Abstract
Background:
Trans-scaphoid perilunate fracture-dislocation and perilunate dislocations are among uncommon injuries, most commonly seen in young patients due to high energy trauma. The treatment can be achieved either surgically by open reduction and internal fixation or closed reduction and casting.
Methods:
To compare surgical versus non-operative results of treatment after trans-scaphoid perilunate fracture-dislocation and isolated perilunate dislocation, we collected the data of 34 patients who were treated at least 5 years before our study, twenty of whom were treated surgically and fourteen were treated non-surgically. We compared clinical and radiological findings in two groups. Functional outcome was assessed by Mayo wrist score for each patient.
Results:
The surgically treated patients had much higher Mayo wrist scores, 85 and 87.78 for perilunate dislocation and trans-scaphoid perilunate fracture-dislocation respectively, while 71 and 71.11 in non-surgically treated group respectively. Wrist range of motion was also more favorable in operative group (55 degrees flexion - 54 degrees extension for trans-scaphoid perilunate fracture-dislocation and 50 degrees flexion, 51 degrees extension for perilunate dislocations)than non-operative group(49 degrees flexion, 48 extension for trans-scaphoid fracture-dislocations and 48 degrees flexion, 50 degrees extension for perilunate dislocation). The radiographic changes showed arthritic changes but those changes did not significantly interfered with functional outcome and wrist scores.
Conclusion:
Regarding our better clinical results after early open reduction and internal fixation for these injuries, we can suggest the operative treatment of these complicated hand injuries.
Keywords: Hand surgery, Non-operative treatment, Open reduction and internal fixation, Perilunate dislocations, Trans-scaphoid fracture-dislocation
Introduction
Perilunate dislocations and trans-scaphoid perilunate fracture-dislocations are among uncommon orthopedic injuries that occur most often in young individuals following high energy trauma (1-6). Although perilunate injuries are rare, but might be easily left undiagnosed in the emergency setting (7, 8). After establishment of the diagnosis, the early closed reduction is performed in the emergency operative room. Surgical and non- operative treatment options have been practiced and have their own supporters as many orthopedic surgeons perform early open reduction and internal fixation and some others prefer casting after closed reduction (1-3).
Various data with wide range of different results exist such as post traumatic arthritis which has been reported to be as high as 36% (7-92%). This reminds us the need of more studies to be done on the subject (4).
The purpose of this study was to compare the clinical results of operative and non-operative treatments in a mid-term follow up and subsequently determining the better choice of treatment for these injuries.
Materials and Methods
In a retrospective study, 34 patients accepted our invitation to enroll in the study who were previously admitted to Imam-Reza and Shahid-Kamyab referral hospitals of Mashhad University of Medical Sciences, Mashhad, Iran with the diagnosis of perilunate dislocation or trans-scaphoid perilunate fracture dislocations (Figure 1). The study was approved by the Ethical Committee of Research at Mashhad University of Medical sciences. All patients were informed of being enrolled in a medical research and they willingly took part in the study. Twenty patients were treated with early open reduction and internal fixation by two senior orthopedic surgeons (FB and HRS) and 14 were treated non-operatively by closed reduction and long arm cast in emergency room. Patients’ charts were reviewed and pre and post operation radiographies were studied. Patients were examined to determine the wrist range of motion and grip strength. To evaluate the extent of joint degenerative changes, AP and lateral radiographs were obtained of all the patients.
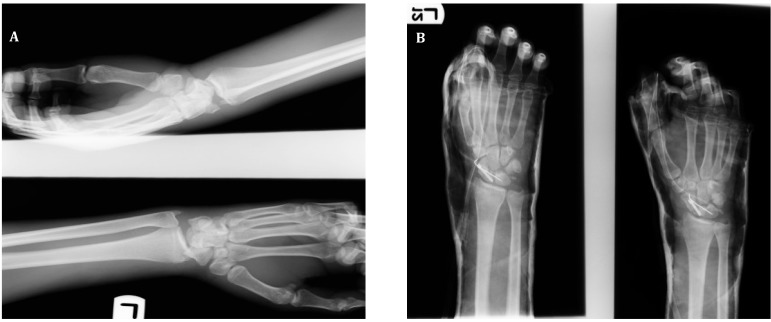
Figure 1.
preoperative(A) and post operative(B) radiography of a 21- year old man with trans-scaphoid perilunate fracture dislocation of the left wrist.
Mayo Wrist Scoree was filled out for every patient. According to this score, patients were categorized into 4 groups as excellent (90-100), good (80-89), fair (60-79), and poor (less than 60). Grip strength was evaluated by a hand dynamometer. We used SPSS 11.5 (SPSS Inc., Chicago, IL) for our database and for statistical analysis.
Results
Among 20 surgically treated patients, 14 had suffered a trans-scaphoid perilunate fracture dislocation and 6 had perilunate dislocation. In 14 non-surgically treated patients, there were 9 trans-scaphoid perilunate fracture dislocations and 5 perilunate dislocations. All the patients were male. The mean age was 27 years (range from 17 to 49 years). Twenty- seven patients were right handed (79%) and 7 patients were left handed (21%). Dominant hand injuries accounted for 31 cases (91%). The mean follow-up period was 67 months (range from 60 to 96months).
Of six patients with perilunate dislocations who were treated surgically, according to Mayo wrist score, there were 3 excellent, 2 good, 1 fair and 1 poor on the last follow-up visit. The mean Mayo wrist score was 85 (Table 1). The mean duration of follow-up in this group was 62.4 months and the mean age of patients was 28 years. Patients didn’t report any consistent pain but occasional pain was reported in 2 patients (33%) and 4 patients (67%) were totally pain free.
Table 1.
Summary of the result of surgical group versus non-surgical group
| Surgically treated | Non surgically treated | |||
|---|---|---|---|---|
| TSPD* | PD** | TSPD | PD | |
| Number of patients | 14(41%) | 6(18%) | 9(26%) | 5(15%) |
| Mean Mayo Wrist Score | 88 | 85 | 71 | 71 |
| Flexion | 55 | 50 | 49 | 49 |
| Extension | 54 | 51.66 | 48 | 50 |
| Degenerative change | 4(11%) | 3(9%) | 3(9%) | 2(6%) |
Trans-scaphoid perilunate dislocation
perilunate dislocation
Fourteen trans-scaphoid perilunate fracture-dislocation patients (70%) which were treated surgically, had 9 excellent, 1 good, 2 fair, and 2 bad results according to Mayo wrist score. The mean Mayo wrist score was 88. The mean duration of follow- up was 65 months and the mean age of the patients was 26 years. Occasional pain was reported in 6 patients (43%), exertional wrist pain in 2 patients (14%) and 6 patients were pain free (43%).
Fourteen Patients were treated non-operatively with closed reduction and casting.Of these 14 patients, 9 were with a trans-scaphoid perilunate fracture-dislocation and 5 were with perilunate dislocation. Among nine fracture dislocations, 2 patients reported excellent results, 2 good, 2 fair and 3 poor according to Mayo wrist score.Mean Mayo wrist score was 71, mean follow-up duration was 69 months and mean age of patients was 27 years.
In six patients with perilunate dislocation who were treated non surgically, we found 1 excellent, 1 good, 2 fair and 1 poor results and the mean Mayo wrist score was 71. The mean follow-up duration was 70 months and mean age of these patients was 27 years. The range of motion results in each group is shown in Table 1.
Based on Herzburge radiographic wrist osteoarthritis classification, osteoarthritis existed in 35% of patients in grade A and A1 and no evidence of grade B and C. There was no difference either in surgical versus non surgical group or also in perilunate dislocation versus trans-scaphoid perilunate dislocation group for degenerative changes. Grip power was measured and compared with the other side and there was not a significant difference between the groups (P≥0.05)(Figure 2).
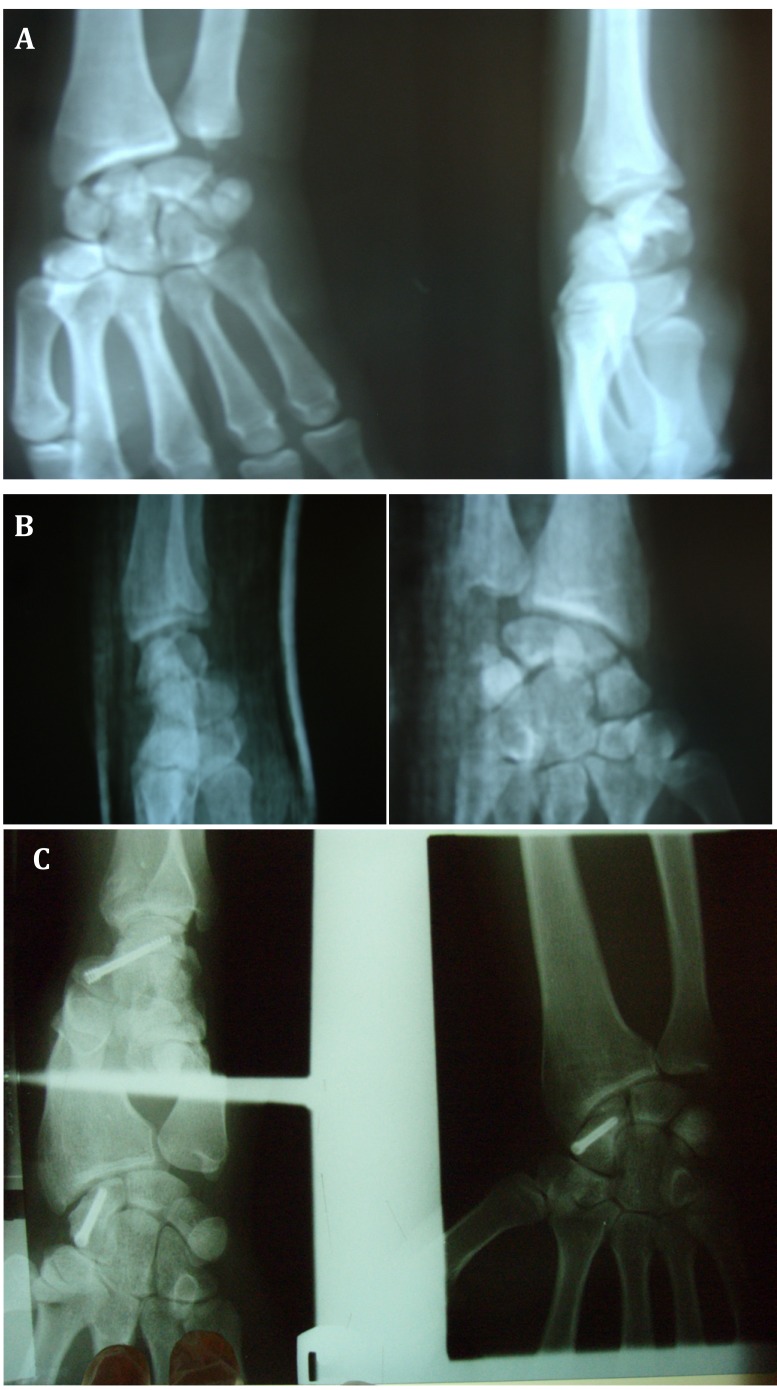
Figure 2.
A. Trans-scaphoid prelunate fracture-dislocation in a 37-year old man due to falling.
B. Anteroposterior and lateral wrist radiography after non successful closed reduction and casting.
C. Follow up radiograghy one year after open reduction and internal fixation, shows complete union and degenerative changes ( Herzburg classification type A ), clinically he had full wrist ROM and no obvious disability.
Discussion
As many topics in orthopedic trauma, there is still ongoing controversy regarding the surgical or non-surgical treatment for trans-scaphoid perilunate fracture-dislocations and perilunate dislocations. In this retrospective study we evaluated the clinical and functional outcome after surgical and non- surgical treatment of trans-scaphoid and isolated perilunate dislocation to determine which brings superior long-term outcomes
Most of previous studies on this subject had conducted short term follow-ups(less than 5 years after treatment) and there are some with longer follow-up durations with mean duration of 2 to 8 years (5, 6). Our study group had passed at least 5 years after treatment. The main problem we faced with, was the small number of our series which was due to the scarcity of the injury in comparison with other hand and wrist injuries (9, 10). Despite the few number of patients in trans-scaphoid perilunate fracture-dislocation and perilunate dislocation groups, our results can suggest almost the same clinical and radiologic results in both groups. The mean Mayo wrist score (65-80) in our study was comparable to other studies. The Mayo wrist score was higher in surgically treated patients (11-13).
The wrist arc of motion was 107 degrees in surgically treated group and 102 degrees in non-surgical group which we believe is due to the earlier rehabilitation and shorter immobilization period.
Degenerative joint changes in the current study accounted 35% that was less than previous studies (50-56%), which we assume is because of the longer follow-up periods in those studies. In this study there was no difference in the end results of two groups so we can conclude that the surgical procedure does not increase the rate of degenerative changes (14-16).
Herzberg reported the occurrence of radio carpal or midcarpal arthritis after 8 years in nearly all patients. But, as he implicated there seems not to be a strong relationship between the clinical function and radiographic changes (3, 11).
Among factors which might impair the wrist function after these injuries is carpal instability, scaphoid non union, and carpal malalignment. All of these with their consequent outcomes make it wise to choose surgery for open reduction and internal fixation. Our findings support this hypothesis that surgically treated patients had much higher Mayo wrist scores and their wrist function was much better reserved than non-surgically treated patients.
References
- 1.Apergis E, Maris J, Theodoratos G, Pavlakis D, Antoniou N. Perilunate dislocations and fracture-dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand Suppl. 1997;275:55–9. [PubMed] [Google Scholar]
- 2.Herzberg G, Comtet JJ, Linscheid RL, Amadio PC, Cooney WP, Stalder J. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg. 1993;18(5): 768–79. doi: 10.1016/0363-5023(93)90041-Z. [DOI] [PubMed] [Google Scholar]
- 3.Su CJ, Chang MC, Liu Y, Lo WH. Lunate and perilunate dislocation. Zhonghua Yi Xue Za Zhi (Taipei) 1996;58:348–54. [PubMed] [Google Scholar]
- 4.Adkison JW, Chapman MW. Treatment of acute lunate and perilunate dislocations. Clin Orthop Relat Res. 1982. pp. 199–207. [PubMed]
- 5.Martinage A, Balaguer T, Chignon-Sicard B, Moteil MC, Dreant N, Leberton E. Perilunate dislocations and fractue-dislocations of the wrist, a review of 14 cases [in French] Cseyhir Main. 2008;27:31–9. doi: 10.1016/j.main.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Cooney WP, Bussey R, Dobyns JH, Llinsch RL. Difficult wrist fractures. Perilunate fractue-dislocations of the wrist. Clin Orthop Relat Res. 1987. pp. 136–47. [PubMed]
- 7.Massoud AH, Naam NH. Functional outcome of open reduction of chronic perilunate injuries. J Hand Surg Am. 2012;37(9 ):1852–60. doi: 10.1016/j.jhsa.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Garg B, Goyal T, Kotwal PP. Staged reduction of neglected transscaphoid perilunate fracture dislocation. a report of 16 cases. J Orthop Surg Res. 2012;7:19. doi: 10.1186/1749-799X-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altissimi M, Mancici GB, Azzara A. Perilunate dislocations of the carpus: A long-term review. Italy J Orthop-Traumatol. 1987;13:491–500. [PubMed] [Google Scholar]
- 10.Pai CH, Wei DC, Hu ST. Carpal bone dislocations: an analysis of twenty cases with relative emphasis on the role of crushing mechanisms. J Trauma. 1993;35:28–35. [PubMed] [Google Scholar]
- 11.Herzber G, Forissier D. Acute dorsal trans-scaphoid fractue-dislocations: medium-term results. J Hand Surg Br. 2002;27(6):498–502. doi: 10.1054/jhsb.2002.0774. [DOI] [PubMed] [Google Scholar]
- 12.Komurku M, Kurklu M, Ozturan KE, Mahirogullari M, Basbozhurt M. Early and delayed treatment of doral transscaphoid perilunate fracture-dislocations. J Orthop Trauma. 2008;22:535–40. doi: 10.1097/BOT.0b013e318183eb23. [DOI] [PubMed] [Google Scholar]
- 13.Souer JS, Rutgers M, Andermahr J, Jupiter JB, Ring D. Perilunate fractue-dislocations of the wrist: comparison of temporary screw versus K-wire fixation. J Hand Surg. 2007;32(3):318–25. doi: 10.1016/j.jhsa.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Knoll VD, Allan C, Trunble TE. Transscaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid one lunotriquetral repair with a dorsal approach. J Hand Surg. 2005;30(6):1145–52. doi: 10.1016/j.jhsa.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Hildebrand KA, Ross DC, Patterson SD, Roth JH, MacDermid JC, King GJ. Dorsal perilunate dislocations and fractue-dislocations: questionnaire, clinical, and radiographic evaluation. J hand Surg. 2000;25(6):1069–79. doi: 10.1053/jhsu.2000.17868. [DOI] [PubMed] [Google Scholar]
- 16.Sotereanos DG, Mitsionis GJ, Giannakopoulos PN, Tomaino MM, Herndon JH. Perilunate dislocation and fractue-dislocation: a critical analysis of the volar-dorsal approach. J Hana Surg. 1997;22(1):49–54. doi: 10.1016/S0363-5023(05)80179-0. [DOI] [PubMed] [Google Scholar]