Abstract
Context
Despite prior evidence supporting cross-sectional associations of depression and alcohol use disorders, there is relatively little prospective data on the temporal relationship of depressed mood and maladaptive drinking, particularly across extended intervals.
Objective
Hypothesizing that depressed mood in childhood is associated with an increased risk for alcohol involvement among drinkers during adolescence and young adulthood, we used prospectively gathered data to assess these relationships by mood level, and by sex and race-ethnicity subgroup.
Design
Cohort study of children followed during late childhood, early adolescence and young adulthood.
Setting and Participants
Two successive cohorts of students from 19 elementary schools in an urban mid-Atlantic region of the United States have been followed since entry into first grade (1985: cohort I, n=1196; 1986: cohort II, n=1115). The students were roughly equally divided by sex (48% female), and predominantly African-American (70%). Between 1989 and 1994, annual assessments were collected on students remaining in the public school system, and between 2000 and 2001, approximately 75% participated in a young adult interview (n=1692).
Measures
Among participants who reported having used alcohol, Cox and multinomial regression analyses were used to assess the association of childhood mood level, as measured by a depression symptom screener, with each alcohol outcome (incident alcohol intoxication, incident alcohol-related problems; DSM-IV alcohol abuse and alcohol dependence).
Results
In adjusted regression analyses among drinkers, a high level of childhood depressed mood was associated with an earlier onset and increased risk for alcohol intoxication, and alcohol-related problems during late childhood and early adolescence, and for the development of DSM-IV alcohol dependence in young adulthood.
Conclusions
Early manifestations associated with possible depressive conditions in childhood helped predict and account for subsequent alcohol involvement, extending across life stages from childhood through young adulthood.
Keywords: alcohol, abuse, depression, mood, risk
Introduction
Depression and alcohol use disorders have been found to co-occur in cross sectional studies of adults and adolescents. This confluence has been well recognized in clinical samples.e.g., 1-4 Although there are exceptions5, patients with comorbid diagnoses tend to have a worse prognosis than those with either diagnosis alone as evidenced by heavier drinking,6-13 and greater depressive symptom severity.14-16 However, some prior investigators have not found these co-morbid associations. For example, Harrington et al.17 completed a case-control study of child and adolescent psychiatric patients and found no association with non-depressive psychiatric disorders in adulthood.
Data from population-based surveys also have documented the co-occurrence between depression and alcohol use disorders.18-20 Despite evidence from cross-sectional data, there is relatively little information available from prospective studies that might aid in improving our understanding of the temporal relationship between these conditions. Findings differ depending on the measurement and methodology used, as well as the timing of the longitudinal assessments.21-25 For example, in a meta-analysis, Hartka et al.23 suggested that over the short term, depression was followed by decreased alcohol use. Yet, over the long term, among women but not men, depression was a positive predictor of alcohol consumption. In addition to inconsistencies in clinical and population-based studies, there also is a paucity of prospective data that extends across life stages.e.g., 26-28 Fergusson and Woodward28 using a birth cohort of New Zealand youth assessed outcomes during young adulthood related to adolescent depression, and found that the association with alcohol use disorders was explained by social, personal and familial characteristics. Rao and colleagues29 followed a sample of female adolescents into early adulthood, and reported that substance use disorders predicted depression, but not the reverse.
Psychological theories used to help explain these associations include the general concept of using alcohol for self-medicating depressive symptoms or general tension reduction30, and by the stress-response dampening model.31 Social learning theorye.g., 32 might explain roles played by alcohol expectancies, coping skills, and self-efficacy in regulation of drinking33-35 especially in the presence of stress or mood symptoms.36-38 Life course developmental models39,40 suggest that both social adaptational status (the interaction between social task demands and how our responses are judged) and psychological well-being form a foundation for mental health and predict subsequent behavioral patterns such as alcohol consumption.39,41 Furthermore, there may be common underlying genetic as well as social or environmental factors which are associated with increased risk for both disorders.42-46 Family history of alcoholism as well as depression may be influential.47,48 Furthermore, other conditions may explain familial associations. In a male twin sample, evidence indicated that antisocial personality disorder may account for the genetic association found between depression and alcohol dependence.49 Chassin et al.,50 found that externalizing but not internalizing symptoms mediated the effects of parental history with alcohol disorders.
In the current report, we used data gathered from two cohorts originally assessed in first grade, and subsequently followed through adolescence and young adulthood. Prior analyses of these cohorts have shown that depressed mood in childhood is associated with alcohol initiation without parental permission.51 Our objective here was to extend these findings among drinkers, to improve our understanding of the temporal relationship of depressed mood with subsequent risk associated with several alcohol outcomes. Using a depression symptom screener, we examined varying levels of non-diagnostic depressed mood to assess whether alcohol involvement might covary with these levels. Specifically, we hypothesized that any level of depressed mood in childhood would be associated with an increased risk for alcohol intoxication and the development of alcohol-related problems during adolescence, and that this association would extend into young adulthood, to possibly account for the occurrence of alcohol abuse or dependence. Because prior evidence indicates these relationships may differ for some subgroups,21,23,52-55 we completed separate analyses by sex and race-ethnicity.
Methods
Study population
The data for these analyses were derived from a prospective study, which began in 1985-86, conducted within the context of a randomized trial of two primary school interventions directed toward academic achievement and classroom behavior. A total of 2,311 students were sampled during two successive school years from those entering the first grade classrooms of 19 elementary schools in an urban mid-Atlantic region of the United States (1985: cohort I, n=1196; 1986: cohort II, n=1115). Parental consent was obtained from 95% of the original cohort. Further details on the study design and data collection are available elsewhere.39,56-58 Specific information relevant to the current report is described below.
Annually between 1989 and 1994, trained interviewers administered face-to-face interviews in private locations at each school. Interviewers were young adults of both sexes, from predominantly minority racial-ethnic backgrounds, similar to the ethnic composition of the study sample. The interview conducted in 1990 is considered the baseline interview for this current report because it was the first year that depressive mood was assessed by face-to-face interview. Of this baseline sample, 92.8% were re-interviewed in 1991 (90.7% cohort I, 94.9% cohort II), 84.7% in 1992 (83.1% cohort I, 86.3% cohort II), 75.7% in 1993 (74.6% cohort I, 76.7% cohort II). In 1994, limited resources were focused on following up youths in cohort II so that they would be followed to a similar mean age as the first cohort (69.0% cohort II, 30.7% cohort I). A total of 77.0% of the baseline sample had at least 3 years of follow-up between 1991 and 1994. Child assent was obtained at the time of each interview. A Certificate of Confidentiality was secured, and the study was approved by the Johns Hopkins Bloomberg School of Public Health Committee on Human Research.
Funding for follow-up was not available during the high school years of these two cohorts. Nonetheless, it was possible to re-engage the follow-up and tracing process such that between 2000 and 2001, approximately 75% of the pupils surviving from the original sample of 2,311 could be traced and face-to-face assessments were completed by trained interviewers in young adulthood (YA; n=1692), including 154 incarcerated individuals. An additional 12% were successfully located, but either chose not to be interviewed (n=142), or were not available (e.g., living out of state with no telephone number, military postings overseas; n=133). The mean age for the YA follow-up was 21 years.
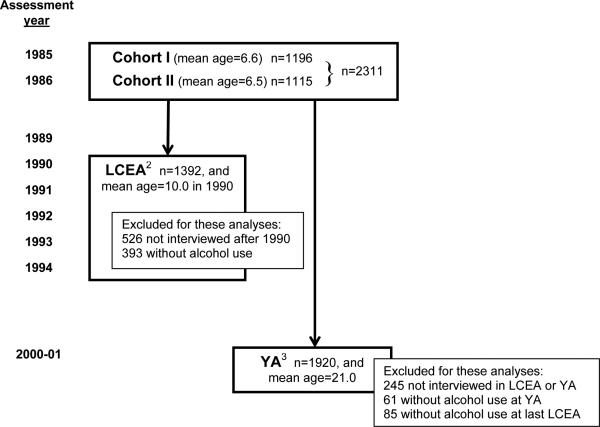
We assessed individuals at two separate life stages, defined here by length of follow-up (see Figure 1 for flow chart of assessments): 1) during late childhood/early adolescence (LCEA follow-up, age range 10-16 years; n=1392) and 2) during young adulthood (age range, 19-24 years; n=1920). The analysis for the LCEA follow-up involved exclusion of 919 youths from the original list of 2,311 students enrolled in first grade (526 youths who did not have at least one interview subsequent to 1990, as well as 393 youths who hadn't initiated alcohol use and therefore were not at risk for transitioning to the alcohol outcomes). The analyses for the YA follow-up included all the individuals who reported alcohol use (1392 individuals who reported alcohol use during LCEA and an additional 528 individuals reporting ever using alcohol when interviewed during YA). Excluded from the YA analysis were the 61 individuals who never used alcohol as reported on the YA interview, 245 individuals who were not followed-up either during adolescence or young adulthood, and 85 individuals who were excluded because they had not begun drinking at their last LCEA contact. Participants with missing follow-up information were more likely to be non-black, and to have paid for lunch as opposed to receiving reduced or free lunch during first grade. In the YA assessment, males were also more likely to be missing (32% vs. 23%).
Figure 1.
Flow chart of cohorts and sample used for the data analyses1. Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
1 The interview completed in 1990 is the baseline interview for this report, because this was first time that an interview assessment of depressed mood was ascertained.
2 LCEA, Late Childhood and Early Adolescent Follow-up. Of the baseline sample in 1990, 92.8% were re-interviewed in 1991 (90.7% cohort I, 94.9% cohort II), 84.7% in 1992 (83.1% cohort I, 86.3% cohort II), 75.7% in 1993 (74.6% cohort I, 76.7% cohort II). In 1994, limited resources were focused on following up youths in cohort II so that they would be followed to a similar mean age as the first cohort (69.0% cohort II, 30.7% cohort I). A total of 77.0% of the baseline sample had at least 3 years of follow-up between 1991 and 1994. The sample for the LCEA analysis was comprised of the 1392 individuals who reported having used alcohol by 1990 and had at least one LCEA interview after 1990.
3 YA, Young Adult Follow-up. Approximately 75% of the pupils surviving from the original sample of 2,311 could be traced and interviewed in young adulthood (YA; n=1692), including 154 incarcerated individuals. The analyses for the YA follow-up included all the individuals who reported alcohol use (1392 individuals who reported alcohol use during LCEA and an additional 528 individuals reporting ever using alcohol when interviewed during YA). Excluded from the YA assessment were the 61 individuals who never used alcohol, 245 individuals never followed-up, and 85 individuals who at last contact as adolescents had not begun drinking.
Measures
Four facets of depressed mood were assessed, based upon four questions that asked about having “been in a bad mood”, “felt sad”, “felt crabby or cranky” and “felt like crying” “all the time or almost all of the time”. Four item probes queried whether each feeling had ever occurred “every day or almost every day” for two weeks, or for the prior two weeks if the mood problem was described as current.59,60 We refer to a “high” level of depressed mood only if: (1) three of the four feelings had been experienced “all the time or almost all the time”, or (2) two of the four feelings were described as being current (within the prior two weeks), as well as having occurred for at least two weeks in the past. “Low” depressed mood refers to youths who (1) had expressed no more than one feeling at any time, or (2) had experienced two of the four feelings (current or in the past but not both). These “high” and “low” level depressed mood classifications were both referenced to youths with no experience with the four facets of mood as of the 1990 assessment. Our rationale for the mood categories was to distinguish those with multiple features or evidence for chronicity in the “high” level group, with those in the “low” level group with only one feeling and little evidence for persistence of depressed mood. We hypothesized that those with greater burden of depressed mood as evidenced by the larger number of features and recurrence or persistence of these feelings would be associated with the highest risk for alcohol involvement. This measure of depressed mood has adequate internal consistency (Cronbach α=0.7), and predictive validity with respect to an adapted version of the Composite International Diagnostic Interview61 (CIDI) - University of Michigan (UM) version module of major depression (relative to those without depressed mood by the time of the 1990 interview, high depressed mood level is associated with CIDI-UM major depression assessed during the 1993-94 interview (odds ratio, OR=3.17; 95% confidence interval, CI=1.68, 5.95; p=<0.001)). However, the measure is a screener questionnaire, and is not intended to be used to diagnose depression. Furthermore, the features measured may be indicative of a range of psychopathology.
Information on alcohol use was based on responses to the question asked each year (1989-1994) regarding whether the student had “ever drunk beer, wine, wine coolers, or any other drink with alcohol in it, even just a sip or taste”. Alcohol intoxication was assessed yearly by the question, “How old were you the first time you got drunk or high on alcohol?”. Individuals with intoxication prior or during the 1990 interview were excluded in order to assess new onset intoxication. Data on the occurrence and age of onset of alcohol-related problems also was assessed through 1994. The alcohol-related problem construct was represented by two groups of indicators:25 1) having social difficulties because of drinking such as trouble in school, home or with the police; or 2) having health or physical problems related to using alcohol such as a sick stomach, feeling panicky, or feeling a hunger to use alcohol. Individuals with alcohol-related problems before or at baseline were removed in order to focus this inquiry upon incident problem drinking.
The interview assessment for the DSM-IV62 classifications of lifetime alcohol abuse and dependence in the YA follow-up was an amended version of the approach used in the United States National Comorbidity Survey Replication and in the World Mental Health Surveys Initiative. The amendment involved the addition of this global alcohol problems screening question: “Was there ever a time in your life when people told you they thought you drank too much or when you thought you might have a drinking problem?“, which was added in an effort to increase sensitivity for clinically significant alcohol dependence. Reed et al.58 provide more detail on this approach (see also the Appendix). Because of the relatively short developmental interval for these new dependence cases (over late adolescence to young adulthood), we included the entire group of individuals who met 3 or more dependence criteria in our definition (70.5% also self-reported 12-month symptom clustering). When we excluded those without self-reported clustering, substantive conclusions were unchanged.
Covariates included in the analyses were: sex and race-ethnicity (where applicable in stratified analyses: African-American vs. all others (>90% non-Hispanic White)), caregiver history of heavy drinking and/or illegal drug use (yes=1, no=0), the youth report of peer alcohol use (yes=1, no=0), age at baseline (continuous variable), level of conduct problems, and neighborhood disadvantage. Caregiver history of heavy drinking and illegal drug use was self-reported by the adult participants. Peer drinking was assessed with one question asking whether participants had any friends who drank alcohol. The presence of conduct problems was assessed using the 11-item Baltimore Conduct Problems and Delinquency Scale (BCPDS), which assesses delinquent and antisocial behavior. This measure was previously described63, and is an adaptation of a self-report measure developed by Elliott and Huizinga for the National Survey of Delinquency and Drug Use.64 For use in our work, the number of items was increased so as to provide full coverage of the DSM criteria for conduct disorder. Responses from the four-point Likert scale (not at all, to 3 or more times in the prior year) were summed, and high and low categories were characterized (above and below the median scale score for this sample). Psychometric analyses suggest good to excellent internal consistency (Cronbach alphas range from 0.74 to 0.86 during middle school). A one-year test-retest for a subsample of middle school youths yielded an intraclass correlation coefficient of 0.63. With respect to concurrent validity, 6th grade youths in the top quartile of the BCPDS were nearly three times more likely than youths below the 75th percentile to be suspended or expelled from school and to be referred for mental health services for antisocial behavior. In terms of predictive validity, for every unit of increase on the BCPDS in grade 6, there was a three-fold increased odds of antisocial personality disorder at age 19-20 (OR=3.31, CI=2.42-4.51). Level of neighborhood disadvantage was assessed using an 18-item scale adapted from one initially developed for use in the National Youth Survey.65 The scale is a self-report measure of neighborhood characteristics, including items that address concepts such as church and religious involvement, whether neighbors take care of each other, and whether neighbors damage or steal property.65,66 Score tertiles were used in the analyses to be consistent with prior use of this scale.66 The data for these potential confounding covariates were gathered at the time of the 1990 interview, except for the BCPDS, which was first assessed in the 1991, and caregiver alcohol and drug use history, which was reported in adulthood. The rationale for including these covariates was based on prior studies, which have shown that these characteristics may influence the occurrence of alcohol involvement.60,66-72
Data analysis
After exploratory data analyses, we completed initial and multiple regression models to assess the strength of the associations between depressed mood levels and the risk for each of the subsequent alcohol-related outcomes. Cox proportional hazard ratios were calculated for time to first alcohol-related problem, and to first episode of alcohol intoxication during the LCEA follow-up. Multinomial regression was used to examine the association of childhood depressed mood with the occurrence of DSM-IV alcohol use disorders during the YA follow-up. The rationale for using multinomial regression in lieu of survival analysis with the YA outcomes was because of a violation of the proportionality assumption of the Cox model for these outcomes, with too few cases to stratify by age groups. A single multinomial regression model was used, with the outcome having four levels: alcohol abuse, alcohol dependence, no alcohol disorder, and drinkers without either disorder (reference category). For all regression models, stratified analyses were completed by sex and race-ethnicity.
Potential confounding was constrained in these analyses via statistical adjustment. To take into account various occurrences of missing information, and to keep the representativeness of the original sample intact, we created dummy-coded covariate categories to denote subgroups with missing covariate data. This approach stabilizes the number of participants contributing information to the regression analyses. An alternative approach to handling missing values (multiple imputation)73 did not alter the results. We also included in the multiple regression analyses a covariate for receipt of subsidized lunch during first grade because this characteristic was associated with attrition. To hold constant the participants’ first grade intervention status, this covariate also was included in the adjusted analyses. Lastly, a variant of the Huber-White sandwich estimator of variance was used to obtain robust standard errors and variance estimates in all regression analyses to accommodate the initial sample design and clustering of students within schools.74
Results
Among the 2311 first graders, a total of 1785 completed at least one follow-up interview after 1990. Because those followed up in LCEA and YA come from the same original study population, the distributions are similar (Table 1). Half of the participants are female, and most are African-American. At the time of the baseline interview for these analyses, close to half of the students were age 10 (mean=10.0 years (standard deviation, SD=0.8)). Forty percent had a caregiver history of either heavy drinking or drug use. Most had received free or subsidized lunches in first grade.
Table 1.
Frequency distribution of baseline characteristics as observed at the time of follow-up during late childhood and early adolescence (LCEA; n=1392) and young adulthood (YA; n=1920). Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
| Characteristics at baseline (1990)1 | Late Childhood and Early Adolescent Follow-up n (%) | Young Adult Follow-up n (%) | ||
|---|---|---|---|---|
| Age (years): | ||||
| 9 | 404 | (29.0) | 603 | (31.4) |
| 10 | 641 | (46.0) | 889 | (46.3) |
| 11 | 312 | (22.4) | 388 | (20.2) |
| 12 | 33 | (2.4) | 37 | (1.9) |
| 13 | 2 | (0.1) | 3 | (0.2) |
| Sex: Female | 671 | (48.2) | 968 | (50.4) |
| Male | 721 | (51.8) | 952 | (49.6) |
| Race-ethnicity2: | ||||
| African-American | 1010 | (72.6) | 1317 | (68.6) |
| Other | 382 | (27.4) | 603 | (31.4) |
| Peer alcohol use: | ||||
| Yes | 201 | (14.4) | 222 | (11.6) |
| No | 802 | (57.6) | 937 | (48.8) |
| missing3 | 389 | (28.0) | 761 | (39.6) |
| Caregiver history of heavy drinking and/or illegal drug use: | ||||
| Yes | 563 | (40.5) | 767 | (39.9) |
| No | 524 | (37.6) | 760 | (39.6) |
| missing3 | 305 | (21.9) | 393 | (20.5) |
| Neighborhood disadvantage (tertiles): | ||||
| Low | 353 | (25.4) | 407 | (21.2) |
| Middle | 334 | (24.0) | 383 | (19.9) |
| High | 304 | (21.8) | 353 | (18.4) |
| missing3 | 401 | (28.8) | 777 | (40.5) |
| Subsidized lunch4: | ||||
| Yes | 805 | (57.8) | 1046 | (54.5) |
| No | 586 | (42.1) | 870 | (45.3) |
| missing5 | 1 | (0.1) | 4 | (0.2) |
| Conduct problems6: | ||||
| Low | 581 | (41.7) | 726 | (37.8) |
| High | 686 | (49.3) | 753 | (39.2) |
| missing3 | 125 | (9.0) | 441 | (23.0) |
Information on all the characteristics listed was gathered at the baseline interview for these analyses (1990), except for subsidized lunch which was gathered from school records in first grade (1985-86), conduct problems which were assessed in1991, and household history of heavy drinking and/or illegal drug use assessed in young adulthood.
A total of 94.5% (n=361) and 96.0% (n=579) of the Other race-ethnicity group is White in the assessments during the LCEA and YA follow-ups, respectively.
These individuals did not provide this information during the LCEA or YA follow-up.
This variable indicates receipt of free or subsidized lunch in first grade.
This information was not available from school records for these individuals.
The categories represent above and below the median of the scale score for this sample.
In Table 2, we present the frequency distribution of depressed mood level at baseline, stratified by sex and race-ethnicity. With respect to the LCEA follow-up, 20% had been in the low depressed mood category at baseline in 1990, and 12% were at the high level. With respect to the YA follow-up, 16% and 10% had been in the low and high baseline categories of depressed mood, respectively. Contrary to our prior hypotheses, there was no appreciable association of sex or race-ethnicity with the baseline assessment of depressed mood.
Table 2.
Frequency distribution of childhood depressed mood level for the youths reporting alcohol use assessed at the time of the follow-up during late childhood and early adolescence (LCEA; n=1392) and young adulthood (YA; n=1920). Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
| Childhood depressed mood level |
Late Childhood and Early Adolescent Follow-up n (%) |
Young Adult Follow-up n (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (n=1392) |
Male (n=721) |
Female (n=671) |
African- American (n=1010) |
Other race- ethnicity1,2 (n=382) |
Total (n=1920) |
Male (n=952) |
Female (n=968) |
African- American (n=1317) |
Other race- Ethnicity1,3 (n=603) |
|
| None | 557 (40.0) | 287 (39.8) | 270 (40.2) | 397 (39.3) | 160 (41.9) | 649 (33.8) | 322 (33.8) | 327 (33.8) | 474 (36.0) | 175 (29.0) |
| Low | 274 (19.7) | 138 (19.1) | 136 (20.3) | 215 (21.3) | 59 (15.4) | 309 (16.1) | 160 (16.8) | 149 (15.4) | 243 (18.5) | 66 (11.0) |
| High | 170 (12.2) | 78 (10.8) | 92 (13.7) | 133 (13.2) | 37 (9.7) | 199 (10.4) | 87 (9.1) | 112 (11.6) | 155 (11.8) | 44 (7.3) |
| missing | 391 (28.1) | 218 (30.2) | 173 (25.8) | 265 (26.2) | 265 (33.0) | 763 (39.7) | 383 (40.2) | 380 (39.3) | 445 (33.8) | 318 (52.7) |
A total of 94.5% (n=361) and 96.0% (n=579) of the Other race-ethnicity group is White during the LCEA and YA follow-up, respectively.
For African-Americans compared with the Other race-ethnicity group during the LCEA follow-up, χ2=12.51(df=3), p<0.001.
For African-Americans compared with the Other race-ethnicity group during the YA follow-up, χ2=65.77 (df=3), p<0.001.
As shown in Table 3, by the time of the LCEA follow-up, 16% of the youths had experienced at least one episode of alcohol intoxication; 22% had experienced alcohol-related problems for the first time. These frequency differences may occur because some underage drinking problems do not require drinking to intoxication. Similar drinking outcome proportions were found for each of the sex and race-ethnicity subgroups. By young adulthood, 12% had developed alcohol abuse, with a greater cumulative incidence proportion of abuse occurring among the male (16%) and non-black (18%) subgroups. A total of 9.5% had developed alcohol dependence, with larger cumulative incidence proportion for males (14%) and for non-blacks (13%). For reasons discussed by Degenhardt et al.,75 this estimate for DSM-IV alcohol dependence should be regarded as possibly conservative, in that the ‘clinical significance’ criterion were in place. Drinkers without evidence of maladaptive or hazardous alcohol problems were not counted in the numerators for these estimates.
Table 3.
Frequency distribution of incident cases of alcohol involvement outcomes among those reporting alcohol use during late childhood and early adolescent (LCEA; n=1392) and young adulthood (YA; n=1920). Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
| Incident cases of alcohol involvement observed during the Late Childhood and Early Adolescence Follow-up n (%) | |||||
|---|---|---|---|---|---|
| Total (n=1392) | Male (n=721) | Female (n=671) | African-American (n=1010) | Other race-ethnicity (n=382) | |
| Alcohol intoxication1 | |||||
| Yes | 218 (15.7) | 105 (14.6) | 113 (16.8) | 166 (16.4) | 52 (13.6) |
| No | 1039 (74.6) | 535 (74.2) | 504 (75.1) | 784 (77.6) | 255 (66.8) |
| missing | 135 (9.7) | 81 (11.2) | 54 (8.1) | 60 (5.9) | 75 (19.6) |
| Alcohol-related problem | |||||
| Yes | 309 (22.2) | 163 (22.6) | 146 (21.8) | 229 (22.7) | 80 (20.9) |
| No | 1076 (77.3) | 555 (77.0) | 521 (77.6) | 778 (77.0) | 298 (78.0) |
| missing | 7 (0.5) | 3 (0.4) | 4 (0.6) | 3 (0.3) | 4 (1.1) |
| Incident cases of alcohol use disorders observed at the Young Adult Follow-up n (%) | |||||
|---|---|---|---|---|---|
| Total (n=1920) | Male (n=952) | Female (n=968) | African-American (n=1317) | Other race-ethnicity (n=603) | |
| Alcohol abuse2 | |||||
| Yes | 237 (12.3) | 154 (16.2) | 83 (8.6) | 126 (9.6) | 111 (18.4) |
| No | 1384 (72.1) | 609 (64.0) | 775 (80.1) | 1018 (77.3) | 366 (60.7) |
| missing | 299 (15.6) | 189 (19.8) | 110 (11.4) | 173 (13.1) | 126 (20.9) |
| Alcohol dependence3 | |||||
| Yes | 183 (9.5) | 132 (13.9) | 51 (5.3) | 103 (7.8) | 80 (13.3) |
| No | 529 (27.6) | 304 (31.9) | 225 (23.2) | 295 (22.4) | 234 (38.8) |
| Other drinkers | 909 (47.3) | 327 (34.3) | 582 (60.1) | 746 (56.6) | 163 (27.0) |
| missing | 299 (15.6) | 189 (19.9) | 110 (11.4) | 173 (13.1) | 126 (20.9) |
For African-Americans and Other race-ethnicity, χ2=59.38 (df=2), p<0.001.
For males and females, χ2=61.92 (df=2), p<0.001; for African-Americans and Other race-ethnicity, χ2=57.99 (df=2), p<0.001.
See text and appendix for details about this assessment of “clinically significant” alcohol dependence syndromes. For males and females, χ2=138.84 (df=3), p<0.001; for African-Americans and Other race-ethnicity, χ2=146.56 (df=3), p<0.001.
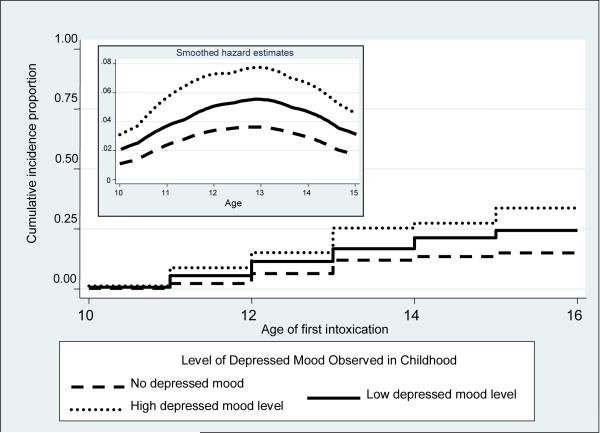
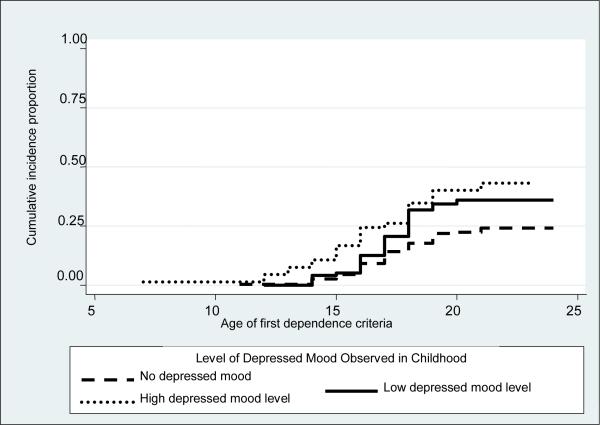
Kaplan-Meier survival curves were estimated for each of the alcohol-related outcomes by depressed mood. Age of first intoxication was earliest for those with high depressed mood at baseline (log-rank test, χ2=18.21 degrees of freedom (df)=2, p< 0.001; Figure 2). The smoothed hazard estimates indicate proportionality, which helped motivate use of the Cox model. Similar findings were found for Kaplan-Meier curves assessing age at first alcohol problem (log-rank test, χ2=10.91 (df=2), p=0.004; figure not shown). With respect to the YA follow-up outcomes, no appreciable association was found for age of first clinical feature of alcohol abuse in relation to baseline depressed mood level (log-rank test, χ2=2.55 (df=2), p=0.28). However, with respect to the first alcohol dependence criteria, individuals with high baseline depressed mood started the process earlier (log-rank test, χ2=10.24 (df=2), p=0.006; Figure 3).
Figure 2.
Kaplan-Meier survival estimates for the age of first alcohol intoxication by level of childhood depressed mood among youth reporting alcohol use1. The insert graph provides the smoothed hazard estimates by depressed mood level. Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
1 Log-rank test, χ2=18.21 (df=2), p<0.001.
Figure 3.
Kaplan-Meier survival estimates for the age of first experience with DSM-IV criteria for alcohol dependence by level of childhood depressed mood among drinkers observed at the young adult follow-up1,2 Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
1 Log-rank test, χ2=10.24 (df=2), p=0.006.
2 See text and appendix for clarification of ‘clinically significant’ alcohol dependence syndrome under observation in this study.
In Table 4, we present the unadjusted and adjusted hazard ratios based on a comparison of subgroups with respect to the onset of alcohol intoxication and alcohol-related problems during the LCEA follow-up. Table 5 presents odds ratios for the occurrence of alcohol abuse and dependence as observed during the YA follow-up interval. Based on covariate-adjusted Cox models, the estimated hazards for alcohol intoxication during the LCEA follow-up among individuals with high childhood depressed mood were roughly two-fold larger than values observed for youths without depressed mood. High depressed mood level at childhood baseline also was associated with the onset of alcohol-related problems among males, and non-blacks. An estimated two-fold increased risk of alcohol dependence was associated with those who had high childhood depressed mood relative to those without these mood indicators (Table 5); for non-blacks, this association was attenuated with wider confidence limits. Childhood depressed mood was not associated with risk of developing alcohol abuse by the time of the YA follow-up. Because our analyses were restricted to drinkers, which theoretically could introduce bias, we also repeated these regression analyses including the non-drinkers as part of the reference group in the Cox models, and as a separate outcome in the multinomial regression analyses. These supplemental analyses led to no differences in substantive conclusions.
Table 4.
Unadjusted and adjusted1 hazard ratios (95% confidence interval) for risk of alcohol intoxication and alcohol-related problems during late childhood and early adolescence (LCEA) by level of childhood depressed mood among youth reporting alcohol use based on Cox regression analyses. Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
| Childhood depressed mood level | Estimated Relative Risk of Alcohol Intoxication during the LCEA Follow-up Interval |
||||
|---|---|---|---|---|---|
| Total | Males | Females | African-American | Other race-ethnicity | |
|
Unadjusted | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 1.65 (1.15-2.37) p=0.007 | 1.79 (1.05-3.06) p=0.03 | 1.53 (0.93-2.54) p=0.10 | 1.42 (0.94-2.15) p=0.10 | 2.95 (1.37-6.34) p=0.006 |
| High | 2.28 (1.55-3.37) p<0.001 | 2.33 (1.29-4.23) p=0.005 | 2.16 (1.28-3.66) p=0.004 | 2.13 (1.39-3.28) p=0.001 | 3.03 (1.21-7.54) p=0.02 |
|
Adjusted 1 | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 1.59 (1.10-2.29) p=0.01 | 1.73 (1.00-2.99) p=0.05 | 1.51 (0.91-2.52) p=0.12 | 1.33 (0.87-2.03) p=0.18 | 2.90 (1.33-6.29) p=0.007 |
| High | 1.99 (1.33-2.97) p=0.001 | 2.06 (1.10-3.87) p=0.024 | 1.99 (1.16-3.42) p=0.013 | 1.77 (1.14-2.76) p=0.01 | 2.78 (1.04-7.40) p=0.04 |
|
Estimated Relative Risk of Alcohol Problems during the LCEA Follow-up Interval | |||||
|
Unadjusted
| |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 1.44 (1.06-1.95) p=0.02 | 1.63 (1.06-2.50) p=0.03 | 1.25 (0.80-1.95) p=0.32 | 1.47 (1.04-2.08) p=0.03 | 1.31 (0.66-2.60) p=0.43 |
| High | 1.68 (1.20-2.35) p=0.003 | 2.23 (1.39-3.58) p=0.001 | 1.29 (0.78-2.11) p=0.32 | 1.50 (1.02-2.22) p=0.04 | 2.33 (1.18-4.58) p=0.01 |
|
Adjusted 1 | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 1.35 (0.99-1.84) p=0.06 | 1.48 (0.95-2.30) p=0.09 | 1.21 (0.77-1.92) p=0.40 | 1.29 (0.91-1.84) p=0.15 | 1.41 (0.71-2.80) p=0.32 |
| High | 1.47 (1.04-2.08) p=0.03 | 1.97 (1.21-3.23) p=0.007 | 1.15 (0.69-1.91) p=0.60 | 1.27 (0.85-1.91) p=0.24 | 2.19 (1.07-4.46) p=0.03 |
The multivariable analyses were adjusted for sex and race (when applicable), age, caregiver history of heavy drinking and/or illegal drug use, peer drinking, neighborhood disadvantage, conduct problems, intervention status, subsidized lunch, and clustering within schools. In order to avoid biases resulting from nonrandom deletion of participants within our prospective study cohorts, and to keep the representativeness of the original sample intact thereby stabilizing the number of participants contributing information to the regression analyses, we created separate categories for subgroups with missing information for each covariate included in each multivariable model.
Table 5.
Unadjusted and adjusted odds ratios (95% confidence interval) for estimated risk of alcohol abuse and alcohol dependence in young adulthood by level of childhood depressed mood among youth reporting alcohol use based on multinomial regression analyses1. Data are from an epidemiologic sample originally recruited at the time of entry into first grade classrooms in 1985-1986 from an urban mid-Atlantic public school system (n=2311).
| Childhood depressed mood level | Estimated Relative Risk of Alcohol Abuse Observed during the YA Follow-up Interval |
||||
|---|---|---|---|---|---|
| Total | Males | Females | African-American | Other race-ethnicity | |
|
Unadjusted | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 0.96 (0.61-1.52) p=0.86 | 0.89 (0.47-1.69) p=0.72 | 0.98 (0.47-2.04) p=0.95 | 0.90 (0.47-1.73) p=0.75 | 1.56 (0.93-2.62) p=0.09 |
| High | 0.53 (0.25-1.16) p=0.11 | 0.62 (0.24-1.60) p=0.32 | 0.63 (0.21-1.95) p=0.42 | 0.52 (0.18-1.53) p=0.24 | 0.62 (0.23-1.65) p=0.34 |
|
Adjusted | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 0.94 (0.57-1.53) p=0.79 | 0.86 (0.47-1.60) p=0.64 | 1.01 (0.53-1.93) p=0.98 | 0.78 (0.40-1.53) p=0.48 | 1.51 (0.88-2.57) p=0.13 |
| High | 0.58 (0.27-1.22) p=0.15 | 0.60 (0.29-1.25) p=0.17 | 0.58 (0.19-1.74) p=0.33 | 0.53 (0.20-1.45) p=0.22 | 0.70 (0.24-2.08) p=0.53 |
|
Estimated Relative Risk of Alcohol Dependence Observed during the YA Follow-up Interval3 | |||||
|
Unadjusted
| |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 1.56 (1.01-2.43) p=0.047 | 1.29 (0.73-2.27) p=0.38 | 2.26 (1.07-4.78) p=0.03 | 1.60 (0.95-2.69) p=0.08 | 2.23 (0.79-6.26) p=0.13 |
| High | 1.82 (1.20-2.76) p=0.005 | 2.00 (1.23-3.23) p=0.005 | 2.56 (1.32-4.96) p=0.005 | 2.21 (1.49-3.29) p<0.001 | 1.42 (0.58-3.47) p=0.45 |
|
Adjusted2 | |||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Low | 1.50 (0.89-2.52) p=0.13 | 1.29 (0.67-2.47) p=0.45 | 2.27 (1.04-4.95) p=0.04 | 1.35 (0.75-2.42) p=0.32 | 2.14 (0.71-6.48) p=0.18 |
| High | 2.07 (1.31-3.26) p=0.002 | 2.20 (1.37-3.52) p=0.001 | 2.55 (1.16-5.62) p=0.02 | 2.46 (1.68-3.61) p<0.001 | 1.38 (0.47-4.09) p=0.56 |
One multinomial regression model was used to assess alcohol abuse and alcohol dependence as separate outcomes, referenced to drinkers without either disorder.
The multivariable model was adjusted for sex and race (when applicable), age, caregiver history of heavy drinking and/or illegal drug use, peer drinking, neighborhood disadvantage, conduct problems, intervention status, subsidized lunch, and clustering within schools. In order to avoid biases resulting from nonrandom deletion of participants within our prospective study cohorts, and to keep the representativeness of the original sample intact thereby stabilizing the number of participants contributing information to the regression analyses, we created separate categories for missing information for all variables in the model.
See text and appendix for clarification of ‘clinically significant’ alcohol dependence syndrome under observation in this study.
Discussion
Consistent with our hypotheses in this prospective study, depressed mood as assessed in childhood helped to predict and may account for increased risk of several manifestations of alcohol involvement. For those relationships that were predictive, the strength of the associations increased with greater severity of depressed mood, but the risk estimates for the subgroup at a lower level of baseline depressed mood were not statistically different from those estimates for children without depressed mood. Higher depressed mood in childhood also signaled earlier onset of alcohol involvement, and in general, congruent risk ratios were observed for the sex and race-ethnicity subgroups under study. For the assessment of mood level with first report of alcohol-related problems, males and non-blacks had the strongest associations. The vulnerability to increased risk for alcohol involvement extended across both life stages under study and was independent of potential causal determinants of maladaptive drinking such as family income in childhood, heavy drinking among caregivers, peer alcohol use, level of conduct problems, and neighborhood disadvantage. Possible explanations for these findings include motives to use alcohol for stress reduction.31,76 Children with early mood symptoms may be more likely to subsequently use alcohol as a method for coping with negative affect.36,77 In addition, the association of childhood depressed mood with later alcohol involvement may be mediated or moderated by alcohol-related expectancies.33,78-82 Familial factors or processes, with both genetic and/or environmental substrates, may influence the development of affective symptoms as well as the occurrence of maladaptive drinking patterns.71,83-87 These processes may be specific for alcohol involvement relatively early in life. 88-90
Our findings are consistent with clinical and population-based cross-sectional data, and extend findings from prior prospective analyses.91-97 However, our findings differ from prior reports which indicate that adolescent depression predicts alcohol disorders only in the presence of conduct disorder symptoms (data for this interaction not shown).91 Our results may differ because we examined mood at an earlier life stage (childhood as opposed to adolescence). In our analyses, early mood level predicted all but one of the alcohol involvement outcomes. We found no association with alcohol abuse. Early depressed mood appears to predict the transition from high-risk drinking to alcohol dependence but not to the occurrence of alcohol abuse alone. Similar findings have been documented in some prior data. In analyses of the National Comorbidity Survey, using retrospective reports from cross-sectional data, mood disorders were positively associated with alcohol dependence, but negatively associated with alcohol abuse among men.97 In the European Study of the Epidemiology of Mental Disorders project, alcohol abuse had the weakest association with depression among all the comorbid patterns assessed.98 Some investigators speculate that field research assessments of the DSM alcohol abuse construct may tap non-pathological drinking patterns that occur part and parcel with adolescent or young adult drinking experiences, particularly for young male drinkers.98,99
One of the issues to consider in understanding these relationships is the role of concurrence and persistence of depressed mood and drinking. These study estimates may challenge the idea that depressed mood must take place concurrently with drinking behaviors to impact the development of some alcohol-related outcomes. Furthermore, depressive conditions that occur in childhood may increase vulnerability for maladaptive drinking outcomes, whereas similar conditions that occur later in life may not be as strongly associated. This “window of vulnerability” may be in place for some but not all comorbid relationships. Childhood mood disturbances occur at a significant stage for neurobiologic development.e.g., 100 During this critical period, mood disturbances may inhibit the normal progression in a child's ability to develop mechanisms to cope with stress and negative expectations, and may increase the likelihood that coping skills to handle stress-related occurrences are poorly developed, or remain immature. Early manifestations of depressive conditions also can be difficult to recognize by families and health care providers. Whether these features are clinically relevant is typically quite a challenge. Our assessment of depressed mood queried about feelings of ‘being crabby’, ‘frequent crying spells’ and ‘being sad’. These feelings are common to many children, and it may be difficult for families and clinicians to recognize when they may be indicative of a psychiatric disturbance, or when further evaluation is warranted. Although early depressive feelings may be a potential predictor of alcohol involvement, other psychopathologic conditions also are associated with risk for alcohol disorders including disruptive behaviors, other substance use, anxiety and affective disorders.101-106
There are several limitations in our analyses which should be mentioned. First, residual confounding may be present (e.g., familial history of psychopathology (depression, anxiety, alcohol dependence, antisocial personality), or participant history of childhood trauma). For example, family history may be associated with early occurrence of depressive conditions, and increased vulnerability for alcohol involvement85,86,107,108 due to genetic vulnerabilities, as well as familial influences such as modeling behavior, provision of support, and parental monitoring.67,70,71,109 However, we were able to include information on report of illicit drug use and heavy drinking in the caregiver which might help to hold constant these potential confounding characteristics. Second, our assessment of depressed mood in childhood did not include a structured psychiatric interview and so cannot be regarded as diagnostic of depression. In addition, the measure used identified features which may be present in a range of psychopathology. However, as we discussed previously, this measure had adequate internal consistency, and was associated with CIDI-UM assessed major depression (evidence of predictive validity). Third, as mentioned previously, our assessment of alcohol dependence focused upon ‘clinically significant dependence syndrome’. As discussed by Degenhardt et al.,75 this use of clinical significance criteria may miss some individuals who developed a milder form of alcohol dependence. Fourth, as with any prospective study, particularly one extending across long intervals, there was participant attrition and missing information. We have addressed these concerns by assessing two statistical strategies: including covariates for missingness in the regression models, and multiple imputation. Yet, the potential for bias remains a possibility. Fifth, generalizability of the findings from this sample of school-attending youths rests upon replication of the findings elsewhere.
Notwithstanding these limitations, the study contributes new information about childhood depressed mood and subsequent alcohol outcomes, as well as possible childhood predictors of alcohol involvement that may extend across adolescence into young adulthood. The effects of internalizing symptoms on transitional and sequential stages of drinking will need to be explored in future research. In addition, this research can be extended from this initial platform of evidence in an exploration of the potential moderating and mediating influences attributable to other drug use, externalizing behaviors, and expectancies associated with drinking alcohol. Whether and how the observed mood manifestations change, persist, or progress through the life stages deserves scrutiny. Co-occurring transitions in drinking behavior may have important implications for identifying and targeting high risk groups for prevention and early intervention efforts.
Acknowledgments
The analyses for this work were supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (AA014869). Data gathering for the study was completed by grants DA04392 and DA09897, and a career development award K05DA015799 (JCA) from the National Institute on Drug Abuse.
Appendix
Description of Protocol for Assessment of Alcohol Problems
1.0 Background
The assessment of alcohol problems for the NIDA ‘Transitions Through Adulthood’ project, which was used for this manuscript, was designed to make the follow-up data congruent with the concurrent ‘National Comorbidity Survey-Replication’ survey (NCS-R) being fielded by Professor Ronald Kessler and collaborators at Harvard University. By keeping the assessment methodology constant, the collaborative research teams would be able to compare and contrast cross-sectional findings from the NCS-R's nationally representative sample with prospective and longitudinal findings from this “Transitions” project.
For this reason, the Transitions team obtained the NCS-R standardized alcohol problems assessment module and prepared to administer it exactly as it was being fielded in the NCS-R. Upon inspection of the module, the Transition team leaders noticed that the NCS-R approach involved assessment of ‘clinically significant’ alcohol dependence, with a conceptual and methodological refinement recommended by Narrow et al. (2002)1,2. This refinement gives emphasis to the DSM-IV stipulation that alcohol dependence should involve a ‘maladaptive pattern’ of drinking with ‘clinically significant impairment or distress.’ As argued by Narrow and colleagues, a neglect of these ‘clinical significance’ issues can yield epidemiological over-estimates of disease burden associated with alcohol dependence and other psychiatric and behavioral disturbances. These issues, introduced by Narrow et al. (2002)1, have been discussed more recently in a series of articles by Degenhardt et al.3-5, in which it has been demonstrated that the proposed refinement does yield some attenuation of the alcohol dependence prevalence estimates, but yields little attenuation of estimates for dependence syndromes involving cannabis, cocaine, or other drugs used illegally or extra-medically. The recommended approach is one that requires the investigator to state whether the object of study is ‘all’ alcohol dependence cases, or the necessary smaller and more conservatively specified number of ‘clinically significant’ alcohol dependence’ cases.
2.0 Specific Standardized Survey Questions about Drinking & Alcohol Problems
The NCS-R approach first posed standardized survey questions about lifetime history of drinking, age of onset of drinking, and facets of drinking such as recency, volume, and frequency. The first question in the module was worded as follows:
The next questions are about your use of alcoholic beverages, including beer, wines, and hard liquor like vodka, gin, or whiskey. How old were you the very first time you ever had a drink with alcohol in it, even just a sip or a taste?
Other illustrative items on facets of drinking included:
Think about the years in your life when you drank alcohol the most. During those years, how often did you usually have at least one alcohol drink - nearly every day, three to four days a week, one to two days a week, one to three days a month, or less than once a month?
2.1 Maladaptive Drinking & Drink-Related Social Role Impairments and Distress
Thereafter, there were standardized questions on the issues of maladaptive drinking, and drink-related social role impairments. Studying these items and the ‘gating’ or ‘skip pattern’ branches within the modules, the Transitions team noticed that the NCS-R ‘clinical significance’ items provided decent coverage of the issues of maladaptive drinking and drink-related social role impairments. The specific sequence of items on these issues are:
[Question 12 series]: The next questions are about problems you may have had because of drinking alcohol.
First, was there ever a time in your life when your drinking or being hung over frequently interfered with your work or responsibilities at school, on the job, or at home?
Was there ever a time in your life when your drinking caused arguments or other serious or repeated problems with your family, friends, neighbors, or co-workers? Did you continue to drink even though it caused problems with these people?
Were there times in your life when you were often under the influence of alcohol in situations where you could get hurt, for example when riding a bicycle, driving, operating a machine, or anything else?
Were you more than once arrested or stopped by the police because of drunk driving or drunk behavior?
There was less complete coverage of drink- or dependence-related distress to the self (i.e., recognized by the drinker) or distress to others (e.g., family members, friends, employers). For this reason, the Transitions team added an item on this topic, as follows, which was intended to increase the sensitivity of the module's items with respect to ‘clinical significant’ alcohol dependence in the DSM-referenced domain of distress:
Was there ever a time in your life when people told you they thought you drank too much or when you thought you might have a drinking problem?
2.2 Alcohol Dependence
The rest of the module was then set up with standardized NCS-R items on alcohol dependence, which permitted algorithmic combination of items into DSM criterion ‘testlets’ such that at least one item in the testlet had to have been experienced if the drinker was to be assigned to the category of ‘clinically significant’ alcohol dependence. The items in the alcohol dependence sub-section of the alcohol module were as follows. Informed readers will recognize the provenance of these items in relation to the original Renard Diagnostic Interview of the 1970s, the Diagnostic Interview Schedule of the late 1970s and 1980s, and the University of Michigan version of the Composite Diagnostic Interview used in the original NCS survey of the early 1990s.
[Question 19 series]: The next questions are about some other problems you may have had because of drinking alcohol.
Was there ever a time in your life when you often had such a strong desire to drink that you couldn't resist taking a drink or found it difficult to think of anything else?
Did you ever need to drink a larger amount of alcohol to get an effect, or did you ever find that you could no longer get a “buzz” or high on the amount you used to drink?
People who cut down or stop drinking after drinking steadily for some time may not feel well. These feelings are more intense and can last longer than the usual hangover. Did you ever have times when you stopped, cut down, or went without drinking and then experienced symptoms like fatigue, headaches, diarrhea, the shakes, or emotional problems?
Did you ever have times when you took a drink to keep from having problems like these?
Did you ever have times when you started drinking even though you promised yourself you wouldn't, or when you drank a lot more than you intended?
Were there ever times when you drank more frequently or for more days in a row than you intended?
Did you have times when you started drinking and become drunk when you didn't want to?
Were there times when you tried to stop or cut down on your drinking and found that you were not able to?
Did you ever have periods of several days or more when you spent so much time drinking or recovering from the effects of alcohol that you had little time for anything else?
Did you ever have a period of a month or longer when you gave up or greatly reduced important activities because of your drinking - like sports, work, or seeing friends or family?
Did you ever continue to drink when you knew you had a serious physical or emotional problem that might have been caused by or made worse by drinking?
Thereafter, the standardized interview schedule poses questions about each reported problem, with respect to age when the problem was first experienced, the recency of the problem, and the drinker's age when that problem was last experienced (so as to enable studies of onset and offset of individual diagnostic criteria).
2.3 Temporal Clustering of Clinical Features of Alcohol Dependence
Because the DSM criteria specify clustering of drink-related problems, there also was a set of standardized questions on temporal clustering -- for example:
Did you ever have three (or more) of these problems in the same year [READ IF NECESSARY TO REMIND ANY YESES MARKED IN QUESTION 12 AND QUESTION 19 SERIES]?
How old were you the first time you had three (or more) of these problems in the same year?
2.4 Additional Items on Recency of Specific Forms of Drink-Related Harm
The Transitions team closed the alcohol module with a series of standardized items on the recency of drink-related physical health harms, familial harms, impulsive behavior later regretted, failure to live up to expectations, and drink-related unhappiness, as follows:
During the past 12 months, how much has your physical health been harmed by your drinking - a lot, some, a little, or not at all?
During the past 12 months, how much has your family been hurt by your drinking?
During the past 12 months, how much have you done impulsive things that you regretted later because of your drinking?
During the past 12 months, how much have you failed to do what was expected of you because of your drinking?
During the past 12 months, how much have you been unhappy because of your drinking?
3.0 Positioning of the Alcohol Module Within the Interview Schedule
The Transitions team positioned the alcohol module as Module F within the sequence of interview schedule modules. That is, it was administered midway through the assessment, and was the 6th module. Prior modules helped establish and promote trust and rapport via a focus on health issues. For example, the very first item of the first module (Module A) started with this introduction and question to help orient the participant to the health-related content of the assessment and to promote engagement with the participant via his or her here and now subjective evaluation of current health status:
To begin, I would like to get a general view of the kind of health problems, physical or mental, that might have been troubling you over the past week. Would you say that you have recently enjoyed good mental and physical health, or have you had problems during the past week?
The Alcohol Module was preceded by a module on the topic of drug opportunities. It was followed by coverage of non-alcohol drug dependence. The length of time from the start of the assessment session to the beginning of Module F on alcohol was approximately 20 minutes. Hence, participants were not too fatigued by the time they were asked the alcohol questions, which then set the context for questions on the sometimes more sensitive topics of illegal drug use or extra-medical drug use (e.g., using more than the doctor prescribed or for reasons other than prescribed).
4.0 The Gating Approach to Assessment of ‘Clinically Significant’ Alcohol Dependence
The Transitions team implemented a gating approach so as to focus the inquiry on DSM-specified ‘clinically significant’ alcohol dependence, as discussed in Section 1 of this appendix, and by Narrow et al., (2002)1,2 and in the series of papers by Degenhardt and colleagues3-5. In particular, the alcohol dependence questions were asked only when the drinker manifest a maladaptive pattern of drinking with clinical significance as measured in terms of the above-referenced items on drink-related social maladaptation, social role impairments, or distress to the drinker or to others. Necessarily, this approach yields smaller and more conservative estimates of the occurrence of the alcohol dependence syndrome than might be obtained if the focus is on more general alcohol dependence syndrome concepts, ignoring the ‘clinical significance’ refinements recommended by Narrow et al. in the 2002 paper.
References for Appendix 1
- 1.Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys' estimates. Arch Gen Psychiatry. 2002;59(2):115–23. doi: 10.1001/archpsyc.59.2.115. [DOI] [PubMed] [Google Scholar]
- 2.Wakefield JC, Spitzer RL. Lowered estimates--but of what? Arch Gen Psychiatry. 2002;59(2):129–30. doi: 10.1001/archpsyc.59.2.129. [DOI] [PubMed] [Google Scholar]
- 3.Degenhardt L, Bohnert KM, Anthony JC. Case ascertainment of alcohol dependence in general population surveys: “gated” versus “ungated” approaches. Int J Methods Psychiatr Res. 2007;16(3):111–23. doi: 10.1002/mpr.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degenhardt L, Cheng H, Anthony JC. Assessing cannabis dependence in community surveys: Methodological issues. Int J Methods in Psychiatr. 2007;16(2):43–51. doi: 10.1002/mpr.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Degenhardt L, Bohnert KM, Anthony JC. Assessment of cocaine and illegal drug dependence in the general population: “gated” vs. “ungated” approaches. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2007.09.024. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
- 1.Salokangas RK, Poutanen O. Risk factors for depression in primary care. Findings of the TADEP project. J Affect Disord. 1998;48(2-3):171–80. doi: 10.1016/s0165-0327(97)00171-7. [DOI] [PubMed] [Google Scholar]
- 2.Brown RA, Monti PM, Myers MG, Martin RA, Rivinus T, Dubreuil ME, Rohsenow DJ. Depression among cocaine abusers in treatment: relation to cocaine and alcohol use and treatment outcome. Am J Psychiatry. 1998;155(2):220–5. doi: 10.1176/ajp.155.2.220. [DOI] [PubMed] [Google Scholar]
- 3.Miller NS, Klamen D, Hoffmann NG, Flaherty JA. Prevalence of depression and alcohol and other drug dependence in addictions treatment population. J Psychoactive Drugs. 1996;29(2):111–24. doi: 10.1080/02791072.1996.10524384. [DOI] [PubMed] [Google Scholar]
- 4.Davidson KM. Diagnosis of depression in alcohol dependence: changes in prevalence with drinking status. Br J Psychiatry. 1995;166(2):199–204. doi: 10.1192/bjp.166.2.199. [DOI] [PubMed] [Google Scholar]
- 5.Davidson KM, Blackburn IM. Co-morbid depression and drinking outcome in those with alcohol dependence. Alcohol Alcohol. 1998;33:482–7. doi: 10.1093/alcalc/33.5.482. [DOI] [PubMed] [Google Scholar]
- 6.Curran GM, Flynn HA, Kirchner J, Booth BM. Depression after alcohol treatment as a risk factor for relapse among male veterans. J Subst Abuse Treat. 2000;19:259–65. doi: 10.1016/s0740-5472(00)00107-0. [DOI] [PubMed] [Google Scholar]
- 7.Bobo JK, McIlvain HE, Leed-Kelly A. Depression screening scores during residential drug treatment and risk of drug use after discharge [published erratum appears in Psychiatr Serv. 1998 June;49(6):828]. Psychiatr Serv. 1998;49(5):693–5. doi: 10.1176/ps.49.5.693. [DOI] [PubMed] [Google Scholar]
- 8.Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR. The effect of depression on return to drinking: a prospective study. Arch Gen Psychiatry. 1998;55(3):259–65. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- 9.Pettinati HM, Pierce JD, Jr, Wolf AL, Rukstalis MR, O'Brien CP. Gender differences in comorbidly depressed alcohol-dependent outpatients. Alcohol Clin Exp Res. 1997;21(9):1742–6. [PubMed] [Google Scholar]
- 10.Donohue B, Acierno R, Kogan E. Relationship of depression with measures of social functioning in adult drug abusers. Addict Behav. 1996;21(2):211–6. doi: 10.1016/0306-4603(95)00051-8. [DOI] [PubMed] [Google Scholar]
- 11.Driessen M, Meier S, Hill A, Wetterling T, Lange W, Junghanns K. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol Alcohol. 2001;36:249–55. doi: 10.1093/alcalc/36.3.249. [DOI] [PubMed] [Google Scholar]
- 12.Roggla H, Uhl A. Depression and relapses in treated chronic alcoholics. Int J Addict. 1995;30(3):337–49. doi: 10.3109/10826089509048730. [DOI] [PubMed] [Google Scholar]
- 13.Brown SA, Inaba RK, Gillin JC, Schuckit MA, Stewart MA, Irwin MR. Alcoholism and affective disorder: clinical course of depressive symptoms. Am J Psychiatry. 1995;152(1):45–52. doi: 10.1176/ajp.152.1.45. [DOI] [PubMed] [Google Scholar]
- 14.Salloum IM, Mezzich JE, Cornelius J, Day NL, Daley D, Kirisci L. Clinical profile of comorbid major depression and alcohol use disorders in an initial psychiatric evaluation. Compr Psychiatry. 1995;36(4):260–6. doi: 10.1016/s0010-440x(95)90070-5. [DOI] [PubMed] [Google Scholar]
- 15.Cornelius JR, Salloum IM, Mezzich J, Cornelius MD, Fabrega H, Ehler JG, Ulrich RF, Thase ME, Mann JJ. Disproportionate suicidality in patients with comorbid major depression and alcoholism. Am J Psychiatry. 1995;152(3):358–64. doi: 10.1176/ajp.152.3.358. [DOI] [PubMed] [Google Scholar]
- 16.Worthington J, Fava M, Agustin C, Alpert J, Nierenberg AA, Pava JA, Rosenbaum JF. Consumption of alcohol, nicotine, and caffeine among depressed outpatients. Relationship with response to treatment. Psychosomatics. 1996;37(6):518–22. doi: 10.1016/S0033-3182(96)71515-3. [DOI] [PubMed] [Google Scholar]
- 17.Harrington R, Fudge H, Rutter M, Pickles A, Hill J. Adult outcomes of childhood and adolescent depression. I. Psychiatric status. Arch Gen Psychiatry. 1990;47(5):465–73. doi: 10.1001/archpsyc.1990.01810170065010. [DOI] [PubMed] [Google Scholar]
- 18.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 19.Weissman MM, Myers JK. Clinical depression in alcoholism. Am J Psychiatry. 1980;137(3):372–373. doi: 10.1176/ajp.137.3.372. [DOI] [PubMed] [Google Scholar]
- 20.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- 21.Moscato BS, Russell M, Zielezny M, Bromet E, Egri G, Mudar P, Marshall JR. Gender differences in the relation between depressive symptoms and alcohol problems: A longitudinal perspective. Am J Epidemiol. 1997;146:966–74. doi: 10.1093/oxfordjournals.aje.a009224. [DOI] [PubMed] [Google Scholar]
- 22.Aneshensel CS, Huba GJ. Depression, alcohol use, and smoking over one year: A four-wave longitudinal causal model. J Abnorm Psychol. 1983;92:134–50. doi: 10.1037//0021-843x.92.2.134. [DOI] [PubMed] [Google Scholar]
- 23.Hartka E, Johnstone B, Leino EV, Motoyoshi M, Temple MT, Fillmore KM. The Collaborative Alcohol-Related Longitudinal Project. A meta-analysis of depressive symptomatology and alcohol consumption over time. Brit J Addict. 1991;86:1283–98. doi: 10.1111/j.1360-0443.1991.tb01704.x. [DOI] [PubMed] [Google Scholar]
- 24.Dixit AR, Crum RM. Depression and the risk of heavy alcohol use in women: A prospective study. Am J Psychiatry. 2000;157:751–758. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- 25.Crum RM, Storr CL, Chan YF. Depression syndromes with risk of alcohol dependence in adulthood: a latent class analysis. Drug Alcohol Depend. 2005;79:71–81. doi: 10.1016/j.drugalcdep.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 26.Costello EJ, Sung M, Worthman C, Angold A. Pubertal maturation and the development of alcohol use and abuse. Drug Alcohol Depend. 2007;88S:S50–S59. doi: 10.1016/j.drugalcdep.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 27.Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug Alcohol Depend. 2007;88S:S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 29.Rao U, Daley SE, Hammen C. Relationship between depression and substance use disorders in adolescent women during the transition to adulthood. J Am Acad Child Adolesc Psychiatry. 2000;39(2):215–22. doi: 10.1097/00004583-200002000-00022. [DOI] [PubMed] [Google Scholar]
- 30.Greeley J, Oei T. Alcohol and tension reduction. In: Leonard KE, Blane HT, editors. Psychological theories of drinking and alcoholism. 2nd ed. The Guilford Press; New York, NY: 1999. pp. 14–53. [Google Scholar]
- 31.Sher KJ, Levenson RW. Risk for alcoholism and individual differences in the stress-response-dampening effect of alcohol. J Abnorm Psychol. 1982;91(5):350–67. doi: 10.1037//0021-843x.91.5.350. [DOI] [PubMed] [Google Scholar]
- 32.Bandura A. Social learning theory. Prentice Hall; Englewood Cliffs, N.J.: 1977. [Google Scholar]
- 33.Evans DM, Dunn NJ. Alcohol expectancies, coping responses and self-efficacy judgments: a replication and extension of Copper et al.'s 1988 study in a college sample. J Stud Alcohol. 1995;56(2):186–193. doi: 10.15288/jsa.1995.56.186. [DOI] [PubMed] [Google Scholar]
- 34.Maisto SA, Connors GJ, Zywiak WH. Alcohol treatment, changes in coping skills, self-efficacy, and levels of alcohol use and related problems 1 year following treatment initiation. Psychol Addict Behav. 2000;14(3):257–266. doi: 10.1037//0893-164x.14.3.257. [DOI] [PubMed] [Google Scholar]
- 35.Christiansen BA, Goldman MS, Brown SA. The differential development of adolescent alcohol expectancies may predict adult alcoholism. Addict Behav. 1985;10:299–306. doi: 10.1016/0306-4603(85)90011-5. [DOI] [PubMed] [Google Scholar]
- 36.Kassell JD, Jackson SI, Unrod M. Generalized expectancies for negative mood regulation and problem drinking among college students. J Stud Alcohol. 2000;61(2):332–340. doi: 10.15288/jsa.2000.61.332. [DOI] [PubMed] [Google Scholar]
- 37.Goldstein AL, Wall AM, McKee SA, Hinson RE. Accesibility of alcohol expectancies from memory: Impact of mood and motives in college student drinkers. J Stud Alcohol. 2004;65:95–104. doi: 10.15288/jsa.2004.65.95. [DOI] [PubMed] [Google Scholar]
- 38.Catanzaro SJ, Laurent J. Perceived family support, negative mood regulation expectancies, coping, and adolescent alcohol use: Evidence of mediation and moderation effects. Addict Behav. 2004;29:1779–1797. doi: 10.1016/j.addbeh.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 39.Kellam SG, Wethamer-Larsson, Dolan LJ, Brown CH, Mayer LS, Rebok GW, Anthony JC, Laudolff J, Edelsohn G, Wheeler L. Developmental epidemiologically based preventive trials: Baseline modeling of early target behaviors and depressive symptoms. Am J Community Psychol. 1991;19:563–584. doi: 10.1007/BF00937992. [DOI] [PubMed] [Google Scholar]
- 40.Mrazek PG, Haggerty RJ, editors. Reducing risks for mental disorders: Frontiers for preventive intervention research. National Academy Press; Washington, DC: 1994. [PubMed] [Google Scholar]
- 41.Kellam SG, Brown CH, Rubin BR, Ensminger ME. Paths leading to teenage psychiatric symptoms and substance use: Developmental epidemiological studies in Woodlawn. In: Guze SB, Earls FJ, Barrett JE, editors. Childhood psychopathology and development. Raven Press; New York: 1983. [Google Scholar]
- 42.Nellissery M, Feinn RS, Covault J, Gelernter J, Anton RF, Pettinati H, Moak D, Mueller T, Kranzler HR. Alleles of a functional serotonin transporter promoter polymorphism are associated with major depression in alcoholics. Alcohol Clin Exp Res. 2003;27(9):1402–8. doi: 10.1097/01.ALC.0000085588.11073.BB. [DOI] [PubMed] [Google Scholar]
- 43.Kendler KS, Health AC, Neale MC, et al. Alcoholism and major depression in women. A twin study of the causes of comorbidity. Arch Gen Psychiatry. 1993;50:690–8. doi: 10.1001/archpsyc.1993.01820210024003. [DOI] [PubMed] [Google Scholar]
- 44.Dohrenwend BP, Levav I, Shrout PE, et al. Socioeconomic status and psychiatric disorders: The causation-selection issue. Science. 1992;255:946–52. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- 45.Maier W, Merikangas K. Co-occurrence and co-transmission of affective disorders and alcoholism in families. Br J Psychiatry. 1996;(Suppl(30)):93–100. [PubMed] [Google Scholar]
- 46.Clark DB, De Bellis MD, Lynch KG, Cornelius JR, Martin CS. Physical and sexual abuse, depression and alcohol use disorders in adolescents: onsets and outcomes. Drug Alcohol Depend. 2003;69(1):51–60. doi: 10.1016/s0376-8716(02)00254-5. [DOI] [PubMed] [Google Scholar]
- 47.Merikangas KR, Risch NJ, Weissman MM. Comorbidity and co-transmission of alcoholism, anxiety and depression. Psychol Med. 1994;24:69–80. doi: 10.1017/s0033291700026842. [DOI] [PubMed] [Google Scholar]
- 48.Schuckit MA, Smith TL, Danko GP, Pierson J, Trim R, Nurnberger JI, Kramer J, Kuperman S, Bierut LJ, Hesselbrock V. A comparison of factors associated with substance-induced versus independent depressions. J Stud Alcohol Drugs. 2007;68(6):805–12. doi: 10.15288/jsad.2007.68.805. [DOI] [PubMed] [Google Scholar]
- 49.Fu Q, Health AC, Bucholz KK, Nelson E, Goldberg J, Lyons MJ, True WR, Jacob T, Tsuang MT, Eisen SA. Shared genetic risk of major depression, alcohol dependence, and marijuana dependence: contribution of antisocial personality disorder in men. Arch Gen Psychiatry. 2002;59(12):1125–32. doi: 10.1001/archpsyc.59.12.1125. [DOI] [PubMed] [Google Scholar]
- 50.Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: predicting young adult substance use disorders, anxiety, and depression. J Abnorm Psychol. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- 51.Crum RM, Storr CL, Ialongo N, Anthony JC. Is depressed mood in childhood associated with an increased risk for initiation of alcohol use during early adolescence? Addict Behav. doi: 10.1016/j.addbeh.2007.05.008. In press (Epub 2007 May 23) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gilman SE, Abraham HD. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alcohol Depend. 2001;63:277–86. doi: 10.1016/s0376-8716(00)00216-7. [DOI] [PubMed] [Google Scholar]
- 53.Wang J, Patten SB. A prospective study of sex-specific effects of major depression on alcohol consumption. Can J Psychiatry. 2001;46:422–5. doi: 10.1177/070674370104600507. [DOI] [PubMed] [Google Scholar]
- 54.King AC, Bernardy NC, Hauner K. Stressful events, personality, and mood disturbance: gender differences in alcoholics and problem drinkers. Addict.Behav. 2003;28(1):171–87. doi: 10.1016/s0306-4603(01)00264-7. [DOI] [PubMed] [Google Scholar]
- 55.Maag JW, Irvin DM. Alcohol use and depression among African-American and Caucasian adolescents. Adolescence. 2005;40(157):87–101. [PubMed] [Google Scholar]
- 56.Kellam SG, Anthony JC. Targeting antecedents to prevent tobacco smoking: Findings from an epidemiologically based randomized field trial. Am J Public Health. 1998;99:1490–5. doi: 10.2105/ajph.88.10.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Storr CL, Reboussin BA, Anthony JC. Early childhood misbehavior and the estimated risk of becoming tobacco-dependent. Am J Epidemiol. 2004;160(2):126–130. doi: 10.1093/aje/kwh184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reed PL, Storr CL, Anthony JC. Drug dependence enviromics: job strain in the work environment and risk of becoming drug-dependent. Am J Epidemiol. 2006;163(5):404–411. doi: 10.1093/aje/kwj064. [DOI] [PubMed] [Google Scholar]
- 59.Wu LT, Anthony JC. Tobacco smoking and depressed mood in late childhood and early adolescence. Am J Public Health. 1999;89(12):1837–40. doi: 10.2105/ajph.89.12.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen LS, Anthony JC, Crum RM. Perceived cognitive competence, depressive symptoms and the incidence of alcohol-related problems in urban school children. J Child Adolesc Subst Abuse. 1999;8(4):37–53. [Google Scholar]
- 61.World Health Organization . World Health Organization, Composite International Diagnostic Interview. World Health Organization; Geneva: 1990. 1990. [Google Scholar]
- 62.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Fourth ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 63.Johnson EO, Arria AM, Borges G, Ialongo N, Anthony JC. The growth of conduct problem behaviors from middle childhood to early adolescence: sex differences and the suspected influence of early alcohol use. J Stud Alcohol. 1995;56(6):661–71. doi: 10.15288/jsa.1995.56.661. [DOI] [PubMed] [Google Scholar]
- 64.Elliott DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Sage Publications; Beverly Hills, CA: 1985. [Google Scholar]
- 65.Elliott DS, Huizinga D, Menard S. Multiple problem youth: delinquency, substance use, and mental health problems. Springer Verlag; New York: 1989. [Google Scholar]
- 66.Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug Alcohol Depend. 1996;43:155–161. doi: 10.1016/s0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- 67.Duncan TE, Duncan SC, Hops H. The effects of family cohesiveness and peer encouragement on the development of adolescent alcohol use: a cohort-sequential approach to the analysis of longitudinal data. J Stud Alcohol. 1994;55(5):588–99. doi: 10.15288/jsa.1994.55.588. [DOI] [PubMed] [Google Scholar]
- 68.Moss HB, Kirisci L. Aggressivity in adolescent alcohol abusers: relationship with conduct disorder. Alcohol Clin Exp Res. 1995;19(3):642–6. doi: 10.1111/j.1530-0277.1995.tb01561.x. [DOI] [PubMed] [Google Scholar]
- 69.Curran PJ, Stice E, Chassin L. The relation between adolescent alcohol use and peer alcohol use: a longitudinal random coefficients model. J Consult Clin Psychol. 1997;65(1):130–40. doi: 10.1037//0022-006x.65.1.130. [DOI] [PubMed] [Google Scholar]
- 70.Mason WA, Windle M. Family, religious, school and peer influences on adolescent alcohol use: a longitudinal study. J Stud Alcohol. 2001;62(1):44–53. doi: 10.15288/jsa.2001.62.44. [DOI] [PubMed] [Google Scholar]
- 71.Nash SG, McQueen A, Bray JH. Pathways to adolescent alcohol use: family environment, peer influence, and parental expectations. J Adolesc Health. 2005;37(1):19–28. doi: 10.1016/j.jadohealth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 72.Fite PJ, Colder CR, O'Connor RM. Childhood behavior problems and peer selection and socialization: risk for adolescent alcohol use. Addict Behav. 2006;31(8):1454–9. doi: 10.1016/j.addbeh.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 73.Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley and Sons; New York: 1987. [Google Scholar]
- 74.STATA Corp. STATA Statistical Software. Release 7.0. Reference Manual. STATA Press; Texas: 2000. [Google Scholar]
- 75.Degenhardt L, Bohnert KM, Anthony JC. Case ascertainment of alcohol dependence in general population surveys: “gated” versus “ungated” approaches. Int J Methods Psychiatr Res. 2007;16(3):111–23. doi: 10.1002/mpr.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rutledge PC, Sher KJ. Heavy drinking from the freshman year into early young adulthood: the roles of stress, tension-reduction drinking motives, gender and personality. J Stud Alcohol. 2001;62:457–466. doi: 10.15288/jsa.2001.62.457. [DOI] [PubMed] [Google Scholar]
- 77.Catanzaro SJ, Wasch HH, Kirsch I, Mearns J. Coping-related expectancies and dispositions as prospective predictors of coping responses and symptoms. J Pers. 2000;68(4):757–788. doi: 10.1111/1467-6494.00115. [DOI] [PubMed] [Google Scholar]
- 78.Cooper ML, Russel M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: moderating effects of gender, coping, and alcohol expectancies. J Abnorm Psychol. 1992;101(1):139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- 79.Laurent J, Catanzaro SJ, Callan MK. Stress, alcohol-related expectancies and coping preferences: a replication with adolescents of the Cooper et al. (1992) model. J Stud Alcohol. 1997;58:644–651. doi: 10.15288/jsa.1997.58.644. [DOI] [PubMed] [Google Scholar]
- 80.Simons-Morton B, Haynie DL, Crump AD, Saylor KE, Eitel P, Yu K. Expectancies and other psychosocial factors associated with alcohol use among early adolescent boys and girls. Addict Behav. 1999;24(2):229–238. doi: 10.1016/s0306-4603(98)00095-1. [DOI] [PubMed] [Google Scholar]
- 81.Cable N, Sacker A. The role of adolescent social disinhibition expectancies in moderating the relationship between psychological distress and alcohol use and misuse. Addict Behav. 2007;32(2):282–295. doi: 10.1016/j.addbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 82.Christiansen BA, Smith GT, Roehling PV, Goldman MS. Using alcohol expectancies to predict adolescent drinking behavior after one year. J Consult Clin Psychol. 1989;57(1):93–99. doi: 10.1037//0022-006x.57.1.93. [DOI] [PubMed] [Google Scholar]
- 83.Catanzaro SJ, Laurent J. Perceived family support, negative mood regulation expectancies, coping, and adolescent alcohol use: evidence of mediation and moderation effects. Addict Behav. 2004;29(9):1779–97. doi: 10.1016/j.addbeh.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 84.Maher BS, Marazita ML, Zubenko WN, Kaplan BB, Zubenko GS. Genetic segregation analysis of alcohol and other substance-use disorders in families with recurrent, early-onset major depression. Am J Drug Alcohol Abuse. 2002;28(4):711–31. doi: 10.1081/ada-120015878. [DOI] [PubMed] [Google Scholar]
- 85.Tambs K, Harris JR, Magnus P. Genetic and environmental contributions to the correlation between alcohol consumption and symptoms of anxiety and depression. Results from a bivariate analysis of Norwegian twin data. Behav Genet. 1997;27(3):241–50. doi: 10.1023/a:1025662114352. [DOI] [PubMed] [Google Scholar]
- 86.Hill EM, Blow FC, Young JP, Singer KM. Family history of alcoholism and childhood adversity: joint effects on alcohol consumption and dependence. Alcohol Clin Exp Res. 1994;18(5):1083–90. doi: 10.1111/j.1530-0277.1994.tb00085.x. [DOI] [PubMed] [Google Scholar]
- 87.Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, Moffitt TE. Association between children's experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002;360(9346):1640–5. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lieb R, Isensee B, Hofler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Arch Gen Psychiatry. 2002;59(4):365–74. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- 89.Puig-Antich J, Goetz D, Davies M, Kaplan T, Davies S, Ostrow L, Asnis L, Twomey J, Iyengar S, Ryan ND. A controlled family history study of prepubertal major depressive disorder. Arch Gen Psychiatry. 1989;46(5):406–18. doi: 10.1001/archpsyc.1989.01810050020005. [DOI] [PubMed] [Google Scholar]
- 90.Kovacs M, Devlin B, Pollock M, Richards C, Mukerji P. A controlled family history study of childhood-onset depressive disorder. Arch Gen Psychiatry. 1997;54(7):613–23. doi: 10.1001/archpsyc.1997.01830190033004. [DOI] [PubMed] [Google Scholar]
- 91.Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug Alcohol Depend. 2007;88S:S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Swendsen JD, Merikangas KR, Canino GJ, Kessler RC, Rubio-Stipec M, Angst J. The comorbidity of alcoholism with anxiety and depressive disorders in four geographic communities. Compr Psychiatry. 1998;39(4):176–184. doi: 10.1016/s0010-440x(98)90058-x. [DOI] [PubMed] [Google Scholar]
- 93.Henry B, Feehan M, McGee R, Stanton W, Moffitt TE, Silva P. The importance of conduct problems and depressive symptoms in predicting adolescent substance use. J Abnorm Child Psychol. 1993;21(5):469–480. doi: 10.1007/BF00916314. [DOI] [PubMed] [Google Scholar]
- 94.Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: effects of timing and sex. J Clin Child Psychol. 1999;28(3):298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- 95.King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psycho-pathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- 96.Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope and alcohol use and abuse in unipolar depression: a 10-year model. J Abnorm Psychol. 2003;112(1):159–165. [PubMed] [Google Scholar]
- 97.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in The National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 98.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lepine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martinez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacin C, Romera B, Taub N, Vollebergh WA, ESEMeD/MHEDEA 2000 Investigators. European Study of the Epidemiology of Mental Disorders (ESEMeD) Project 12-Month comorbidity patterns and associated factors in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand. Suppl. 2004;(420):28–37. doi: 10.1111/j.1600-0047.2004.00328.x. [DOI] [PubMed] [Google Scholar]
- 99.de Graaf R, Bijl RV, Spijker J, Beekman AT, Vollebergh WA. Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance use disorders--findings from the Netherlands Mental Health Survey and Incidence Study. Soc Psychiatry Psychiatr Epidemiol. 2003;38(1):1–11. doi: 10.1007/s00127-003-0597-4. [DOI] [PubMed] [Google Scholar]
- 100.Nolan CL, Moore GJ, Madden R, Farchione T, Bartoi M, Lorch E, Stewart CM, Rosenberg DR. Prefrontal cortical volume in childhood-onset major depression. Arch Gen Psychiatry. 2002;59:173–179. doi: 10.1001/archpsyc.59.2.173. [DOI] [PubMed] [Google Scholar]
- 101.Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry. 2007;64(10):1145–52. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- 102.Goldstein RB, Dawson DA, Saha TD, Ruan WJ, Compton WM, Grant BF. Antisocial behavioral syndromes and DSM-IV alcohol use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res. 2007;31(5):814–28. doi: 10.1111/j.1530-0277.2007.00364.x. [DOI] [PubMed] [Google Scholar]
- 103.Kuperman S, Schlosser SS, Kramer JR, Bucholz K, Hesselbrock V, Reich T, Reich W. Developmental sequence from disruptive behavior diagnosis to adolescent alcohol dependence. Am J Psychiatry. 2001;158(12):2022–6. doi: 10.1176/appi.ajp.158.12.2022. [DOI] [PubMed] [Google Scholar]
- 104.Kushner MG, Sher KJ, Erickson DJ. Prospective analysis of the relation between DSM-III anxiety disorders and alcohol use disorders. Am J Psychiatry. 1999;156(5):723–32. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- 105.Goodwin RD, Lieb R, Hoefler M, Pfister H, Bittner A, Beesdo K, Wittchen HU. Panic attack as a risk factor for severe psychopathology. Am J Psychiatry. 2004;161(12):2207–14. doi: 10.1176/appi.ajp.161.12.2207. [DOI] [PubMed] [Google Scholar]
- 106.Frye MA, Altshuler LL, McElroy SL, Suppes T, Keck PE, Denicoff K, Nolen WA, Kupka R, Leverich GS, Pollio C, Grunze H, Walden J, Post RM. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry. 2003;160(5):883–9. doi: 10.1176/appi.ajp.160.5.883. [DOI] [PubMed] [Google Scholar]
- 107.Conway KP, Swendsen JD, Merikangas KR. Alcohol expectancies, alcohol consumption, and problem drinking: the moderating role of family history. Addict Behav. 2003;28(5):823–36. doi: 10.1016/s0306-4603(02)00265-4. [DOI] [PubMed] [Google Scholar]
- 108.Warner LA, White HR, Johnson V. Alcohol initiation experiences and family history of alcoholism as predictors of problem-drinking trajectories. J Stud Alcohol. 2007;68(1):56–65. doi: 10.15288/jsad.2007.68.56. [DOI] [PubMed] [Google Scholar]
- 109.Ary DV, Tildesley E, Hops H, Andrews J. The influence of parent, sibling, and peer modeling and attitudes on adolescent use of alcohol. Int J Addict. 1993;28(9):853–80. doi: 10.3109/10826089309039661. [DOI] [PubMed] [Google Scholar]