 Scores at Month 1
| Month 1 PSWQ | Month 1 BAI | Month 1 BDI-2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Indirect | 95% CI | Indirect | 95% CI | Indirect | 95% CI | ||||
| Lower | Upper | Lower | Upper | Lower | Upper | ||||
| Pre-Int Score | .79 | .60 | .96 | .44 | .25 | .60 | .78 | .56 | .98 |
| Condition | −2.96 | −5.77 | .15 | −.49 | −.90 | −.06 | −.23 | −.67 | .19 |
| DTS Score | −.23 | −.40 | −.06 | −.04 | −.05 | −.02 | −.03 | −.05 | −.001 |
| Indirect Effect | −1.20 | −2.85 | −.22 | −.19 | −.34 | −.08 | −.13 | −.31 | −.02 |
Note. PSWQ = Penn State Worry Questionnaire. BAI = Beck Anxiety Inventory. BDI-2 = Beck Depression Inventory-2. DTS = Distress Tolerance Scale. Pre-Int Score = Concordant pre-intervention score. CI = Confidence interval. Significant effects are in bold.
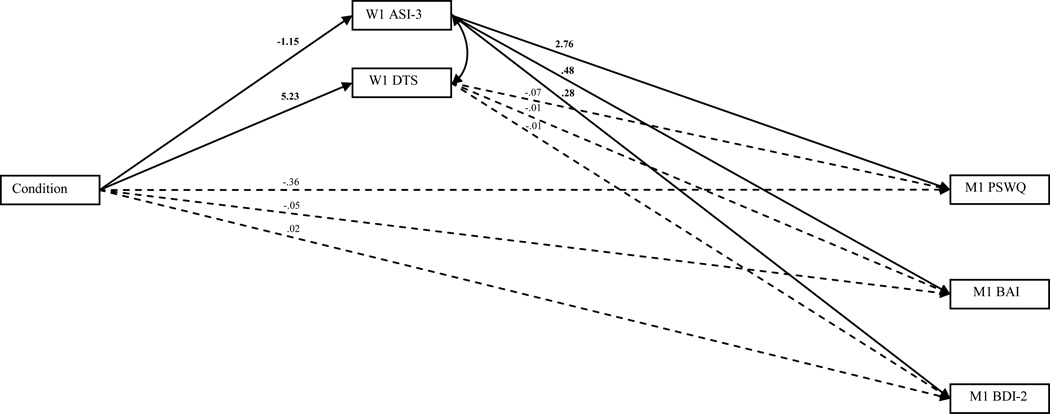
Finally, the unique effects of mediation pathways from intervention condition to month 1 PSWQ, BAI, and BDI-2 scores through week 1 ASI-3 and DTS scores were examined by a multiple mediation model including both mediation pathways (see Figure 1). This model provided exceptional fit to the data (χ2 = 19.51, p = .49, CFI = 1.00, RMSEA = .00). For month 1 PSWQ scores, only the mediation effect from intervention condition through week 1 ASI-3 scores remained significant (B = −3.18, 95% CI −5.16, −1.70]). For month 1 BAI scores, only the mediation effect from intervention condition through week 1 ASI-3 scores remained significant (B = −.55, 95% CI −.83, −.33]). Finally, the same pattern was found for month 1 BDI-2 scores, as only the mediation pathway through week 1 ASI-3 scores remained significant (B = −.32, 95% CI −.61, −.05]).
Figure 1.
Multiple mediation model examining the effects of intervention condition (i.e., 1 = PHET, 2 = ASERT) on month 1 PSWQ, BAI, and BDI-2 scores through ASI-3 and DTS scores at week 1. ASI-3 = Anxiety Sensitivity Index-3. DTS = Distress Tolerance Scale. PSWQ = Penn State Worry Questionnaire. BAI = Beck Anxiety Index. BDI-2 = Beck Depression Inventory-2. Nonsignificant pathways are represented by the dashed lines. Baseline levels of the mediators and outcome variables (omitted from the figure) were controlled for in the analysis.
Discussion
The current study provides an initial investigation of the effects of a computer-assisted AS intervention on other tolerance constructs (i.e., DT and DI) as well as symptoms of anxiety, worry, and depression. In line with our hypothesis, the AS intervention significantly decreased AS (as reported in Keough & Schmidt, 2012) and significantly increased DT while not significantly affecting DI at the week 1 follow-up. These results are conceptually consistent with previous studies that have found AS and DT to be more closely related than AS and DI (Bernstein et al., 2009; Mitchell et al., 2013).
In support of our hypothesis, the AS intervention significantly decreased symptoms of anxiety, worry, and depression, although only marginally for depression, at the month 1 follow-up. These findings are consistent with previous work finding single-session AS interventions to be efficacious in the amelioration of anxiety and mood symptoms (Mitchell et al., 2014; Schmidt et al., in press), although the marginal direct effects on depression may indicate that the intervention is more efficacious in treating anxiety symptoms than mood symptoms. Further, these reductions in anxiety, worry, and depression were statistically mediated by both prior changes in AS and prior changes in DT when considered separately, improving upon prior studies that did not temporally parse changes in mediators/outcomes or examine other affect tolerance variables in separate models (Schmidt et al., in press; McHugh et al., 2014). However, when changes in AS and changes in DT were considered as competing mediators only the indirect pathways via AS remained significant for all psychopathology variables. These results provide strong evidence that the manner in which the AS intervention improves symptom expression is indeed through AS, per se, and not through other related constructs.
The current study provides important information for our theoretical understanding of both the relationships between these tolerance constructs and how interventions that target AS affect anxiety and mood symptoms. The two main conceptual models of the relationships between AS, DT, and DI agree on the distinction between emotional (AS and DT) and physical tolerance (DI), however, one model posits AS to be a lower order facet of DT (Mitchell et al., 2013) while the other considers AS and DT to be parallel lower order facets of a higher emotional tolerance (Bernstein et al., 2009). If AS is a lower order facet of DT, than an efficacious AS intervention should also impact DT, but if AS and DT have a parallel relationship a circumscribed AS intervention would not necessarily impact DT. The results of our study clearly support AS as a lower order facet of DT given the significant changes in DT due to the intervention, however, a parallel relationship between AS and DT is not necessarily precluded by these results. It is important to note that this logic only holds if the intervention is truly circumscribed to AS.
With regard to the mechanisms through which the AS intervention affects symptoms of anxiety, worry, and depression it is clear from these results that although the AS intervention improved participants’ DT, symptom amelioration at follow-up did not occur via these changes. Therefore it is possible that reductions in DT, in the context of reductions in AS, are redundant with regard to symptom amelioration. However, further research examining the specific subfactors (i.e., tolerance, absorption, appraisal, regulation; Simons & Gaher, 2005) of DT that are affected by an AS intervention would be worthwhile. It is possible that there are subfactors of DT that were unaffected by the AS intervention and these unaffected subfactors could serve as appropriate targets for supplemental intervention components that could result in additional symptom reduction. As the intervention did not reduce DI it seems that targeting DI via a separate intervention component could also result in symptom reduction, although specific techniques for reducing DI have not yet been established. It is possible that repeated exposure to physical tolerance tasks (e.g., cold pressor immersion) could result in lower DI. Researchers should investigate whether an intervention targeting emotional (AS, DT) and physical (DI) tolerance is superior to targeting emotional tolerance in isolation.
It is important to note a few of the limitations of the current study. One of the main limitations of the current study is the reliance on self-report measures of tolerance constructs and symptoms, leaving open method variance concerns. Using a more integrated approach by including neurophysiological and/or behavioral indicators would provide a more balanced assessment (see Leyro et al., 2010 for a review). Despite the presence of a follow-up assessment to see changes in symptoms over time, this period was relatively short (i.e. 1 month). Future research should investigate the effects of an AS focused intervention over a longer duration. Although there were a significant number of individuals in the present sample who met criteria for an Axis-I diagnosis (i.e., 45%, see Keough & Schmidt, 2012 for a detailed report) the majority of the sample was sub-threshold. Schmidt et al. (in press) and Mitchell et al. (2014) examined the effects of an AS cognitive concerns intervention in a sample with greater diagnostic rates, but it would be interesting to investigate the effects of a more global AS intervention (e.g., ASERT) in a more severe sample. Finally, it will be important to investigate the effects of an AS intervention on other theoretically relevant tolerance constructs such as frustration tolerance or intolerance of uncertainty (Leyro et al., 2010).
Despite these limitations, this study significantly advances the current literature by examining the effects of an AS focused intervention on other tolerance constructs (i.e., DT and DI) and the mediational pathways through which such an intervention causes change in psychopathological symptoms. As we move forward it will be important for investigators to continue to elucidate the specific mechanisms of efficacious interventions in order refine our treatments to provide the most efficient care possible.
Highlights.
We investigated the effects of an anxiety sensitivity (AS) intervention.
The intervention reduced AS and increased distress tolerance (DT).
The intervention reduced symptoms of anxiety, worry, and depression.
AS and DT both mediated changes in symptom variables.
When considered in the same model, only the AS mediation remained.
Acknowledgements
This investigation was supported in part by National Institutes of Mental Health Award (1F31 MH086174-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Mediation models including week 1 DIS scores were examined and, as expected, were found not to be significant.
Contributor Information
Aaron M. Norr, Email: norr@psy.fsu.edu.
Nicholas P. Allan, Email: allan@psy.fsu.edu.
Richard J. Macatee, Email: macatee@psy.fsu.edu.
Meghan E. Keough, Email: mkeough@u.washington.edu.
Norman B. Schmidt, Email: schmidt@psy.fsu.edu.
References
- Allan NP, Macatee RJ, Norr AM, Schmidt NB. Direct and interactive effects of distress tolerance and anxiety sensitivity on generalized anxiety and depression. Cognitive Therapy and Research. (in press). [Google Scholar]
- Anestis MD, Gratz K, Bagge CL, Tull MT. The interactive role of distress tolerance and borderline personality disorder in suicide attempts among substance users in residential treatment. Comprehensive Psychiatry. 2012 doi: 10.1016/j.comppsych.2012.04.004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Epstein N, Steer RA. An inventory for measuring clinical anxiety - psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beekman ATF, de Beurs E, van Balkom AJLM, Deeg DJH, van Dyck R, van Tilburg W. Anxiety and depression in later life: Co-occurrence and communality of risk factors. The American Journal of Psychiatry. 2000;157:89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Pine DS, Lieb R, Wittchen H-U. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Archives of General Psychiatry. 2010;67:47–57. doi: 10.1001/archgenpsychiatry.2009.177. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Vujanovic AA, Moos R. Integrating anxiety sensitivity, distress tolerance, and discomfort intolerance: a hierarchical model of affect sensitivity and tolerance. Behavior Therapy. 2009;40:291–301. doi: 10.1016/j.beth.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Bernstein A. Discomfort intolerance: Evaluation of incremental validity for panic-relevant symptoms using 10% carbon dioxide-enriched air provocation. Journal of Anxiety Disorders. 2009;23:197–203. doi: 10.1016/j.janxdis.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Storey KM. Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety, Stress & Coping: An International Journal. 2008;21:117–128. doi: 10.1080/10615800701762675. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Keough ME, Schmidt NB. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors. 2007;32:1957–1963. doi: 10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capron DW, Norr AM, Macatee RJ, Schmidt NB. Distress Tolerance and Anxiety Sensitivity Cognitive Concerns: Testing the Incremental Contributions of Affect Dysregulation Constructs on Suicidal Ideation and Suicide Attempt. Behavior Therapy. 2013;44:349–358. doi: 10.1016/j.beth.2012.12.002. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Enns MW, Freeman P, Walker JR. Anxiety sensitivity and major depression: examination of affective state dependence. Behaviour Research and Therapy. 2001;39:1349–1356. doi: 10.1016/s0005-7967(00)00106-6. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Taylor S, Enns MW. Fear of cognitive dyscontrol in relation to depression symptoms: comparisons between original and alternative measures of anxiety sensitivity. Journal of Behavior Therapy and Experimental Psychiatry. 1999;30:301–311. doi: 10.1016/s0005-7916(99)00026-9. [DOI] [PubMed] [Google Scholar]
- de Graaf R, Bijl RV, Smit F, Vollebergh WAM, Spijker J. Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: Findings from the Netherlands Mental Health Survey and Incidence Study. The American Journal of Psychiatry. 2002;159:620–629. doi: 10.1176/appi.ajp.159.4.620. [DOI] [PubMed] [Google Scholar]
- Dennhardt AA, Murphy JG. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors. 2011;25:595–604. doi: 10.1037/a0025807. [DOI] [PubMed] [Google Scholar]
- DeVellis RF. Scale development: Theory and applications. 2 ed. Thousand Oaks California: Sage; 2003. [Google Scholar]
- Ellis AJ, Fischer KM, Beevers CG. Is dysphoria about being red and blue? Potentiation of anger and reduced distress tolerance among dysphoric individuals. Cognition and Emotion. 2010;24:596–608. [Google Scholar]
- Feldner MT, Zvolensky MJ, Babson K, Leen-Feldner EW, Schmidt NB. An integrated approach to panic prevention targeting the empirically supported risk factors of smoking and anxiety sensitivity: Theoretical basis and evidence from a pilot project evaluating feasibility and short-term efficacy. Journal of Anxiety Disorders. 2008;22:1227–1243. doi: 10.1016/j.janxdis.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardenswartz CA, Craske MG. Prevention of panic disorder. Behavior Therapy. 2001;32:725–737. [Google Scholar]
- Gorka SM, Ali B, Daughters SB. The role of distress tolerance in the relationship between depressive symptoms and problematic alcohol use. Psychology of Addictive Behaviors. 2012;26:621–626. doi: 10.1037/a0026386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant DM, Beck JG, Davila J. Does anxiety sensitivity predict symptoms of panic, depression, and social anxiety? Behaviour Research and Therapy. 2007;45:2247–2255. doi: 10.1016/j.brat.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Huang K, Szabó M, Han J. The relationship of low distress tolerance to excessive worrying and cognitive avoidance. Behaviour Change. 2009;26:223–234. [Google Scholar]
- Kapson HS, Leddy MA, Haaga DAF. Specificity of effects of cognitive behavior therapy on coping, acceptance, and distress tolerance in a randomized controlled trial for smoking cessation. Journal of Clinical Psychology. 2012;68:1231–1240. doi: 10.1002/jclp.21903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychological Medicine. 2007;37:453–462. doi: 10.1017/S0033291706009135. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, stressful life events in the prediction of episodes of major depression. The American Journal of Psychiatry. 2004;161:631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety symptomatology: the association with distress tolerance and anxiety sensitivity. Behavior Therapy. 2010;41:567–574. doi: 10.1016/j.beth.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keough ME, Schmidt NB. Refinement of a brief anxiety sensitivity reduction intervention. Journal of Consulting and Clinical Psychology. 2012:766–772. doi: 10.1037/a0027961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA: Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;136:576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotan G, Tanay G, Bernstein A. Mindfulness and distress tolerance: Relations in a mindfulness preventive intervention. International Journal of Cognitive Therapy. 2013;6:371–385. [Google Scholar]
- Macatee RJ, Capron DW, Guthrie W, Schmidt NB, Cougle JR. Emotion dysregulation in pathological worry: The roles of emotional reactivity, distress tolerance, and life stressors. Manuscript submitted for publication. 2013 [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- McHugh RK, Kertz SJ, Weiss RB, Baskin-Sommers AR, Hearon BA, Björgvinsson T. Changes in distress intolerance and treatment outcome in a partial hospital setting. Behavior Therapy. 2014;45:232–240. doi: 10.1016/j.beth.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer T, Miller M, Metzger R, Borkovec T. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mitchell MA, Capron DW, Raines AM, Schmidt NB. Reduction of cognitive concerns of anxiety sensitivity is uniquely associated with reduction of PTSD and depressive symptoms: A comparison of civilians and veterans. Journal of Psychiatric Research. 2014;48:25–31. doi: 10.1016/j.jpsychires.2013.10.013. [DOI] [PubMed] [Google Scholar]
- Mitchell MA, Riccardi CJ, Keough ME, Timpano KR, Schmidt NB. Understanding the associations among anxiety sensitivity, distress tolerance, and discomfort intolerance: A comparison of three models. Journal of Anxiety Disorders. 2013;27:147–154. doi: 10.1016/j.janxdis.2012.12.003. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne B, Melchior M, Goldberg D, Poulton R. Generalized anxiety disorder and depression: Childhood risk factors in a birth cohort followed to age 32 years. In: Goldberg D, Kendler KS, Sirovatka PJ, editors. Diagnostic issues in depression and generalized anxiety disorder: Refining the research agenda for DSM-V. Arlington, VA, US: American Psychiatric Association; 2010. pp. 217–239. [Google Scholar]
- Muthen LK, Muthen BO. Mplus User's Guide. 6th ed. Los Angeles, CA: Muthen & Muthen; 1998–2011. [Google Scholar]
- Norr AM, Oglesby ME, Capron DW, Raines AM, Korte KJ, Schmidt NB. Evaluating the unique contribution of intolerance of uncertainty relative to other cognitive vulnerability factors in anxiety psychopathology. Journal of Affective Disorders. 2013;151:136–142. doi: 10.1016/j.jad.2013.05.063. [DOI] [PubMed] [Google Scholar]
- Olthuis J, Watt MC, Mackinnon SP, Stewart SH. Telephone-delivered CBT for high anxiety sensitivity: A randomized controlled trial. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0037027. (in press). [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, Allan NP. Development and radomized clinical trial evaluating the efficacy of a brief intervention targeing cognitive anxiety sensitivity. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0036651. (in press). [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety Sensitivity Amelioration Training (ASAT): A longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders. 2007;21:302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Cromer KR, Buckner JD. Discomfort Intolerance: Evaluation of a Potential Risk Factor for Anxiety Psychopathology. Behavior Therapy. 2007;38:247–255. doi: 10.1016/j.beth.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Fitzpatrick KK. Discomfort intolerance: Development of a construct and measure relevant to panic disorder. Journal of Anxiety Disorders. 2006;20:263–280. doi: 10.1016/j.janxdis.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatric Research. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- Smits JAJ, Powers MB, Cho Y, Telch MJ. Mechanism of change in cognitive-behavioral treatment of panic disorder: Evidence for the fear of fear mediational hypothesis. Journal of Consulting and Clinical Psychology. 2004;72:646–652. doi: 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- Starr LR, Davila J. Responding to anxiety with rumination and hopelessness: Mechanism of anxiety-depression symptom co-occurrence? Cognitive Therapy and Research. 2012;36:321–337. doi: 10.1007/s10608-011-9363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Boston: Pearson Education; 2007. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Timpano KR, Buckner JD, Richey JA, Murphy DL, Schmidt NB. Exploration of anxiety sensitivity and distress tolerance as vulnerability factors for hoarding behaviors. Depression and Anxiety. 2009;26:343–353. doi: 10.1002/da.20469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Gratz KL. Further examination of the relationship between anxiety sensitivity and depression: The mediating role of experiential avoidance and difficulties engaging in goal-directed behavior when distressed. Journal of Anxiety Disorders. 2008;22:199–210. doi: 10.1016/j.janxdis.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Viana AG, Rabian B. Perceived attachment: Relations to anxiety sensitivity, worry, and GAD symptoms. Behaviour Research and Therapy. 2008;46:737–747. doi: 10.1016/j.brat.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Watt MC, Stewart SH, Birch CD, Bernier D. Brief CBT for high anxiety sensitivity decreases drinking problems, relief alcohol outcome expectancies, and conformity drinking motives: Evidence from a randomized controlled trial. Journal of Mental Health. 2006a;15:683–695. [Google Scholar]
- Watt MC, Stewart SH, Lefaivre M-j, Uman L. A brief cognitive-behavioral approach to reducing anxiety sensitivity decreases pain-related anxiety. Cognitive Behaviour Therapy. 2006b;35:248–256. doi: 10.1080/16506070600898553. [DOI] [PubMed] [Google Scholar]
- Williams AD, Thompson J, Andrews G. The impact of psychological distress tolerance in the treatment of depression. Behaviour Research and Therapy. 2013;51:469–475. doi: 10.1016/j.brat.2013.05.005. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Jr, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37:197–206. [Google Scholar]
- Zvolensky MJ, Schmidt NB, Bernstein A, Keough ME. Risk-factor research and prevention programs for anxiety disorders: A translational research framework. Behaviour Research and Therapy. 2006;44:1219–1239. doi: 10.1016/j.brat.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Leyro T. Distress tolerance: Theory, measurement, and relations to psychopathology. Current Directions in Psychological Science. 2010;19:406–410. doi: 10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]