Abstract
Background
The global burden of atrial fibrillation (AF) is unknown.
Methods and Results
We systematically reviewed population-based studies of AF published 1980–2010, from the 21 Global Burden of Disease (GBD) regions to estimate global/regional prevalence, incidence, as well as morbidity and mortality related to AF (DisModMR software). Of 377 potential studies identified, 184 met pre-specified eligibility criteria. The estimated number of individuals with AF globally in 2010 was 33·5 million [(20·9 million males (UI, 19·5–22·2 million) and 12·6 million females (UI, 12·0–13·7 million)]. Burden associated with AF, measured as disability adjusted life-years (DALYs), increased by 18·8% (UI, 15·8–19·3) in males and 18·9% (UI, 15·8–23·5) in females, from 1990 to 2010. In 1990, the estimated age-adjusted prevalence rates of AF (per 100,000 population) were 569·5 in males [95% uncertainty interval (UI), 532·8–612·7] and 359·9 in females (UI, 334·7–392·6); the estimated age-adjusted incidence rates were 60·7/100,000 person-years in males (UI, 49·2–78·5) and 43·8 in females (UI, 35·9–55·0). In 2010 the prevalence rate increased to 596·2 (UI, 558·4–636·7) in males and 373·1 (UI, 347·9–402·2) in females; incidence rate increased to 77·5 (UI, 65·2–95·4) in males and 59·5 (UI, 49·9–74·9) in females. Mortality associated with AF was higher in females, and increased by 2-fold (UI, 2·0–2·2) and 1·9-fold (UI, 1·8–2·0) in males and females, respectively, from 1990 to 2010.
Conclusions
These findings provide evidence of progressive increases in overall burden, incidence, prevalence and AF-associated mortality between 1990–2010. Systematic, global surveillance of AF is required to better direct prevention and treatment strategies.
Keywords: atrial fibrillation, epidemiology, incidence, burden, prevalence, global
Atrial fibrillation (AF) is the most common arrhythmia of clinical significance.1 In adjusted models, AF is associated with increased morbidity, especially stroke and heart failure, as well as increased mortality.2–5 AF constitutes a significant public health problem, and estimates suggest that this condition accounts for 1% of the National Health Service budget in the United Kingdom6 and $16–26 billion of annual US expenses.7, 8
Several regional studies suggest rising prevalence and incidence of AF.9–13 These secular trends may in part be explained by the demographic transition to an inverted age pyramid, as frequency of AF increases with advancing age. Others have demonstrated an increase in AF incidence after age-adjustment, which is probably a reflection of comorbidities and cardiovascular risk factors in addition to other factors such as lifestyle changes.14, 15 In the United States, it is estimated that the number of adults with AF would more than double by the year 2050;16 even higher increases have been predicted.14
In view of the emergence of AF as a ‘growing epidemic’,15, 17 an assessment of the global burden of AF is warranted. We therefore conducted a comparative assessment of the burden of AF across defined time periods based on available epidemiological data from the 21 Global Burden of Disease (GBD) regions.
Methods
The Global Burden of Disease Study
Our analysis was performed within the framework of the latest GBD, Injuries, and Risk Factors Study (GBD 2010 Study).18 The GBD 2010 Study is a collaborative effort led by a consortium that includes Harvard University, the Institute for Health Metrics and Evaluation at the University of Washington, Johns Hopkins University, the University of Queensland, the University of Tokyo, Imperial College London, and the World Health Organization. It follows on the original GBD 1990 Study commissioned by the World Bank in 1991 and aims to systematically assess global data on all diseases and injuries. GBD 2010 provides a common instrument for assessing mortality as well as morbidity. The goal was to provide comparable estimates at different time periods, with analysis of secular trends. Detailed information about the data, techniques and methods for estimation of different disease parameters have been published elsewhere.19–21
Search Strategy and Data Sources
As a subcommittee of the GBD 2010 Committee on Cardiovascular Disease and following the GBD 2010 protocol, the GBD Arrhythmias Panel performed a systematic review of the available literature (Appendix 1) to identify epidemiological studies of AF (1980–2010) that were population-based. For the initial identification of published studies we used the following search terms: “atrial fibrillation”, “atrial flutter”, “epidemiology”, “incidence”, “prevalence”, “mortality”, and “case fatality rate”. MEDLINE, EMBASE and LILACS were queried for studies published between 1980 and 2010 (for LILACS the time period was 1982–2010). There were no restrictions based on language of publication. Details of the search are outlined in Appendix 2. The initial search (Phase 1) generated abstracts that were reviewed (Phase 2) based on pre-specified inclusion and exclusion criteria (Appendix 3). Whereas all studies on AF epidemiology in the general population were included, studies that were conducted on selected clinical sub-groups such as inpatients or those with heart failure were excluded, in order to arrive at accurate estimates of AF burden at a population-wide level. The selected abstracts underwent full text reviews (Phase 3) to confirm eligibility, generating a final list of publications selected for abstraction. Each publication was assigned to one of 21 epidemiologic regions as designated in GBD 2005. In order to minimize potential bias due to inconsistent case definitions of AF all published studies of paroxysmal, persistent or permanent/chronic AF and atrial flutter were included.
Statistical Methods
Incidence rate was defined as the annual number of new cases with AF, divided by the population at mid-year. Prevalence rate was defined as the overall number of cases with the total population as denominator. Prevalence and incidence rates were age-adjusted. Rates were presented per 100,000 persons or person-years with 95% uncertainty intervals (UI). The denominators were derived from the United Nations (UN) population database (http://www.un.org/esa/population/) and classifications of countries, regions and groups (e.g. developed and developing countries) followed the definitions of the World Bank (http://data.worldbank.org/about/country-classifications) and GBD core team decisions.22
Modeling of AF as a cause of death
Mortality associated with AF was estimated using an integrated method with information of several country level covariates utilized to inform the analysis.19 All combinations of the covariates with a significant coefficient (P<0·05) and expected direction of the effect were used to estimate the number of deaths. The performance of each model in terms of external validity was evaluated and constituted the final ensemble model estimate. External validity criteria were employed to rank all models and produce ensemble results.23 The covariates and external validity of the ensemble model are reported in Appendix 4 (Tables 1 and 2). In the next step, each individual cause of death was adjusted to obtain overall cardiovascular mortality (CoDCorrect process)19. The GBD method provides the mortality rate attributable to AF, as opposed to total case fatality rate in AF patients.
Table 1.
Estimated age-adjusted prevalence rates with 95% Uncertainty Intervals of Atrial Fibrillation (per 100,000) for males and females.
| Year | 1990 | 1995 | 2000 | 2005 | 2010 |
|---|---|---|---|---|---|
| Males | |||||
| Global, All Ages | 569·5 (532·8–612·7) | 578·1 (541·2–620·9) | 586·8 (549·8–629·5) | 595·1 (557·3–639·0) | 596·2 (558·4–636·7) |
| Age ≥ 35 years | 1,307·4 (1,222·5–1,407·3) | 1,327·3 (1,243·2–1,425·7) | 1,347·6 (1,263·4–1,445·8) | 1,366·6 (1,281·0–1,467·1) | 1,368·5 (1,280·8–1,462·7) |
| Developed Countries | 608·2 (547·0–693·5) | 625·6 (564·0–712·5) | 643·1 (580·3–730·2) | 660·0 (594·5–740·8) | 660·9 (597·1–738·2) |
| Developing Countries | 546·6 (503·0–599·6) | 551·1 (506·6–604·8) | 555·8 (511·0–610·1) | 561·3 (517·5–618·4) | 565·7 (522·9–617·6) |
| Females | |||||
| Global, All Ages | 359·9 (334·7–392·6) | 363·4 (338·5–395·3) | 366·7 (342·0–397·8) | 369·6 (345·5–399·9) | 373·1 (347·9–402·2) |
| Age ≥ 35 years | 826·5 (768·4–902·3) | 834·7 (776·6–909·2) | 842·3 (784·7–915·5) | 849·0 (792·4–919·6) | 856·8 (797·7–923·5) |
| Developed Countries | 362·5 (319·3–422·3) | 370·1 (326·7–429·5) | 377·5 (334·0–436·8) | 385·1 (340·1–446·8) | 387·7 (343·8–450·0) |
| Developing Countries | 358·2 (329·8–393·0) | 359·0 (330·8–394·0) | 359·8 (331·5–395·0) | 360·9 (331·6–396·0) | 366·1 (337·4–400·8) |
Table 2.
Estimated age-adjusted incidence rates with 95% Uncertainty Intervals of Atrial Fibrillation (per 100,000 person years) for males and females.
| Year | 1990 | 2010 |
|---|---|---|
| Males | ||
| Global, All Ages | 60·7 (49·2–78·5) | 77·5 (65·2–95·4) |
| Age ≥ 35 years | 141·0 (114·6–182·6) | 181·2 (152·6–222·8) |
| Developed Countries | 78·4 (67·5–91·9) | 123·4 (107·6–141·5) |
| Developing Countries | 50·0 (33·8–76·8) | 53·8 (38·7–79·8) |
| Females | ||
| Global, All Ages | 43·8 (35·9–55·0) | 59·5 (49·9–74·9) |
| Age ≥ 35 years | 102·0 (83·9–127·9) | 139·7 (117·1–175·3) |
| Developed Countries | 52·8 (45·0–62·9) | 90·4 (77·8–104·5) |
| Developing Countries | 36·0 (24·5–54·7) | 40·0 (27·2–62·6) |
Modeling of morbidity associated with AF
We used incidence, prevalence, excess mortality, and AF mortality rate (estimated by CODEm process) in a Bayesian meta-regression tool (DisMod-MR: Figure 1).21 DisMod-MR estimates a generalized negative binomial model for all the epidemiological data with fixed and random effects. Data modeled with fixed effects include age, covariates that predict country variation in the quantity of interest, variation across studies due to attributes of the study protocol, and random effects of super-region, region, and country. DisMod-MR can be used to estimate age-sex- country specific prevalence from heterogeneous and often sparse data sets. We used DisMod to estimate the total number of patients living with AF. The history of at least one confirmed AF episode is the common definition of AF used in prevalence studies. We used this definition in the modeling and estimation of different epidemiological parameters such as prevalence, incidence, and case fatality (excess mortality rate).21
Figure 1.
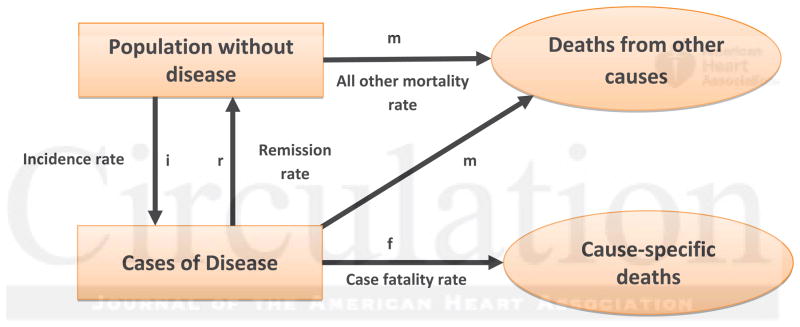
Conceptual disease model. Flow-chart illustrating the conceptual disease model utilized (DisMod-MR software). The model includes the number of people without the disease (AF in this case), the number of people with the disease, the number of deaths associated with the disease, and the number of deaths from all other causes. The transitions between these states are represented by i: incidence, r: remission, ƒ: case fatality, and m: all other mortality. In the case of AF, remission was assumed to be zero. (Modified from: Barendregt et al. A generic model for the assessment of disease epidemiology: the computational basis of DisMod II. Popul Health Metr. 2003 Apr 14; 1:4. Copyright © 2003 Barendregt et al; licensee BioMed Central Ltd.) (AF- Atrial Fibrillation).
As for all conditions assessed in the GBD project, burden associated with AF was measured as disability adjusted life-years (DALYs). The DALY metric was introduced in the original GBD 1990 study as a means of assessing the disability of chronic disorders.22 DALYs combine information regarding premature death (years of life lost, YLL) as well as disability caused by the condition (years lived with disability, YLD). One DALY corresponds to one lost year of health and is calculated as YLL plus YLD. As previously described in detail,24, 25 YLDs are calculated by multiplying the estimated number of incident cases by the average duration of the disease and a disability weight factor (range 0–1 where 0 is total health and 1 is total disability). Disability weights for sequelae of multiple disease conditions were estimated by four population-based surveys in Bangladesh, Indonesia, Peru, and Tanzania, a telephone survey in the United States, and an open-access web-based survey.26 AF sequelae were defined as “daily medication and at least minimal interference with daily activities” and accordingly assigned a disability weight of 0·031.
Role of the Funding Source
The funding sources had no influence over the study, the interpretation of the results, writing of the manuscript or the decision to submit for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Data Availability
The initial search generated 4,574 abstracts (Appendix 1). Of these, 377 (8·2%) published studies were identified as meeting initial criteria. After full text review, 193 studies were excluded (i.e. did not meet the pre-specified quality measures) and the remaining184 studies moved to the abstraction stage. The majority of studies were from Western Europe and North America (35·9% and 35·6% of included data sources, respectively).
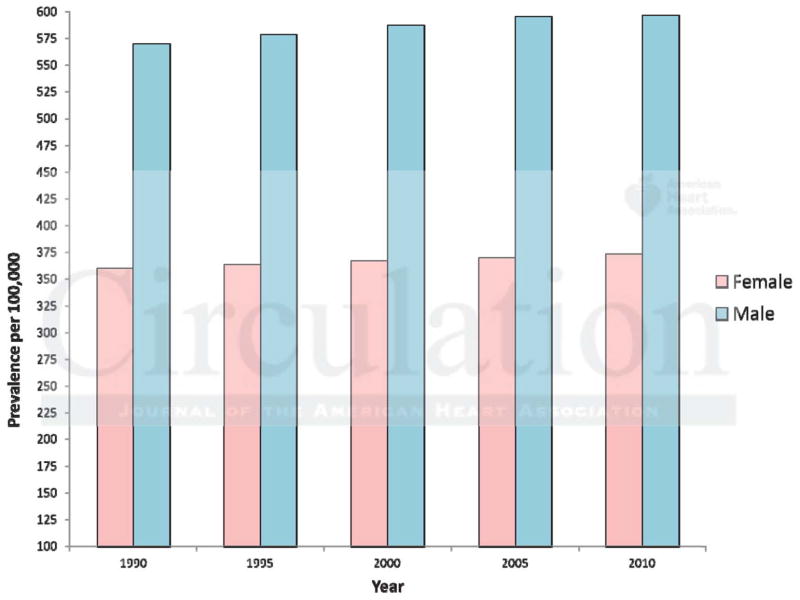
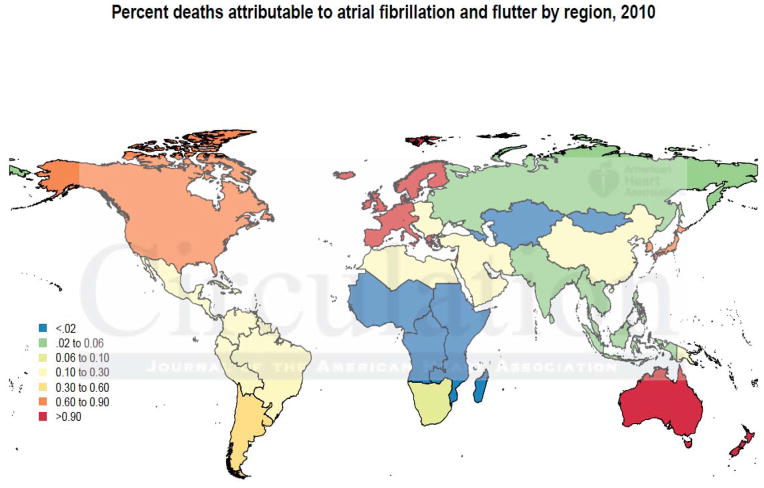
Prevalence of AF
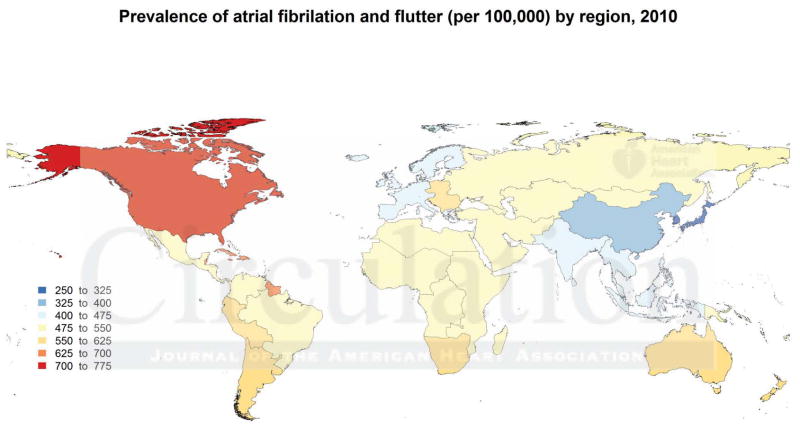
Table 1 shows the estimated age-adjusted AF prevalence rates stratified by sex (complete data for all GBD regions in Supplemental Tables 1a & 1b; Figure 2). In 1990 the estimated global prevalence rates (per 100,000 population) were 569·5 in males (95% UI, 532·8–612·7) and 359·9 (UI, 334·7–392·6) in females. In 2010, prevalence rates were 596·2 (UI, 558·4–636·7) in males and 373·1 (UI, 347·9–402·2) in females. The prevalence rates showed a modest increase between 1990 and 2010 (Figure 3) across both sexes. Developed countries had higher prevalence rates compared to developing countries, however this difference was more pronounced in males than in females. For all time points, the prevalence was higher in males compared to females. There was significant variation in prevalence between GBD regions. The lowest prevalence rates (2010) were estimated in Asia Pacific region for both males and females (340·2 and 196·0 respectively). The highest rates were estimated in North America (925·7 for males and 520·8 for females). The prevalence and incidence for Sub- Saharan Africa was lower compared to a developed region such as North America. Overall, for the Sub-Saharan Africa super region, in 2010, the prevalence of AF (age-adjusted, per 100,000 population) was 659.8 (95% UI 511.0–850.4) for males and 438.1 (340.2–561.0) for females. The median change in prevalence was higher in developed countries, with the largest increase noted in North America (40.1%) and the least change in Sub Saharan Africa, East (3.4%; Supplemental Table 2). Prevalence rates increased significantly with increasing age (Supplemental Figures 1A & 1B), with rates in the ≥35 year population observed to be more than double the overall prevalence. Applying the DisMod MR estimated prevalence rates to the world population of 2010, the estimated number of individuals with AF globally is 20·9 million (95% UI 19·5–22·2 million) males and 12·6 million (UI, 12·0–13·7 million) females.
Figure 2.
World Map Showing the Age-adjusted Prevalence rates (per 100,000 population) of AF in the 21 Global Burden of Disease (GBD) regions, 2010 (AF- Atrial Fibrillation).
Figure 3.
Prevalence of AF: 1990 to 2010. Estimated age-adjusted global prevalence of Atrial Fibrillation (per 100,000 population) for males and females from 1990 to 2010 (AF- Atrial Fibrillation).
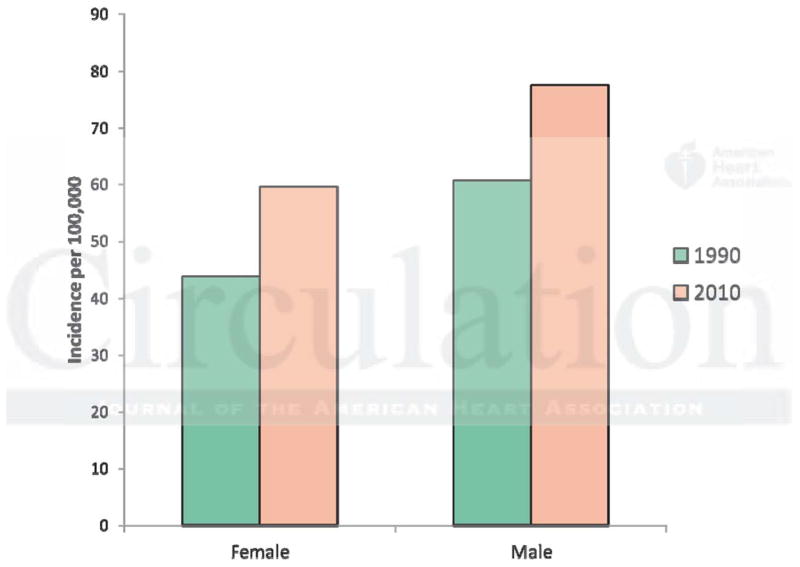
Incidence of AF
Table 2 shows the estimated age-adjusted incidence rates of AF stratified by sex (complete data for all GBD regions in Supplemental Tables 3a & 3b). In 1990 the overall incidence rates of the world population were 60·7 (UI, 49·2–78·5) per 100,000 person-years in males and 43·8 (UI, 35·9–55·0) in females. In 2010, the estimated incidence rates were higher, 77·5 (UI, 65·2–95·4) in males and 59·5 (UI, 49·9–74·9) in females as shown in Figure 4. There were significantly higher (~2-fold) incidence rates in developed regions when compared to developing countries. For both time periods, similar to the observations for prevalence, AF incidence rates were higher in males compared to females. Again, there was great variation between GBD regions. The lowest incidence rates (2010) were estimated in the Asia Pacific region for both males and females (33·8 and 19·8 respectively). The highest rates were estimated in North America (264·5 for males and 196·3 for females). As for prevalence, the incidence rates were also lower in the Sub-Saharan region, reported as 58.4 (43.7–78.5) and 42.7 (31.1–60.5) in males and females respectively. Incidence rates were also higher in the older age-groups (Supplemental Figures 2A & 2B).
Figure 4.
Incidence of AF: 1990 & 2010. Estimated age-adjusted global incidence (per 100,000 person years) for males and females for 1990 and 2010. (AF- Atrial Fibrillation)
When applying the estimated incidence rates to the world population of 2010, the estimated number of new AF cases per year is 2·7 million (95% UI 2·3–3·3 million) for males and 2·0 million (UI, 1·7–2·6 million) for females.
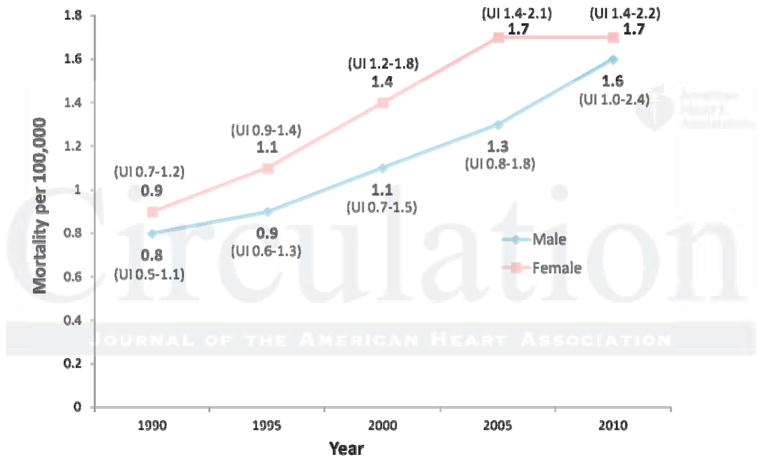
Mortality and Disease Burden associated with AF
The age-adjusted mortality rate (per 100,000 population) for AF in 1990 was 0·8 (UI, 0·5–1·1) for males and 0·9 (UI, 0·7–1·2) for females. The age-adjusted mortality rate increased to 1·6 (UI, 1·0–2·4) and 1·7 (UI, 1·4–2·2) in 2010, representing 2 fold (UI, 2·0–2·2) and 1·9 fold (UI, 1·8–2·0) increases, for males and females respectively (Table 3; full data for all GBD regions as Supplemental Tables 4a & 4b). Mortality increased steadily through 1995, 2000 and 2005 (Figure 5), especially in the developed world. Mortality associated with AF was higher in females overall; this was mainly driven by comparatively higher mortality in females (compared to males) in developing countries (Figure 6). In 2010, the estimated numbers of total deaths (males and females) represented less than 1% of the global mortality in the vast majority of the 21 GBD regions (Figure 7).
Table 3.
Estimated age-adjusted mortality rates with 95% Uncertainty Intervals (per 100,000) associated with Atrial Fibrillation for males and females.
| Year | 1990 | 1995 | 2000 | 2005 | 2010 |
|---|---|---|---|---|---|
| Males | |||||
| Global, All Ages | 0·8(0·5–1·1) | 0·9(0·6–1·3) | 1·1(0·7–1·5) | 1·3(0·8–1·8) | 1·6(1·0–2·4) |
| Age ≥ 35 years | 1·9(1·3–2·8) | 2·2(1·4–3·1) | 2·7(1·7–3·6) | 3·2(2·0–4·4) | 3·8(2·4–5·8) |
| Developed Countries | 1·3(0·9–1·9) | 1·6(1·1–2·2) | 2·0(1·3–2·7) | 2·3(1·6–3·2) | 2·7(1·9–4·3) |
| Developing Countries | 0·4(0·2–0·8) | 0·4(0·2–0·8) | 0·5(0·3–0·9) | 0·6(0·3–1·1) | 0·7(0·4–1·3) |
| Females | |||||
| Global, All Ages | 0·9(0·7–1·2) | 1·1(0·9–1·4) | 1·4(1·2–1·8) | 1·7(1·4–2·1) | 1·7(1·4–2·2) |
| Age ≥ 35 years | 2·2(1·8–3·0) | 2·7(2·2–3·4) | 3·5(2·8–4·4) | 4·0(3·4–5·0) | 4·2(3·4–5·4) |
| Developed Countries | 1·1(1·0–1·3) | 1·4(1·2–1·6) | 1·9(1·7–2·2) | 2·3(2·0–2·7) | 2·4(2·0–3·0) |
| Developing Countries | 0·7(0·4–1·4) | 0·8(0·4–1·4) | 0·9(0·5–1·5) | 0·9(0·6–1·6) | 1·0(0·6–1·7) |
Figure 5.
Mortality Associated with AF: 1990 to 2010. Estimated age-adjusted mortality (per 100,000 population) associated with AF from 1990 to 2010 (AF- Atrial Fibrillation).
Figure 6.
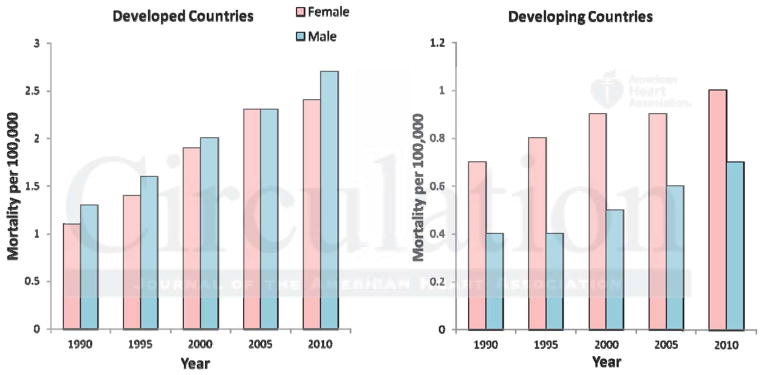
Mortality Associated with AF stratified by sex and type of Region (Developed vs. Developing). Mortality associated with AF was higher in males and females in the Developed regions. The significantly higher mortality in females in the Developing regions is responsible for the overall higher AF-related mortality among females compared to males (AF- Atrial Fibrillation).
Figure 7.
Proportion of Global deaths Associated with AF in 2010. The map shows color-coded proportions (in percentages) of global deaths in 2010 associated with AF (AF- Atrial Fibrillation)
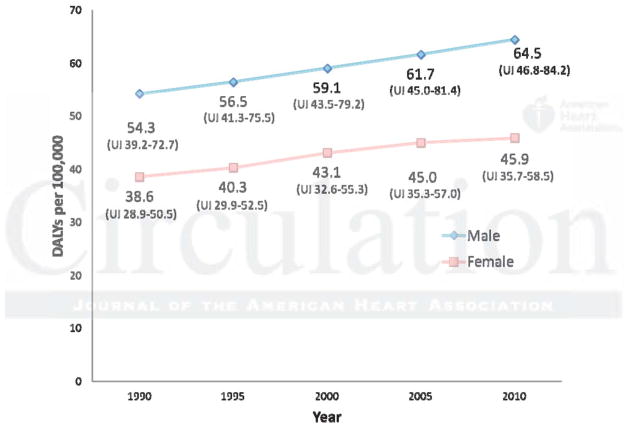
The estimated age-adjusted DALYs (per 100,000 population) due to AF were 54·3 (UI, 39·2–72·7) and 38·6 (UI, 28·9–50·5) in 1990 for males and females respectively. This number increased to 64·5 (UI, 46·8–84·2) and 45·9 (UI, 35·7–58·5) in 2010, representing increases of 18·8% (UI, 15·8–19·3) and 18·9% (UI, 15·8–23·5) for males and females respectively (Table 4; complete data for all GBD regions as Supplemental Tables 5a & 5b; Figure 8). In keeping with the higher incidence and prevalence of AF, the DALYs were higher in developed compared to developing countries. The rate of change in DALYs was also higher in developed compared to developing countries (Supplemental Table 2).
Table 4.
Estimated age-adjusted DALYs with 95% Uncertainty Intervals (per 100,000) associated with Atrial Fibrillation for males and females.
| Year | 1990 | 1995 | 2000 | 2005 | 2010 |
|---|---|---|---|---|---|
| Males | |||||
| Global, All Ages) | 54·3 (39·2–72·7) | 56·5 (41·3–75·5) | 59·1 (43·5–79·2) | 61·7 (45·0–81·4) | 64·5 (46·8–84·2) |
| Age ≥ 35 years | 125·2 (90·5–167·1) | 130·4 (95·8–174·0) | 136·6 (100·9–182·7) | 142·6 (104·1–188·0) | 149·3 (108·7–194·5) |
| Developed Countries | 63·4 (47·2–83·9) | 67·8 (50·7–89·5) | 72·8 (54·7–94·9) | 77·2 (58·4–100·5) | 81·5 (60·8–106·2) |
| Developing Countries | 48·2 (33·3–65·6) | 49·2 (34·5–67·8) | 50·6 (35·6–69·4) | 52·2 (36·4–70·9) | 54·5 (37·7–73·2) |
| Females | |||||
| Global, All Ages | 38·6 (28·9–50·5) | 40·3 (29·9–52·5) | 43·1 (32·6–55·3) | 45·0 (35·3–57·0) | 45·9 (35·7–58·5) |
| Age ≥ 35 years | 89·3 (67·1–116·6) | 93·5 (69·5–121·2) | 100·2 (76·1–128·2) | 104·6 (82·3–132·1) | 106·8 (82·9–135·8) |
| Developed Countries | 39·6 (30·0–51·8) | 42·6 (32·5–54·7) | 47·0 (36·9–59·9) | 50·1 (40·0–63·2) | 51·0 (39·8–63·7) |
| Developing Countries | 37·0 (26·3–49·5) | 37·6 (26·6–51·3) | 38·9 (27·8–53·2) | 39·8 (29·2–52·5) | 41·1 (30·5–54·4) |
DALYs- Disability Adjusted Life Years
Figure 8.
DALYs Related to AF. Estimated age-adjusted DALYs (per 100,000) related to AF: 1990 to 2010 (AF- Atrial Fibrillation; DALYs- Disability Adjusted Life-Years)
Discussion
Our systematic review of the current worldwide epidemiological data on AF confirms the emergence of this condition as a global epidemic, with significant and progressive effects on estimated disability and mortality. Furthermore there were specific differences identified based on age and GBD region that are likely to have significant implications for global public health.
As expected, higher rates of AF were observed in older age groups. For example, males 75–79 years have double the prevalence rate compared to males age 65–69 years, and more than 5-fold higher prevalence compared to males age 55–59 years. The 2010 rates are higher than 1990 with increases in both prevalence and incidence rates in both sexes. Other regional studies have reported an increasing prevalence of AF, especially in the developed world. Piccini et al. reported a greater increase in the prevalence of AF (from 41.1 to 85.8 per 1000 between 1993 to 2007, with an annual rate of increase of about 5%)13 compared to the present study, which is likely to be related to differences in the population studied with the former study being restricted to elderly Medicare beneficiaries in the United States. The annual new cases of AF globally in 2010 were estimated at close to 5 million, which together with the increasing trends observed, highlight the observation that the burden of AF is growing rapidly.
The exact reasons for these trends are unknown but may be partly explained by aging trends in the global population. One hypothesis for the increasing incidence is that AF in the majority of people is a vascular disease due to hypertension, atherosclerosis, and other cardiovascular risk factors, which increase arterial stiffness, cause diastolic dysfunction, and atrial volume overload, resulting in AF. Analysis of global risk factors in the GBD 2010 study showed that high blood pressure is the number one risk factor globally (increasing from 4th position in 1990), accounting for 7% of all global DALYs. High body mass index ranks sixth in the global list, ascending from 10th position in 1990. Deaths attributable to hypertension increased by 28.8% from 1990 to 2010, while deaths attributable to obesity increased by 71.7%18. Thus, it appears that the increase in AF burden potentially could be linked to such risk factors at a global level. While these alterations can be observed as part of the aging process, they are also likely to be involved independently of aging. While a renewed focus on risk factors may help, other contributors to increasing AF incidence such as aging of the population, better survival from other disease conditions and improved diagnosis need to be acknowledged as well.
Temporal trends in AF prevalence may in addition, result from lead time bias (such that AF cases may be diagnosed earlier in their course), increased survival from coexistent cardiovascular conditions such as ischemic heart disease and heart failure due to improved management of such cardiovascular comorbidities resulting in a larger high-risk group. In addition, increased awareness of AF symptoms and clinical diagnosis also likely play a role. Of interest, the change in AF prevalence from 2005 to 2010 was seen to be minimal, especially among males in the developed countries as opposed to developing countries. While the exact reason for the leveling of prevalence rates is difficult to ascertain, one possibility may be an improved awareness and focus on management of risk factors in the developed world.
AF is known to have a significant impact on health care costs, with the major cost-drivers being hospitalizations, stroke, and loss of productivity.6, 27, 28 In the present study, AF was associated with less than 1% of all deaths in most World Health Organization (WHO) regions. However, AF is known to co-exist and interact with other conditions contributing to a worse prognosis than for individuals without AF. For example, recent meta-analyses have shown that patients with heart failure and myocardial infarction have worse outcomes if they also have AF.29, 30 Moreover, new-onset AF in heart failure patients might be associated with a particularly poor prognosis.31, 32
There were significant variations in the AF burden by GBD region, with developed countries having a greater burden overall. Published studies suggest that individuals of European ancestry have a higher incidence and prevalence of AF. Furthermore, recent reports indicate that higher degree of European ancestry is associated with an increased predisposition to AF.33 However, part of the global variation in AF epidemiology may also be attributable to better surveillance in developed countries. In the 1990 GBD study, no specific data for AF was reported, but cardiovascular diseases as a group accounted for 9·7% of the global DALYs with ischemic heart disease being the fifth ranking disorder in total number of DALYS (~47x106) behind lower respiratory infections, diarrheal diseases, perinatal disorders, and unipolar major depression.34 In 2010, ischemic heart disease moved up to the number one position; with cardiovascular disease accounting for 11·8% of global DALYs. With the exception of Sub-Saharan Africa and Oceania, cardiovascular disease ranked among the top three causes of DALYs in most regions.20 In keeping with these trends, DALYs related to AF increased by about 18% from 1990 to 2010. Although the absolute DALYs related to AF (about 52 per 100,000 overall) is much lower compared to conditions such as chronic obstructive lung disease (1114 per 100,000), diabetes mellitus (680 per 100,000) and chronic kidney disease (307 per 100,000)20, as discussed earlier, AF can interact with other diseases in multiple ways, potentially contributing to worse outcomes. The rise of cardiovascular disease burden in developing countries possibly indicates an ongoing transition towards non-communicable diseases, earlier associated more with developed nations. Especially with current, rapidly evolving demographic changes in large population centers of the developing world, the effects of the rising global AF burden merits careful consideration with respect to distribution of dwindling health care resources. Additionally there is an urgent need to design and deploy effective surveillance strategies for AF that will guide future, WHO-region specific prevention.
Limitations
Our study has several limitations. AF is a heterogeneous condition, and in a subset of individuals can be asymptomatic.35, 36 Both features underscore the difficulties associated with making accurate estimates of the burden of this disease. Therefore our findings could represent an underestimate. In addition, we note that differences in extent of patient surveillance, including access to health care, use of routine electrocardiograms and assessment of electrical devices such as pacemakers may be contributing to secular trends. We also acknowledge the inability of observational data to accurately estimate the relative importance of various factors contributing to such trends. Moreover, we cannot rule out the possible impact of publication-bias and did not actively seek out unpublished manuscripts or data. Estimation of the mortality associated with AF was performed based on modeling the causes of death using input from all available cause of death data. As with any cause of death analysis, assignment of cause of death may be prone to some misclassification. Further, any inferences about future trends should be made with caution trategies since the rapid development of surveillance and treatment strategies might change mortality and prevalence rates. Due to the low availability of data from several regions, our findings should be interpreted with caution. Regional differences in AF burden do exist, but our observations may not always be a reliable estimate, due to geographical disparity of data density and non-representative population bias, as well as estimates based on imputations. However, even though the need for better estimates particularly in the developing world is crucial, our report likely represents the ‘best available’ data source for global policy and decision making. Targeted population surveillance studies of AF could fill the gaps in data and permit more reliable burden of disease estimates in coming decades.
Conclusion
There have been progressive increases in the worldwide prevalence and incidence of AF with significant effects on associated morbidity and mortality, findings that have implications for public health policy and health care costs. Evidence for geographic variation in AF burden, especially in developing versus developed nations indicates that systematic, global surveillance of AF is required to formulate effective region-specific prevention and treatment strategies.
Supplementary Material
Acknowledgments
Funding Sources: This research was supported by core funding from the Bill & Melinda Gates Foundation. SSC holds the Pauline and Harold Price Endowed Chair of Cardiac Electrophysiology at the Heart Institute, Cedars-Sinai Medical Center, Los Angeles, CA. RH is supported by a grant from the Swedish Research Council (#2011-1071). EJB is supported by 1R01HL092577; 1R01HL102214; 1RC1HL101056; 1R01AG028321. MR is supported by a grant from the Netherlands Organization for Scientific Research (Veni grant 016·136·055). The funding sources had no influence over the study or the interpretation of the results.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Zamorano JL. Acc/aha/esc 2006 guidelines for the management of patients with atrial fibrillation: A report of the american college of cardiology/american heart association task force on practice guidelines and the european society of cardiology committee for practice guidelines (writing committee to revise the 2001 guidelines for the management of patients with atrial fibrillation): Developed in collaboration with the european heart rhythm association and the heart rhythm society. Circulation. 2006;114:e257–354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: Population-based estimates. Am J Cardiol. 1998;82:2N–9N. doi: 10.1016/s0002-9149(98)00583-9. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: The framingham heart study. Circulation. 1998;98:946–952. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 4.Thrall G, Lane D, Carroll D, Lip GY. Quality of life in patients with atrial fibrillation: A systematic review. Am J Med. 2006;119:448 e441–419. doi: 10.1016/j.amjmed.2005.10.057. [DOI] [PubMed] [Google Scholar]
- 5.Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, D’Agostino RB, Murabito JM, Kannel WB, Benjamin EJ. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: The framingham heart study. Circulation. 2003;107:2920–2925. doi: 10.1161/01.CIR.0000072767.89944.6E. [DOI] [PubMed] [Google Scholar]
- 6.Stewart S, Murphy NF, Walker A, McGuire A, McMurray JJ. Cost of an emerging epidemic: An economic analysis of atrial fibrillation in the uk. Heart. 2004;90:286–292. doi: 10.1136/hrt.2002.008748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee WC, Lamas GA, Balu S, Spalding J, Wang Q, Pashos CL. Direct treatment cost of atrial fibrillation in the elderly american population: A medicare perspective. J Med Econ. 2008;11:281–298. doi: 10.3111/13696990802063425. [DOI] [PubMed] [Google Scholar]
- 8.Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the united states. Circ Cardiovasc Qual Outcomes. 2011;4:313–320. doi: 10.1161/CIRCOUTCOMES.110.958165. [DOI] [PubMed] [Google Scholar]
- 9.Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, D’Agostino RB, Massaro JM, Beiser A, Wolf PA, Benjamin EJ. Lifetime risk for development of atrial fibrillation: The framingham heart study. Circulation. 2004;110:1042–1046. doi: 10.1161/01.CIR.0000140263.20897.42. [DOI] [PubMed] [Google Scholar]
- 10.Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, Stijnen T, Lip GY, Witteman JC. Prevalence, incidence and lifetime risk of atrial fibrillation: The rotterdam study. Eur Heart J. 2006;27:949–953. doi: 10.1093/eurheartj/ehi825. [DOI] [PubMed] [Google Scholar]
- 11.Stewart S, Hart CL, Hole DJ, McMurray JJ. Population prevalence, incidence, and predictors of atrial fibrillation in the renfrew/paisley study. Heart. 2001;86:516–521. doi: 10.1136/heart.86.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolf PA, Benjamin EJ, Belanger AJ, Kannel WB, Levy D, D’Agostino RB. Secular trends in the prevalence of atrial fibrillation: The framingham study. Am Heart J. 1996;131:790–795. doi: 10.1016/s0002-8703(96)90288-4. [DOI] [PubMed] [Google Scholar]
- 13.Piccini JP, Hammill BG, Sinner MF, Jensen PN, Hernandez AF, Heckbert SR, Benjamin EJ, Curtis LH. Incidence and prevalence of atrial fibrillation and associated mortality among medicare beneficiaries, 1993–2007. Circ Cardiovasc Qual Outcomes. 2012;5:85–93. doi: 10.1161/CIRCOUTCOMES.111.962688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in olmsted county, minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–125. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 15.Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: Clinical implications. J Am Coll Cardiol. 2001;37:371–378. doi: 10.1016/s0735-1097(00)01107-4. [DOI] [PubMed] [Google Scholar]
- 16.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The anticoagulation and risk factors in atrial fibrillation (atria) study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 17.Lip GY, Kakar P, Watson T. Atrial fibrillation--the growing epidemic. Heart. 2007;93:542–543. doi: 10.1136/hrt.2006.110791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, 3rd, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Hanafiah KM, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, 3rd, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stockl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2013;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA, 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De Leon FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2013;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basanez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabe E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fevre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gonzalez- Medina D, Gosselin R, Grainger R, Grant B, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Laden F, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Levinson D, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mock C, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O’Donnell M, O’Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA, 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leon FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiebe N, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD. Disability-adjusted life years (dalys) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2013;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 21.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basanez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabe E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fevre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gosselin R, Grainger R, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Ma J, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O’Donnell M, O’Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA, 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leon FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Years lived with disability (ylds) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, Naghavi M, Salomon JA, Shibuya K, Vos T, Wikler D, Lopez AD. Gbd 2010: Design, definitions, and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 23.Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: An integrated approach using codem. Popul Health Metr. 2012;10:1. doi: 10.1186/1478-7954-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global burden of disease study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 25.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 26.Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, Begum N, Shah R, Karyana M, Kosen S, Farje MR, Moncada G, Dutta A, Sazawal S, Dyer A, Seiler J, Aboyans V, Baker L, Baxter A, Benjamin EJ, Bhalla K, Bin Abdulhak A, Blyth F, Bourne R, Braithwaite T, Brooks P, Brugha TS, Bryan-Hancock C, Buchbinder R, Burney P, Calabria B, Chen H, Chugh SS, Cooley R, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, Davis A, Degenhardt L, Diaz-Torne C, Dorsey ER, Driscoll T, Edmond K, Elbaz A, Ezzati M, Feigin V, Ferri CP, Flaxman AD, Flood L, Fransen M, Fuse K, Gabbe BJ, Gillum RF, Haagsma J, Harrison JE, Havmoeller R, Hay RJ, Hel-Baqui A, Hoek HW, Hoffman H, Hogeland E, Hoy D, Jarvis D, Karthikeyan G, Knowlton LM, Lathlean T, Leasher JL, Lim SS, Lipshultz SE, Lopez AD, Lozano R, Lyons R, Malekzadeh R, Marcenes W, March L, Margolis DJ, McGill N, McGrath J, Mensah GA, Meyer AC, Michaud C, Moran A, Mori R, Murdoch ME, Naldi L, Newton CR, Norman R, Omer SB, Osborne R, Pearce N, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Pourmalek F, Prince M, Rehm JT, Remuzzi G, Richardson K, Room R, Saha S, Sampson U, Sanchez-Riera L, Segui-Gomez M, Shahraz S, Shibuya K, Singh D, Sliwa K, Smith E, Soerjomataram I, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Taylor HR, Tleyjeh IM, van der Werf MJ, Watson WL, Weatherall DJ, Weintraub R, Weisskopf MG, Whiteford H, Wilkinson JD, Woolf AD, Zheng ZJ, Murray CJ. Common values in assessing health outcomes from disease and injury: Disability weights measurement study for the global burden of disease study 2010. Lancet. 2013;380:2129–2143. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blomstrom Lundqvist C, Lip GY, Kirchhof P. What are the costs of atrial fibrillation? Europace. 13(Suppl 2):ii9–12. doi: 10.1093/europace/eur087. [DOI] [PubMed] [Google Scholar]
- 28.Bruggenjurgen B, Rossnagel K, Roll S, Andersson FL, Selim D, Muller-Nordhorn J, Nolte CH, Jungehulsing GJ, Villringer A, Willich SN. The impact of atrial fibrillation on the cost of stroke: The berlin acute stroke study. Value Health. 2007;10:137–143. doi: 10.1111/j.1524-4733.2006.00160.x. [DOI] [PubMed] [Google Scholar]
- 29.Mamas MA, Caldwell JC, Chacko S, Garratt CJ, Fath-Ordoubadi F, Neyses L. A meta-analysis of the prognostic significance of atrial fibrillation in chronic heart failure. Eur J Heart Fail. 2009;11:676–683. doi: 10.1093/eurjhf/hfp085. [DOI] [PubMed] [Google Scholar]
- 30.Jabre P, Roger VL, Murad MH, Chamberlain AM, Prokop L, Adnet F, Jouven X. Mortality associated with atrial fibrillation in patients with myocardial infarction: A systematic review and meta-analysis. Circulation. 2011;123:1587–1593. doi: 10.1161/CIRCULATIONAHA.110.986661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swedberg K, Olsson LG, Charlesworth A, Cleland J, Hanrath P, Komajda M, Metra M, Torp-Pedersen C, Poole-Wilson P. Prognostic relevance of atrial fibrillation in patients with chronic heart failure on long-term treatment with beta-blockers: Results from comet. Eur Heart J. 2005;26:1303–1308. doi: 10.1093/eurheartj/ehi166. [DOI] [PubMed] [Google Scholar]
- 32.Ahmed A, Perry GJ. Incident atrial fibrillation and mortality in older adults with heart failure. Eur J Heart Fail. 2005;7:1118–1121. doi: 10.1016/j.ejheart.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 33.Marcus GM, Alonso A, Peralta CA, Lettre G, Vittinghoff E, Lubitz SA, Fox ER, Levitzky YS, Mehra R, Kerr KF, Deo R, Sotoodehnia N, Akylbekova M, Ellinor PT, Paltoo DN, Soliman EZ, Benjamin EJ, Heckbert SR Candidate-Gene Association Resource S. European ancestry as a risk factor for atrial fibrillation in african americans. Circulation. 2010;122:2009–2015. doi: 10.1161/CIRCULATIONAHA.110.958306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global burden of disease study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 35.Furberg CD, Psaty BM, Manolio TA, Gardin JM, Smith VE, Rautaharju PM. Prevalence of atrial fibrillation in elderly subjects (the cardiovascular health study) Am J Cardiol. 1994;74:236–241. doi: 10.1016/0002-9149(94)90363-8. [DOI] [PubMed] [Google Scholar]
- 36.Blackshear JL, Kopecky SL, Litin SC, Safford RE, Hammill SC. Management of atrial fibrillation in adults: Prevention of thromboembolism and symptomatic treatment. Mayo Clin Proc. 1996;71:150–160. doi: 10.4065/71.2.150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The initial search generated 4,574 abstracts (Appendix 1). Of these, 377 (8·2%) published studies were identified as meeting initial criteria. After full text review, 193 studies were excluded (i.e. did not meet the pre-specified quality measures) and the remaining184 studies moved to the abstraction stage. The majority of studies were from Western Europe and North America (35·9% and 35·6% of included data sources, respectively).