Abstract
Background:
Although the majority of soft tissue masses are benign, it is important to consider malignancy in differential diagnoses. Because most soft tissue sarcomas present as a painless mass, clinicians must watch for signs suggestive of malignancy, including large size, rapid growth, and site deep into the deep fascia.
The purpose of this study was to determine the relative prevalence according to sex and age, site of tumor, skeletal distribution, and treatment (surgery, chemotherapy and radiotherapy) before and after surgery, and ascertain the relative frequency of these tumors in specific anatomic sites and age groups based on pathological studies.
Methods:
A total of 308 patients, with a musculoskeletal tumor were evaluated retrospectively. All of the patients enrolled into this study were referred to the Beirouni Hospital of Damascus University with a proven diagnosis of malignant soft tissue tumors from the beginning of January 2008 until the end of 2010.
The prevalence of the malignant soft tissue tumors in these patients was analyzed. For purposes of analysis, all lesions were placed in 1 of 9 categories: hand and wrist, forearm, humorous (arm), proximal limb girdle (axilla and shoulder), foot and ankle, thigh, hip and buttocks region, trunk, and other lesions. Age and sex also were recorded.
Results:
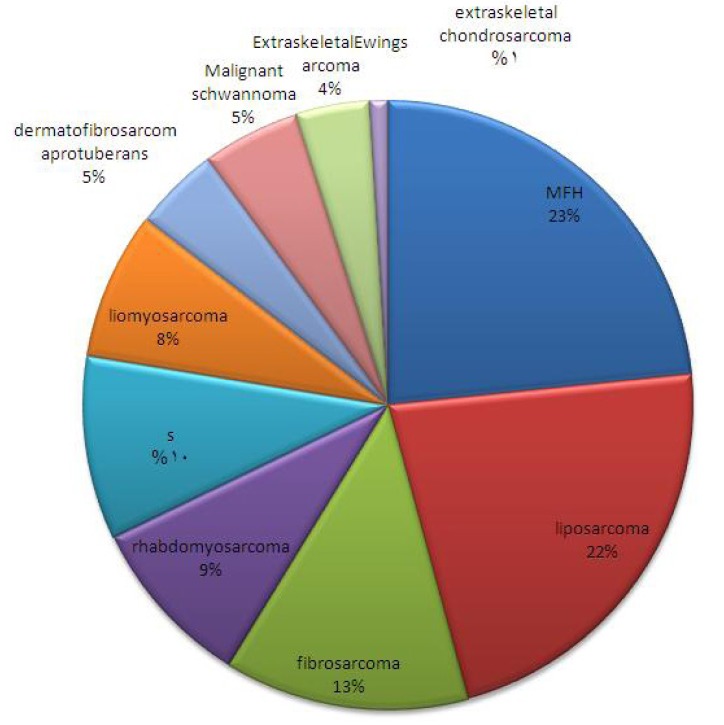
Malignant tumors consisted of seven diagnostic categories: malignant fibrous histiocytoma (23%), liposarcoma (22%), rhabdomyosarcoma (9%), leiomyosarcoma (8%), malignant schwannoma (5%), dermatofibrosarcoma protuberans (5%), synovial sarcoma (10%), fibrosarcoma (13%), extraskeletal chondrosarcoma (1%), and extraskeletal Ewing sarcoma (4%).
Conclusions:
Despite the multitude of pathologic possibilities, most malignant soft-tissue tumors are classified into a small number of diagnoses. These may be further defined when the site of the lesion and the age of the patient are considered. Knowledge of tumor prevalence will assist radiologists in establishing a suitably ordered differential diagnosis when a soft-tissue tumor has a nonspecific radiologic appearance.
Key words: Oncology, Sarcoma, Syria
Introduction
Malignant soft tissue tumors, or soft tissue sarcomas, are more common than bone sarcomas. About 8,000 new tumor cases occur each year in the United States, which represents only about 1% of all malignant tumors (1). They usually occur in adults and present as a large painless or painful soft tissue mass. Because benign soft tissue “lumps” are far more common than malignant ones, the diagnosis of a soft tissue sarcoma may be made after excision of a presumed benign mass at a local hospital or in the doctor’s office.
Soft tissue tumors are also classified by their tissue type and grade. Thus, the higher the grade, the greater the chance for aggressive growth at the original site, and this is true for metastases, at distant sites.
Staging a soft tissue tumor involves evaluating the histology (tissue grade) of the tumor, how extensive the tumor is at the primary site, and whether or not there are distant metastases. All of these characteristics help describe the tumor’s behavior (biologic activity), the patient’s prognosis, and the best treatment option.
MRI scanning is the best imaging study for soft tissue tumors because of its sensitivity in showing differences between normal and sarcoma tissue. It also clearly shows the relation of the tumor to nearby nerves and blood vessels. Moreover, a chest CT scan is always necessary to rule out lung metastases and a biopsy is done to determine diagnosis.
Soft tissue sarcomas that develop in the limbs and the axial area, even those that are diagnosed early using appropriate methods and are treated adequately, have a 5-year survival rate of between 62 and 84% (2, 3).
Materials and Methods
Of 378 patients with a diagnosis of malignant soft tissue sarcoma of the limb treated at Beirouni Hospital between 2008 to the end of 2010, we studied 308 cases based on our inclusion criteria and 70 cases were excluded.
Malignant soft tissue sarcoma was diagnosed based on entries in final pathology reports. Mesenchymal lesions that originated in soft tissue were included in the study.
The characteristics of the 308 cases of malignant soft tissue sarcoma were analyzed based on tumor types determined at final diagnosis, the anatomical locations of tumors in limbs, for purposes of analyzing all lesions were placed in 1 of 9 categories: hand and wrist, forearm, humorous, proximal limb girdle (axilla and shoulder), foot and ankle, hip and buttocks region, thigh, trunk, and other lesions.
Malignant tumors were classified into seven diagnostic categories: malignant fibrous histiocytoma, liposarcoma, rhabdomyosarcoma, leiomyosarcoma, malignant schwannoma, dermatofibrosarcoma protuberans, synovial sarcoma, fibrosarcoma, extraskeletal chondrosarcoma and others.
Then the patients based on tumor type were grouped into the following age groups: 1-9 years, 10-19 years, 20-29 years, 30-39 years, 40-49 years, 50-59 years, 60- 69 years and above 70 years old. In addition, patient`s sex and place of living were recorded. Beirouni Hospital of Damascus University is the largest referral center for malignancies in Syria and the study was approved by research committee of our institution.
The treatment method of patients in the study was grouped into the following groups: neoadjuvant chemotherapy, adjuvant chemotherapy, neoadjuvant radiotherapy, adjuvant radiotherapy, wide resection surgery, radical surgery, amputations and no treatment.
Results
In this group of 308 cases, 143 (45%) were males and 175 (55%) were females, with a male:female ratio of 0.8:1. The distribution of cases was as follows: malignant fibrous histiocytoma (23%), liposarcoma (22%), rhabdomyosarcoma (9%), leiomyosarcoma (8%), malignant schwannoma (5%), dermatofibrosarcoma protuberans (5%), synovial sarcoma (10%), fibrosarcoma (13%), extraskeletal chondrosarcoma (1%), and extraskeletal Ewing sarcoma (4%) (Figure 1).
Figure 1.
Distribution of cases based on type of tumors.
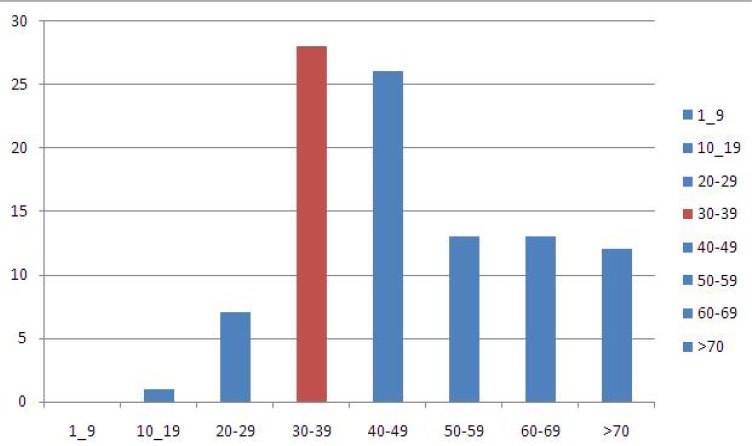
The frequency of cases with soft tissue sarcomas based on age was as follows: 1-9 years: 9 (3%) cases; 10-19 years: 31 (10%) cases; 20-29 years: 49 (16%) cases; 30- 39 years: 58 (19%) cases; 40-49 years: 55 (18%); 50-59 years: 50 (16%) cases; 60-69 years: 31cases (10%) and more than 70 years: 24 cases (8%) (Figure 2).
Figure 2.
Frequency of cases with soft tissue sarcomas based on age.
Malignant fibrous histiocytoma was the most frequent tumors and frequently occurred in patients > 40 years old (Table 1 and Figure 3), while 46% of fibrosarcoma cases involved adults between 40 and 60 years of age (Figure 4).
Table 1.
Frequency of malignant fibrous histiocytoma based on age
| Percent | Frequency | MFH |
|---|---|---|
| 0 | 0 | 9-9 |
| 7 | 5 | 19-10 |
| 18 | 13 | 29-20 |
| 10 | 7 | 39-30 |
| 18 | 13 | 49-40 |
| 18 | 13 | 59-50 |
| 18 | 13 | 69-60 |
| 11 | 8 | <70 |
| 100 | 72 |
Figure 3.
Frequency of malignant fibrous histiocytoma based on age.
Figure 4.
Frequency of fibrosarcoma based on age.
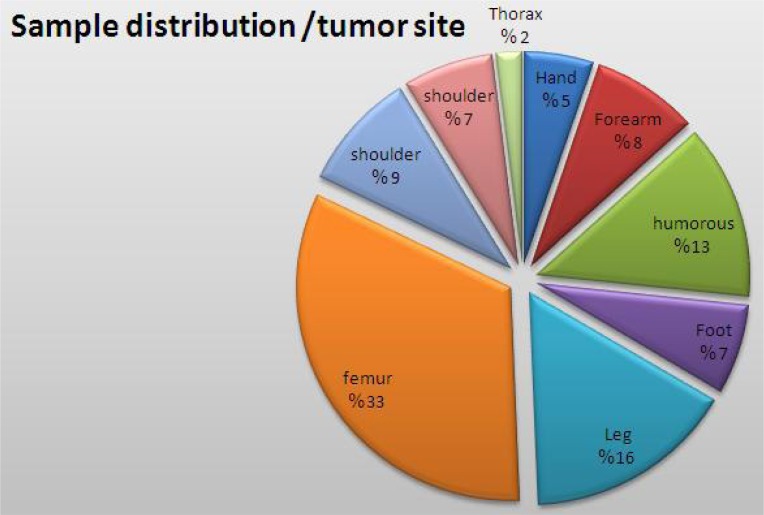
Of the 308 cases of soft tissue sarcomas, the tumor was observed involving every part of the body as follows: hand and wrist: 16 cases (5%); forearm: 25 cases (8%); humerus: 41 cases (13%); proximal limb girdle (axilla and shoulder): 28 cases (9%); foot and ankle: 21 cases (7%); leg: 49 cases (16%); hip and buttocks region: 21 cases (7%); femur:101 cases (33%); and the trunk: 6 cases (2%) (Figure 5).
Figure 5.
Distribution of tumors based on every part of the body.
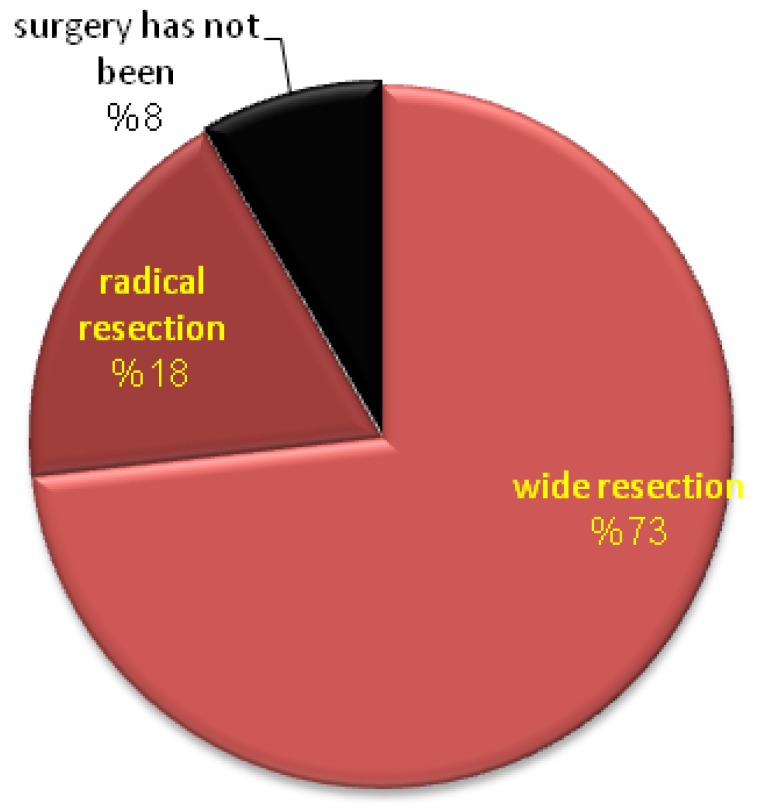
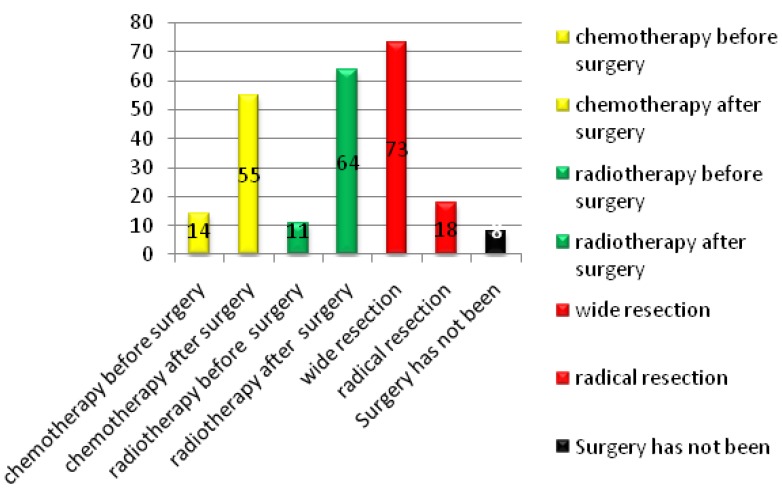
Wide resection was performed in most cases, which is the preferred treatment in most cancer referral centers to salvage the limb. Radical resection was performed in a few cases that were mostly malignant fibrous histiocytoma (MFH). Most studies have focused on survival after surgical treatment and chemoradiotherapy, which is the most important and perhaps only indicator for evaluation of treatment modalities. Surgery was performed in 92% of cases and wide resection was used for 73% of patients (Figure 6).
Figure 6.
Distribution of cases based on surgical techniques ratio/ %.
Fourteen percent of patients undergoing neoadjuvant chemotherapy and adjuvant chemotherapy were performed in 55% of patients. Radiotherapy was performed in 11% of cases before surgery and 64% after surgery (Figure 7).
Figure 7.
Distribution of cases based on how to treatment.
Discussion
In this study, we calculated population-based incidence rates of soft tissue. This report is the largest study of soft tissue tumors in the Syrian population to date. We used the recent 2002 WHO criteria to define histological subtypes of soft tissue sarcoma and included all cases, regardless of site of origin except bones and joints. This approach provided a valuable opportunity to determine accurate and clinically applicable incidence rates by histological type and subtypes.
By comparing the result of different studies, the most common soft tissue tumor was MFH. In 2002, WHO declassified MFH as a formal diagnostic entity and renamed it as an undifferentiated pleomorphic sarcoma as the most common followed by liposarcoma. Other similar results have been obtained in other studies (4). Also, Gustafson al. reported that MFH and grade IV were the most common soft tissue tumor (5). Similarly the most common soft tissue tumor was MFH in our patients (Figure 1).
However, in another study conducted by Toro et al, the most common soft tissue tumor was leiomyosarcoma (23.9%) (6).
In our series, female prevalence (55%) was slightly higher, which is consistent with most previous studies, although some previous studies reported higher incidence in males (1,4,5,7-11). Thus with this inconsistency in the results of different studies, no clear trend in gender predilection can be stated.
Age-specific rates for all soft tissue tumors were elevated by increased age (especially between 30-59 years). The peak incidence was about 30-39 years, with marginal decreases in 40-49 years. Gustafson et al. reported that the median age was 64 years (5). Wibmer et al. found that the highest peak was around the age of 60 years (7). The most common anatomic site of involvement was the thigh (33%), followed by the leg and arm.
The main surgical procedure in most cases was wide local excision (margins of at least 1 cm).
Radical excisions were applied to the small number of patients and the majority of those cases were MFH. For 8% of the patients surgery was not performed due to the patient’s refusal of surgery or poor medical conditions.
References
- 1.Kransdorf MJ. Malignant soft-tissue tumors in a large referral population: distribution of diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164(1):129–34. doi: 10.2214/ajr.164.1.7998525. [DOI] [PubMed] [Google Scholar]
- 2.Noria A, Davis A, Kandlel R, Levesque J, O’Sullivan B, Wunder J, et al. Residual disease following unplanned excision of soft tissue sarcoma of an extremity. J Bone Joint Surg Am. 1996;78(5 ):650–5. doi: 10.2106/00004623-199605000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Simon MA, Enneking WF. The management of softtissue sarcomas of theextremities. Ann Surg. 1982;196(3):305–15. [Google Scholar]
- 4.Rosenthal TC, Kraybill W. Soft Tissue Sarcomas: Integrating Primary Care Recognition with Tertiary Care Center Treatment. Am Fam Physician. 1999;60(2 ):567–72. [PubMed] [Google Scholar]
- 5.Gustafson P. Soft tissue sarcoma. Epidemiology and prognosis in 508 patients. Acta Orthop Scand Suppl. 1994;259:1–31. [PubMed] [Google Scholar]
- 6.Toro JR, Travis LB, Wu HJ, Zhu K, Fletcher CD, Devesa SS. Incidence patterns of soft tissue sarcomas, regardless of primary site, in the surveillance, epidemiology and end results program, 1978-2001: An analysis of 26,758 cases. Int J Cancer. 2006;119(12 ):2922–30. doi: 10.1002/ijc.22239. [DOI] [PubMed] [Google Scholar]
- 7.Wibmer C, Leithner A, Zielonke N, Sperl M, Windhager R. Increasing incidence rates of soft tissue sarcomas? A population based epidemiologic study and literature review. Ann Oncol. 2010;21(5 ):1106–11. doi: 10.1093/annonc/mdp415. [DOI] [PubMed] [Google Scholar]
- 8.Ross JA, Severson RK, Davis S, Brooks JJ. Trends in the incidence of soft tissue sarcomas in the United States from 1973 through 1987. Cancer. 1993;72(2 ):486–90. doi: 10.1002/1097-0142(19930715)72:2<486::aid-cncr2820720226>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 9.Levi F, La Vecchia C, Randimbison L, Te VC. Descriptive epidemiology of soft tissue sarcomas in Vaud, Switzerland. Eur J Cancer. 1999;35(12 ):1711–6. doi: 10.1016/s0959-8049(99)00179-3. [DOI] [PubMed] [Google Scholar]
- 10.Storm HH. Cancers of the soft tissues. Cancer Surv. 1993;19:197–217. [PubMed] [Google Scholar]
- 11.Zahm SH, Fraumeni JF., Jr The epidemiology of soft tissue sarcoma. Semin Oncol. 1997;24(5 ):504–14. [PubMed] [Google Scholar]