Abstract
Background
Mothers of infants hospitalized in the neonatal intensive care unit (NICU) are at risk for clinically significant levels of depression and anxiety symptoms; however, the maternal/infant characteristics that predict risk have been difficult to determine. Previous studies have conceptualized depression and anxiety symptoms separately, ignoring their comorbidity. Moreover, risk factors for these symptoms have not been assessed together in one study sample.
Objectives
The primary aim of this study was to determine whether a diagnostic classification approach or a common-factor model better explained the pattern of symptoms reported by NICU mothers, including depression, generalized anxiety, panic, and trauma. A secondary aim was to assess risk factors of aversive emotional states in NICU mothers based on the supported conceptual model.
Method
In this cross-sectional study, a nonprobability convenience sample of 200 NICU mothers completed questionnaires assessing maternal demographic and infant health characteristics, as well as maternal depression and anxiety symptoms. Structural equation modeling was used to test a diagnostic classification model, and a common-factor model of aversive emotional states and the risk factors of aversive emotional states in mothers in the NICU.
Results
Maximum likelihood estimates indicated that examining symptoms of depression and anxiety disorders as separate diagnostic classifications did not fit the data well, whereas examining the common factor of negative emotionality rendered an adequate fit to the data, and identified a history of depression, infant illness, and infant prematurity as significant risk factors.
Discussion
This study supports a multidimensional view of depression, and should guide both clinical practice and future research with NICU mothers.
Keywords: anxiety, depression, hospitalized newborns, mother, neonatal intensive care unit
Each year in the U.S., approximately 480,000 infants are born prematurely, representing 12% of live births (Hamilton, Martin, & Ventura, 2011). Mothers of newborn infants who are hospitalized in the neonatal intensive care unit (NICU) exhibit high rates of aversive emotional states, including clinically significant symptoms of depression and anxiety disorders (Jubinville, Newburn-Cook, Hegadoren, & Lacaze-Masmonteil, 2012). These symptoms have been shown to affect both the mother’s quality of life and her infant’s development (O’Connor, Heron, Golding, Beveridge, & Glover, 2002; O’Hara & McCabe, 2013). The prevalence of poor psychological well-being among NICU mothers highlights a critical role for NICU nurses: “neonatal care providers have a unique relationship with mothers and a golden opportunity to identify symptoms and provide appropriate referrals and support” (C. T. Beck, 2003, p. 37).
Traditionally, studies of emotional well-being of NICU mothers examined symptoms of depression and anxiety disorders independently from one another, treating the disorders as though each is accompanied by a distinct set of symptoms. For the purposes of the present study, this approach to examining aversive emotional states will be referred to as a diagnostic classification approach because depression and anxiety disorder symptoms were classified as separate. Reliance on this diagnostic classification conceptual approach is, however, problematic because a large body of research instead supports a common-factor model of aversive emotional states (Mineka, Watson, & Clark, 1998). Here, symptoms of depression, generalized anxiety, panic, and trauma are not considered completely distinct constructs, but rather are viewed as manifestations of a person’s general tendency to experience aversive emotions. A clear understanding of the conceptual nature of aversive emotional states in NICU mothers is critical for developing screening protocols aimed to identify women in need of emotional support or intervention. The present study utilized structural equation modeling to assess the fit of epidemiological data to these two conceptual models.
Background
Prevalence
Depression
The stress of having a newborn hospitalized in the NICU raises a mother’s risk for significant depressive symptoms. While clinically significant depressive symptoms are common in the general population of mothers during their first three months postpartum a meta-analytic review found a 19% prevalence rate (Gavin et al., 2005); between 28% and 67% of NICU mothers reported elevated levels of depressive symptoms (Davis, Edwards, Mohay, & Wollin, 2003; Lefkowitz, Baxt, & Evans, 2010; Miles, Holditch-Davis, Schwartz, & Scher, 2007; Pinelli et al., 2008; Singer et al., 1999). A longitudinal study suggests that these clinically significant levels of depressive symptoms persist: 63% of NICU mothers had elevated depression symptoms scores early on, when the infant was hospitalized; and, at the two-month, post-birth assessment, 30% still reported elevated symptoms (Miles et al., 2007). Further, these depressive symptoms are severe. Based on limited data, approximately 33% of NICU mothers reported suicidal thoughts (Lefkowitz et al., 2010), a rate significantly higher than the 14% reported by postpartum women with nonhospitalized newborns (Lindahl, Pearson, & Colpe, 2005).
Anxiety
Compared to the substantial number studies concerning postpartum depression, significantly fewer studies have assessed postpartum anxiety disorders in community samples of postpartum women (Ross, McLean, & Psych, 2006). Nevertheless, with regard to the relative prevalence of anxiety disorders in NICU mothers, the results of a three-year longitudinal study that directly compared prevalence of generalized anxiety in three groups of mothers are particularly informative (Singer et al., 1999). At infant gestational age of one month, the prevalence of clinically significant levels of generalized anxiety symptoms was markedly higher in mothers of high- and low-risk preterm infants than mothers of term infants: 26%, 23%, 7%, respectively (Singer et al., 1999). Among studies of NICU mothers only, prevalence estimates of clinically significant anxiety symptoms of generalized anxiety range from 18% to 43% (Carter, Mulder, Bartram, & Darlow, 2005; Rogers, Kidokoro, Wallendorf, & Inder, 2013).
The prevalence of other anxiety disorders (e.g., panic, obsessive-compulsive, and post-traumatic stress) has not been widely assessed in community samples of postpartum women (Ross & McLean, 2006). Of the few studies that have assessed the prevalence of these specific anxiety disorders in NICU mothers, two included a control group of mothers of term infants, which allowed a direct comparison of prevalence rates in the two groups. They found NICU mothers had significantly more symptoms of obsessive-compulsive disorder (Singer et al., 1999) and acute post-traumatic stress disorder (PTSD; Vanderbilt, Bushley, Young, & Frank, 2009). In a study limited to NICU mothers, 28% met diagnostic criteria for acute stress disorder one week after their infant was admitted (Jubinville et al., 2012). Similarly, one month after infant NICU admission, PTSD was diagnosed in 15% of NICU mothers (Lefkowitz, et al., 2010). No studies assessing the prevalence of panic disorder in NICU mothers were located.
Risk
Risk factors for postpartum depression have been extensively assessed in general community samples of postpartum women. Three meta-analyses consistently identified moderate to strong associations between postpartum depressive symptoms and history of depression, prenatal depression or anxiety, low self-esteem, stressful life events, and poor social support (O’Hara & McCabe, 2013). In contrast, relatively fewer studies have assessed risk factors for depression in NICU mothers (Bergström, Wallin, Thomson, & Flacking, 2012; Carter et al., 2005; Mew, Holditch-Davis, Belyea, Miles, & Fishel, 2003; Rogers et al., 2013), and/or anxiety (Carter et al., 2005; Jubinville et al., 2012; Lefkowitz et al., 2010; Rogers et al., 2013). The results of these studies varied widely and are, therefore, not conclusive.
Limitations of Current Research
In retrospect, the limitations in assessing risk factors for depression or anxiety disorder symptoms in NICU mothers likely arose from key methodological flaws. First, many studies that examined risk factors had small sample sizes (e.g., < 100) limiting statistical power to detect stable or generalizable significant associations (Jubinville et al., 2012; Lefkowitz et al., 2010; Rogers et al., 2013; Vanderbilt et al., 2009; Zelkowitz & Milet, 2001). Second, although a wide range of maternal demographic and infant health status characteristics were assessed as risk factors across these studies, the relative significance of these potential risk factors have not been assessed in a single, large sample. Finally, consistent with the current diagnostic classification system that characterizes depression, generalized anxiety, panic, and trauma as separate disorders (American Psychiatric Association, 2013), these epidemiological studies of NICU mothers reflect a diagnostic classification conceptual framework (see Figure 1a) in which depression and anxiety disorder symptoms were assessed independently from one another—without accounting for possible overlap. Nevertheless, a diagnostic classification approach to examining aversive emotional states is problematic in part because these disorders share key overlapping symptoms, and are heterogeneous, highly comorbid disorders (den Hollander-Gijsman et al., 2012).
Figure 1.
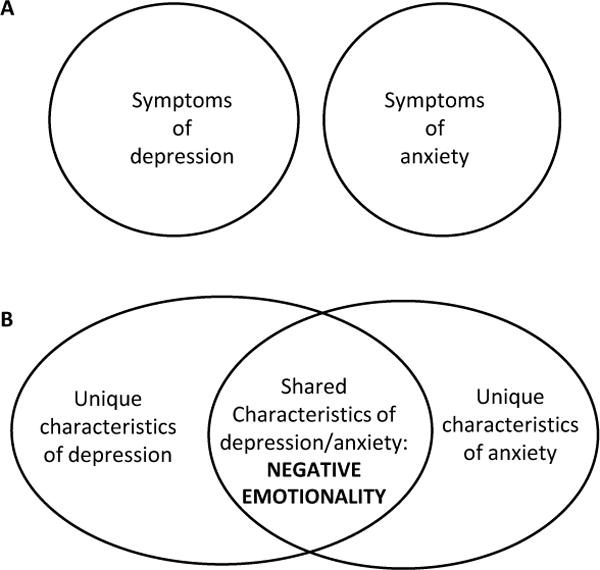
Conceptualization of relationships between depression and anxiety. The Venn diagram in panel A represents the traditional conceptualization of depression and anxiety as distinct disorders. Panel B, the Venn diagram represents current conceptualization of depression and anxiety. Depression and anxiety are characterized by variance that is shared between the disorders and variance that is unique to each disorder.
Although a diagnostic classification approach has been the predominant approach in quantitative epidemiological studies of aversive emotional states in NICU mothers, an early phenomenological study of women’s experiences with postpartum depression recognized that at the heart of this disorder lie symptoms of depression and anxiety (C. T. Beck, 1992). In an aptly titled publication, The Many Faces of Postpartum Depression, the author notes: “not every mother suffering from postpartum depression will present with the same constellation of symptoms” (C. T. Beck & Indman, 2005, p. 573). This multifaceted conceptualization of postpartum depression aligns with the common-factor conceptual framework (see Figure 1b).
Negative Emotionality: A Common-Factor Conceptual Framework
Negative emotionality is defined as the disposition to experience aversive emotions (Watson & Clark, 1984; Watson & Tellegen, 1985). Research has demonstrated that negative emotionality is a relatively stable trait, and common characteristics of people who exhibit high levels of negative emotionality include feeling anxious and stressed, being prone to sadness and guilt, and having experiences of anger and frustration (Watson & Clark, 1984). These common characteristics of negative emotionality are similar to symptoms of both depression and anxiety disorders, and previous research has identified significant correlations of moderate magnitude between negative emotionality and symptoms of these disorders (Gamez, Watson, & Doebbeling, 2007; Watson, Gamez, & Simms, 2005). As such, negative emotionality has been proposed as a construct that explains the comorbidity among depression and anxiety disorders (Mineka et al., 1998), and has provided a framework with which to unify them.
Both genetic and phenotypic data demonstrate that negative emotionality is a common factor that underlies both depression and anxiety disorders (Kendler, Neale, Kessler, Heath, & Eaves, 1993; Mineka et al., 1998). In other words, symptoms of depression and anxiety disorders can be conceptualized as indicators of negative emotionality. What this means is that individuals with high levels of negative emotionality are likely to experience aversive emotional states that may manifest as symptoms of depression or anxiety disorders; and these symptoms may even rise to the level of a syndromal manifestation of these disorders. This strong empirical support for this common-factor model suggests that inconsistencies noted in the study of aversive emotional states in NICU mothers may be a result of improper conceptualization of symptoms of depression and anxiety disorders. Whereas previous research has examined risk factors of specific aversive emotional states in NICU mothers, it may be more informative to examine risk factors of negative emotionality in these mothers of hospitalized newborns.
Study Aims
To address the shortcomings of prior research in identifying reliable risk factors of aversive emotional states, a single large sample of NICU mothers was assessed for a range of maternal demographic and infant health status risk factors and symptoms of depressive and anxiety disorders, including generalized anxiety, panic, and trauma. Utilizing structural equation modeling, the primary study objective was to examine risk factors of aversive emotional states in NICU mothers from the perspective of two conceptual frameworks—to determine which conceptual model best fit the data. A secondary goal was to determine significant risk factors of aversive emotional states in NICU mothers, based on the supported conceptual model.
Methods
Design
The data for this cross-sectional study were collected during the screening phase of an open-trial evaluation of a nurse-delivered depression counseling treatment (Segre, Chuffo-Siewert, Brock, & O’Hara, 2013). To identify women with elevated depressive symptoms for the treatment trial phase, a nonprobability convenience sample of NICU mothers was enrolled into the screening phase.
Setting and Sample
The study setting was a Level IV NICU of a Midwestern academic medical center with 70 private beds and approximately 800 annual admissions. Recruitment and enrollment into the screening phase continued until the sample size of the feasibility open trial was sufficient. Enrollment of 23 women into the treatment trial required screening NICU mothers from December 2010 to May 2012. During this time 571 NICU mothers were eligible (i.e., infant hospitalized on the NICU, 18 years of age, and English speaking) to receive a brochure describing the screening phase of the study. Of these women, a convenience sample of 200 mothers of NICU infants (35%) enrolled and completed the screening assessment. Based on the factor structure of the proposed models and the hypothesized factor loadings (i.e., > 0.6), a sample size of 200 was deemed adequate for the proposed analyses (Gagne & Hancock, 2006).
Measures
Maternal and infant characteristics
Demographic information was collected using a 17-item questionnaire that assessed maternal characteristics (i.e., maternal age, ethnicity, race, marital status, education, employment status, income, self-reported of history of depressed mood, and whether they were currently receiving treatment for an emotional health issue). Infant health characteristics included infant birth weight and gestational age, as well as a dichotomous variable (based on maternal self-report) of infant health complications (e.g., persistent pulmonary hypertension, infection, multiple congenital anomalies, or other significant infant illnesses).
Negative emotionality
To create a latent negative emotionality factor, symptoms that reflect empirical models of aversive emotional states (Slade & Watson, 2006) that are likely to be experienced by mothers on the NICU were assessed; these include symptoms of depression, as well as anxiety disorders, including general anxiety, panic, and trauma.
The Edinburgh Postnatal Depression Scale (EPDS), a 10-item, self-report instrument for assessing depressive symptoms in postpartum women (Cox, Holden, & Sagovsky, 1987) was used in this study. Items are scored on a scale from 0 to 3 and reflect mood in the last seven days, including symptoms of sad mood, lack of interest, guilt, anxiety, and suicidal ideation. Using a cutoff score of 12 or above, the EPDS has been validated against DSM-III-R criteria (Wickberg & Hwang, 1996); reporting high sensitivity (96%) and moderate specificity (48%). Thus, clinically significant depressive symptoms were set, in our study, as an EPDS cutoff score of ≥ 12. In the current study, reliability of the EPDS scores was α = 0.89.
The Beck Anxiety Inventory (BAI) was used to assess levels of general anxiety symptoms among NICU mothers. The BAI contains 21 affective and somatic symptoms of anxiety that are rated on a 4-point scale of experienced severity (A. T. Beck, Epstein, Brown, & Steer, 1988). The recommended BAI severity scores fall into four categories: Scores between 0 and 7 represent minimal, nonclinically significant symptoms; scores between 8 and 15 represent mild anxiety symptoms; scores between 16 and 25 represent moderate symptoms; and scores between 26 and 63 represent severe symptoms (A. T. Beck, et al., 1988). Psychometrically, the results of the initial validation study demonstrated high reliability using coefficient alpha (α = 0.92) and discriminant validity, with the average BAI score significantly higher in groups of people diagnosed with an anxiety disorder than in groups of depressed individuals (Beck et al., 1988). In this study, the reliability estimate for BAI scores was α = 0.91.
Panic and trauma symptoms
To assess panic and trauma (anxiety symptoms likely to affect NICU mothers), the Panic and Traumatic Intrusions subscales of the Inventory of Depression and Anxiety Symptoms (IDAS; Watson et al., 2007) was used. The IDAS, a 64-item, 5-point Likert-scale self-report instrument, consists of 10-symptom subscales, including: insomnia, appetite loss, appetite gain, lassitude, suicidality, ill temper, well-being, panic, social anxiety, and traumatic intrusions. The Panic subscale includes eight items (e.g., “my heart was racing or pounding; I was trembling or shaking”); and the Traumatic Intrusions subscale includes four items (e.g., “I got upset thinking about something bad that happened; I had bad memories of something scary that happened”). Individuals are asked to rate symptom severity—over the past two weeks—on a 5-point Likert-scale from “not at all” to “extremely.” An initial validation study of the IDAS demonstrated strong convergent and discriminant validity in these two subscales (Watson et al., 2007). A second study confirmed the validity and extended the findings to include evidence of strong criterion validity in relation to diagnosable panic disorder (correlation with Panic subscale = .47) and PTSD (correlation with traumatic intrusions subscale = 0.43) (Watson et al., 2008). Reliability of scores on the panic subscale in the current sample using coefficient alpha was α = 0.83; for the traumatic intrusions subscale scores, α = 0.84.
Procedures
Participant recruitment/enrollment and assessment
All procedures for this study were approved by the university’s institutional review board. All mothers of NICU infants who were English speaking, and 18 years of age or older, received a recruitment brochure describing the study. Interested women returned contact information on a tear-off card and gave it to the unit secretary. Research team staff members, who were also nursing students working on the NICU, followed up with these interested women by describing the study, completing the informed consent enrollment process, distributing and collecting the study-assessment packets, and providing gift card compensation.
Statistical analyses
Descriptive statistics, prevalence estimates, and correlations were analyzed in SPSS version 19.0. Descriptive statistics were used to examine the means, standard deviations, and frequencies of maternal demographic and psychological characteristics, as well as infant health status variables. Prevalence estimates were calculated using cutoff points/severity ranges on the EPDS and BAI (see Measures) to determine the percentage of NICU mothers reporting clinically significant levels depression and general anxiety symptoms, and their comorbidity. Correlations were examined to identify significant associations among study variables. Study variables that correlated at greater than .70 were standardized and aggregated before being submitted to structural equation modeling (SEM).
Two models of aversive emotional states were specified, tested, and compared using SEM. Specification of the traditional dimensional classification approach is presented in Figure 2, in which individual measures of depression and anxiety disorders are individually regressed onto proposed NICU risk factors. Specification of the common-factor approach is presented in Figure 3, in which a measurement model is used to create a latent variable of maternal negative emotionality, which is then regressed onto proposed NICU risk factors. The latent variable of maternal negative emotionality represents the shared variance among symptoms of depression and anxiety disorders (i.e., modeling comorbidity).
Figure 2.
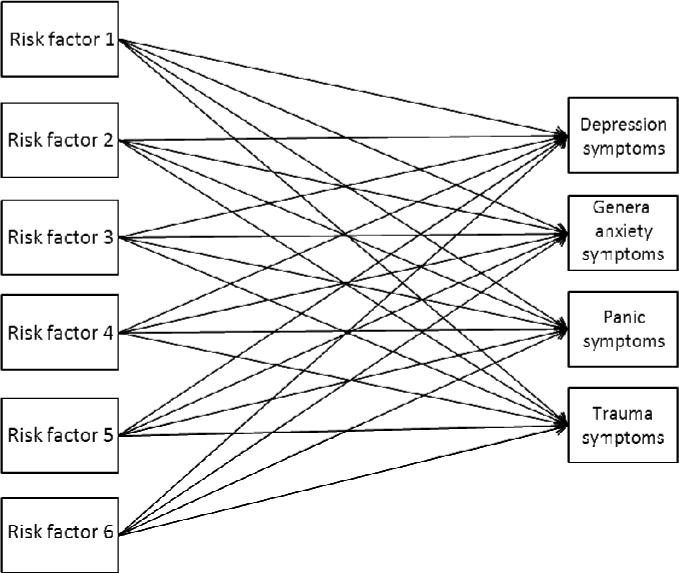
This model depicts a diagnostic classification approach to examining risk factors of symptoms of depression and anxiety in NICU mothers. Risk factors of depression, general anxiety, panic, and trauma are examined independent from one another.
Figure 3.
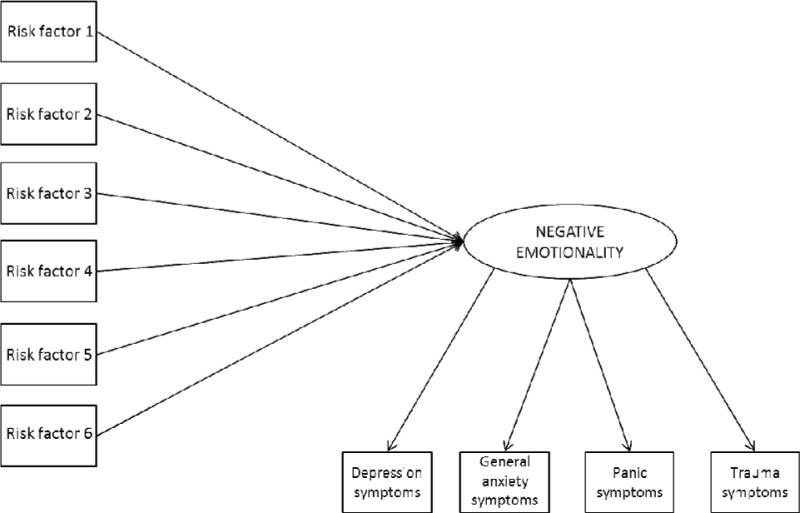
This model depicts a common-factor approach to examining risk factors of symptoms of depression and anxiety in NICU mothers. Negative emotionality is represented as the shared variance among symptoms of depression, general anxiety, panic, and trauma.
Next, the two conceptual models were tested. Models were estimated in Mplus 6 (Muthén & Muthén, 1998–2010), using maximum likelihood estimation (ML). Cases with missing data on exogenous variables (i.e., variables that are not influenced by any other variable in the model), such as infant illness and history of perinatal depressed mood, were excluded from analyses; cases with data missing on endogenous variables (i.e., variables that are influenced by other variables in the model), such as EPDS scores, were adjusted for missing data, using full information maximum-likelihood estimation (FIML). Global model fit provides an estimate of how well a set of observed data fit a proposed model. These analyses examined global fit in a variety of ways, including the chi-square to degrees of freedom ratio: χ2/df (Wheaton, Muthén, Alwin, & Summers, 1977); the standardized root mean squared residual (SRMR; Hu & Bentler, 1999); the root mean squared error of approximation (RMSEA; Browne & Cudeck, 1993); and the comparative fit index (CFI; Bentler, 1990). Adequate model-data fit was defined by χ2/df values of below 2.0, SRMR and RMSEA values less than 0.08, and CFI values greater than 0.90.
Finally, the two conceptual models were compared. The Bayesian information criterion (BIC) was used to assess relative fit, or a comparison of the two competing models. In the event that the two models tested in these analyses both demonstrated acceptable fit to the data, and a model selection approach must be used, the BIC provides a measure of overall model fit—with smaller values reflecting better relative fit (Raftery, 1995).
After the two conceptual models were specified, tested, and compared, and the best-fitting model was identified, specific risk factors of aversive emotional states in NICU mothers were examined. Standardized parameter estimates of the supported model were examined for statistical significance, magnitude, and direction of effect. All risk factors were examined within the same model, so results reflected the association between a risk factor and aversive emotional states while adjusting for other risk factors in the model.
Results
As indicated in Table 1, this sample contained predominately White, non-Hispanic women, who reported an average age of 28 years (range 18 to 45) and an average education level of 15 years (range 8 to 20). Over half of the participants were married (61.8%; N = 123) and employed (66.3%; N = 132), with almost half (45.1%; N = 83) reporting annual incomes higher than $50,000. Sixteen percent (N = 31) of mothers indicated they were currently receiving psychological treatment (i.e., counseling and/or medication).
Table 1.
Descriptive of Maternal and Infant Characteristics
| Variable | n | M | Mdn | SD |
|---|---|---|---|---|
| Age (years) | 199 | 28.1 | 27.0 | 5.7 |
| Education (years) | 199 | 14.6 | 14.0 | 2.5 |
| Infant birth weight (grams) | 199 | 2154.0 | 2041.0 | 1043.0 |
| Gestational age (weeks) | 193 | 34.0 | 34.0 | 5.0 |
| Time of measurement (days) | 193 | 13.0 | 8.0 | 24.0 |
|
|
||||
| Frequency | % | |||
|
|
||||
| Married | 199 | 123 | 61.8 | |
| Race | 198 | |||
| Caucasian | 178 | 89.9 | ||
| African American | 12 | 6.1 | ||
| Hispanic | 193 | 11 | 5.7 | |
| Employed | 199 | 132 | 66.3 | |
| Receiving psychological treatment | 199 | 31 | 15.6 | |
| History of perinatal depression | 198 | 81 | 40.9 | |
| Any infant illness or complication | 200 | 112 | 56.0 | |
| Income | 184 | — | — | |
| < 5,000 | 14 | 7.6 | ||
| 5–10,000 | 14 | 7.6 | ||
| 11–20,000 | 14 | 7.6 | ||
| 21–30,000 | 23 | 12.5 | ||
| 31–40,000 | 15 | 8.2 | ||
| 41–50,000 | 21 | 11.4 | ||
| > 50,000 | 83 | 45.1 | ||
Most study participants completed study measures within the first week of their infants’ hospitalization: median = 8 days, range 0 to 300 days. Infant birth weights ranged from 397 to 4,706 grams, and gestational age ranged from 23 to 41 weeks. Nearly 60% (N = 112) of mothers reported that their infants experienced additional post-delivery complications, such as persistent pulmonary hypertension, infections, or multiple congenital anomalies. Approximately 41% (N = 81) of the women in the sample endorsed a previous history of perinatal, depressed mood.
The demographics of the participants reflected the population of mothers seen in the same NICU unit during the study timeframe. De-identified, demographic data for all NICU mothers were obtained from the hospital electronic database, which also contained demographics for the 200 current study participants. Study participants did not differ from the general population of NICU mothers on age (t(198) = .70, p = .49), race (Fisher’s exact test: p = .06), or parity (t(199) = −0.63, p = .53). Participants did, however, have infants with a lower gestational age than the general population of NICU mothers (34 weeks vs. 35 weeks; t(192) = −4.74, p < .0001).
It was found that 25.5 % of NICU mothers (N = 50) reported clinically significant symptoms of depression (i.e., EPDS score ≥ 12). Anxiety symptoms, as measured by self-report on the BAI, were minimal in 42.1% of participants (N = 82), mild in 30.3% (N = 59), moderate in 17.4% (N = 34), and severe in 10.3% (N = 20). Comorbidity of clinically significant depression and anxiety symptoms was also observed. Of the 53 women who reported moderate to severe levels of anxiety symptoms, 51% also reported clinically significant depression symptoms. Similarly, of the 49 women reporting clinically significant depression symptoms, 55% reported moderate to severe levels of anxiety symptoms. Overall, 14% (N = 27) of the sample endorsed both clinically significant symptoms of depression and moderate to severe symptoms of anxiety.
Prediction of Risk: Comparison of Two Conceptual Models
Correlations among the study variables are presented in Table 2. The BAI and IDAS-panic measures correlated greater than 0.70 (r = 0.78; p < .001), which was not unexpected because both measures extensively assess physiological symptoms of anxiety. Thus, the BAI and IDAS-panic measures were aggregated into a single composite variable labeled anxious arousal, to reflect the emphasis on the physiological arousal represented in these two measures. Similarly, gestational age and infant birth weight correlated greater than .70 (r = .88) and were aggregated into a single composite variable labeled prematurity.
Table 2.
Correlations among Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. EPDS | — | ||||||||||||||||
| 2. BAI | .56 | — | |||||||||||||||
| 3. IDAS-Panic | .42 | .78 | — | ||||||||||||||
| 4. IDAS-Trauma | .51 | .66 | .63 | — | |||||||||||||
| 5. AnxArousalb | .52 | .94 | .94 | .69 | — | ||||||||||||
| 6. Marrieda | −.11 | −.17 | −.10 | −.15 | −.14 | — | |||||||||||
| 7. Maternal age | .00 | −.13 | −.07 | −.06 | −.11 | .29 | — | ||||||||||
| 8. Caucasiana | .06 | .00 | −.03 | −.07 | −.01 | .24 | .03 | — | |||||||||
| 9. Education | −.05 | −.04 | −.01 | −.07 | −.02 | .48 | .40 | .08 | — | ||||||||
| 1. Income | −.06 | −.14 | −.01 | −.06 | −.08 | .54 | .43 | .20 | .59 | — | |||||||
| 11. Employeda | .01 | −.02 | −.07 | −.11 | −.04 | .22 | .21 | .21 | .32 | .33 | — | ||||||
| 12. Time on NICU | .10 | −.01 | .01 | .08 | .00 | −.03 | −.08 | .03 | −.06 | .08 | .02 | — | |||||
| 13. HxDEPa | .49 | .43 | .28 | −.36 | .38 | −.20 | −.02 | −.10 | −.11 | −.16 | .04 | −.03 | — | ||||
| 14. Infant illnessa | .18 | .18 | .18 | .13 | .20 | −.01 | .14 | .08 | .06 | .05 | −.01 | .00 | .07 | — | |||
| 15. Infant BW | −.09 | −.04 | .03 | −.01 | .00 | .11 | .09 | .20 | .04 | .09 | −.04 | −.23 | −.02 | .33 | — | ||
| 16. GA | −.05 | −.06 | .00 | −.07 | −.02 | .07 | .06 | .16 | −.02 | .04 | −.05 | −.28 | −.01 | .31 | .88 | — | |
| 17. Prematurityb | −.07 | −.05 | .02 | −.05 | −.01 | .08 | .09 | .17 | .00 | .05 | −.05 | −.27 | −.01 | .34 | .97 | .97 | — |
| M | 8.02 | 11.63 | 11.04 | 5.79 | 0.00 | n/a | 28.14 | n/a | 14.60 | 6.54 | n/a | 13.36 | n/a | n/a | 2154.3 | 33.58 | 0.01 |
| SD | 5.38 | 9.49 | 3.93 | 2.91 | 1.89 | n/a | 5.66 | n/a | 2.50 | 3.60 | n/a | 24.30 | n/a | n/a | 1042.6 | 4.70 | 1.94 |
Note. N = 179–200. EPDS = Edinburgh Postnatal Depression Scale; BAI = Beck Anxiety Inventory; IDAS = Inventory of Depression and Anxiety Symptoms; AnxArousal = Anxious arousal; NICU = Newborn intensive care unit; HxDEP = History of Depression; BW = Birth weight in grams; GA = Gestational age. Correlations significant at p < .05 are shown in bold and at p < .01 are bold and underlined. Descriptive statistics for binary variables are available in Table 1.
Binary variable.
z-score aggregate variable.
Maximum likelihood estimates revealed that the traditional diagnostic classification approach of examining separate measures of aversive emotional states (see Figure 4) was a poor fit to the data (see Table 3). Because this model was a poor fit to the data, parameter estimates were not examined and the model was respecified for further testing. The respecified model was a more parsimonious model in which each risk factor was restricted to have the same magnitude of effect on all three measures of aversive emotional states. In other words, the risk factor of marital status was restricted to have the same effect on symptoms of depression, anxious arousal, and trauma. This restricted diagnostic classification model was also a poor fit to the data (see Table 3); therefore, parameter estimates were not examined.
Figure 4.
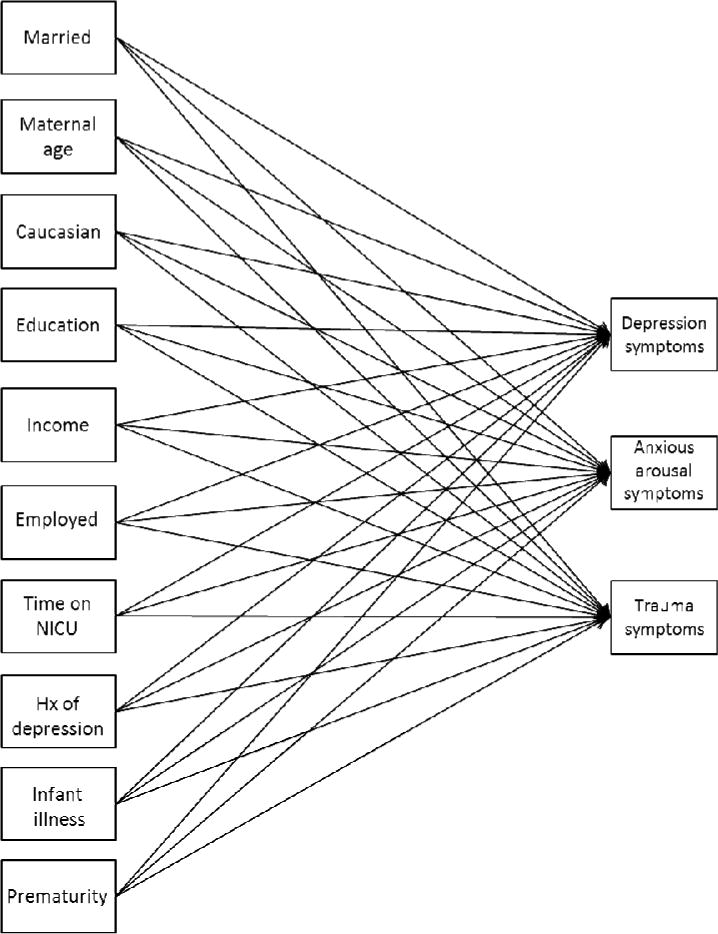
Specification of the final tested diagnostic classification model.
Table 3.
Fit Indices for Tested Models
| Model | q | χ2 | df | χ2/df | SRMR | RMSEA | CFI | BIC |
|---|---|---|---|---|---|---|---|---|
| Diagnostic classification model | 33 | 112.72 | 3 | 37.57 | 0.06 | 0.47 | 0.52 | 2589.52 |
| Diagnostic classification model- restricted | 13 | 154.09 | 23 | 6.70 | 0.09 | 0.18 | 0.43 | 2528.41 |
| Common-factor model | 17 | 32.16 | 20 | 1.61 | 0.03 | 0.06 | 0.95 | 2421.86 |
Note. q = Number of free parameters estimated in the model; df = degrees of freedom; SRMR = Standardized root mean squared residual; RMSEA = Root mean squared error of approximation; CFI = Comparative fit index; BIC = Bayesian information criterion.
In contrast to the diagnostic classification approach, the common-factor approach of examining risk factors of negative emotionality showed an adequate fit to the data (see Table 3). Examination of the parameter estimates (see Figure 5) showed that the observed symptoms of depression and anxiety disorders represented acceptable and significant indicators of negative emotionality in NICU mothers (all estimates ≥ 0.68). The BIC statistic for each tested model is presented in Table 3; however, because the traditional diagnostic classification model of examining separate measures of aversive emotional states was not a good fit to the data, model selection based on the BIC statistic was not warranted.
Figure 5.
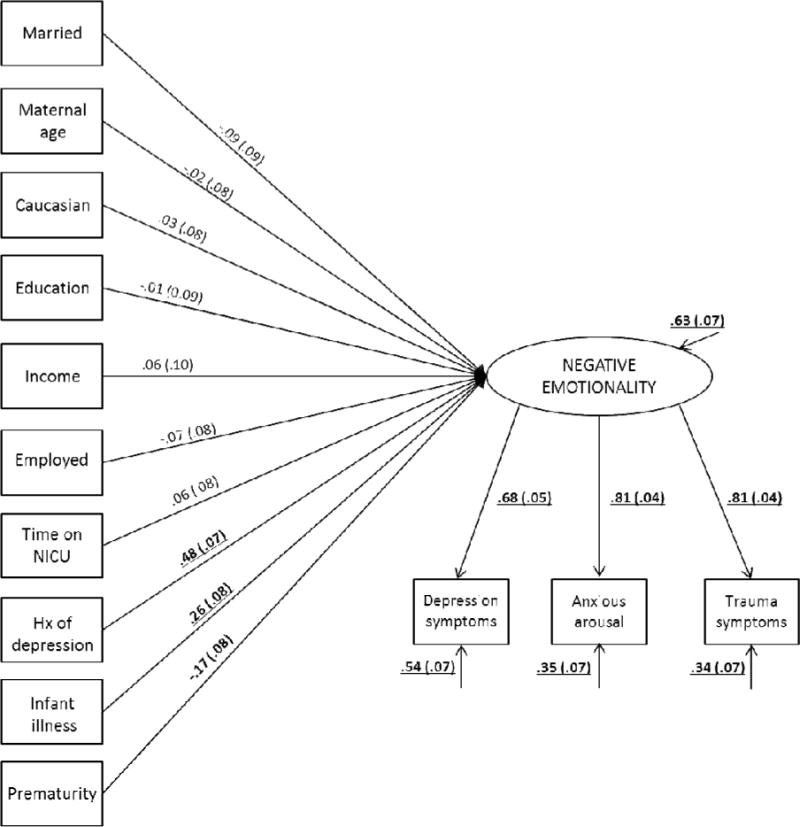
Standardized parameter estimates for the common-factor model. Standard errors are reported in parentheses. Arrows pointing from negative emotionality to aversive emotional states represent standardized factor loadings. Unlabeled arrows pointing to each endogenous variable represent residual (unaccounted for) variance in each of those variables. Significant estimates are indicated in bold for p < .05, in bold and underlined for p < .001.
Risk Factors for Negative Emotionality in NICU Mothers
Parameter estimates of the supported model (see Figure 5) showed that none of the maternal demographic characteristics were significantly associated with negative emotionality in NICU mothers (all p > .05). In contrast, infant illness, prematurity (an aggregate of infant birth weight and age), and maternal self-reported history of perinatal depressed mood were all significantly associated with negative emotionality in NICU mothers. In other words, the presence of infant illness, greater prematurity, and history of perinatal depressed mood were significantly associated with higher levels of negative emotionality. Overall, the specified model in Figure 5 accounted for 37% of the variance in negative emotionality.
Discussion
Consistent with prior prevalence estimates (Miles et al., 2007; Rogers et al., 2013), approximately one quarter of the NICU mothers in the sample reported elevated depressive symptoms, and moderate to severe anxiety symptoms. Past epidemiological studies of NICU mothers typically assessed risk factors of depression and anxiety disorders separately, reflecting a diagnostic classification model and rendering inconsistent results. Departing from this conceptual zeitgeist, the current study uniquely utilized structural equation modeling to compare the fit of epidemiological data—both to two different models of examining risk factors of aversive emotional states in the NICU. One model represented the traditional diagnostic classification approach of examining risk factors of separate measures of depression and anxiety symptoms. The second model examined risk factors of the overlap among symptoms of depression and anxiety disorders, labeled here as negative emotionality, or the underlying tendency to experience aversive emotional states. Consistent with Beck’s conceptualization that depression and anxiety symptoms can both be central to the experience of postpartum depression (Beck, 1992), the results indicate that the common-factor conceptual model was an adequate fit to the observed data, whereas the diagnostic classification conceptual model was not supported in this dataset. The model supported in this study not only agrees with empirically supported models of depression and anxiety in nonpostpartum samples (Mineka et al., 1998), it also provides a robust assessment of negative emotionality in NICU mothers, explaining 37% of the variance of this construct.
Utilizing a common-factor conceptual model, three significant risk factors of negative emotionality in NICU mothers were identified: a maternal history of depression; greater infant prematurity; and infant health complications beyond prematurity. The finding that a history of maternal depression is a key risk factor, and is consistent with considerable evidence from community samples of postpartum women that show their situational vulnerability to depression can be predicted by a history of depression (O’Hara & McCabe, 2013). The other two risk factors identified as significant predictors of negative emotionality in this study—infant prematurity and health complications—are unique to NICU mothers and cannot be compared with the results of studies of general postpartum samples. Nonetheless, it is expected that infants that are more premature, or have an additional health complications, will have mothers who feel depressed and/or anxious.
Although meta-analyses of studies of community samples of postpartum women also identify income as a risk factor with modest association with depressive symptoms (O’Hara & McCabe, 2013), it is interesting to note that, in this study, income was not significantly associated with negative emotionality. This negative finding aligns with results of prior studies of NICU mothers that assessed the association of income and symptoms of depression (Brooten et al., 1988; Rogers et al., 2013) and anxiety (Vanderbilt et al., 2009). This lack of association is compelling because the sample included women with wide range of annual incomes, and with almost one quarter (22.8%) reporting annual incomes below the federal poverty line (Iowa Department of Human Services, 2012). Thus, one cannot assume that just because a woman does not have significant economic resources that she will be emotionally vulnerable. Conversely, and equally important, is that one cannot assume that women with economic resources are protected.
Several methodological limitations of the current study are noteworthy. First, the study sample was somewhat demographically homogeneous: ethnic-minority women and those with less educational attainment were not adequately represented. Second, mothers with previous history of depression may be overrepresented in this sample. Specifically, almost half (41%) of the 200 study participants reported a history of depression, suggesting a potential overrepresentation of emotionally vulnerable women. This limitation is somewhat offset by the demographic comparability of the study’s participants and all mothers in the NICU, as well as the possibility that emotional vulnerability may be a risk factor for prematurity. Third, maternal social support, also a significant predictor of elevated depressive symptoms in previous research of NICU mothers (Singer, Davillier, Bruening, Hawkins, & Yamashita, 1996), was not assessed in this study. Fourth, the assessment of current psychological treatment did not require participants to specify which symptoms (anxiety or depression) prompted treatment. Finally, the assessment of infant illness relied on the mother’s self-report only and was analyzed as a dichotomous variable. While mothers’ perceptions of infant illness severity are likely a key component of negative emotionality; an objective rating of infant illness severity may also be important to capture. In light of these limitations, the next step should be to replicate this study in a setting with broad representation of ethnic-minority women that assesses not only the risk factors included in this study, but also assesses social support as well as a chart-based assessment of level of infant illness severity.
Notwithstanding methodological limitations, the significant risk factors identified in this study—history of perinatal depression, greater infant prematurity and infant health complications—are not only clinically intuitive, they explained 37% of the variance in negative emotionality in NICU mothers. In line with the principles of family-centered care (Gooding et al., 2011), NICU nurses are ideally situated to identify emotionally at-risk NICU mothers (Beck, 2003). The substantial association of negative emotionality to the three identified risk factors empirically bolsters the idea that they should be used early to identify NICU mothers with clinically significant symptoms. At a minimum level of screening, women with these risk factors should be further assessed. In line with the conclusion that “depression is not necessarily the first or most important symptom of mothers suffering from postpartum depression,” (C. T. Beck & Indman, 2005, p. 570), the results support a multidimensional conceptualization of aversive emotional states that is consistent with the common-factor model. Translated into clinical practice, this result suggests screening should assess symptoms of both depression and anxiety disorders.
For researchers, findings from this study highlight how an underlying tendency to experience aversive emotional states may manifest in the NICU. Not only may mothers display symptoms of depression and general anxiety, they may also demonstrate symptoms of other anxiety disorders. The focus was on symptoms of panic disorder and PTSD; however, research shows negative emotionality is associated with symptoms of other anxiety disorders, including social anxiety disorder and obsessive compulsive disorder (Gamez et al., 2007; Watson et al., 2005). Thus, future studies may benefit by expanding the conceptual model of negative emotionality to include a wider range of aversive emotional states experienced by mothers of infants on the NICU. It should further be noted that, although this study examined a common-factor model of aversive emotional states in NICU mothers, this conceptual framework can be incorporated into the study of perinatal mental health more generally. Indeed, models of negative emotionality have been used to study risk factors and consequences of aversive emotional states in nonperinatal populations (Fresco, Williams, & Nugent, 2006; Henson, Derlega, Pearson, Ferrer, & Holmes, 2013; Stewart, Rand, Hawkins, & Stines, 2011).
The findings identify risk factors of the shared component of depression and symptoms of anxiety disorders (i.e., negative emotionality). Future research should also identify risk factors of the unique components of these aversive emotional states. A large portion of the variance in depression symptoms is shared with many of the anxiety disorders (i.e., negative emotionality), but each of these aversive emotional states has unique components that must be considered (Mineka et al., 1998). For example, low positive affect (i.e., joy, enthusiasm, engagement) is a unique component of depression, that is, it does not appear to be associated with generalized anxiety, panic, or trauma (Watson et al., 2005).
Conclusion
Mothers of NICU-hospitalized infants are emotionally vulnerable. The identification and treatment of their emotional distress, in the form of depression and or anxiety symptoms, is a critical facet of holistic, NICU nursing care that benefits the mother, and enhances her ability to engage with the nursing team, and, ultimately, the infant.
Acknowledgments
The authors acknowledge the assistance of NICU nursing staff (Jennifer Nieman, MSN, NNP-BC & Jade Kalmes, MSN, NNP-BC), undergraduate research team members (Kathryn Schmalzer, BSN RN, Rachel Rauenbuehler, BSN RN, Erin Schrieber, BSN, RN; Daniel Lose, BSN, RN), Austin Williamson for comments on manuscript drafts, Diana Colgan, PhD, the College of Nursing editor, and importantly, the mothers who participated in this research.
Funding for this research was provided to Drs. Segre and Siewert by the Social Science Funding Program, Vice President for Research Office of the University of Iowa. During the period of the conduct of this research Lisa S. Segre, PhD was supported by a NIMH K-23 Award (Grant MH075964). All authors are employees of the University of Iowa. Jennifer McCabe was a paid research assistant for the development of this manuscript.
Footnotes
The authors have no conflicts of interest to report.
Contributor Information
Lisa S. Segre, Assistant Professor, College of Nursing, University of Iowa.
Jennifer E. McCabe, Doctoral Candidate, Clinical Psychology, Department of Psychology, University of Iowa.
Rebecca Chuffo-Siewert, Clinical Associate Professor, College of Nursing, University of Iowa and Neonatal Nurse Practitioner, University of Iowa Children’s Hospital.
Michael W. O’Hara, Professor, Department of Psychology, University of Iowa.
References
- American Psychiatric Association. Diagnostic and statisical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck CT. The lived experience of postpartum depression: A phenomenological study. Nursing Research. 1992;41:166–171. [PubMed] [Google Scholar]
- Beck CT. Recognizing and screening for postpartum depression in mothers of NICU infants. Advances in Neonatal Care. 2003;3:37–46. doi: 10.1053/adnc.2003.50013. [DOI] [PubMed] [Google Scholar]
- Beck CT, Indman P. The many faces of postpartum depression. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2005;34:569–576. doi: 10.1177/0884217505279995. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bergström EB, Wallin L, Thomson G, Flacking R. Postpartum depression in mothers of infants cared for in a Neonatal Intensive Care Unit—Incidence and associated factors. Journal of Neonatal Nursing. 2012;18:143–151. doi: 10.1016/j.jnn.2011.11.001. [DOI] [Google Scholar]
- Brooten D, Gennaro S, Brown LP, Butts P, Gibbons AL, Bakewell-Sachs S, Kumar SP. Anxiety, depression, and hostility in mothers of preterm infants. Nursing Research. 1988;37:213–216. [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, NJ: Sage; 1993. pp. 136–162. [Google Scholar]
- Carter JD, Mulder RT, Bartram AF, Darlow BA. Infants in a neonatal intensive care unit: Parental response. Archives of Disease in Childhood—Fetal & Neonatal Edition. 2005;90:F109–F113. doi: 10.1136/adc.2003.031641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Davis L, Edwards H, Mohay H, Wollin J. The impact of very premature birth on the psychological health of mothers. Early Human Development. 2003;73:61–70. doi: 10.1016/S0378-3782(03)00073-2. [DOI] [PubMed] [Google Scholar]
- den Hollander-Gijsman ME, Wardenaar KJ, de Beurs E, van der Wee NJA, Mooijaart A, van Buuren S, Zitman FG. Distinguishing symptom dimensions of depression and anxiety: An intergrative approach. Journal of Affective Disorders. 2012;136:693–701. doi: 10.1016/j.jad.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Williams NL, Nugent NR. Flexibility and negative affect: Examining the associations of explanatory flexibility and coping flexibility to each other and to depression and anxiety. Cognitive Therapy and Research. 2006;30:201–210. doi: 10.1007/S10608-006-9019-8. [DOI] [Google Scholar]
- Gagne P, Hancock GR. Measurement model quality, sample size, and solution propriety in confirmatory factor models. Multivariate Behavioral Research. 2006;41:65–83. doi: 10.1207/S15327906mbr4101_5. [DOI] [PubMed] [Google Scholar]
- Gamez W, Watson D, Doebbeling BN. Abnormal personality and the mood and anxiety disorders: Implications for structural models of anxiety and depression. Journal of Anxiety Disorders. 2007;21:526–539. doi: 10.1016/j.janxdis.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstetrics & Gynecology. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: Origins, advances, impact. Seminars in Perinatology. 2011;35:20–28. doi: 10.1053/j.semperi.2010.10.004. [DOI] [PubMed] [Google Scholar]
- Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2010. National Vital Statistic Reports. 2011;60:1–25. http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_02.pdf. [PubMed] [Google Scholar]
- Henson JM, Derlega VJ, Pearson MR, Ferrer R, Holmes K. African American students’ responses to racial discrimination: How race-based rejection sensitivity and social contraints are related to psychological reactions. Journal of Social and Clinical Psychology. 2013;32:504–529. doi: 10.1521/jscp.2013.32.5.504. [DOI] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Iowa Department of Human Services. National poverty guidelines. Calendar years 2000 through 2012. 2012 Retrieved from: http://www.dhs.state.ia.us/Partners/Reports/PeriodicReports/PovertyGuidelines.html.
- Jubinville J, Newburn-Cook C, Hegadoren K, Lacaze-Masmonteil T. Symptoms of acute stress disorder in mothers of premature infants. Advances in Neonatal Care. 2012;12:246–253. doi: 10.1097/ANC.0b013e31826090ac. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Major depression and phobias: The genetic and environmental sources of comorbidity. Psychological Medicine. 1993;23:361–371. doi: 10.1017/S0033291700028464. [DOI] [PubMed] [Google Scholar]
- Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU) Journal Clinical Psychology in Medical Settings. 2010;17:230–237. doi: 10.1007/S10880-010-9202-7. [DOI] [PubMed] [Google Scholar]
- Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Archives of Women’s Mental Health. 2005;8:77–87. doi: 10.1007/S00737-005-0080-1. [DOI] [PubMed] [Google Scholar]
- Mew AM, Holditch-Davis D, Belyea M, Miles MS, Fishel A. Correlates of depressive symptoms in mothers of preterm infants. Neonatal Network. 2003;22:51–60. doi: 10.1891/0730-0832.22.5.51. [DOI] [PubMed] [Google Scholar]
- Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. Journal of Developmental & Behavioral Pediatrics. 2007;28:36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- O’Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children’s behavioural/emotional problems at 4 years: Report from the Avon Longitudinal Study of Parents and Children. British Journal of Psychiatry. 2002;180:502–508. doi: 10.1192/bjp.180.6.502. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, McCabe JE. Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- Pinelli J, Saigal S, Wu YWB, Cunningham C, DiCenso A, Steele S, Turner S. Patterns of change in family functioning, resources, coping and parental depression in mothers and fathers of sick newborns over the first year of life. Journal of Neonatal Nursing. 2008;14:156–165. doi: 10.1016/j.jnn.2008.03.015. [DOI] [Google Scholar]
- Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. https://www.stat.washington.edu/raftery/Research/PDF/socmeth1995.pdf. [Google Scholar]
- Rogers CE, Kidokoro H, Wallendorf M, Inder TE. Identifying mothers of very preterm infants at-risk for postpartum depression and anxiety before discharge. Journal of Perinatology. 2013;33:171–176. doi: 10.1038/jp.2012.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, McLean LM, Psych C. Anxiety disorders during pregnancy and the postpartum period: A systematic review. Journal of Clinical Psychiatry. 2006;67:1285–1298. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- Segre LS, Chuffo-Siewert R, Brock RL, O’Hara MW. Emotional distress in mothers of preterm hospitalized infants: A feasibility trial of nurse-delivered treatment. Journal of Perinatology. 2013;33:924–928. doi: 10.1038/jp.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Davillier M, Bruening P, Hawkins S, Yamashita TS. Social support, psychological distress, and parenting strains in mothers of very low birthweight infants. Family Relations. 1996;45:343–350. doi: 10.2307/585507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281:799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Stewart JC, Rand KL, Hawkins MAW, Stines JA. Associations of the shared and unique aspects of positive and negative emotional factors and sleep quality. Personality and Individual Differences. 2011;50:609–614. doi: 10.1016/j.paid.2010.12.004. [DOI] [Google Scholar]
- Vanderbilt D, Bushley T, Young R, Frank DA. Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: A preliminary study. Journal of Developmental & Behavioral Pediatrics. 2009;30:50–56. doi: 10.1097/DBP.0b013e318196b0de. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin. 1984;96:465–490. doi: 10.1037/0033-2909.96.3.465. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. doi: 10.1016/j.jrp.2004.09.006. [DOI] [Google Scholar]
- Watson D, O’Hara MW, Chmielewski M, McDade-Montez EA, Koffel E, Naragon K, Stuart S. Further validation of the IDAS: Evidence of convergent, discriminant, criterion, and incremental validity. Psychological Assessment. 2008;20:248–259. doi: 10.1037/a0012570. [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, Stuart S. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychological Assessment. 2007;19:253–268. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Watson D, Tellegen A. Toward a consensual structure of mood. Psychological Bulletin. 1985;98:219–235. doi: 10.1037/0033-2909.98.2.219. [DOI] [PubMed] [Google Scholar]
- Wheaton B, Muthén B, Alwin DF, Summers GF. Assessing reliability and stability in panel models. In: Heise DR, editor. Sociological methodology 1977. San Francisco, CA: Jossey-Bass; 1977. pp. 84–136. [Google Scholar]
- Wickberg B, Hwang CP. Counselling of postnatal depression: A controlled study on a population based Swedish sample. Journal of Affective Disorders. 1996;39:209–216. doi: 10.1016/0165-0327(96)00034-1. [DOI] [PubMed] [Google Scholar]
- Zelkowitz P, Milet TH. The course of postpartum psychiatric disorders in women and their partners. Journal of Nervous and Mental Disease. 2001;189:575–582. doi: 10.1097/00005053-200109000-00002. [DOI] [PubMed] [Google Scholar]


