Abstract
Objective
To examine whether self-medication with drugs confers risk of comorbid mood and drug use disorders.
Method
A longitudinal, nationally representative survey was conducted by the National Institute on Alcohol Abuse and Alcoholism. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) assessed DSM-IV psychiatric disorders, self-medication, and sociodemographic variables at two time points. A total of 34,653 adult, U.S. participants completed both waves of the survey. Wave 1 was conducted between 2001–2002 and Wave 2 interviews took place 3 years later (2004–2005). Logistic regression and population attributable fractions were calculated to obtain estimates of the association between self-medication and incident disorders.
Results
Logistic regression analyses revealed that self-medication with drugs conferred a heightened risk of new-onset drug dependence among those with baseline mood disorders [adjusted odds ratio (AOR)=7.65; 95% confidence interval (CI) 3.70–15.82, p<.001], and accounted for over 25% of incident drug dependence disorders among people with mood disorders. Among those with comorbid mood and drug use disorders at baseline, self-medication with drugs was associated with the persistence of drug abuse (AOR=2.47; 95%CI=1.34–4.56, p<0.01), accounting for over one-fifth of the persistence of drug use disorders at three year follow-up.
Conclusion
Self-medication with drugs amongst individuals with mood disorders confers substantial risk of developing incident drug dependence, and is associated with the persistence of comorbid mood and drug use disorders. These results clarify a pathway that may lead to the development of mood and drug use disorder comorbidity, and indicate an at-risk population with potential points of intervention for prevention of comorbidity.
Keywords: Self-medication, mood disorders, drug dependence, comorbidity, epidemiology
INTRODUCTION
Both mood disorders and substance use disorders occur frequently in the general population, with lifetime prevalence rates of approximately 15–20%.1 Individually, each set of disorders is associated with substantial disability, poor quality of life, and ineffective treatment for patients.2,3 While mood and substance use disorders are each common in their own right, they also co-occur frequently in the same individual.4–7 Approximately 20% of people with an alcohol or drug use disorder have a co-occurring mood disorder, and a similar proportion of individuals with a mood disorder also endorse symptoms and behaviors of a comorbid substance use disorder.5 Undoubtedly, the consequences of such comorbidity are considerable: individuals with two (or more) psychiatric conditions often report more severe symptomatology8, disability9, longer duration of illness10, and greater rates of mental health service utilization11, relative to a non-comorbid cohort.
While much is known about the negative consequences of co-morbidity, the underlying cause of mental illness/substance use disorder co-occurrence has received less research attention. One etiologic theory to account for the relationship between mood and substance use disorder co-morbidity asserts that a direct causal relationship leads one disorder to predispose an individual to develop a second disorder.12 The “self-medication” or “tension-reduction” theory13, focuses on the use of alcohol or drugs as a method of self-medicating, or coping, with affective symptoms. Historically, this theory has been used to account for the comorbidity found in alcohol use and anxiety disorders14–18, and is exemplary of such a direct causal relationship. Other authors (e.g. Markou et al19, Swan20) have examined the self-medication theory in the context of mood and substance use disorder co-morbidity and have postulated similar underlying neurological substrates and common mechanisms that may help to explain the coalescence of these two groups of conditions.
Although a frequently considered hypothesis, there is relatively little known about the use of drugs or prescription medications to self-medicate depressive or other mood symptoms in population-based samples. Population-based studies are less affected by selection bias that influences clinical samples. Previous studies of the National Epidemiological Survey of Alcohol and Related Conditions (NESARC) dataset have examined self-medication using cross-sectional assessments of co-occurring conditions21–23 and found strong associations of using alcohol and drugs to self-medicate mood disorders with comorbid psychopathology. We aimed to extend these analyses using longitudinal information from both Waves 1 and 2 of the NESARC, in order to assess the temporal association of using drugs and prescription medications to self-medicate mood symptoms with the subsequent new onset of drug use disorders (i.e. drug abuse and drug dependence). Our primary goal was to assess whether self-medication of affective symptoms with drugs would be associated with an increase in the incidence of drug use disorders over time. We hypothesized that individuals who reported using drugs to self-medicate negative mood symptoms at baseline would be at increased risk for the new development of drug use disorders at the time of the follow-up interview. We further examined whether self-medication is associated with comorbidity among people with neither disorder at baseline, or with persistence of comorbidity among individuals with both mood and drug use disorders at baseline.
A secondary objective of the study was to examine whether self-medication of subthreshold mood symptoms among people with drug use disorders at baseline predicted incident mood disorders. Based on previous cross-sectional studies showing a high prevalence of self-medication in mood disorders21, we hypothesize that this behavior will be associated with higher rates of co-morbid mental illness.
METHODS
SAMPLE
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is a longitudinal, nationally representative survey conducted by the National Institute of Alcohol Abuse and Alcoholism (NIAAA). Wave 1 of the NESARC occurred between 2001 and 2002 and consisted of a total of 43,093 respondents from the United States adult, non-institutionalized population. Wave 2 of the NESARC was carried out between 2004 and 2005 and yielded a total sample of 34,653 respondents who had also taken part in Wave 1. The overall response rate was 70.2%. The sampling frame of the NESARC was based on the US Bureau of the Census Supplementary Survey data, and has been described in greater detail elsewhere.24 Respondents were contacted in writing, informed of the nature of the survey and its potential uses, and were ensured of confidentiality and told that participation was voluntary. The ethics protocol for the NESARC was reviewed and approved by the U.S. Census Bureau and the U.S. Office of Management and Budget. Data were weighted to account for sampling biases and to ensure representativeness of the U.S. population based on the 2000 Census. Additional information about the NESARC sampling design and methodology is available elsewhere.25
MEASURES
Sociodemographic Variables
Eight sociodemographic variables were assessed at Wave 1 of the NESARC. These included: gender, annual household income, ethnicity, age, region of residence, marital status, education and urban status. Annual income was divided into four categories ($0-$19,999; $20,000–$34,999; $35,000–$59,999; and $60,000+), as were ethnicity (White, Black, Native American or Asian, and Latino or Hispanic), age (18–29, 30–44, 45–64, and 65+), and region (Northeast, Midwest, South, and West). Marital status was classified as one of: (1) married/cohabitating, (2) divorced/separated/widowed, or (3) never married. Education was categorized as (1) less than high school, (2) high school, and (3) some college or higher. Urban status classified participants into either (1) urban or (2) rural groups.
Assessment of Mental Disorders
The Alcohol Use Disorders and Associated Disabilities Interview Schedule IV (AUDADIS-IV)26 generated diagnoses in accordance with the diagnostic and statistical manual of mental disorders (DSM-IV-TR).27 The reliability and validity of the AUDADIS-IV ranges from good to excellent across diagnoses.28 Lifetime and past-year diagnoses consisted of mood (dysthymia, mania, hypomania and depression), anxiety (panic disorder, social phobia, specific phobia and generalized anxiety disorder), and substance use disorders (alcohol and drug abuse and dependence). Specific medicines or drugs inquired about included sedatives (e.g. sleeping pills, barbiturates, chloral hydrate), tranquilizers (e.g. benzodiazepines), opioid painkillers (e.g. codeine, Demerol), amphetamines (e.g. Benzadrine, Mehadrine), cannabis, and cocaine. Lifetime diagnoses also included personality disorders (paranoid, schizoid, schizotypal, antisocial, borderline, histrionic, narcissistic, avoidant, dependent, and obsessive-compulsive). In order to receive a particular diagnosis, participants had to endorse the minimum number of symptoms in accordance with DSM-IV. The Wave 1 interview measured presence of axis I disorders at any point in the lifetime as well as within the past year. Interviews at Wave 2 measured presence of axis I disorders in the past year and at any point in the three-year interval between surveys. New onset (incident) disorders were defined by excluding those who met criteria for the disorder at any point in their lifetime (at Wave 1 interview), and including those who met criteria for the disorder in the Wave 2 three-year interval. For the aggregate “any” incident disorder categories, those who met criteria for any one of the individual disorders assessed at baseline (for example, any of the four mood disorders – dysthymia, mania, hypomania and depression) were excluded.
Self-Medication
Self-medicating behavior was assessed at the Wave 1 survey within four different mood disorder categories (dysthymia, mania, hypomania and depression). Participants who endorsed a minimum number of mood symptoms were asked if at any time in the past they had used drugs for the purpose of ameliorating mood symptoms. For example, the following item was used to assess self-medication of depressive symptoms: “Did you ever take any medicines or drugs on your own, that is, without a prescription or in greater amounts, or more often or longer than prescribed to help improve your mood or to make yourself feel better when you felt sad, blue, depressed, or down/didn’t care about or enjoy things?” Responses to self-medication questions were coded as either “yes” or “no”. Participants who answered “no” to the self-medication question (among those who endorsed sufficient mood symptoms to warrant asking this question) were set as the reference category in logistic regression analyses. Individuals who engaged in self-medication only with alcohol were excluded from the analyses.
STATISTICAL ANALYSES
Suitable statistical weights were applied to ensure representativeness of the NESARC data. Due to the complex sampling design of the NESARC, SUDAAN’s Taylor Series Linearization was utilized in the calculation of standard error estimates.29 Cross-tabulation and frequency calculations were conducted to determine descriptive information on sociodemographic and incident mental disorder variables for the entire NESARC sample. Prevalence was estimated for individuals who used any drugs in the past year and reported self-medication at Wave 1. Descriptive statistics and population attributable fractions (PAFs) were calculated, and multiple logistic regression analyses were performed, in order to obtain information on self-medication within each subpopulation of interest in the current study. In each regression analysis conducted in the current study, self-medication was set as the dependent variable and models were adjusted for sociodemographics and Wave 1 lifetime co-morbidity (axis I and II disorders).
Firstly, among those diagnosed with any lifetime mood disorder at Wave 1, regression analyses were conducted to examine the impact of endorsement of self-medication with drugs on incident drug use disorders. The two drug use disorders (drug abuse and dependence) were examined in separate analyses, as was a summary variable (“any drug use disorder”). The proportion of incident disorders that could be attributed to self-medication within mood disorders was calculated using population attributable fractions (PAFs).
Secondly, among those diagnosed with a lifetime drug use disorder at Wave 1, regression analyses were conducted to examine the impact of endorsement of self-medication with drugs on incident mood disorders. Among those with drug use disorders at baseline, separate models were tested with each individual incident mood disorder as independent variables. An “any incident mood disorder” model was also tested. PAFs were calculated to determine the proportion of incident mood disorders that were attributable to self-medication with drugs among those with lifetime drug use disorders at baseline.
Among participants with both mood and drug use disorders in the past year at baseline, the effect of self-medication with drugs on the persistence of each disorder was calculated with logistic regression analyses. Similar regression and PAF analyses were also performed within the population of individuals who did not meet criteria for a mood disorder or drug use disorder at Wave 1 in order to determine the effect of self-reported self-medication with drugs on the development of either incident drug use disorders or mood disorders. Crosstabulation analyses were performed to determine the frequency of use of each specific drug at Wave 1, and the frequency of dependence by drug type at Wave 2, among individuals who self-medicated their mood symptoms and later became dependent on drugs.
RESULTS
Table 1 presents information on sociodemographic characteristics in the total NESARC sample. Approximately 2.0% of the Wave 2 sample met criteria for new-onset drug use disorders (1.1% for incident drug abuse, and 0.8% for incident drug dependence).
Table 1.
Wave 1 Sociodemographic Characteristics and Wave 2 Incident Mental Disorders among the entire NESARC Sample
| Entire NESARC Sample n = 34653 |
|
|---|---|
| Sociodemographic Variables | n(%)1 |
| Gender | |
| Male | 14564 (47.9) |
| Female | 20089 (52.1) |
| Age | |
| 18–29 | 6719 (21.8) |
| 30–44 | 11013 (30.9) |
| 45–64 | 10917 (31.1) |
| 65+ | 6004 (16.2) |
| Ethnicity | |
| White | 20174 (70.9) |
| Black | 6577 (11.0) |
| American Indian/Alaskan | 580 (2.2) |
| Asian/Hawaiian | 966 (4.3) |
| Hispanic | 6356 (11.6) |
| Marital Status | |
| Married | 18413 (63.1) |
| Wid/Sep/Div | 8564 (16.5) |
| Never Married | 7676 (20.5) |
| Region | |
| Northwest | 6444 (19.7) |
| Midwest | 7540 (23.1) |
| South | 12833 (35.2) |
| West | 7836 (22.0) |
| Income | |
| $0–19 999 | 8959 (20.3) |
| $20 000–34 999 | 7309 (19.6) |
| $35 000–59 999 | 8812 (26.3) |
| $60 000+ | 9573 (33.8) |
| Education | |
| Less than high school | 5744 (14.6) |
| High school | 9955 (29.0) |
| Some college or more | 18954 (56.3) |
| Urbanicity | |
| Urban | 11672 (28.9) |
| Rural | 22981 (71.1) |
| Incident Disorders | |
| Incident drug abuse | 322 (1.1) |
| Incident drug dependence | 264 (0.8) |
| Incident drug use disorder | 586 (2.0) |
Percentages are weighted to account for sampling biases.
Crosstabulations were calculated among those with mood disorders and substance use to determine frequency of self-medication. Among individuals with a mood disorder who used any drugs in the past year, 38.1% reported self-medication with drugs. Among individuals with a co-morbid mood and drug use disorder at Wave 1, 34.2% of individuals reported self-medication with drugs.
Table 2 presents frequency distributions, adjusted odds ratios, and PAFs of incident drug use disorders among participants with any lifetime mood disorder (table 2 – top half), and among those with any lifetime mood disorder who engage in self-medication with drugs (table 2 – bottom half). Among individuals who met criteria for a baseline mood disorder, 3.0% developed an incident drug use disorder. Regression analyses revealed that among those with mood disorders at baseline, the risk of incident drug abuse and drug dependence was increased approximately two-fold relative to those without a lifetime mood disorder at baseline. Among individuals who met criteria for a baseline mood disorder and reported self-medication with drugs, 5.6% developed an incident drug use disorder. Regression analyses revealed that self-medication with drugs among those with mood disorders at baseline was associated with a substantially increased odds of incident drug dependence (AOR=7.65; 95% CI=3.70–15.82, p<0.001), independently of the effects of sociodemographic factors and comorbid psychiatric illness. One-quarter of new onset drug dependence disorders were attributable to self-medication.
Table 2.
Incident Drug Use Disorders among those with a History of any Lifetime Mood Disorder at Baseline (Wave 1), broken down by Self-Medication status
| Incident Drug Use Disorder |
Any Lifetime Mood Disorder | |||
|---|---|---|---|---|
| No (n = 27571) |
Yes (n = 7082)1 |
|||
| n(%)2 | n(%) | Adjusted Odds Ratio3 (95% Confidence Interval) |
PAF4 | |
| Drug Abuse (n=322) |
234 (1.0) | 88 (1.5) | 1.96 (1.51–2.56)*** |
1.46 (0.8–2.3) |
| Drug Dependence (n=264) |
166 (0.7) | 98 (1.6) | 2.066 (1.42–3.01)*** |
1.76 (0.7–3.1) |
| Any Drug Use Disorder (n=586) |
400 (1.6) | 186 (3.0) | 1.936 (1.53–2.42)*** |
2.76 (1.6–4.1) |
| Incident Drug Use Disorder |
Self-Medication of Lifetime Mood Disorder with Drugs1 | |||
| No (n = 5428) |
Yes (n = 546) |
|||
| n(%) | n(%) | Adjusted Odds Ratio (95% Confidence Interval) |
PAF | |
| Drug Abuse (n=67) |
65 (1.4) | 2 (0.5) | -- | -- |
| Drug Dependence (n=74) |
49 (1.1) | 25 (5.2) | 7.65 (3.70–15.82)*** |
25.7 (12.3–43.5) |
| Any Drug Use Disorder (n=141) |
114 (2.5) | 27 (5.6) | 4.11 (2.33–7.25)*** |
14.8 (6.9–25.9) |
7082 respondents met criteria for lifetime mood disorder at Wave 1. The bottom half of the table presents analyses of those that engaged in self-medication with drugs [and excluded those who used alcohol exclusively to self-medicate (n=1108)].
Percentages are weighted column percents (for example, among those who met criteria for baseline mood disorder, 1.5% developed incident drug abuse) and were weighted to account for sampling biases.
Odds ratios were adjusted for the following sociodemographic variables: gender, age, income, marital status, education level, ethnicity, region, and urban status as well as any lifetime psychiatric disorder at Wave 1.
Population Attributable Fraction.
Note: Only those who met criteria for any lifetime mood disorder at Wave 1 and did not meet criteria for the substance use disorder in question were included in these analyses.
p < .001
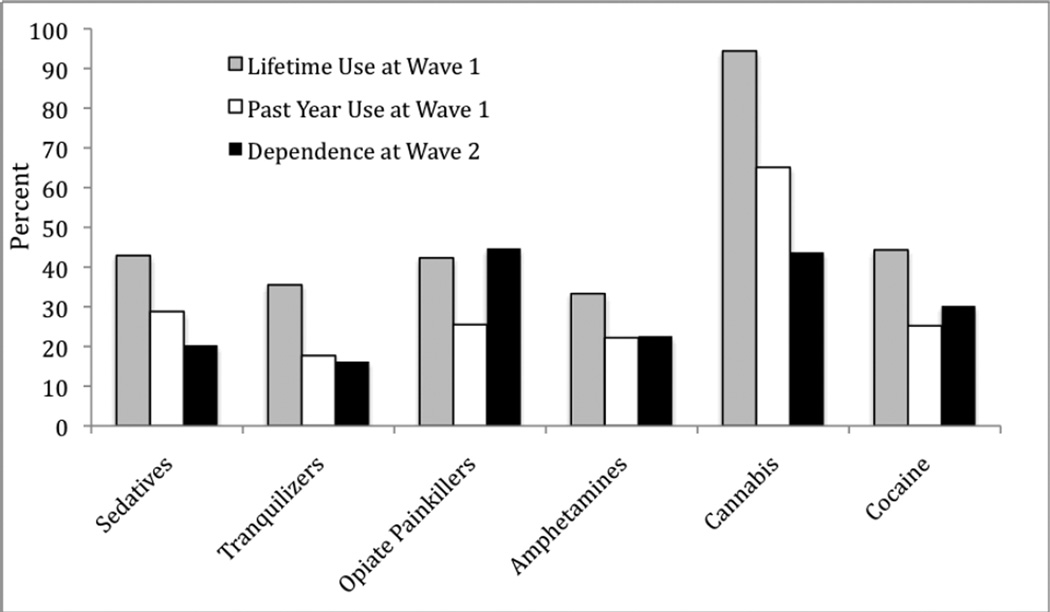
Figure 1 displays the types of drugs used at Wave 1 (both lifetime and past year) and the categories of drug dependence at Wave 2 among individuals with baseline mood disorders who endorsed self-medication with drugs at Wave 1 and subsequently developed drug dependence at Wave 2. When examined by drug class, the highest rates of dependence were observed for cannabis (43.7%) and opioid dependence (44.7%). Cannabis was commonly used by people who self-medicated mood symptoms at Wave 1; 94% had used cannabis at some point in their lifetime, with almost two-thirds (65%) using it within the past year. There were also high rates of prescription drug use among those who self-medicate, with almost half of them using sedatives and opioid painkillers in their lifetime. Interestingly, for amphetamines, cocaine, and in particular opioid painkillers, a relatively large proportion of those who reported lifetime or past year use of these substances at Wave 1 later went on to develop dependence at Wave 2, underscoring the addictive potential of these particular drug classes.
Figure 1.
The types of drugs used at Wave 1 and the categories of drug dependence at Wave 2 among individuals with baseline mood disorders who endorsed self-medication at Wave 1 and subsequently developed drug dependence at Wave 2 (n=25).
Among those with drug use disorders at baseline who reported using drugs to self-medicate lifetime sub-threshold mood symptoms, the prevalence of incident mood disorders ranged from 1.8% (dysthymic disorder) to 5.5% (bipolar disorder type I). Regression analyses revealed that self-medication with drugs was not significantly associated with any new onset mood disorders meeting DSM-IV criteria.
Table 3 presents frequency distributions, adjusted odds ratios, and population attributable fractions of persistent drug use disorders at Wave 2 among those with lifetime co-morbid mood and drug use disorders at baseline, who reported self-medication with drugs. Among those with co-morbid mood and drug use disorders at baseline, self-medication with drugs was associated with both the persistence of drug abuse (AOR=2.47; 95%CI=1.34–4.56, p<0.01), and the persistence of any drug use disorder (AOR=2.02; 95%CI=1.46–2.80, p<0.001). Population attributable fraction results suggests that self-medication accounted for over one-fifth of the persistence of drug use disorders at three year follow-up. Self-medication was not associated with the persistence of mood disorders among those with comorbidity at baseline.
Table 3.
Persistence of Drug Use Disorders among those with Co-morbid Mood and Drug Use Disorders at Baseline
| Persistence of Wave 2 Disorder |
Lifetime Wave 1 Mood and Drug Use Disorder Co-morbidity | |||
|---|---|---|---|---|
| Self-Medication with Drugs | ||||
| No (n=) |
Yes (n=) |
|||
| n(%)1 | n(%) | Adjusted Odds Ratio2 (95% Confidence Interval) |
PAF3 | |
| Drug Abuse (n=85) |
54 (7.3) | 31 (18.3) | 2.47 (1.34–4.56)** |
21.2 (5.9–39.4) |
| Drug Dependence (n=73) |
28 (13.6) | 45 (16.2) | 1.12 (0.63–1.99) |
1.9 (−6.4–13.8) |
| Any Drug Use Disorder (n=247) |
120 (13.0) | 127 (26.3) | 2.02 (1.46–2.80)*** |
21.2 (10.8–32.1) |
Percentages are weighted column percents. For example 7.3% of those who did not self-medicate (and met criteria for co-morbid mood and drug abuse disorders) continued to meet drug abuse criteria at follow-up.
Odds ratios were adjusted for the following sociodemographic variables: gender, age, income, marital status, education level, ethnicity, region, and urban status as well as any lifetime psychiatric disorder at Wave 1.
Population Attributable Fraction.
Note: In each regression analysis, the baseline population included those with mood disorders and the persistent drug use disorder of interest. For example, for persistent drug abuse, the baseline population consisted of those who met lifetime criteria for any mood disorder and for drug abuse.
p<.01;
p< .001
DISCUSSION
To our knowledge, the present study is the first to longitudinally demonstrate the role of self-medication with drugs in the genesis of incident drug use disorder comorbidity among people with mood disorders in a representative sample of the U.S. population. Although previous studies have demonstrated an association between substance use and mood disorders4–7, and have shown that the presence of a substance use disorder confers risk for the subsequent development of a mood disorder (and vice versa), the factors that mediate this relationship have been examined less frequently. The focus on individuals who self-medicate affective symptoms with drugs (both illicit and prescription) as opposed to alcohol is also a unique aspect of this study. The results of this study are novel in that self-medication is identified as a factor that underscores the risk of developing a co-morbid disorder in specific populations. Self-medication has generally been overlooked in the area of mood disorders, yet appears to be a common behavior with significant negative consequences. Our findings may have important clinical implications for patient assessment, and could provide a target for treatment efforts to attenuate or prevent future substance use disorder comorbidity.
The findings from this study indicate that among individuals with a mood disorder at baseline who use drugs to self-medicate their symptoms, the odds of developing a new-onset drug use disorder within the next 3 years increased up to 7-fold, relative to those with mood disorders who do not self-medicate. Over 25% of incident drug dependence diagnoses were found to be attributable to self-medication in this population. These findings persisted even after accounting for the effects of other mental disorders and numerous potentially confounding sociodemographic variables. The control of confounding effects and longitudinal design of this study provide new evidence in support of the self-medication hypothesis and suggest a potentially causative role in the etiology of mood and drug use disorder comorbidty. Furthermore, the strength of the association and high PAF value for incident drug dependence emphasize the importance of self-medication in comorbidity development. Our findings thus support the notion that self-medication is a behavior that substantially magnifies the risk of developing co-morbid drug use and mood conditions.
The results of this study also give us important clues as to the types of drugs utilized by those with mood disorders to self-medicate their affective symptoms, as well as the addictive potential of various substances. Our results show that cannabis is used commonly by those with mood disorders who engage in self-medication, prior to the development of a drug use disorder. Almost half of the people who then develop subsequent drug dependence become dependent on cannabis. Cannabis use in this population may be a double-edged sword: the potential of cannabis to exert antidepressant effects has been examined by some authors (e.g. Gruber et al30), as has the notion that heavy cannabis use exacerbates, rather than ameliorates, depressive symptoms31. Other substances such as amphetamines, cocaine, and opioid painkillers, although used less commonly than cannabis, are nonetheless used by individuals with mood disorders who attempt to self-medicate their affective symptoms. Our data support the notion that the addictive potential of these substances is significant in this population, since the frequency rates of past-year use at baseline are almost equivalent to the rates of new-onset drug dependence with these drugs at 3 years follow-up. Another important observation is that many of the incident drug dependence diagnoses among people who self-medicate are for prescription drugs. This finding suggests that physicians need to carefully assess and follow their mood disorder patients who self-medicate, since there is a high risk of developing dependence to commonly prescribed psychotropics and painkillers.
There are several limitations to this study that warrant mentioning. Firstly, only one explanatory mechanism (self-medication) was examined to elucidate the development of mood and drug use disorder co-morbidity. Other possible mechanisms, including hereditary and shared etiological factors, may also play an important role. Secondly, self-medication behavior was not objectively assessed. Responses to questions about self-medication were obtained by way of self-report, and may therefore be subject to recall bias. In addition, the short time period between the two surveys may not have been sufficient to capture the full extent of incident disorders that result from self-medicating; future longitudinal studies may aim to examine self-medication using a longer time-frame. Thirdly, a lack of experimental design precludes us from making definitive statements in regard to causality. Although Bradford Hill’s criteria32 of temporality, plausibility, and coherence are met by the current study design, there are other elements for establishing causality (e.g. strength of association and biological gradient) that are not addressed herein. Fourthly, certain populations (e.g. those under 18 years of age and those currently residing in institutional settings) were excluded from the NESARC survey, and our results may therefore not generalize to these individuals. Finally, the amount of substances used for self-medication, and frequency of self-medication, was not assessed in the NESARC survey. The quantity of drugs consumed is an important potential confounder since it is possible that those who use substances more frequently or in greater amounts will be more likely to develop incident drug use disorders. It is also possible that greater amounts of substance use could reflect other types of drug use motivations, in addition to self-medication. Future studies in this area should strive to mitigate these limitations and focus on possible clinical interventions that address self-medication of affective symptoms, with the aim of preventing subsequent psychiatric co-morbidity.
In conclusion, the results of this study support the notion that self-medication with drugs amongst individuals with mood disorders confers substantial risk of developing incident drug dependence. These results clarify a pathway that may lead to the development of mood and drug use disorder comorbidity, and indicate to clinicians an at-risk population. Careful inquiry about self-medication would appear warranted, as early detection and intervention could potentially prevent persistent mood and drug use disorder comorbidity for individual patients and reduce the overall public health burden of these commonly co-occurring mental health conditions.
Acknowledgments
Funding Support:
This work was generously supported by grants/awards from the National Institute on Alcohol Abuse and Alcoholism (AA016346) to Dr. Crum, the National Institute of Drug Abuse (DA030460) to Dr. Mojtabai, the Manitoba Health Research Chair to Dr. Sareen, and the Manitoba Health Research Council Establishment Award and Canadian Institutes of Health Research New Investigator Award (#113589) to Dr. Bolton.
REFERENCES
- 1.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ormel J, Petukhova M, Chatterji S, Guilar-Gaxiola S, Alonso J, Angermeyer MC, Bromet EJ, Burger H, Demyttenaere K, de GG, Haro JM, Hwang I, Karam E, Kawakami N, Lepine JP, Medina-Mora ME, Posada-Villa J, Sampson N, Scott K, Ustun TB, Von KM, Williams DR, Zhang M, Kessler RC. Disability and treatment of specific mental and physical disorders across the world. Br J Psychiatry. 2008;192:368–375. doi: 10.1192/bjp.bp.107.039107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saarni SI, Suvisaari J, Sintonen H, Pirkola S, Koskinen S, Aromaa A, Lonnqvist J. Impact of psychiatric disorders on health-related quality of life: general population survey. Br J Psychiatry. 2007;190:326–332. doi: 10.1192/bjp.bp.106.025106. [DOI] [PubMed] [Google Scholar]
- 4.Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(2):247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- 5.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Wang P, Wells KB, Zaslavsky AM. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sbrana A, Bizzarri JV, Rucci P, Gonnelli C, Doria MR, Spagnolli S, Ravani L, Raimondi F, Dell'osso L, Cassano GB. The spectrum of substance use in mood and anxiety disorders. Compr Psychiatry. 2005;46(1):6–13. doi: 10.1016/j.comppsych.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Roy-Byrne PP, Stang P, Wittchen HU, Usten BT, Walters EE, Kessler RC. Life-time panic-depression comorbidity in the National Comorbidity Survey: association with symptoms, impairment, course and help seeking. Br J Psychiatry. 2000;176:229–235. doi: 10.1192/bjp.176.3.229. [DOI] [PubMed] [Google Scholar]
- 9.Bijl RV, Ravelli A. Psychiatric morbidity, service use, and need for care in the general population: results of the Netherlands Mental Health Survey and Incidence Survey. Am J Public Health. 2000;90:602–607. doi: 10.2105/ajph.90.4.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Arch Gen Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 12.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158(6):848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 13.Quitkin FM, Rifkin A, Kaplan J, Klein DF. Phobic anxiety syndrome complicated by drug dependence and addiction. A treatable form of drug abuse. Arch Gen Psychiatry. 1972;27(2):159–162. doi: 10.1001/archpsyc.1972.01750260013002. [DOI] [PubMed] [Google Scholar]
- 14.Bibb JL, Chambless DL. Alcohol use and abuse among diagnosed agoraphobics. Behav Res Ther. 1986;24:49–58. doi: 10.1016/0005-7967(86)90149-x. [DOI] [PubMed] [Google Scholar]
- 15.de Graaf R, Bijl RV, Smit F, Vollebergh WA, Spijker J. Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: findings from the Netherlands Mental Health Survey and Incidence Study. Am J Psychiatry. 2002;159:620–629. doi: 10.1176/appi.ajp.159.4.620. [DOI] [PubMed] [Google Scholar]
- 16.Sareen J, McWilliams L, Cox B, Stein MB. Does a U-shaped relationship exist between alcohol use and DSM-III-R mood and anxiety disorders? J Affect Disord. 2004;82:113–118. doi: 10.1016/j.jad.2002.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Swendsen JD, Merikangas KR, Canino GJ, Kessler RC, Rubio-Stipec M, Angst J. The comorbidity of alcoholism with anxiety and depressive disorders in four geographic communities. Compr Psychiatry. 1998;39:176–184. doi: 10.1016/s0010-440x(98)90058-x. [DOI] [PubMed] [Google Scholar]
- 18.Thomas SE, Randall CL, Carrigan MH. Drinking to cope in socially anxious individuals: a controlled study. Alcohol Clin Exp Res. 2003;27(12):1937–1943. doi: 10.1097/01.ALC.0000100942.30743.8C. [DOI] [PubMed] [Google Scholar]
- 19.Markhou A, Kosten TR, Koob GF. Neurobilogical similarities in depression and drug dependence: A self-medication hypothesis. Neuropsychopharmacology. 1998;18:135–174. doi: 10.1016/S0893-133X(97)00113-9. [DOI] [PubMed] [Google Scholar]
- 20.Swan AC. The strong relationship between bipolar and substance-use disorder: Mechanisms and treatment implications. Ann N Y Acad Sci. 2010;1187:276–293. doi: 10.1111/j.1749-6632.2009.05146.x. [DOI] [PubMed] [Google Scholar]
- 21.Bolton J, Robinson J, Sareen J. Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. J Affect Disord. 2009;115(3):367–375. doi: 10.1016/j.jad.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Robinson J, Sareen J, Cox B, Bolton J. Correlates of self-medication for anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Nerv Ment Dis. 2009;197:873–878. doi: 10.1097/NMD.0b013e3181c299c2. [DOI] [PubMed] [Google Scholar]
- 23.Robinson J, Sareen J, Cox BJ, Bolton J. Self-medication of anxiety disorders with alcohol and drugs: results from a nationally representative sample. J Anxiety Disord. 2009;23:38–45. doi: 10.1016/j.janxdis.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 24.Falk D, Yi H, Hilton M. Age of onset and temporal sequencing of lifetime DSM-IV alcohol use disorders relative to comorbid mood and anxiety disorders. Drug Alcohol Depend. 2008;94:234–245. doi: 10.1016/j.drugalcdep.2007.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grant B, Moore T, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 26.Grant B, Dawson D, Hasin D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. text rev. Washington, DC: Author; 2000. [Google Scholar]
- 28.Ruan W, Goldstein R, Chou S, Smith S, Saha T, Pickering R, Dawson, Huang B, Stinson F, Grant B. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Research Triangle Institute. Software for Survey Data Analysis (SUDAAN), Version 8.0. Research Triangle Park, NC: Research Triangle Institute; 2002. [Google Scholar]
- 30.Gruber AJ, Pope HG, Brown ME. Do patients use marijuana as an antidepressant? Depression. 1996;4(2):77–80. doi: 10.1002/(SICI)1522-7162(1996)4:2<77::AID-DEPR7>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 31.Degenhardt G, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98:1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- 32.Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]