Abstract
Background
Concern over the sustainability of the National Health Service is often focussed on rising numbers of hospital admissions, particularly among older people. Hospital admissions are enumerated routinely by the Hospital Episode Statistics (HES) Service, but published data do not allow individual level service use to be explored. This study linked information on Hertfordshire Cohort Study (HCS) participants with HES inpatient data. with the objective of describing patterns and predictors of admissions among individuals.
Methods
2997 community-dwelling men and women aged 59-73 years completed a baseline HCS assessment between 1998 and 2004; HES and mortality data to 31/03/2010 were linked with the HCS database. This paper describes patterns of hospital use among the cohort at both the admission and individual person level.
Results
The cohort experienced 8741 admissions; rates were 391 per 1000 person-years among men (95%CI 380, 402) and 327 among women (95%CI 316,338), p<0.0001 for gender difference. 1187 men (75%) and 981 women (69%) were admitted to hospital at least once; among these, median numbers of admissions were 3 in men (IQR 1,6) and 2 in women (IQR 1,5). 48% of those ever admitted had experienced an emergency admission and 70% had been admitted overnight.
Discussion
It is possible to link routinely collected HES data with detailed information from a cohort study. Hospital admission is common among community dwelling ‘young-old’ men and women. These linked datasets will facilitate research into lifecourse determinants of hospital admission and inform strategies to manage demand on the National Health Service.
Keywords: hospital admissions, older people, hospital episode statistics, data linkage, healthcare burden
Introduction
The House of Lords’ recently published ‘Ready for Ageing?’ report [1] follows a succession of publications emotive in their concern about the effect of rising hospital admissions on the National Health Service (NHS). It has been suggested that hospitals are ‘on the edge’ [2] and that admissions are ‘out of control’ [3]. The ‘Ready for Ageing?’ report suggested that the burden from long term conditions associated with an ageing population may underlie these trends in hospital admissions. Furthermore it proposed that intervention by improved community services earlier in the disease process could circumvent unnecessary admissions and prevent ‘older people drifting into hospital avoidably’, and concluded that the NHS needs to transform to cope with increasing demand and at the same time improve quality of care. However the emphasis was on managing long-term conditions rather than preventive strategies: it did not consider the lifecourse determinants of hospital admission [1].
Clinical and administrative details of inpatient admissions and outpatient appointments at NHS hospitals in England are collected routinely by the Hospital Episode Statistics (HES) service [4]. They are used in a wide range of healthcare analyses and are important in informing policy on health and social care. They show a rise in the number of inpatient admissions between 2000/01 and 2010/11 focused in the oldest age groups, for example by 33% at 65-74, 45% at 75-84 and 48% at 85+ [5]. A projected increase in the proportion of older people aged 65+ from 17% of UK population in 2010 to 23% in 2035 [6] will increase the number of admissions further.
However these routine data cannot be used to identify patterns and determinants of admissions in individuals. Linkage of HES data with a well-characterised birth cohort study would enable investigation of lifecourse determinants of hospital admission. Only one UK cohort study (the Paisley Renfrew Study [7]) has previously been linked with HES data, but follow-up with regard to hospital admissions ceased in 1995. In the context of recent rises in hospital admissions and a growing awareness of the implications of an ageing population, an update of this research is long overdue.
Between 1998 and 2004, 2997 community-dwelling men and women aged 59-73 years participated in the baseline phase of the Hertfordshire Cohort Study during which their health, lifestyle and socioeconomic characteristics were assessed [8]. We have linked the HCS database with HES records for the study participants to the end of March 2010, thereby yielding a novel and important resource for research into the lifecourse determinants of hospital admission. This paper outlines the process of data linkage and describes patterns of hospital use among the cohort at both the admission and individual person level.
Materials and methods
The Hertfordshire Cohort Study
The Hertfordshire Cohort Study comprises a group of men and women born in that county between 1931 and 39 whose birth, infancy and early childhood were documented by Health Visitors. 1579 men and 1418 women who still lived in Hertfordshire between the end of 1998 and 2004 were interviewed at home and subsequently attended clinics for detailed physiological investigations. These included anthropometry, spirometry, ECGs and blood tests for assessment of cardiovascular and genetic risk. Subsamples underwent a battery of tests of physical performance, DXA scans and knee x-rays. Combining details from the health visitors’ records, information from the interview and measurements made in clinic produced a social and biological lifecourse overview for each individual at baseline. Methods have been described in more detail elsewhere, and the representativeness of the cohort to older people in England has been assessed [8].
Linkage with HES data
The Hertfordshire Cohort Study fulfils the two important prerequisites for linkage with HES data. First, NHS number is recorded and cross-referenced with the internal serial number. It is used purely for tracking participants, who are flagged for continuous notification of death on the Central Register at the NHS Information Centre, and is never included in analysis files.
Secondly, participants gave signed consent for the investigations they underwent in clinic and (on the same form) for researchers to access their medical records in the future. Permission to obtain a HES extract for HCS participants covering the period 01/04/98-31/03/10 was granted by the Ethics and Confidentiality Committee of the National Information Governance Board
HES Records
A hospital episode is a period of care under one consultant, several of which may be recorded during the period between admission and discharge. The HES data obtained for linkage with HCS comprised 15 variables for each episode experienced by a member of the cohort (HES ID and NHS numbers; gender; date, method and source of admission; date and destination at discharge; main specialty; primary and other diagnoses coded to ICD-10 [9]; and primary and other procedures coded to OPCS-4 [10]).
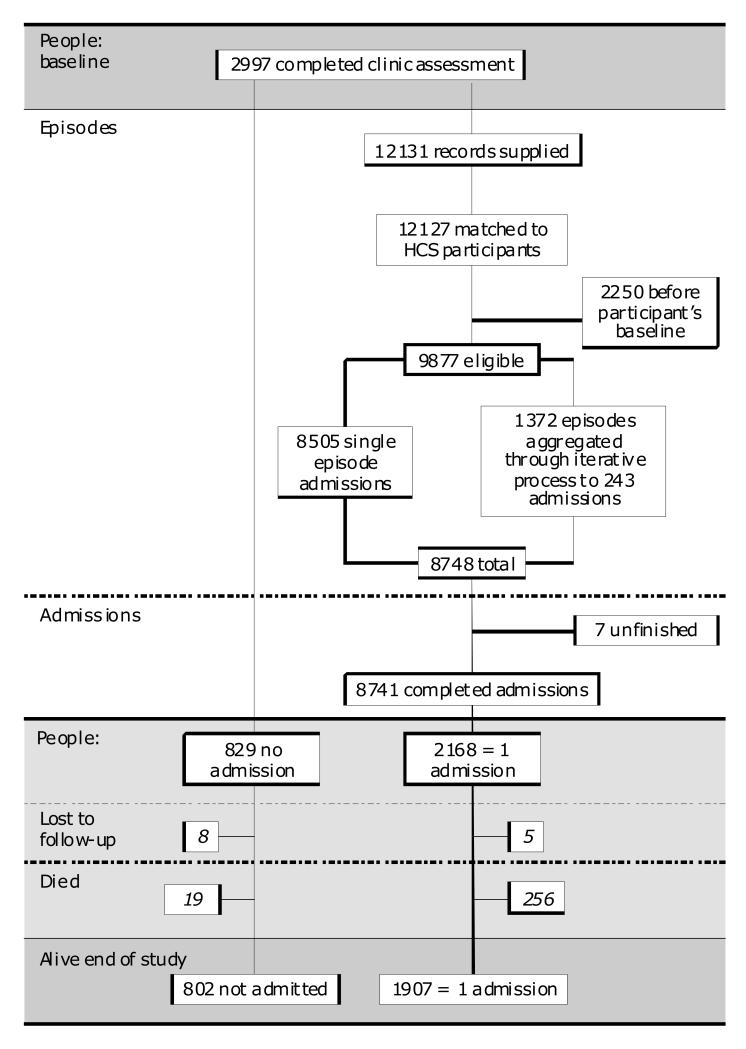
Data were prepared for analysis in two stages and as illustrated in figure 1. First, admission and discharge dates were checked for chronological consistency within and between episode records for the same individual. Common discrepancies included discharge dates that were missing, that preceded the admission date of the same episode, or that succeeded the admission date of a subsequent one. Second, validated consecutive or concurrent episodes were collapsed into one completed admission record, all contributing diagnosis and procedure codes being retained. A total of 8741 admissions was identified among 2168 HCS participants after their date of HCS baseline but before 31/3/10; 829 had no admissions. Mortality data from the NHS Central Register were dovetailed with the combined HCS and HES admissions databases; 275 members of the cohort died during the follow-up period, 19 without admission, 127 during an admission and 129 after being discharged alive. Records relating to the same individual were brought together to create a personal admissions history alongside details of death where appropriate.
Figure 1.
Study Structure
Statistical methods
Data were described at both the admissions and individual levels using means and standard deviations (SD), medians and inter-quartile ranges (IQR) and frequency and percentage distributions. Admission rates were calculated per 1000 person/years according to gender and age groups. All analyses were carried out using Stata 12.1 [11].
Results
Characteristics of admissions
Of 8741 admissions accrued by members of the cohort, 5183 (59%) involved a male patient, 6504 (74%) were elective and 5057 (58%) were day cases. Only 13% lasted more than one week. The median length of stay amongst all admissions was 1 day (IQR 1-4); among overnight admissions it was 5 days for both genders, (IQR 2-9 in men and 3-9 in women). In 98% of admissions patients came from and/or returned to their usual residence. General surgery (n=1257) and general medicine (n=1119) accounted for larger proportions of admissions than any other specialty (14 and 13% respectively). At least one surgical procedure was carried out during 6622 (75.8%) of the admissions; the most common being endoscopy of the bladder, endoscopy of upper GI tract, cataract surgery, angiography, knee replacement and hip replacement in 468, 454, 385, 350, 176 and 174 admissions respectively.
Rates of admission
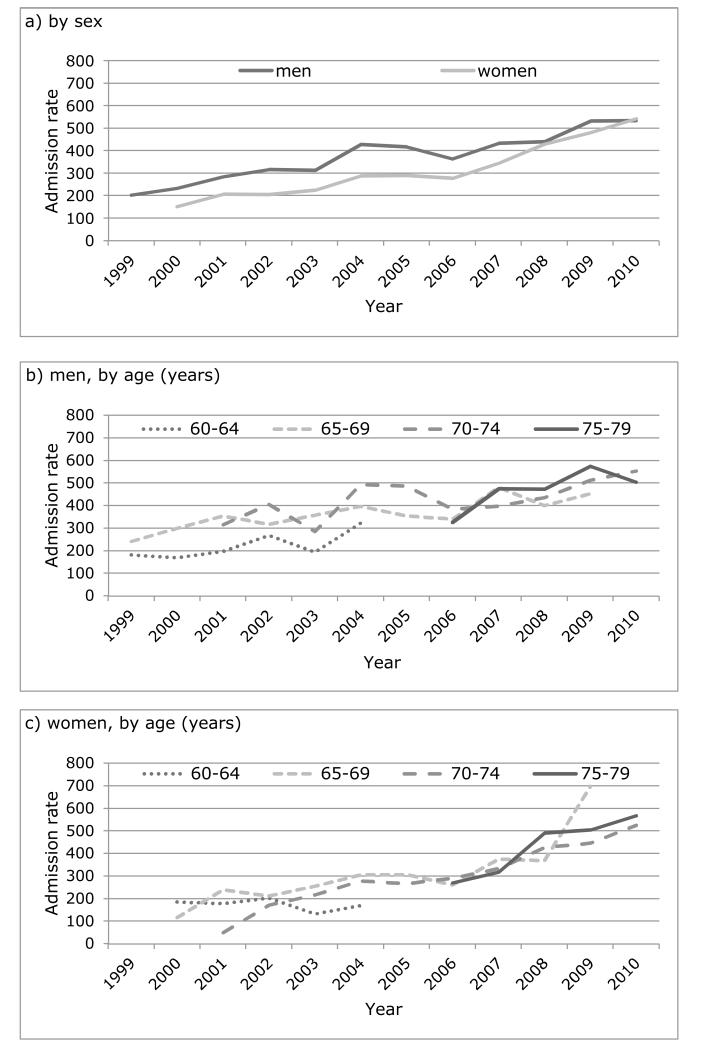
Overall rates of admission per 1000 person-years across the follow-up period were 391 among men [95%CI 380,402] and 327 among women [95%CI 316,338], p<0.0001 for gender difference. Figure 2 shows rates of admission by year, gender and age group; rates of admission increased significantly over time irrespective of adjustment for gender and age (p<0.001 for all).
Figure 2.
Rates of admission per 1000 person years, 1999-2010
Patterns of admission at the individual person level
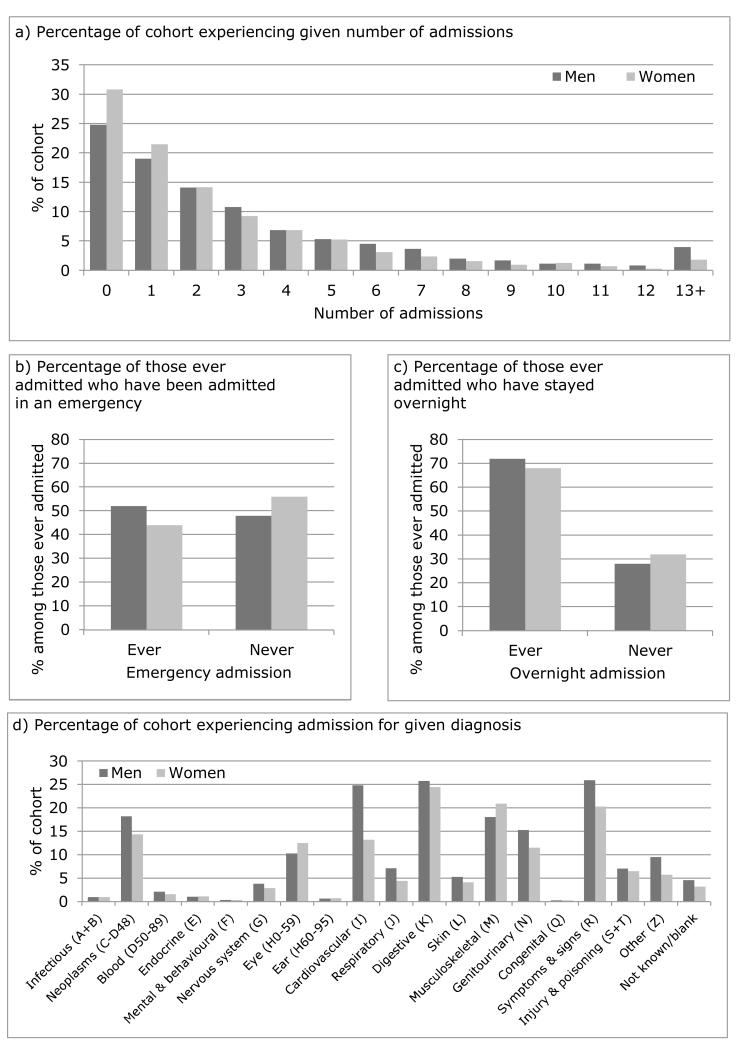
75% (1187) men and 69% (981) women were admitted to hospital at least once during the follow-up period. Figure 3(a) shows the percentage distribution of number of admissions experienced, by gender. Among those who were admitted at least once, the median number of admissions was 3 (IQR 1-6) among men, and 2 (IQR 1-5) among women, with maxima of 34 in men and 56 in women. Nearly half (48%) of those ever admitted had experienced an emergency admission (figure 3b), and over two-thirds (70%) had been admitted overnight at least once (figure 3c). Overall, ever admitted men spent a median of 8 days (IQR 3-22) in hospital during the follow-up period and ever admitted women a median of 6 days (IQR 2-16). High total days’ stay resulted from both frequent day case admissions (eg for procedures such as haemodialysis or blood transfusions) and fewer long ones (eg for diagnoses such as mental illness).
Figure 3.
Individual level admissions characteristics
Figure 3(d) shows the proportion of the overall cohort experiencing an admission by ICD chapter of primary diagnosis. Men most commonly experienced admissions coded to chapter R (signs and symptoms), chapter K (digestive disease) and chapter I (cardiovascular disease). Among women, the equivalent ranking for frequency of occurrence of admissions involving specific ICD-10 chapters was first, chapter K (digestive disease); followed by chapter M (musculoskeletal disease), and chapter R (signs and symptoms).
1992 (91.9%) of ever-admitted cohort members had at least one surgical procedure carried out during an admission, the most common being endoscopy of the upper GI tract, angiography, cataract surgery, endoscopy of the bladder, knee replacement and hip replacement in 345, 303, 262, 225, 148 and 136 people respectively.
Deaths among cohort members
275 members of the cohort died during the follow-up period; 189 (12%) men and 86 (6.1%) women. 19 deaths (11 men and 8 women) occurred among people who had no admissions, 127 (89 men and 38 women) during an admission and 129 (89 men and 40 women) after being discharged.
Discussion
We have shown that it is possible to link routinely collected HES data with detailed information collected as part of a cohort study. Hospital admission is common among community-dwelling men and women in early old age; 75% of men and 69% of women were admitted to hospital at least once during the 10-year follow-up period. Presence of co-morbidity is common in early old age [12], and this paper suggests that the burden of ill-health translates into substantial NHS service use. A healthy responder bias was apparent in HCS [8], a study based in the relatively affluent South East of England: for these reasons the healthcare burden of the ageing national population is likely to be even greater than these data suggest.
HCS is the first English cohort study to use record linkage to identify individual-level longitudinal patterns of service use among a group of well-characterised individuals. The facility to link individual-level admissions episodes within HES data has been used infrequently; linkage with outside sources (eg the National Joint Registry [13], a cancer registry [14;15], or the General Practice Research Database [16]) is rarer still. The Oxford Record Linkage Study (ORLS) is an example of a study which has linked births, deaths and hospital admissions at the individual level [17-20]; however, the ORLS was not able to consider individual level characteristics other than those recorded routinely. In Scotland record linkage is routine [21]. Maternity records and births, cancer registrations, hospital discharges and deaths are permanently linked. This fact has been exploited by a group of cohorts collectively known as MIDSPAN studies [7]; three samples originally screened in middle age in the 1960s and 70s, along with a fourth comprising their offspring. The Paisley Renfrew study is one of them, and comprises over 15 000 men and women sampled from the population of two industrial towns in central Scotland whose health profile was characterised at age 45-64. Follow-up of hospital admissions was reported to 1995 [22;23], by which time 79% of the cohort had experienced at least one, and an average of 4.6 admissions over a 23 year period. The study concluded that a high proportion of hospital days accrued near the time of death and that the absolute demand for hospital services was ‘strikingly large and increasing over time’. This study demonstrated that baseline lung function, BMI and deprivation were important predictors of subsequent admission. Patterns and predictors of hospital admissions have not been reported since 1995.
Our study had some limitations: first, doubts have been expressed over both case ascertainment and coding accuracy in Hospital Episode Statistics and errors have been shown to exist, including adults apparently treated in paediatrics, children in geriatrics and men in obstetrics and gynaecology [24]. Given that 17.5 million finished consultant episodes were recorded during 2011-12 [4], some mistakes are hardly surprising. Furthermore, case ascertainment has been compared with a number of source registers, for example the ‘yellow-card’ system for reporting adverse drug reactions [25], police statistics on road traffic accidents [26] and cancer registry data [27] and in general, HES have been found to be the more complete. In addition, discharge coding accuracy was assessed in a systematic review published in 2011, which reported an improvement since payment by results was introduced in 2002 and found the accuracy of the primary diagnostic code to be 96.0% (IQR 89.3-96.3). The authors concluded that routinely collected data are sufficiently robust for research and managerial decision making [28]. Secondly, a healthy responder bias has been described in HCS and the study was conducted in the relatively affluent southeast of England [8]. However the demographic, social and medical characteristics among HCS participants have been shown to be broadly comparable with those in the nationally representative Health Survey for England [8].
Our study also had many strengths. First, the data used were collected routinely by the Hospital Episode Statistics service for England. They cover all patients treated in NHS hospitals however funded, and NHS patients treated in private hospitals. Only privately funded patients attending private hospitals and those treated outside England are excluded. Secondly, HES data have the advantage that they are not subject to the effects of attrition of the sickest members of the cohort. Response bias, which is introduced if the least healthy individuals are selectively lost to follow-up, is a particular problem among ageing cohorts [29]. HES data accrue for all members of the cohort, whether they live independently or not, and irrespective of cognitive ability. Thirdly, continued follow-up through hospital admissions into advanced old-age is possible; a new data linkage service [30] launched by the NHS Information Centre in September 2012 should streamline the process. Finally, older people differ in the use they make of hospital services, and whilst some experience many admissions, others need none at all. It is possible to link records within HES to produce individual histories that differentiate those with many admissions from those with few, but people with no admissions clearly generate no records and would thus be omitted from such linked data. Linkage with the Hertfordshire Cohort Study enables individuals who experienced hospital admission to be contrasted with those who did not.
In summary, we have shown that it is possible, with appropriate consents, to link routinely collected HES data with the detailed information collected as part of a cohort study. Moreover, we have shown that hospital admission is common among community-dwelling young-old men and women. Given the current level of concern about the sustainability of the NHS in the face of an ageing population, the linked HCS/HES database represents an important resource for research into lifecourse determinants of hospital admission. The potential of the linked dataset extends beyond the descriptive results presented in this paper and offers the opportunity to identify social, biological and medical predictors of admission. This research will inform strategies called for by the House of Lords to manage demand on the NHS.
Key points.
Concern over the sustainability of the National Health Service is focussed on rising numbers of hospital admissions, particularly among older people.
We have shown that it is possible to link routinely collected HES data with detailed information collected as part of a cohort study
Hospital admission is common among community dwelling ‘young-old’ men and women.
These linked datasets will facilitate research into lifecourse determinants of hospital admission and inform strategies to manage demand on the National Health Service.
References
- 1.House of Lords Select Committee on Public Service and Demographic Change. Ready for Ageing. Stationery Office; 2013. (HL Paper 140). [Google Scholar]
- 2.Royal College of Physicians . Hospitals on the edge? The time for action. Royal College of Physicians; London: 2012. [Google Scholar]
- 3.Robinson P. Are hospital admissions out of control? CHKS; Alcester: 2010. [Google Scholar]
- 4.HESonline [accessed 29/08/13];Headline Figures, 2010-11. NHS Information Centre for Health and Social Care. 2012 http://www.hscic.gov.uk/hes.
- 5.NHS Information Centre Elderly people account for bigger proportion of NHS hospital activity every year, report shows. [accessed 10/05/12]. content no longer available.
- 6.Office for National Statistics . Population ageing in the United Kingdom its constituent countries and the European Union. Office for National Statistics; London: 2012. [Google Scholar]
- 7.Hart CL, MacKinnon PL, Watt GCM, et al. The Midspan studies. Int J Epidemiol. 2005;34:28–34. doi: 10.1093/ije/dyh348. [DOI] [PubMed] [Google Scholar]
- 8.Syddall HE, Aihie Sayer A, Dennison EM, Martin HJ, Barker DJP, Cooper C. Cohort Profile: The Hertfordshire Cohort Study. Int J Epidemiol. 2005;34:1234–1242. doi: 10.1093/ije/dyi127. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organisation International Classification of Diseases (ICD) 2011.
- 10.Health and Social Care Information Centre OPCS-4 classification. 2013.
- 11.Statacorp . Stata Statistical Software Release 10. Statacorp LP; College Station TX: 2007. [Google Scholar]
- 12.Pierce MB, Silverwood RJ, Nitsch D, et al. Clinical disorders in a post war British cohort reaching retirement: evidence from the first national birth cohort study. PLoS one. 2012;7:e44857. doi: 10.1371/journal.pone.0044857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stafford G, Charman S, Borroff M, Newell C, Tucker J. Total hip replacement for the treatment of acute femoral neck fractures: results from the National Joint Registry of England and Wales at 3-5 years after surgery. Ann R Coll Surg Engl. 2012;94:193–198. doi: 10.1308/003588412X13171221589720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maddams J, Utley M, Moller H. A person-time analysis of hospital activity among cancer survivors in England. Br J Cancer. 2011;105:S38–S45. doi: 10.1038/bjc.2011.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Downing A, Wilson R. Older people’s use of accident and emergency services. Age Ageing. 2005;34:24–30. doi: 10.1093/ageing/afh214. [DOI] [PubMed] [Google Scholar]
- 16.van Staa T, Patel D, Gallagher A, de Bruin M. Glucose-lowering agents and the patterns of risk for cancer: a study with the General Practice Research Database and secondary care data. Diabetologia. 2012;55:654–665. doi: 10.1007/s00125-011-2390-3. [DOI] [PubMed] [Google Scholar]
- 17.Acheson ED, Evans JG. The Oxford Record Linkage Study: A review of the method with some preliminary results. Proc R Soc Med. 1964;57:269–274. doi: 10.1177/003591576405700409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldacre MJ, Ferguson JA. In-patient workload in medical specialties: 1. Demographic profiles and time trends from linked statistics. QJM. 1995;88:649–659. [PubMed] [Google Scholar]
- 19.Ashton CM, Ferguson JA, Goldacre MJ. In-patient workload in medical specialties: 2. Profiles of individual diagnoses from linked statistics. QJM. 1995;88:661–672. [PubMed] [Google Scholar]
- 20.Goldacre MJ, Ferguson JA, Welch A, Kettlewell MGW. Profiles of workload in general surgery from linked hospital statistics. Br J Surg. 1993;80:1073–1077. doi: 10.1002/bjs.1800800854. [DOI] [PubMed] [Google Scholar]
- 21.Kendrick S. The Scottish Record Linkage System. Information Services Division (ISD) NHS Scotland; 2012. [Google Scholar]
- 22.Hanlon P, Walsh D, Whyte BW, Scott S, Lightbody P, Gilhooly MLM. Hospital use by an ageing cohort: an investigation into the association between biological, behavioural and social risk markers and subsequent hospital utilization. J Public Health Med. 1998;20:467–476. doi: 10.1093/oxfordjournals.pubmed.a024804. [DOI] [PubMed] [Google Scholar]
- 23.Hanlon P, Walsh D, Whyte BW, Scott SN, Lightbody P, Gilhooly MLM. The link between major risk factors and important categories of admission in an ageing cohort. J Public Health Med. 2000;22:81–89. doi: 10.1093/pubmed/22.1.81. [DOI] [PubMed] [Google Scholar]
- 24.Brennan L, Watson M, Klaber R, Charles T. The importance of knowing context of hospital episode statistics when reconfiguring the NHS. BMJ. 2012;344:2432. doi: 10.1136/bmj.e2432. [DOI] [PubMed] [Google Scholar]
- 25.Barrow P, Waller P, Wise L. Comparison of hospital episodes with ‘drug-induced’ disorders and spontaneously reported adverse drug reactions. Br J Clin Pharmacol. 2006;61:233–237. doi: 10.1111/j.1365-2125.2005.02554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gill M, Goldacre MJ, Yeates DG. Changes in safety on England’s roads: analysis of hospital statistics. BMJ. 2006;333:73–75. doi: 10.1136/bmj.38883.593831.4F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moller H, Richards S, Hanchett N, et al. Completeness of case ascertainment and survival time error in English cancer registries: impact on 1-year survival estimates. Br J Cancer. 2011;105:170–176. doi: 10.1038/bjc.2011.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burns EM, Rigby E, Mamidanna R, et al. Systematic review of discharge coding accuracy. J Public Health. 2011;34:138–148. doi: 10.1093/pubmed/fdr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howe LD, Tilling K, Galobardes B, Lawlor DA. Loss to follow-up in cohort studies. Bias in estimates of socioeconomic inequalities. Epidemiol. 2013;24:1–9. doi: 10.1097/EDE.0b013e31827623b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Data Linkage Service [accessed 29/08/13];Health and Social Care Information Centre. http://www.hscic.gov.uk/dles.