Abstract
Background:
Tumors involving the hand skeleton are rare. However, a basic knowledge of hand tumors is necessary for every clinician. This is due to the importance of distinguishing typical benign tumors from life or limb threatening malignant ones.
Methods:
This study is a review of 99 cases of osseous hand tumors presented to the department of orthopedic surgery, Imam Khomeini Hospital in Tehran, Iran, from December 1990 to February 2011.
Results:
Ninety-one cases were benign osseous tumors of the hand and eight tumors were malignant which four of them were considered as primary and four considered as metastatic type. The most common benign tumors were enchondroma and osteoid osteoma. Other benign tumors were epidermoid bone cyst, giant cell tumor of the bone, aneurysmal bone cyst, osteoblastoma, and osteochondroma. Primary malignant tumors were extremely rare and we have reported two chondrosarcomas, one osteosarcoma and one Ewing’s sarcoma involving the hand skeleton.
Conclusion:
This study indicates that the history, physical examination, laboratory and radiographic data as well as clinicians’ knowledge of specific hand tumors are required for the best management strategy. New techniques could lead to earlier diagnosis, prevent complications and indentify the most effective type of treatment.
Keywords: Benign bone tumors, Hand tumors, Malignant bone tumors, Surgical management
Introduction
Hand skeleton tumors can be categorized into benign, primary malignant and metastatic groups. The most prevalent tumors are in the benign group (1-3). Malignant and metastatic osseous tumors of the hand are extremely rare, however, worthy to report (4, 5). In a few studies about bony tumors in the hand, enchondroma was reported up to 90% tumors (1-3). Due to the rarity and lack of a large study, the true incidences of other bony tumors of the hand are not exactly known. Because of the great importance of the hand in the body and its high utility, even smallest problems in the hand need to be approached seriously. However, presence of an osseous hand tumor is rare and early investigation is of great importance (6). In this study, we have reviewed 99 cases of osseous hand tumors which were diagnosed, managed and followed in one center over a twenty year period.
Materials and Methods
From December 1990 to February 2011, one hundred and twenty-two patients with osseous hand tumors admitted to the Department of Orthopedic Surgery, Imam Khomeini Hospital, affiliated with Tehran University of Medical Sciences. Twenty-three (18.8% of total cases with hand tumor) were excluded from the study because of the previous adjacent skin malignancy or incomplete follow-up examinations. Ultimately, ninety-nine patients were enrolled in the present study. The optimal surgical intervention was employed as indicated and then, the patients were followed. Data were evaluated to estimate the prevalence, rates and associated factors related to osseous hand tumors such as demographic data, surgical method and recurrence.
Results
Ninety-nine patients with osseous hand tumors were assessed. Their history at the time of admission included sixty-eight complains of a mass growth, sixty-four complains of pain, nine complains of limited range of movement in adjacent joint and seven complains of pathologic fracture at the site of the tumor. Two patients were diagnosed incidentally. Demographic data of all patients are presented in Table 1. Ninety-one (91.9%) tumors were benign. Thirty-one (34.1% of patients with benign osseous tumors) patients had enchondroma. Nineteen (61.3%) patients with enchondroma were female and twelve (38.7%) patients were male. The mean ± SD age was 32.7± 9.1 (age ranged, 8 to 72 years). The locations of the tumors were noted as follows: nineteen patients with proximal phalangeal involvement, four patients with middle phalangeal involvement and eight patients with metacarpal involvement. Fifteen (48.4%) patients complained of the bone pain at the tumor site. In addition, six (19.3%) patients had a fracture at the site of the tumor with a minor trauma. Surgical treatment of the tumor was performed after the fracture healing about six weeks. Curettage and bone grafting appeared to be successful in 29 (93.5%) cases and two (6.5%) cases recurred (mean follow up, 95 months). Malignant degeneration was not observed in the second operation in recurrent cases and repeated curettage and bone grafting was successful in both patients.
Table 1.
Clinical Data of the Patients
| Tumor | Number of Cases (n) | Age (Mean± Standard Deviation), Range | Sex | Complaint | site | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Mass | Pain | Limited ROM* | Fracture | Incidental | Distal radius | Carpal | Metacarpal | Phalanx | Recurrence | |||
| Enchondroma | 31 | 32.7± 9.1 (8, 72) | 12 | 19 | 23 | 15 | 1 | 6 | 2 | 0 | 0 | 8 | 23 | 2 |
| Osteoid Osteoma | 25 | 27.5± 8.6 (12, 48) | 13 | 12 | 2 | 23 | 6 | 0 | 0 | 1 | 4 | 4 | 16 | 3 |
| Epidermoid Cyst | 10 | 43.5± 14.5 (12, 78) | 7 | 3 | 10 | 6 | 0 | 0 | 0 | 0 | 0 | 2 | 8 | 1 |
| Giant Cell Tumor | 8 | 39.5± 11.7 (22, 62) | 5 | 3 | 8 | 4 | 0 | 0 | 0 | 4 | 0 | 0 | 4 | 3 |
| Aneurysmal Bone Cyst | 7 | 22.7+ 6.7 (14, 35) | 3 | 4 | 7 | 2 | 2 | 1 | 0 | 1 | 0 | 2 | 4 | 3 |
| Osteoblastoma | 6 | 16± 4.2 (11, 21) | 4 | 2 | 6 | 6 | 0 | 0 | 0 | 0 | 0 | 2 | 4 | 1 |
| Osteochondroma | 4 | 17.7± 3.8 (13, 23) | 1 | 3 | 4 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 0 |
| Metastasis | 4 | 33± 18.5 (16, 62) | 2 | 2 | 4 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | - |
| Chondrosarcoma | 2 | 65± 3 (62, 68) | 1 | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | - |
| Ewing’s Sarcoma | 1 | 16 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | - |
| Osteosarcoma | 1 | 22 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | - |
ROM, Range of Motion
Twenty-five (27.5% of benign osseous tumors) cases of osteoid osteoma were managed. Thirteen (52%) cases were male and twelve (48%) cases were female with mean age of 27.5 ± 8.6 (age ranged, 12 to 48 years). The average time from the onset of symptoms to diagnosis was 18 months (range, 2 to 60 months). Surgical curettage or excision was the treatment of choice in our cases which appeared to be successful in total of twenty-two (88%) patients (mean follow up, 98 months) (Figure 1). Recurrence was occurred in three (12%) patients due to incomplete excision. Curettage or excision was successful in recurrent cases.
Figure 1.
Osteoid Osteoma of the hand: A 28-year-old man complained of pain in proximal phalanx of ring finger from four months ago. A. Clinical pictures. B. Radiographic appearance. C. T 99 bone scan shows increased uptake in the ring finger. D. CT scan shows sclerotic nidus and confirms diagnosis. E. Removal of nidus by surgery.
Ten (11% of benign osseous tumors) cases were diagnosed as epidermoid bone cyst. History of trauma was positive in five (50%) patients. Mean age of diagnosis was 43.5 ± 14.5 (age ranged, 12 to 78 years). Treatment consisted of curettage followed by the bone grafting with only one (10%) recurrence case (mean follow up, 99 months). The recurrent case was successfully treated with repeated curettage and bone grafting.
Eight (8.8% of benign osseous tumors) patients were assessed with giant cell tumor (GCT) of bone included four cases with proximal phalangeal and four cases with distal radius involvement. Mean age of the diagnosis was 39.5 ± 11.7 (range, 22 to 62 years). Three (37.5%) cases recurred after initial management. Initial management in two phalangeal tumors was resection with interposition bone grafting and proximal interphalangeal joint arthrodesis by k-wire. Initial management in two other phalangeal tumors was extended curettage by cryosurgery as adjuvant and bone grafting that tumor was recurred with this technique. Secondary operation was performed as a resection with interposition bone grafting and proximal interphalangeal joint arthrodesis by k-wire. Four patients with distal radius GCTs were treated with extended curettage by cryosurgery. Recurrence occurred in one distal radius tumor. Recurrent tumor treated resection with interposional bone grafting and arthrodesis of radiocarpal joint by dorsal plating. No recurrence occurred in patients who initially or secondary managed with this protocol (mean follow up, 106 months).
Aneurysmal bone cyst was diagnosed in seven (7.7%) patients. They were managed with curettage and bone grafting and followed. Recurrence was noted in three (42.9%) cases. Resection and arthrodesis with interpositional bone grafting was the second operation choice for recurred cases. No additional recurrence was reported after a sufficient period of follow-up examinations (mean follow up, 118 months).
Osteoblastoma was diagnosed in six (6.6% of benign bone tumors) patients. Our treatment was curettage and bone grafting. Only one (16.7%) case was recurred. Resection and interpositional bone grafting was performed in second operation without any recurrence (mean follow up, 81 months). In addition, four (4.4% of benign bone tumors) cases of osteochondroma were noted. Resection was performed and none of them recurred (mean follow up, 94 months).
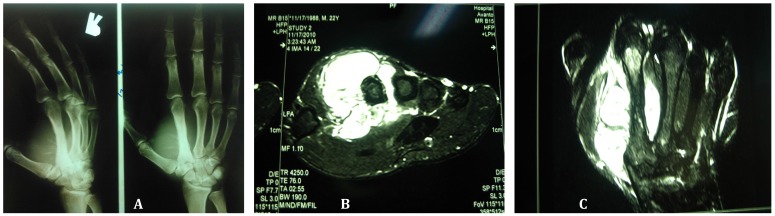
Eight (8.1%) cases of malignant osseous hand tumors were also diagnosed and managed. Four (50%) tumors were primary. Two (25% of malignant osseous tumors) chondrosarcomas were managed; one in a 62–year-old male and one in a 68-year-old female, both locating in their metacarpal bones. Ray amputation was performed in both cases. One (12.5% of malignant osseous tumors) osteosarcoma in the second metacarpal bone of a 22 year old male was also reviewed (Figure 2). The patient treated by a ray amputation combined with neoadjuvant and adjuvant chemotherapy. Other primary malignant tumor of the hand was one (12.5% of malignant osseous tumors) Ewing’s sarcoma in a 16-year-old male in the forth metacarpal bone. Ray amputation combined with neoadjuvant and adjuvant chemotherapy was performed in this case. None of the four patients experienced recurrence after 68 months of follow up examination. Four (50% of malignant osseous tumors) metastatic osseous hand tumors were also reviewed. They comprised one leukemic infiltration in a 16–year-old male, one breast cancer metastasis in a 36-year-old female, one metastasis from adenocarcinoma of the colon in a 48-year-old male and one metastasis from esophageal carcinoma in a 62-year-old male. All patients complained of pain. Amputation through the joint proximal to the level of involvement performed in all metastatic involvement cases. This method was successful in pain reduction but mean survival was 5.5 months and all metastatic patients expired due to underling neoplasm.
Figure 2.
Osteosarcoma in a 22-year-old man in the second metacarpal bone.
A: “sunburst” periosteal reaction in radiography. B: Axial MRI image. C: Coronal MRI image.
Discussion
Enchondroma is the most common type of the hand tumor (1, 3, 7). In the present study population, enchondroma was the most frequent diagnosis and thirty-one (34.1%) benign osseous tumors were diagnosed with enchondroma. The most common site of involvement that has been reported is proximal phalanges with nineteen (61.3%) tumors of the total study population were located at this site (1, 8, 9). Central lucent lesion with symmetric cortical expansion and thinning is a characteristic radiographic appearance which leads to complications such as pain and pathologic fracture (2, 3, 9, 10). The fracture is allowed to heal before tumoral excision (1-3). Curettage and bone grafting is the treatment of choice, with rare recurrence rate ranging from 2% to 15% (1, 3, 10). Radiographic follow-ups are recommended postoperatively after one year to evaluate the recurrence (1, 7). Recurrence needs further investigations to assess the possibility of chondrosarcoma (1, 2).
As previously reported, osteoid osteoma was the second frequent osseous tumor of the hand (2, 11). Female to male occurrence ratio is 2-4 to 1. Most cases occur in the second decade of life (11). Pain is a usual presentation with a dull ache shifting to a severe localized pain which aggravates during the night and alleviates dramatically with nonsteroidal anti-inflammatory drugs (1, 2, 12). Diagnosis is often delayed in comparison with other bone tumors and often lasts more than one year (13-14). Surgical management of the above mentioned tumor is excision of the central nidus (3). Either en-bloc resection or curettage is usually curative (2, 3). In 2002, Sluga et al reported the rate of 12% local recurrence after curettage for peripheral osteoid osteomas and 4.5% after resection (14). Patients presented in the present study population were also managed either with resection or curettage and three (12%) cases recurred. The present study does not include any multicentric osteoid osteomas and recurrence was due to an incomplete excision.
Epidermoid bone cysts are the third common benign hand tumors (1). In more than half of the cases, patients have a previous history of major or minor trauma (8, 15). Eight (80%) tumors in our cases were diagnosed with the distal phalanges. Curettage and bone grafting is curative with low recurrence rates; with only one (10%) case recurred in the present study (1, 8).
Giant cell tumor of the bone is a rare benign hand tumor which can be locally invasive (16, 17). Age of the patient (<40 years), multifocal involvement and higher recurrence rates up to 50% have been previously reported (1, 16, 18). A 50-year Mayo Clinic study reported superior results of resection or ray amputation over curettage as 36% recurrence compared with 79% (19). In 2010, Vergara- Fernandez et al concluded that giant cell tumor resection and bone grafting is a favorable treatment (20). High recurrence rates for giant cell tumor have been repeatedly reported (18, 19, 21, 22). This is believed to be because of an inadequate treatment such as incomplete surgical excision and presentation at advanced stages which complicates the treatment (1, 16, 19, 20, 21). In addition, there is a possibility that tumors at distal radius have higher recurrence rates (21). Our study confirms that simple excision is incomplete in giant cell tumor treatment and it is more important than location of the tumor.
Aneurysmal bone cyst is a rare condition and an optimal treatment has not yet been determined (23, 24). Treatment with curettage and bone grafting has been repeatedly demonstrated with high recurrence rates approaching to 60% (24, 25). However, resection of the tumor followed by autograft reconstruction has been more successful (23, 25). We had recurrence in three (42.9%) of our patients who initially managed with curettage and bone grafting. However, curettage method is not a suitable choice of treatment in this hand tumor. Recently, the role of cryosurgery in local recurrence rate reduction is becoming more prominent (24).
Benign osteoblastoma accounts for 3% of total benign bone tumors with rare occurrence in hand (26). A history of a dull, aching pain, often at rest has been reported (27). All six (100%) cases in our study population presented with a painful mass. Excision of the tumor after diagnosis with a CT-guided biopsy is the recommended choice of treatment (28).
Osteochondroma is a rare benign tumor, occasionally involving the phalanges (29). It is usually a painless slow-growing mass. However, complications such as fracture, bone deformity and mechanical joint problems can cause symptoms (30-32). In cases with clinical symptoms, excision has been suggested as a treatment with low morbidity (33). In the present study, we did not have any patients recurring after sufficient period of follow-up.
Malignant bone tumors of the hand are less prevalent and require more careful preoperative planning with a wider surgical margin to ensure complete removal of the tumor (4, 5). Chondrosarcomas have been previously reported to occur more frequently in the elderly; as our patients were 62 and 68 years of age (5, 34). Osteosarcoma’s peak prevalence is in the second decade of life and our patient was diagnosed at the age of 22 (35). The prognosis of the hand osteosarcoma is better, than for the same lesion located elsewhere. Modern management involves accurate clinical staging and treatment with neoadjuvant chemotherapy combined with a wide resection or amputation followed by adjuvant chemotherapy (35).
One case of Ewing’s sarcoma was also reported. Ewing’s sarcoma of the hand has the same prognosis as other extremity sites (5). It has been stated that because of its rarity in the hand, no standard treatment recommendation exists (36).
We reviewed four cases of metastatic tumors of the hand skeleton. About 0.1% of osseous metastases are found in the hand (5). The most common primary site is the lung, followed by the renal and breast cancers (5, 37). Palliative radiation, amputation and bisphosphonate therapy have been recommended as optional treatments. The metastatic lesion in the hand has a poor prognosis with a median survival of 5 to 6 months (5).
Most osseous tumors of the hand are benign. Often, a precise case history, physical examination, plain radiographs and laboratory examinations are adequate for diagnosis and appropriate treatment. Further diagnostic investigation is recommended if there is any suspicion before excisioinal biopsy or curettage as a definitive diagnostic and therapeutic procedure. If there is any suspicion to malignancy or in some benign situations, incisional biopsy is recommended. A proper diagnostic and surgical plan to osseous tumor of the hand, such as adjunctive treatment or appropriate margin of excision, reduces the risk of recurrence and further surgery.
References
- 1.Hsu CS, Hentz VR, Yao J. Tumours of the hand. Lancet Oncol. 2007;8:157–66. doi: 10.1016/S1470-2045(07)70035-9. [DOI] [PubMed] [Google Scholar]
- 2.Muir JM, Bhandari M, Dunlop RB. Common Primary Tumors of Bone. Can J Diagn. 2001. May, pp. 121–132.
- 3.Payne WT, Greg M. Benign Bony and Soft Tissue Tumors of the Hand. J Hand Surg Am. 2010;35A:1901–1910. doi: 10.1016/j.jhsa.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 4.Frassica FF, Amadio PC, Wold LE, Dobyns JH. Primary malignant bone tumors of the hand. J Hand Surg Am. 1989;14A:1022–8. doi: 10.1016/s0363-5023(89)80054-1. [DOI] [PubMed] [Google Scholar]
- 5.Puhaindran ME, Athanasian EA. Malignant and Metastatic Tumors of the Hand. J Hand Surg Am. 2010;35A:1895–1900. doi: 10.1016/j.jhsa.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Conolly WB, Loon JV. Tumors of the Hand. J R Soc Med. 2004;97:606. [Google Scholar]
- 7.Figl M, Leixnering M. Retrospective review of outcome after surgical treatment of enchondromas in the hand. Arch Orthop Trauma Surg. 2009;129:729–734. doi: 10.1007/s00402-008-0715-6. [DOI] [PubMed] [Google Scholar]
- 8.Butler ED, Hamill JP, Seipel RS, Lorimier AA. Tumors of the Hand, A Ten Year Survey and Report of 437 Cases. Am J Surg. 1960;100:293–302. doi: 10.1016/0002-9610(60)90302-0. [DOI] [PubMed] [Google Scholar]
- 9.Kim CH. Enchondroma of the Lunate. Arch Plast Surg. 2012;39(6 ):678–680. doi: 10.5999/aps.2012.39.6.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jafari D, Shariatzadeh H, Najd Mazhar F, Ghahremani MH, Jalili A. Enchondroma of the hand: the role of biopsy in the course of diagnosis and treatment. Med J Islam Repub Iran. 2011;25(3 ):127–30. [Google Scholar]
- 11.Shaikh S, Lombay B. Osteoid osteoma: diagnosis and treatment. Magy Radiol. 2008;82:16–24. [Google Scholar]
- 12.Kitsoulis P, Mantellos G, Vlychouv m. Osteoid osteoma. Acta Orthop Belg. 2006;72:119–125. [PubMed] [Google Scholar]
- 13.Jafari D, Najd Mazhar F. Osteoid Osteoma of the Trapezoid Bone. Arch Iranian Med. 2012;15(12 ):777–9. [PubMed] [Google Scholar]
- 14.Sluga M, Windhager R, Pfeiffer M, Dominkus M, Kotz R. Peripheral osteoid osteoma, Is there still a place for traditional surgery? J Bone Joint surg. 2002;84(2 ):249–51. doi: 10.1302/0301-620x.84b2.12347. [DOI] [PubMed] [Google Scholar]
- 15.Stack HG. Tumours of the hand. Br Med J. 1960. Mar, pp. 919–22. [DOI] [PMC free article] [PubMed]
- 16.Biscaglia R, Bacchini P, Bertoni F. Giant Cell Tumor of the Bones of the Hand and Foot. Cancer. 2000;88(9 ):2022–32. doi: 10.1002/(sici)1097-0142(20000501)88:9<2022::aid-cncr6>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 17.Haque AU, Moatasim A. Giant Cell Tumor of Bone: A Neoplasm or a Reactive Condition? Int J Clin Exp Pathol. 2008;1:489–501. [PMC free article] [PubMed] [Google Scholar]
- 18.Sanfilippo AM, Kulenovic E. Giant Cell Tumor. Appl Radiol. 2008;00:37–9. [Google Scholar]
- 19.Wittig JC, Simpson BM, Bickels J, Kellar-Graney KL, Malawer MM. Giant Cell Tumor of the Hand: Superior Results With Curettage, Cryosurgery, and Cementation. J Hand Surg Am. 2001;26A:546–55. doi: 10.1053/jhsu.2001.22525. [DOI] [PubMed] [Google Scholar]
- 20.Vergara-Fernandez HJ, Ortiz-Arellano D, Martinez-Hernandez B, Mosinoz R, Arellano J. Hand reconstructive surgery secondary to giant cell tumor. Acta Ortop Mex. 2010;24:343–8. [PubMed] [Google Scholar]
- 21.Harness NG, Mankin HJ. Giant-Cell Tumor of the Distal Forearm. J Hand Surg Am. 2004;29A:188–93. doi: 10.1016/j.jhsa.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Suresh SS, Zaki H. Giant Cell Tumor of Tendon Sheath: Case Series and Review of Literature. J Hand Microsurg. 2010;2:67–71. doi: 10.1007/s12593-010-0020-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jafari D, Jamshidi K, Najd mazhar F, Shariatzade H, Liaghat O. Expansile aneurysmal bone cyst in the tubular bones of the hand treated with en bloc excision and autograft reconstruction: a report of 12 cases. J Hand Surg Am. 2011;36:648–55. doi: 10.1177/1753193411420033. [DOI] [PubMed] [Google Scholar]
- 24.Athanasian EA, McCormack RR. Recurrent Aneurysmal Bone Cyst of the Proximal Phalanx Treated With Cryosurgery: A Case Report. J Hand Surg Am. 1999;24A:405–12. doi: 10.1053/jhsu.1999.0405. [DOI] [PubMed] [Google Scholar]
- 25.Frassica FJ, Amadio PC, Wold LE, Beabout JW, Rochester M. Aneurysmal bone cyst: Clinicopathologic features and treatment of ten cases involving the hand. J Hand Surg Am. 1988;13A:676–83. doi: 10.1016/s0363-5023(88)80122-9. [DOI] [PubMed] [Google Scholar]
- 26.Lichtenstein L, Sawyer WR. Benign Osteoblastoma Further Observations and Report of Twenty Additional Cases. J Bone Joint Surg. 1964;46:755–65. [PubMed] [Google Scholar]
- 27.Giffen NV, Smet LD. Osteoblastoma of the proximal ulna, an unusual cause of ulnar wrist pain. A case report. Acta Orthop Belg. 2005;71:736–9. [PubMed] [Google Scholar]
- 28.Bahouq H, Allali F, Hajjaj-Hassouni N. Osteoblastoma of scaphoid of the carpus: a case report. Pan Afr Med J. 2011;8:39. doi: 10.4314/pamj.v8i1.71154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carroll R. Epidermal (Epithelial) Cysts of the hand skeleton. Am J Surg. 1953;85:327. doi: 10.1016/0002-9610(53)90617-5. [DOI] [PubMed] [Google Scholar]
- 30.Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: Review of the Clinical, Radiological and Pathological Features. In vivo. 2008;22:633–46. [PubMed] [Google Scholar]
- 31.Saglik Y, Altay M, Unal VS, Basarir K, Yildi Y. Manifestations and management of osteochondromas : A retrospective analysis of 382 patients. Acta Orthop Belg. 2006;72:748–55. [PubMed] [Google Scholar]
- 32.Schnirring-Judge M, Visser J. Resection and Reconstruction of an Osteochondroma of the Hallux: A Review of Benign Bone Tumors and a Description of an Unusual Case. J Foot Ankle Surg. 2009;48:495–505. doi: 10.1053/j.jfas.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Bottner F, Rodl R, Kordish I, Winklemann W, Gosheger G, Lindner N. Surgical treatment of symptomatic osteochondroma A three to eight year follow-up study. J Bone Joint Surg Br. 2003;85:1161–5. doi: 10.1302/0301-620x.85b8.14059. [DOI] [PubMed] [Google Scholar]
- 34.Roberts PH, Price CHG. Chondrosarcoma of the Bones of the Hand. J Bone Joint Surg Br. 1977;59:213–21. doi: 10.1302/0301-620X.59B2.873982. [DOI] [PubMed] [Google Scholar]
- 35.Gibbs JCP, Weber K, Scarborough MT. Malignant Bone Tumors. Instr Course Lect. 2005;51:413–28. [PubMed] [Google Scholar]
- 36.Sforzo CR, Scarborough MT, Wright TW. Bone-forming tumors of the upper extremity and Ewing's Sarcoma. Hand Clin. 2004;20:303–15. doi: 10.1016/j.hcl.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 37.Kumar PP, Kovi J. Metastases to Bones of the Hands and Feet. J Natl Med Assoc. 1978;70:837–40. [PMC free article] [PubMed] [Google Scholar]