Abstract
Around the world, members of racial/ethnic minority groups typically experience poorer health than members of racial/ethnic majority groups. The core premise of this article is that thoughts, feelings, and behaviors related to race and ethnicity play a critical role in healthcare disparities. Social psychological theories of the origins and consequences of these thoughts, feelings, and behaviors offer critical insights into the processes responsible for these disparities and suggest interventions to address them. We present a multilevel model that explains how societal, intrapersonal, and interpersonal factors can influence ethnic/racial health disparities. We focus our literature review, including our own research, and conceptual analysis at the intrapersonal (the race-related thoughts and feelings of minority patients and non-minority physicians) and interpersonal levels (intergroup processes that affect medical interactions between minority patients and non-minority physicians). At both levels of analysis, we use theories of social categorization, social identity, contemporary forms of racial bias, stereotype activation, stigma, and other social psychological processes to identify and understand potential causes and processes of health and healthcare disparities. In the final section, we identify theory-based interventions that might reduce ethnic/racial disparities in health and healthcare.
Keywords: ethnicity/race, health and healthcare, disparities, explicit and implicit bias, intergroup processes
Across a broad spectrum of mental and physical illnesses, members of socially disadvantaged groups typically experience poorer physical and mental health than members of socially advantaged groups. This is a persistent social problem in at least 126 countries, which include 94.4% of the world’s population (Dorling, Mitchell, & Pearce, 2007). There are two general classes of explanations of this pervasive public health problem. The first is that these differences reflect biological and genetic differences in the populations to which the different groups belong. Given that biology and genes clearly play important roles in people’s mental and physical health (Chase, (2012; Vogelstein, & Kinzler, 2002), there is certainly some merit to this explanation. The second explanation is that the differences reflect a social problem, health disparities. Health disparities (or inequalities) refer to systematic variations in the mental or physical well-being of members of different social groups that specifically result from inequitable economic, political, social, and psychological processes (Braveman, 2006). This article only considers health disparities. However, these two kinds of explanations are not mutually exclusive; indeed, recent research strongly suggests that genetic and social factors have a reciprocal relationship as they affect health and a host of other outcomes (e.g., Cole, 2009).
One influential contributor to health status disparities is healthcare disparities, which are inequalities in access to and/or the quality of medical care among different social groups. In other words, it is posited that members of socially disadvantaged groups experience poorer health than their counterparts from socially advantaged groups because they receive poorer healthcare. In this article, to limit the scope of this review, we primarily focus on how social psychological processes, specifically those related to intergroup relations and intergroup bias, can produce healthcare disparities. However, we note that there are other literatures on how some of the same kinds of social psychological variables may more directly affect people’s health. For example, there is a large body of research on how perceived and actual discrimination directly affect the physical and mental health of members of target groups (e.g., Brondolo, Hausmann, et al., 2011; Fuller-Powell, Evans, & Ong, 2012; Hagiwara, Penner Gonzalez, & Albrecht in press; Penner & Hagiwara, in press).
Until relatively recently, healthcare disparities have been primarily studied by social epidemiologists, public health researchers, health economists, and political scientists. These scholars have mainly focused primarily on societal and structural causes of this social problem, such as differences in health insurance coverage and access to comparable medical facilities. These remain important and useful approaches to understanding healthcare disparities. Nevertheless, in the last decade or so reports in the United States (US) and Europe (e.g., Institute of Medicine [IOM], 2003; Nazroo & Karlsen, 2001; Shavers, Fagan, Jones, Klein, Boyington, Moten & Rorir, 2012) on the role of bias and discrimination in healthcare disparities have brought increased attention to the relevance of social psychology and related disciplines to the study of healthcare disparities. This review presents an overview of our own and other researchers’ social psychological analyses of healthcare disparities.
In the review, we focus on healthcare disparities among members of racial/ethnic minorities because this is the focus of the clear majority of research on healthcare disparities (Shavers et al., 2012). However, race/ethnicity is not the only group characteristic that has been linked to healthcare disparities. For example, patients who have lower socioeconomic status (SES) have developmental, mental or physical disabilities, are elderly, are members of certain religions, and/or are gay, lesbian, bisexual, or transgendered all experience healthcare disparities (Daponte-Codia et al., 2008; Dilley, Simmons, Boysun, Pizacari, & Stark, 2010; Lahelma & Lunberg, 2009; Linehan, Walsh, Van Schrojenstein Lantman-de Valk, Kerr, & Dawson, 2009; Mobaraki & Söderfeldt, 2010; Obeidat et al., 2010). Because we base our analysis on generalizable psychological processes and intergroup dynamics, we believe that most of the models and theories we present can be readily applied to these other forms of bias and healthcare disparities beyond those involving race/ethnicity.
Our review also primarily presents research conducted in the US. This is because in the US: substantial differences in the health status of Whites and of racial/ethnic minorities, especially those who self-identify as Black and/or African/Afro-Caribbean American have been very well documented (see National Center for Health Statistics, 2011); racial healthcare disparities have received relatively more attention in both the medical and psychological literatures than in other countries; and there has been a long-standing interest in racial bias in social psychological research (Allport, 1954; Dovidio, 2001).
The attention given to healthcare disparities in the US has led some health researchers to suggest that serious healthcare disparities are largely confined to countries in which healthcare systems are primarily privately financed, such as the US. There is, indeed, ample evidence that structural differences in the healthcare systems and how they are financed affect patients’ access to healthcare and the quality of care provided (IOM, 2003). However, research clearly shows that throughout the world racial/ethnic minorities typically receive poorer healthcare than members of racial/ethnic majority groups. For example, racial/ethnic healthcare disparities are found in countries with government supported healthcare systems, such as Canada (Frohlich, Ross, & Richmond, 2006), Israel (Nakash, Saguy, & Levav, 2012), New Zealand (Harris et al., 2006), Sweden (Rostila, 2010), the United Kingdom (UK; Bécares, Stafford, & Nazroo, 2009), Serbia (Sujoldžić, Peternel, Kulenvoić, & Terzić, 2006), and in many Latin American countries (Casas, Dachs, & Bambas, 2001). In summary, healthcare disparities among racial/ethnic minorities and majorities represent a ubiquitous multinational problem.
In our review of healthcare disparities, we begin by considering some factors other than racial bias and discrimination that might covary with membership in a racial minority and affect the quality of healthcare people receive. We readily acknowledge the importance of these other factors, but a core argument of this article is that even when these factors are controlled, racial-minority patients’ and non-minority physicians’ race-related thoughts, feelings, and behaviors can each influence the quality of the healthcare members of racial minorities receive and thus produce disparities in health status. This argument is presented in a three-level model of the causes of healthcare disparities that can lead to health status disparities. The levels of analysis -- societal, intrapersonal, and interpersonal -- are clearly interrelated and overlap with one another, but for the purpose of organizational clarity we consider them separately. After presenting the model, we suggest interventions at each of these levels for addressing racial disparities in healthcare.
Causes of Racial Healthcare Disparities
As Bhopal (2007) rightly pointed out in his discussion of racial health and healthcare disparities in the UK and Europe, “[t]he causes of the inequalities in health status and quality of healthcare that are so easily demonstrable by ethnicity and race are complex and difficult to disentangle” (p. 238). However, several factors have been identified as major contributors to healthcare disparities.
Socioeconomic Status
One major potential source of racial1 healthcare disparities is socioeconomic status (SES). In many countries SES strongly covaries with race, such that racial minorities on average have lower SES than racial majorities. Low SES is an environmental stressor and has direct, deleterious affects on people’s health (e.g., Fuller-Powell et al., 2012), but here we are concerned with SES and healthcare disparities. Research has shown that healthcare providers often provide poorer care to low SES individuals (Hall, Roter, & Katz, 1988) perhaps in part because, relative to high SES patients, low SES patients may be seen as having poorer self-control, and less likely to adhere to treatment recommendations (van Ryn & Burke, 2000). Other potential causes of poorer healthcare for low SES individuals may be that many people with low SES are not able to take time off work to seek medical help or afford health insurance and/or copays. However, racial healthcare disparities exist across all levels of SES and are evident even among the most affluent groups (De Lew & Weinick, 2000; Elster, Jarosik, VanGeest, & Fleming, 2003; McGuire, Alegria, Cook, Wells, & Zaslavsky, 2006). Statistically controlling for differences in SES reduces but does not eliminate healthcare disparities between racial groups (Saha, Arbelaez, & Cooper, 2003). Thus, SES is an important cause of healthcare disparities but, by itself, is not a sufficient explanation of the racial healthcare disparities reported throughout the world.
Language Proficiency
Research in several different countries has shown that language barriers faced by immigrants often play a role in healthcare disparities among racial minorities. For instance, in the US, limited English language proficiency is associated with decreased utilization of preventive healthcare services (Linsky, McIntosh, Cabral, & Kazis, 2010), longer hospital stays (John-Baptiste et al., 2004), poorer health control (Fernandez et al., 2010), and increased medical errors (Divi, Koss, Schmaltz, & Loeb, 2007; see Norredam et al., 2004 for similar findings from Denmark). However, the fact remains that in many countries, healthcare disparities commonly occur among members of racial minorities comprised almost exclusively of native language speakers (Kirby, Taliaferro, & Zuvekas, 2006), suggesting that language barriers only explain a portion of healthcare disparities.
Health Literacy
Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services they need to make appropriate health decisions (Nielsen-Bohlman & Panzer, 2004). Health information provided to the lay public may include complex and unfamiliar terms; individuals with limited health literacy may experience difficulty processing such information and become so discouraged or intimidated that they may become reluctant to seek healthcare. In the US, there is a strong association between level of health literacy and race (Cooper, Hill, & Powe, 2002; Paasche-Orlow, Parker, Gazmararian, Nielson-Bohlman, & Rudd, 2005); thus some health researchers argue that health literacy rather than social variables is a major cause of racial healthcare disparities. Indeed, studies in the US sometimes find that when differences in health literacy are controlled, the size of healthcare disparities between racial minorities and Whites in the US is reduced (Osborn, Paasche-Orlow, & Wolf, 2007). However, evidence of healthcare disparities tyoically remains even after controlling for health literacy (e.g., Franks, Muennig, Lubetkin, & Jia, 2006; Williams, Mohammed, Leavell, & Collins, 2010).
Although health literacy may be a unique cause of healthcare disparities, in practice it may be hard to disentangle the role of health literacy in racial healthcare disparities from the effects of racial attitudes and beliefs. For example, physicians may be less accurate in judging the health literacy of Black than White patients (Kelly & Haidet, 2007), suggesting that health literacy’s impact on medical interactions may, in part, be moderated by physicians’ racial attitudes or cultural competence. Also, health literacy levels among Blacks may be influenced by the fact that they have a much higher level of distrust of physicians and the medical system than Whites (Dovidio et al., 2008), which in turn may cause them to seek medical information less often than Whites and to be less accepting of the information they obtain. Such reactions would serve to reduce a person’s health literacy.
Taken together, there is substantial evidence that SES, language proficiency and health literacy contribute to inequalities in the relative quality of healthcare different racial groups receive. However, these explanations, which primarily focus just on the attributes of racial minority-group members, do not provide a sufficient explanation of racial healthcare disparities. Social psychological processes also play an important role.
An increasing number of public health researchers and government officials have begun to focus on how race-related thoughts, feelings, and actions may relate to racial healthcare disparities. For example, in their article in the European Journal of Public Health, Agyemang, Seeleman, Suurmond, and Stronks (2007) argued that “the time is right to take discrimination in health and welfare services more seriously in Europe” (p. 241). Research reports in the UK, New Zealand, the US, and Sweden have made similar arguments (IOM, 2003; Nazroo & Karlson, 2001; New Zealand Ministry of Health, 2002; Shavers et al., 2012; Swedish National Institute of Public Health, 2006). In the next section, we provide explanations of how and why racial-related phenomena contribute to healthcare disparities and then some possible solutions to the problem.
Multilevel Processes of Healthcare Disparities
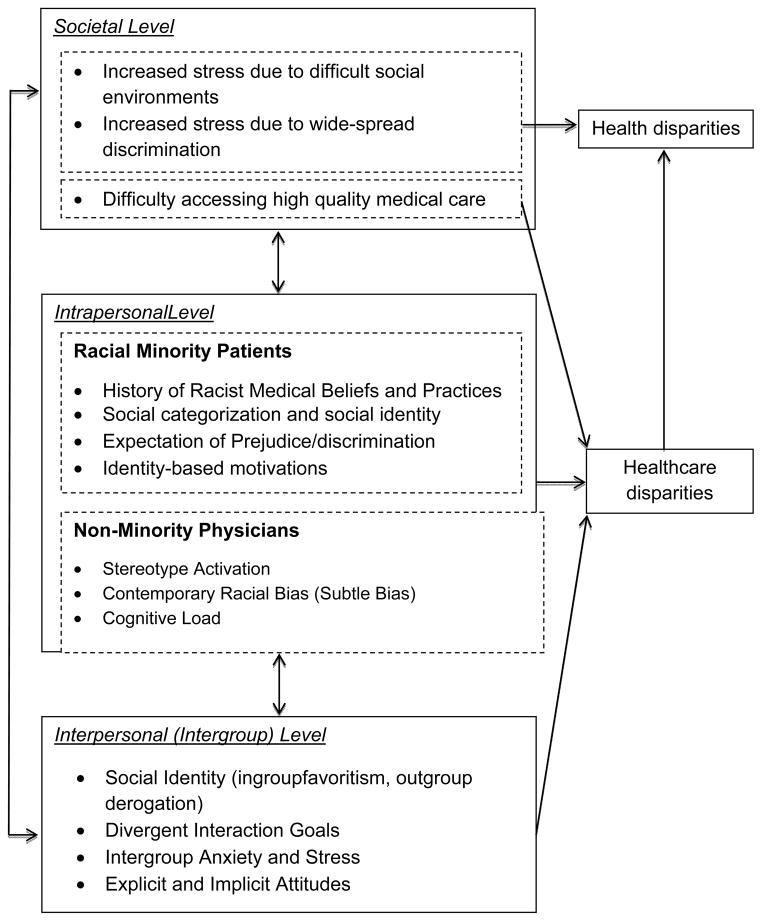
The model presented in Figure 1 presents causes of healthcare disparities (and thus health status disparities). The model considers three separate but clearly interrelated processes that might be associated with healthcare disparities: societal, intrapersonal, and interpersonal processes. For purposes of clarity, the three levels in the model are discussed separately, but as the bi-directional arrows in Figure 1 indicate, there are interrelationships and complementary influences among the levels. In this section, we briefly describe each level of analysis. Then, in the next section, we more fully examine specific processes within the intrapersonal and interpersonal levels. In the exposition of these parts of the model, we use social psychological theory and research on explicit and implicit social cognitions, social identity and categorization, and related intergroup processes to help us better understand how racial bias and discrimination may produce healthcare disparities and thus disparities in the health of members of minority groups. Because our focus is on social psychological processes rather than societal/structural processes responsible for racial healthcare disparities, we give much more emphasis to the latter two levels than to the societal/structural one.
Figure 1.
A multi-level model of the causes of healthcare and health status disparities
Societal-Level Processes
The first level of analysis, the societal or structural level, focuses on how race-related social environments, institutional practices, and attitudes that characterize a particular society, region, or specific community affect healthcare disparities. At this level of analysis, the presumed causes of healthcare disparities are not primarily psychological processes occurring within and between individuals. Rather, healthcare disparities are presumed to be manifestations of widespread racial bias and/or discrimination. More specifically, they are race-related historical, societal, economic, and structural factors that result in certain racial minority groups experiencing persistent and widespread unfair treatment and institutional discrimination in a variety of realms.
One consequence of societal-level processes is that racial minorities may live in difficult social environments, characterized by, for example, less mobility, greater isolation from other segments of the population, fewer treatment options available to them, less exposure to treatment innovations, and fewer high quality medical facilities within close proximity (IOM, 2003; Saldana-Ruiz, Clouston, Rubin, Coleen, & Link, 2013). These challenging social environments may prevent racial minorities from receiving the same quality of healthcare as people living in better-resourced neighborhoods.
Bias and discrimination at a societal or structural level may also be related to healthcare disparities in other, less direct, but important ways. Recent research by Reid, Dovidio, Ballester, and Johnson (2013) illustrates this process. Reid et al. examined how community level stigma may affect the efficacy of health interventions directed at minority group members. The interventions, conducted in various communities around the US, were intended to increase condom usage among Black Americans. In their meta-analysis of 70 separate studies, Reid et al. found that interventions were most effective when Whites in the community had positive attitudes toward Blacks and residential segregation was low. Reid and colleagues posit that Blacks living in communities with widespread negative attitudes toward Blacks and high levels of residential segregation may feel they are the targets of discrimination and stigmatization and as a result, trust members of outgroups less. When outgroup members offer Black community members health-related interventions, they may be less likely to accept them.
Finally, as already noted, feelings of being the target of discrimination may serve as a life stressor for racial minorities, increasing the physiological load on their bodies and thus their susceptibility to various diseases. For example, Sims et al. (2012) found in large sample of Black adults a significant association between exposure to discrimination and the prevalence of hypertension (also see Major, Mendes, & Dovidio, 2013).
Our model therefore posits that at the societal level, racial/ethnic bias and discriminatory norms, policies, and practices can create social environments and conditions that can directly lead to healthcare disparities. Further, it also appears that bias and discrimination at a societal level may create psychological environments that can also produce healthcare disparities among members of a stigmatized target group.
There is considerable overlap between the next two levels of the model, intrapersonal and interpersonal processes; however as noted, we believe that to best understand the psychological processes that underlie healthcare disparities we need to consider them separately. For the purposes of this article, the intrapersonal level concerns what is “within” a person – that is, thoughts and feelings that operate at both explicit and implicit levels and affect people’s reactions to a socially defined group in the absence of direct contact with a member of that group and/or in situations where they actually encounter a person perceived to be a member of that group. Specifically, the intrapersonal level of the model concerns how the race-related thoughts and feelings of minority patients and of non-minority physicians affect healthcare related thoughts, feelings, and actions. For example, Black patients’ feelings about past racial discrimination may affect things such as the kind of medical care they seek, what they think of the care they receive, the health behaviors in which they engage and perhaps most importantly their reactions to interactions with healthcare providers. In a similar fashion, racial bias and stereotyping among physicians may affect diagnosis and treatment decisions, and perhaps most importantly their reactions to racial minority patients.
The interpersonal level in the model focuses on medical interactions between patients from one ethnic/racial group and physicians from another racial group. At this level, the analysis concerns what patients and physicians say and do during these interactions and how each reacts to the other’s words and actions. This is an important aspect of racial healthcare disparities in the US (and elsewhere) because racial minority patients are much more likely than racial majority patients to engage in racially discordant medical interactions (e.g., Black patient, White physician). For example, in the US approximately 75% of Black patients see non-Black physicians when they seek medical help (Chen, Fryer, Phillips, Wilson, & Pathman, 2005). This statistic also reflects the dramatic under representation of racial minorities in medical school and medical practice (Nunez-Smith et al., 2012). For instance, in the US, where Blacks are about 12% of the population only about 4% of all physicians self-identify as Black; this percentage has been the same for about the last 30 years (O’Reilly, 2013).
Although we use the term interpersonal to describe this level of the model, one might quite reasonably also use the term intergroup contact to describe racially discordant medical interactions. In primary care interactions, patients and physicians may often be, at most, only minimally acquainted with one another prior to their interaction. Thus, while the physician and patient are in a face-to-face interaction that involves considerable dialogue, in a racially discordant medical interaction they may react to one another more as representatives of a (different) group than as individuals. From this perspective, such interactions may represent one of the kinds of intergroup contact described by Brown and Hewstone (2005). Specifically, a racially discordant medical interaction may often be an instance of intergroup contact in which intergroup differences are salient and important, but it is also interpersonal because the patient may provide sensitive, personalized information to the physician.
As already noted, the race-related thoughts and feelings patients and physicians bring with them to racially discordant medical interactions have an extremely important influence on what transpires during the interaction. Specifically, these intrapersonal processes influence what each party says and does during the interaction, which, in turn, shapes what the other says/does during the interaction and, thus, the quality of communication in the medical interaction. However, as we discuss, there are other interpersonal (or intergroup) processes that can affect communication between the participants and we shall consider them as well. Whatever the cause, the quality of communication can affect the quality of treatment decisions each party makes and, in the case of the patients, also influence how likely it is that they will adhere to these treatment decisions.
Social Psychological Theory and Racial Healthcare Disparities
In this section, we review social psychological research on how the ways people think about and respond emotionally to others (intrapersonal processes) and how people interact with each other (interpersonal processes) can result in healthcare disparities.
Intrapersonal-Level Processes
A core assumption of our approach to health disparities is that, as the IOM (2003) report posited, race-related attitudes and beliefs play a critical role in healthcare disparities and thus are responsible for disparities in health status. Race-related stereotyping and attitudes can be conscious or explicit; that is, people are aware of their thoughts and feelings and can manage them consciously. However, as the result of over-learned racial associations, stereotypes and attitudes can also be automatic, nonconscious or implicit (Greenwald & Banaji, 1995); that is people may not be aware of these feelings and thoughts (Dovidio & Gaertner, 2004; Gaertner & Dovidio, 1986; Wilson, Lindsey, & Schooler, 2000). The intrapersonal level of the model concerns processes through which an individual’s own race-related thoughts and feelings affect their healthcare-related thoughts, feelings, and behaviors. While these intrapersonal processes obviously have social origins and consequences, in this section we consider instances where their impact on healthcare disparities is substantially independent of the thoughts, feelings and actions of another person. We consider these intrapersonal processes in patients and physicians separately.
Racial minority patients
Black patients prefer to see Black physicians (Chen et al., 2005) and report higher quality care and greater satisfaction with their medical care when the physician is Black than when the physician is White (Cooper et al., 2003; Garcia, Paterniti, Romano, & Kravitz, 2003). Importantly, racial minority individuals’ negative perceptions of physicians are directly linked to their healthcare-related behaviors. For example, Black patients are more likely to schedule and keep appointments with Black than White physicians (LaVeist, Nuru-Jeter, & Jones, 2003). Additionally, racial minorities (at least in the US) are more likely to delay or fail to seek mental healthcare (Kessler et al., 1996; Sussman, Robins, & Earls, 1987; Zhang, Snowden, & Sue, 1998) and terminate treatment prematurely (Sue, Zane, & Young, 1994), compared to racial majorities.
These racial minority patients’ negative perceptions of physicians may be at least partially due to lack of trust. When compared to members of majority racial groups, members of racial minority groups are more likely to experience mistrust of and dissatisfaction with their medical care (Boulware, Cooper, Ratner, LaVeist, & Powe, 2003; Halbert, Armstrong, Gandy, & Shaker, 2006) and to believe they are mistreated by healthcare providers (Thorburn & Bogart, 2005). Furthermore, individuals who are less trusting of physicians are less likely to use preventive services (Carpenter et al., 2009; Thompson, Valdimarsdottir, Winkel, Jandorf, & Redd, 2004) and adhere to physicians’ recommendations (Bogart, Wagner, Galvan, & Banks, 2010; et al., 2013; Penner et al., 2013; Saha, Jacobs, Moore, & Beach, 2001).
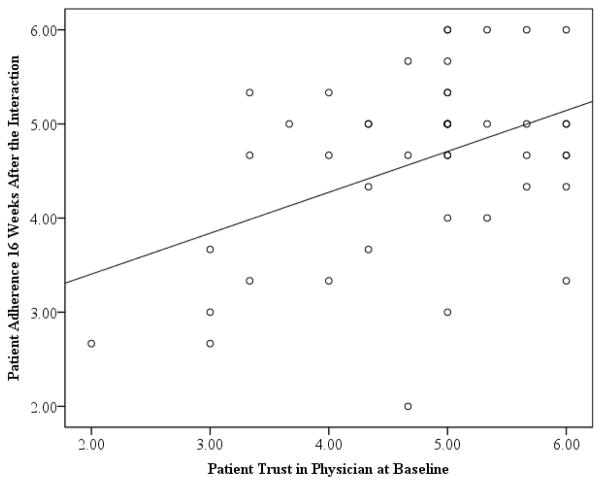
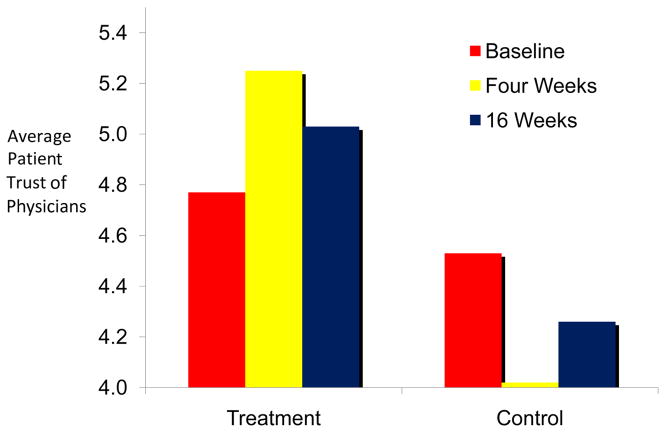
This relationship is illustrated in data that we collected from a primary care clinic in a large US city (Detroit) (Hagiwara et al., 2013). This study is one of a series of studies conducted in this setting, which is described in more detail in a later section. Immediately before Black clinic patients (n = 80) had their appointment with a non-Black physician we measured how much they trusted physicians in general, using two items taken from Dugan, Trachtenberg, and Hall’s (2005) Interpersonal Trust in a Physician short form: (a) “I completely trust the doctors’ decisions about which medical treatments are best,” and “All in all, I trust doctors completely.” Sixteen weeks after their appointment with the doctor in the clinic, these patients received a mail survey about their adherence to their own physician’s treatment recommendations (using items from the RAND Health’s Medical Outcomes Study; Hays et al., 1994; e.g., “I followed my doctor’s suggestions exactly; I found it easy to do the things my doctor suggested I do.”). Figure 2 presents a scatter plot of the relationship between the Black patients’ trust of physicians prior to racially discordant medical interactions and their adherence to their own physician’s recommendations 16 weeks after the interactions. There was a significant positive relationship (r (45) = .43, p=.003) between general trust and specific adherence.
Figure 2.
The association between patient trust and subsequent adherence. Copyright © 2013 Elsevier. Racial attitudes, social control, and adherence in racially discordant medical interactions. Hagiwara, N. et al., Social Science and Medicine, 87, 123–131.
Although our emphasis is on social psychological explanations of these thoughts and feelings, one cannot consider the attitudes and feelings of racial minority patients without first placing them in a social and historical context. A substantial portion of racial minorities’ mistrust of medical care and preference for racially concordant physicians very likely has its origins in the general levels of racism and racial discrimination that are part of the past (and sometimes the present) history of many western industrialized countries. Embedded in this history is the dismal legacy of racist beliefs and practices in the medical profession (Byrd & Clayton, 2000). For example, in the US and Europe, polygenism—the theory that human races were separate biological species—dominated scientific theory from the early 17th century until perhaps as recently as the early 20th century (Byrd & Clayton, 2000; 2002). Blacks, Latinos, and other socially disadvantaged racial minority groups were also frequently used as participants in dangerous medical experiments without their willing consent and with little regard for their welfare (Byrd & Clayton, 2000). Thus, it cannot be overlooked that some of racial minorities’ mistrust of general medical care (and even of their individual physicians) is rooted in harsh and potentially traumatic historical realities (Earnshaw, Bogart, Dovidio, & Williams, 2013). This mistrust may represent a rational response to a system that has ill-served racial minority patients in the past. However, we believe there are other more basic social psychological processes at work as well.
Social categorization and social identity (Tajfel & Turner, 1979; see also Abrams & Hogg, 2010) also play important roles in what racial minority patients think and feel about their medical care and their healthcare related behavior. Because human beings are constantly required to process large amounts of complex information, they develop strategies to reduce cognitive effort and preserve cognitive resources by using categorization and generalization of information (Macrae, Milne, & Bodenhausen, 1994). Categorization and application of social categories to evaluations, perceptions, and treatment of others clearly help people function more effectively in everyday life. However, the process of social categorization inevitably makes a person’s social identity more salient and provides the basis for intergroup bias (Otten & Moskowitz, 2000).
In addition, according to Social Identity Theory (Tajfel & Turner, 1979), when people’s group membership is salient, their feelings of esteem are closely tied to their group’s status and they respond in ways that promote their group’s distinctiveness and enhance its status. People generally assume that ingroup members share their attitudes and beliefs (Robbins & Krueger, 2005), and they expect outgroup members to have a contrasting perspective (Mullen, Dovidio, Johnson, & Copper, 1992). Minority-group members are particularly vigilant to cues of bias from outgroup members (Vorauer, 2006). These psychological processes systematically influence the perceptions and behavior of minority patients. In this context, their identity as a member of a racial minority group that has been the target of prejudice and discrimination is highly salient.
Expectations of prejudice/discrimination among minority patients play an important role in intergroup encounters generally, and in medical interactions, specifically. Richeson and Shelton (2007) demonstrated that when Blacks interact with Whites, they often worry they will be the target of prejudice and/or confirm negative stereotypes associated with their racial groups. Thus, one source of racial minority patients’ possible negative reactions to the healthcare system may be expectations they will experience stereotyping, prejudice, or discrimination in their medical care. Related to this, Burgess, Warren, Phelan, Dovidio, and van Ryn (2010) argue that racial minority patients in racially discordant medical interactions may experience stereotype threat, which involves the activation of cultural stereotypes about one’s group and triggers stereotype-confirming behavior. This may have particularly detrimental effects on the responses of racial minorities to healthcare interventions that might reinforce these stereotypes. For example, some Black patients could be reluctant to participate in classes that provide health information (e.g., cancer screening, diabetes care, prenatal care) because they may fear this would reinforce stereotypes about their intellectual abilities and educational achievements.
However, such feelings are probably not uniform across racial minority group members; there are clearly individual differences in recognition and expectations of racial bias. Theories such as stigma consciousness (Pinel, 1999) or race-based rejection sensitivity (Mendoza-Denton, Downey, Purdie, Davis, & Pietrzak, 2002) concern the chronic affective and cognitive consequences of being the target of stereotyping, prejudice, and discrimination. According to these theories, individuals who score high on stigma consciousness or race-based rejection sensitivity often expect to be the target of prejudice. Research has shown that individuals who expect to be the target of prejudice evaluate intergroup interactions more negatively (Butz & Plant, 2006) and make efforts to avoid them (Mendoza-Denton, et al., 2002; Shelton & Richeson, 2006; Swim & Hyers, 1999). In addition, it has been shown that when individuals expect to be a target of prejudice and discrimination, they become vigilant for signs of prejudice and discrimination (Major & Townsend, 2010; Shelton & Richeson, 2006), resulting in a confirmation of their negative expectations.
In the healthcare context, heightened sensitivity to discrimination and prejudice due to past experiences may influence how racial minority patients perceive their physicians and thus healthcare related decisions. For example, Greer (2010) found that Black hypertension patients who perceived their physicians to be racially biased were less likely to make future appointments than patients who did not perceive their physicians in this way. Importantly, general expectations of prejudice and discrimination that are not directly related to healthcare or specific healthcare facilities/personnel can also affect patients’ health-related attitudes and behaviors. Benkert, Peters, Clark and Keves-Foster (2006) reported that the more racism Blacks perceive in the world around them, the less trust they have in the healthcare system.
Perceptions of general discrimination – including experiences of bias outside the medical encounter and in everyday life – can also affect reactions to individual medical interactions. We (Penner et al., 2009) used a larger sample (n=142) of Black patients at the same inner-city clinic employed in the Hagiwara et al. (2013) study (described earlier) to examine the impact of perceived discrimination. Immediately prior to the meeting with the doctor, we assessed patients’ general experiences with discrimination. To do this, we used items from Brown’s (2001) Self-Perceived Racial and Ethnic Discrimination Scale, in which respondents were asked whether they had ever experienced unfair treatment in each of seven social domains: jobs, education, medical treatments (added to Brown’s original list), job applications, police encounters, housing, and dealing with neighbors. In our sample, the majority of patients (56.4%) reported they had experienced discrimination in the past at least in one domain. In mail surveys, sent 4 and 16 weeks after their appointment with the doctor, patients reported on their adherence to the doctor’s recommendations (Hays et al., 1994), as well as their self-reported health using the 20-Item Short Form Health Survey (Ware, Sherbourne, & Davies, 1992), which assesses physical functioning, role functioning, social functioning, mental health, pain, and current general health status.
We found that, when compared to Black patients who reported experiencing relatively little past discrimination, those who reported experiencing high levels of past discrimination expressed significantly less satisfaction with their medical interactions and closeness with the physician they had just seen. Black patients who experienced higher levels of discrimination were also less likely to adhere to their physician’s recommendations four weeks after the visit, and this lower adherence, in turn, was associated with poorer health status among these patients 16 weeks after the visit. Casagrande, Gary, LaVeist, Gaskin, and Cooper (2007) also found that experiences with discrimination were associated with delays in seeking medical care and poor medical adherence even when controlling for medical mistrust.
Racial minority patients’ negative health-related attitudes and behaviors may not always be the result of negative perceptions of physicians and medical care. They may also sometimes be the result of strong identification with their own racial group and consequent identity-based motivations. According to the Identity-Based Motivation Model (Oyserman, Fryberg & Yoder, 2007), in order to maintain their social identity, people tend to engage in behaviors that are perceived to be what other ingroup members typically do, regardless of whether the behaviors have objectively positive or negative consequences for them (see also Rostila, 2010). Thus, if individuals perceive that exercising and maintaining a healthy diet is the norm for their social group, they are apt to engage in regular exercise and healthy eating habits. In contrast, if individuals believe that many fellow ingroup members smoke and/or value smoking, they are likely to smoke even if they recognize the negative consequences of smoking.
Oyserman et al. (2007) have shown that racial minorities (i.e., Black Americans, Mexican Americans, and Native Americans) viewed health promotion behaviors, such as exercising, getting enough sleep, and eating fruits and vegetables, as outgroup-defining behaviors and unhealthy behaviors as ingroup-defining behaviors. Oyserman et al. (2007) also investigated the effects of increasing the salience of racial identity among racial minorities. When the minority participants’ social identities were made salient (via contrasting them to a White middle-class social identity), they expressed more feelings of fatalism about improving their health and had more difficulty correctly identifying health-related knowledge.
Non-minority physicians
There is more than ample evidence that racial minorities receive less appropriate and aggressive healthcare than members of racial majorities. Disparities have been found in the general level of care Black and White patients receive (Harris, Andrews, & Elixhauser, 1997; Lee, Gehlbach, Hosmer & Baker, 1997) and in the treatment of specific diseases. These disparities cut across specific mental and physical diseases, and healthcare settings (IOM, 2003). Regarding mental health, racial minorities are less likely to receive mental healthcare and receive poorer quality care when they are treated (DHHS, 2001; Wang, Berglund, & Kessler, 2000; Young, Klap, Sherbourne, & Wells, 2001). For example, Mallinger and Lamberti (2007) studied Black and White patients with schizophrenia who were receiving antipsychotic medications. They found that Black patients were less than likely than White patients to receive other medications to control the ancillary symptoms of schizophrenia. Mental healthcare disparities remain even when SES and relevant demographic factors are controlled (Snowden, 2003).
Turning to physical health, racial disparities are also found in the treatment of cardiac disease and many different cancers, including breast, lung, prostate, colorectal and other gastrointestinal cancers (e.g., Berger, Lund, & Brawley, 2007; Griggs, Sorbero, Stark, Heininger, & Dick, 2003; Lin & Virgo, 2013; Morris et al. 2008; Shavers et al., 2004; Underwood et al., 2004). One might expect that in situations in which swift and decisive action is required racial healthcare disparities might disappear, but treatment disparities also exist in emergency room settings. For example, racial minorities with symptoms of a heart condition are less likely than White patients to receive analgesics, and their myocardial infarctions are more likely to be missed. These disparities exist even when one controls for levels of disease severity and factors such as SES, demographic characteristics and insurance availability (Pope et al., 2000; Todd, Deaton, D’Adamo, & Goe, 2000; Todd, Lee, & Hoffman, 1994; Todd, Samaroo, & Hoffman, 1993). Finally, healthcare disparities can be found in pediatric practices as well. In a study of over one million medical encounters, Gerber et al. (2013) found that physicians were significantly less likely to give antibiotics to their Black than their White patients, and if antibiotics were given to Black children they were less likely to be broad spectrum drugs.
It would be an oversimplification to attribute these and a host of other treatment disparities simply to physician race-related thoughts and feelings. Treatment disparities are a complex social problem with multiple causes, many of which are likely at the societal level of explanation, and of course, patient preferences and decisions play important roles in what treatments are provided. In this section, we only consider those treatment disparities that theory or empirical evidence suggest may be due to race-related intrapersonal processes among physicians. As was the case with patient effects, we rely heavily on theories that have their origins in social categorization and social identity processes. These include stereotype activation, contemporary racial bias, and cognitive load.
Stereotype activation, stemming from social categorization among physicians, may at least partially explain the apparent contradiction between the widely expressed condemnation of bias in medical care by healthcare professionals and the well-documented treatment disparities that continue to exist. van Ryn and her colleagues (van Ryn, 2002; van Ryn, Burgess, Malat, & Griffin, 2006) have proposed a social-cognitive model that uses social categorization processes to explain how patients’ race influences physicians’ diagnosis and treatment decisions. According to this model, physicians more or less automatically categorize their patients into social groups based on race, which is often the most salient social group cue. Upon categorization, stereotypes and prejudice associated with racial groups in which the patient is categorized are activated.
These activated stereotypes then influence physicians’ perceptions of patients and expectations about patient adherence, which in turn affect physicians’ treatment decisions. For instance, it has been shown that physicians stereotype Black patients as poorer, less educated, less intelligent, less trustworthy, more likely to engage in risky health behaviors, and less likely to comply with medical recommendations than White patients (e.g., Moskowitz et al., 2011; Sabin, Rivara, & Greenwald, 2008; Street, Gordon & Haidet, 2007; van Ryn & Burke, 2000). These negative stereotypes and expectations about Blacks may further influence physicians’ treatment decisions, such that they may be less likely to recommend an appropriate treatment for Black than White patients (Bogart, Catz, Kelly, & Benotsch, 2001; van Ryn et al., 2006). For example, van Ryn et al. (2006) examined physicians’ decisions to recommend coronary bypass surgery for Black and White patients with the same cardiac conditions. They found that physicians were more likely to recommend this procedure to Whites than Blacks, but this effect was fully mediated by the physicians’ perceptions that the Black patients were less educated and had a less active lifestyle. Moskowitz et al. (2011) have also shown that physicians trust non-White patients less than White patients when prescribing opioid analgesics; this occurs despite the fact that rates of illicit use and opioid analgesic misuse between these two groups are similar.
Stereotypes activated by social categorization also influence how people interpret others’ behaviors and intentions (Duncan, 1976). Explicit and implicit stereotypes associated with social categories may therefore also influence physicians’ diagnostic assessments. As an example, Hirsh, Jensen, and Robinson (2010) found that nurses evaluate pain expressed by patients differently based on their beliefs and expectations as to how individuals with certain social characteristics would react to pain. More recently, Moskowitz, Stone, and Childs (2012) used a priming paradigm and found that White doctors were faster to recognize diseases and conditions such as HIV, drug abuse, obesity, and stroke after being subliminally primed with a Black face (compared to a White face). Moskowitz et al. thus concluded that physicians’ initial reactions to patients may be influenced by racial/ethnic stereotypes about the frequency of certain diseases (including behavior disorders such as drug abuse) among Blacks relative to Whites. This stereotyping may lead to misdiagnoses and inappropriate treatments. Importantly, in neither the Hirsch et al. or Moskowitz et al. study did the participants have any conscious awareness of their biases. These findings suggest that healthcare professionals may be biased “even in the absence of the practitioners’ intent or awareness” (Moskowitz et al., 2012, p. 996).
No study to date has systematically examined how accurate physicians’ negative stereotypes about racial minority patients are. However, as noted above, racial minorities are indeed less likely to adhere to physicians’ medical recommendations (Bogart et al., 2010; Saha et al., 2010) and keep appointments (LaVeist et al., 2003). Thus, as with any other stereotypes, there may be some basis to some of physicians’ expectations about racial minority patients. Nevertheless, the major problem with stereotype activation is that negative expectations based on stereotypes are generalized to the entire social group regardless of whether particular individuals actually possess stereotypical characteristics. Furthermore, when physicians act on their negative expectations about racial minority patients, the patients may ultimately confirm the negative expectations by acting in accord with these negative stereotypes (i.e., self-fulfilling prophecy; Merton, 1948), thus resulting in a vicious circle. For example, physicians who expect their minority patients to be less adherent to their medical recommendations may devote less time to discussing the condition and treatment with minority patients, which then leads minority patients to understand the recommendation less well. This lack of understanding the doctor’s recommendation, in turn, may produce less adherence – creating the self-fulfilling prophecy in the medical encounter (see also Perloff, Bonder, Ray, Ray, & Siminoff, 2005).
Within the medical profession, explicit expressions of racial bias are especially rare, and behavior that might represent such bias in medical care is widely and vigorously condemned (Green et al., 2007; Penner Albrecht, Orom, Coleman & Underwood, 2010; Penner, Eggly, Griggs, Orom, & Underwood, 2012). Despite this, there is evidence of more subtle, perhaps often unintentional, contemporary racial bias. The majority of physicians show a moderate to strong implicit preference for Whites relative to Blacks (Sabin, Nosek, Greenwald & Rivara, 2009; Sabin et al., 2008). Moreover, such biases do affect treatment decisions. For example, in a vignette study, Green et al. (2007) found that implicit racial bias affected physician recommendations for Black patients with acute coronary syndromes. As implicit racial bias increased, so did the likelihood that physicians would treat a White patient more aggressively and appropriately than a Black patient. More recently, Sabin and Greenwald (2012) used vignettes involving pediatric patients and found that as physicians’ pro-White bias increased, their willingness to prescribe narcotics for Black children with pain due to surgery decreased.
Theories of contemporary racial bias, such as Aversive Racism Theory (e.g., Dovidio & Gaertner, 2004; Gaertner & Dovidio, 1986), Symbolic Racism (Kinder & Sears, 1981), and the Justification-Suppression Model (Crandall & Eshleman, 2003), would lead us to expect that such discriminatory actions are most likely to occur when a situation allows people to rationalize that their actions toward racial minorities are not due to racism but due to something else. In the health context, one situation in which this may occur is when the guidelines or cues for appropriate medical decisions are somewhat ambiguous. For instance, few guidelines for treating pain exist because many patients’ reports of pain are diffuse, nonspecific, and difficult to empirically verify and quantify (Green et al., 2003). Studies have shown that, as predicted by these theories, across a variety of different kinds of pain and medical settings, racial minority patients are more likely to be undertreated for pain than Whites (e.g., Burgess, van Ryn, Crowley-Metoka, & Malat, 2006; Green et al., 2003). Burgess et al. (2006) argued that implicit stereotypes about Blacks (e.g., less accurate in their self-reports, more likely to abuse drugs) may cause physicians to either underestimate the seriousness of the pain or overestimate the likelihood a patient might abuse pain medications. However, importantly, in this situation, physicians could also rationalize the under-treatment of Blacks by using other factors that are much more justifiable and apparently nondiscriminatory (e.g., patients’ inability to accurately describe pain; differences in ability to tolerate pain) than their bias against Blacks. Trawalter, Hoffman, and Waytz (2012) found that people believe that Blacks and individuals from lower SES feel less pain when injured than White upper SES individuals. Such biased perceptions may also be held by physicians.
Finally, we consider some circumstances in which physicians may be more likely to make less appropriate diagnosis and treatment decisions for racial minority patients than racial majority patients. The cognitive load that physicians experience when making their decisions may be a significant factor in their responses to minority, relative to majority, patients. A depletion of cognitive resources due to increased cognitive load is likely to increase the probability that people will engage in automatic rather than controlled cognitive processes because they need to prioritize multiple cognitive processes. When one encounters a member of an outgroup, the activation and application of social categories are rather automatic and require minimum cognitive efforts, whereas individuation of that person requires conscious efforts (Brewer, 1988; Fiske, Lin & Neuberg, 1999). Therefore, when people are under high cognitive load, they are more likely to rely on social categories and stereotypes as opposed to individuating information (Bodenhausen & Wyer, 1985).
As mentioned earlier, Richeson and Trawalter (2005) showed that racially discordant interactions often activate Whites’ need to self-regulate their behaviors in order to avoid appearing to be racist. This engagement in self-regulation depletes their cognitive resources. Because contemporary physicians are encouraged to act and treat all patients in the same way, they are likely to engage in self-regulation which in turn results in depletion of cognitive resources. Additionally, among physicians, such effects may be exacerbated by their workload. In most industrialized countries, caseloads and work demands on physicians have increased dramatically (Shirom, Nirel, & Vinokur, 2006). Thus, physicians may be more inclined to rely on stereotypes associated with their patients’ racial groups as they make diagnostic and treatment decisions in higher-stress clinical situations.
In summary, intrapersonal processes in the form of explicit and implicit race-related thoughts and feelings affect what minority patients and their physicians think and do in regard to healthcare. Although some of the theories and models we have presented have not been directly tested in healthcare settings, those that have provided substantial evidence for the utility of social psychological theory for an understanding of how intrapersonal processes can help us understand racial healthcare disparities.
Interpersonal-Level Processes
As already discussed, there is a high probability that when a member of a racial minority group sees a physician, the physician will not be a member of this group (Nunez-Smith et al., 2012). These racially discordant medical interactions are usually qualitatively different from racially concordant medical interactions. It has been shown, for example, that, relative to racially concordant medical interactions, racially discordant interactions are shorter in length (Cooper et al., 2003), less patient-centered (Johnson, Saha, Arbelaez, Beach, & Cooper, 2004), less positive (Cooper et al., 2003; Johnson et al., 2004; Street et al., 2007), and involve fewer attempts at relationship building (Siminoff, Graham, & Gordon, 2006). Furthermore, White physicians spent significantly less time planning treatment, providing health education, engaging in informal conversation, and answering questions with Black than White patients (Oliver, Goodwin, Gotler, Gregory, & Strange, 2001).
We have explored interpersonal-level processes in medical interactions in cancer treatment settings. We collected data over five years at two large comprehensive cancer centers in different regions of the US, one in Detroit, Michigan and the other in Tampa, Florida. At the center of this research are analyses of 235 video recordings of discussions between cancer patients eligible for clinical trials and their oncologists (see Albrecht, et al., 2008). Although, one might think the video recording of these interactions would affect the behavior of patients and physicians, in fact, we have found that after the first minute or so of the discussions, they pay almost no attention to the camera (Penner, Orom, Albrecht, Franks, Foster, & Ruckdeschel, 2007)
A portion of these discussions (about 30%) were racially discordant medical interactions between Black patients and their non-Black physician (either medical oncologists or oncological surgeons). Our analyses of these interactions focus primarily on communication between the parties. The studies we describe here do not contain data on either patient or physician race-related thoughts or affect. They do, however, speak to healthcare disparities. For example, we have conducted two separate kinds of analyses to compare how much information physicians provide to Black and White patients when they discuss clinical trials. In one study (Penner, Eggly, Harper, Albrecht, & Ruckdeschel, 2007) coders watched the video and used a checklist to record how many of a list of potential drug side effects were discussed with patients. Physicians were almost twice as likely to mention any side effects with White than Black patients (75% versus 45%) and, if side effects were discussed, Whites had more of them described to them than did Blacks. (The two groups of patients did not differ in education.)
Eggly, Barton, Winckles, Penner, and Albrecht (in press) conducted a discourse analysis of discussions of clinical trials with two matched (on SES) small samples of Black and White patients. In the discourse analysis, transcripts were made of all the conversations. Topic areas (a set of coherent related utterances about a main idea) were identified from the transcripts, and then the words spoken by the physician about each of these topics were counted. Overall the physicians used more words in the discussions with Whites than with Blacks, and said more words specifically about clinical trials (1867 versus 1090 words; effect size (d) = 1.06). Furthermore, physicians spoke more about the study purpose and about risks to White than Black patients (risk: 390 versus 211 words (d = .65).
We have also found that Black cancer patients are less likely than White cancer patients to receive important general information in oncology settings. Eggly et al. (2011) studied the frequency of direct questions (that is, questions that directly place the burden on the physician to respond, such as, “Will I lose my hair if I have chemotherapy?”) and indirect questions (e.g., “My sister’s hair fell out when she received chemotherapy.”). Eggly et al. found that Black cancer patients, as compared to White cancer patients, asked fewer questions, and a smaller proportion of these were direct questions (also see Gordon, Street, Sharf, Kelly, & Souchek, 2006). These findings point to the fundamentally different nature of the interpersonal exchange that occurs in racially discordant than racially concordant medical interactions.
We now consider some of the social psychological processes that may explain these effects. Because the behavior of patients and physicians is highly interdependent in medical interactions, we discuss the influence of social psychological processes on the patient-physician interaction rather than on patients and physicians separately.
Social identity
As previously discussed, the process of social categorization, which conserves cognitive resources, makes social identity more salient and provides the basis for intergroup bias (Otten & Moskowitz, 2000). According to Social Identity Theory (Tajfel & Turner, 1979), when group membership becomes salient, as often occurs in racially discordant medical interactions, people derive their self-image from the social categories to which they perceive themselves as belonging. Thus, they strive to achieve or maintain positive social group images.
Group membership is very likely to be salient in racially discordant medical interactions as racial membership (i.e., racial minorities vs. racial majorities) is one of the most frequently used features for categorizing people into different social groups. Consistent with this, Street, O’Malley, Cooper and Haidet (2008) reported that patients feel more personal and ethnic shared identity with their physician in racially concordant than racially discordant medical interactions. Several processes are associated with social identity and attempts to achieve or maintain positive social group images. We posit that these processes may contribute to racial disparities in the quality of medical interactions. Communication across group lines is often less effective than within groups not only because people are generally less accurate at perceiving expressions of emotion displayed by outgroup than ingroup members (Elfenbein & Ambady, 2002; Young & Hugenberg, 2010), but also because they are biased in their misperceptions. For instance, people are more likely to perceive a hostile face as belonging to an outgroup member (Dunham, 2011) and to misinterpret neutral facial expressions as conveying anger for outgroup than ingroup members (Hugenberg & Bodenhausen, 2004).
One way to achieve or maintain positive images of one’s own social group is to perceive, evaluate, and treat ingroup members more positively than outgroup members (i.e., ingroup favoritism) and/or outgroup members more negatively than ingroup members (i.e., outgroup derogation; see Dovidio & Gaertner, 2010). At the same time, ingroup members tend to see members of outgroups as homogeneous (Boldry, Gaertner, & Quinn, 2007) and are less trusting of them than members of their own group (Foddy, Platow, & Yamagishi, 2009). In addition, they also expect that outgroup members will be biased against them as well (Judd, Park, Yzerbyt, Gordijn, & Muller, 2005). These differential responses to ingroup versus outgroup members are likely to affect the quality of racially discordant medical interactions.
Because both patients and physicians are likely to strive to achieve or maintain their positive racial group images, they may engage in ingroup favoritism, outgroup derogation, or both. As a consequence, healthcare disparities based on ingroup favoritism would likely reflect particularly positive affect toward ingroup patients/physicians, whereas healthcare disparities based on outgroup derogation would reflect negative affect toward outgroup patients/physicians.
Divergent interaction goals
Another way to achieve or maintain positive social group images is to present oneself in a positive manner. Shelton, Richeson and their colleagues (e.g., Bergsieker, Shelton & Richeson, 2010; Shelton, Richeson, Salvatore, & Trawalter, 2005) propose that in interracial interactions, individuals’ salient social identities are each associated with different or even conflicting interaction motives or goals. Specifically, in such interactions, participants from racial majority groups may be concerned with not appearing to be prejudiced, while racial minority participants may be equally concerned with not being the target of prejudice or discrimination (Richeson, Trawalter, & Shelton, 2005; Shelton et al., 2005) and/or not confirming racial stereotypes (Bergsieker, et al., 2010). In support of this latter proposal, Bergsieker et al. (2010) found that Latinos and Blacks, but not Whites, were much more concerned with being respected and seen as competent when they were in racially discordant dyads than in racially concordant ones. These divergent interaction goals of majority and of minority participants may undermine effective communication between them. For example, in a recent analysis of physician-patient interdependence in racially discordant medical interactions Hagiwara, Kashy and Penner (under review) found that non-Black physicians’ perceptions of the extent which they and their Black patients were working as a team during a medical interaction were essentially orthogonal to the patients’ perceptions of “teamness.” This kind of lack of convergence in perceptions of the interaction is seen by many researchers as a major cause of disparities in minority use of healthcare services (Ashton et al., 2003).
Additionally, when individuals are concerned with self-presentation, they often engage in self-regulation. As described above, self-regulation requires cognitive resources as individuals try to monitor for undesirable behaviors while executing more desirable behaviors during medical interactions. Because cognitive resources are limited, individuals engaging in self-regulation often are unable to attend to other tasks (Engle, Conway, Tuholski, & Shisler, 1995; Hartley & Adams, 1974; Muraven & Baumeister, 2000). This self-focus may result in individuals appearing to lack interest in their interaction partners. For instance, Shelton et al. (2005) found that when Whites self-regulated their behaviors, apparently to avoid appearing biased, Blacks interpreted this excessive self-regulation as a lack of interest in them. These findings suggest that divergent interaction goals of minority patients and majority physicians and their attempts at self-regulation to attain these goals could result in ineffective communication during medical interactions. Poor communication during the medical interaction, in turn, could also result in more negative feelings after a medical interaction, even if these feelings did not exist prior to the interaction. Some empirical support for this conjecture comes from Gordon et al. (2006), who studied trust among Black and White lung cancer patients. Gordon and colleagues reported that while the two groups did not differ on trust of the oncologists prior to the interaction, Black patients had lower post-visit trust than White patients. Patient perceptions of how the physician communicated with them (e.g., how informative, how supportive the physician was) predicted post-visit trust.
Intergroup anxiety and stress
Intergroup anxiety and stress is another process that may also shape racially discordant medical interactions. The theory of intergroup anxiety proposed by Stephan and Stephan (1985) also provides a possible explanation for why the quality of racially discordant medical interactions is often poorer than that of racially concordant ones even when physicians and patients may not hold negative attitudes toward and/or perceptions of one another. According to the intergroup anxiety theory, people’s expectations that their interactions with outgroup members can go wrong can often result in intergroup anxiety. This general negative arousal, in turn, may result in a desire to minimize interactions with outgroup members or even in hostility toward outgroup members (Islam & Hewstone, 1993).
However, as already noted, physicians and patients often cannot avoid racially discordant medical interactions. Thus, racially discordant interactions may often be awkward, threatening, and distressing (Trawalter, Richeson, & Shelton, 2009; Shelton, West, & Trail, 2010). Indeed, Trawalter et al. (2009) propose that people’s behavior in racially discordant interactions can be understood as “initial stress reactions and subsequent coping responses” (p. 243). Under such circumstances, the choice of how to cope with this stressor depends on whether the person sees the situation as a challenge or a threat (Blascovich, Mendes, Hunter, Lickel, & Kowai-Bell, 2001). If people feel they have enough resources to cope with the stressor, they are likely to perceive the stressor as a challenge and respond in an effective, productive manner. By contrast, if people believe they do not have enough resources to cope with the stressor, they see it as a threat and their response is likely to lead to a negative and unproductive interaction. Threatened individuals may, depending on perceived resources, antagonize their partner, psychologically withdraw from the interaction, or as suggested above, overcompensate (Trawalter et al., 2009). All of these responses are consistent with the descriptions of racially discordant medical interactions provided earlier in this section.
Explicit and implicit attitudes
Much of our own recent research has focused on the influence of physicians’ implicit attitudes, both directly and in combination with their explicit attitudes, on the interpersonal-level dynamics of medical encounters. As we have already discussed, race-related thoughts and feelings can affect non-Black physician and Black patient healthcare-related thoughts, feelings, and actions independent of actual interactions between them. In this section, we consider how race-related affect and cognitions can affect the quality of racially discordant medical interactions. We illustrate several of these processes with our own research in this area, which highlights the distinction between explicit and implicit racial bias. As already noted, although there is typically an association between explicit and implicit processes, this association is often rather small. Furthermore, explicit and implicit racial bias can influence behaviors in different ways (Bargh, 1999; Dovidio & Fazio, 1992; Fazio, 1990). More specifically, explicit bias generally predicts deliberative, controllable behaviors, whereas implicit bias generally predicts spontaneous behaviors that are hard to monitor and control (Chen & Bargh, 1997; Dovidio, Kawakami, & Gaertner, 2002; Wilson et al., 2000). Thus, individuals may not be able to self-regulate undesirable behaviors stemming from implicit bias, which would affect their interactions with people who are the object of this bias.
The impact of implicit physician bias on racially discordant medical interactions has been the focus of much of our research on health disparities. Earlier, in the section on intrapersonal-level processes, we briefly discussed two findings from our research at the primary care clinic showing that if Black patients report experiencing more racial discrimination in their everyday life (Penner et al., 2009) and/or feeling less trust in physicians (Hagiwara et al., 2013), they are less likely to adhere to a non-Black doctor’s medical recommendations. In this section, we discuss a series of studies related directly to interpersonal-level processes that draw on various measures in the longitudinal database collected on this sample of Black patients and their physicians at the clinic. Thus, we offer more details of the social environment and research procedures to provide a context for the work.
The clinic is in the inner city of Detroit, Michigan. The great majority of Detroit residents self-identify as Black/African American, and Detroit is one of the most racially segregated cities in the US (US Census: http://www.census.gov/2010census/). Over two years, we recruited 156 Black patients at the clinic. (There were three non-Black patients at the clinic during this time, and their data were excluded from the analyses). The sample was predominantly female (76%), and all patients had health insurance. Participants were of quite low SES: 45% had annual family incomes of less than $20,000 USD, which is below the official US government “poverty level” for a family of four (US Census http://www.census.gov/hhes/www/poverty/data/threshld/). Another 30% had family incomes of less than $40,000, and almost 30% had less than 12 years of formal education (i.e., did not graduate from an American high school). There were no systematic effects for patient SES across our studies, perhaps in part due to the limited range of income in the patient sample. The physicians were 19 medical residents. Most were East Asian, which is quite common in the US for primary care clinics in low SES minority communities (IOM, 2003). Ten of the physicians were women.
Patients were approached by a Black research coordinator when they arrived for a scheduled medical appointment; 73% agreed to participate. After being consented, patients provided demographic information and completed the measures that have already been described (i.e., experience with discrimination, Brown, 2001; trust in physicians, Dugan, et al. 2005; past adherence with physicians’ recommendations, Hays et al. 1994; and self-reported health, Ware et al., 1992) before they saw their physician.
Patients then interacted with the physician. One hundred and thirty-six of these interactions were video recorded. Immediately following the interaction, patients completed several measures, including a 14 item measure of the extent to which they believed the physician was patient-centered (e.g., “How much did the doctor seem interested in you as a person”; Stewart et al., 2000), and their perceptions of physician warmth/coldness, and their satisfaction with the encounter (“Overall how satisfied were you with today’s visit with the doctor?”). The patients also answered items about trust in the physician they had just seen (e.g. “All in all, I have complete trust in this doctor,” Dugan et al. 2005) and two items that measured team perceptions (“The doctor and I worked together as a team to solve our medical problems”; “I felt like the doctor and I were members of the same team trying to solve my medical problems.”)
As already noted, four and sixteen weeks after the interaction, we sent patients mail questionnaires asking them about their health (Ware et al., 1992) and their adherence to their own physician’s recommendations (Hayes et al., 1994). Patients also received the measures of physician-specific and general trust (Dugan et al., 2005). (Attrition across all the data collection points was relatively low (about 35%) and controlling for attrition did not change any findings that we report.
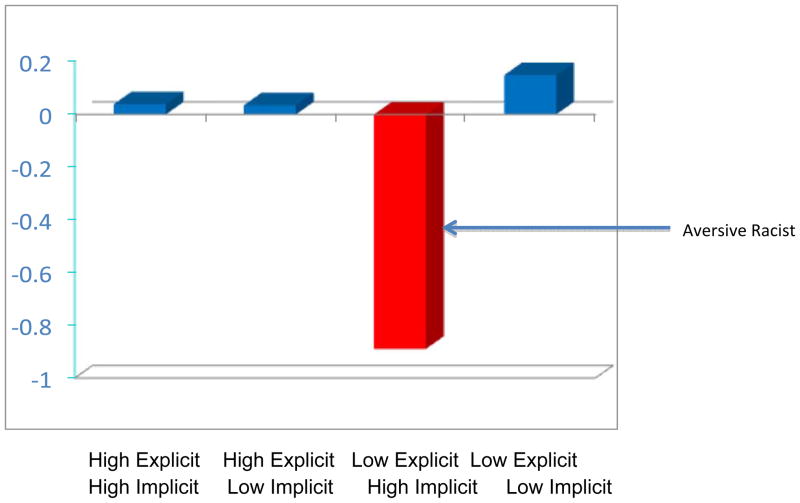
When the physicians enrolled in the study, they provided demographic information, and 15 of them completed measures of explicit racial bias (a combination of racial attitude items from scales by Brigham, 1993, and McConahay, 1986) and a race-based Implicit Association Test (IAT; Greenwald, Nosek, & Banaji, 2003). Immediately after the interactions, physicians completed two team items parallel to those completed by the patients.
To examine the dynamics of the interpersonal-level processes in these medical interactions, we (Hagiwara et al., 2013) used the video recorded interactions to examine the amount of time physicians and patients each talked during the interactions; then they computed ratios of physician to patient talk time (i.e., physician-patient talk time ratio). Relative talk time was chosen for several reasons. First, relative talk time is considered a valid measure of participants’ motivation to dominate an interaction (Dovidio, Brown, Heltman, Ellyson, & Keating, 1988; Mast, 2002). Second, there is clinical significance to the relative amount of time patients and physicians talk during medical interactions because it is believed to be related to health care outcomes, such as patient satisfaction and adherence. For example, according to the Patient-Centered Communication Model (Stewart et al., 2000), greater physician talk time is associated with less patient satisfaction and adherence, while greater patient talk time is associated with more satisfaction adherence (e.g., Hahn, 2009). (However, as Hagiwara et al. noted, these relationships have not been specifically tested in racially discordant medical interactions.) And third, people are better at self-regulating how explicit racial bias is manifested in more planned behaviors than they are at regulating how implicit racial bias is manifested in more spontaneous behaviors (Dovidio & Gaertner, 2004). Thus, how much time physicians talk (a relatively spontaneous behavior that nay not be strongly self-regulated) may systematically reflect physicians’ implicit racial bias.
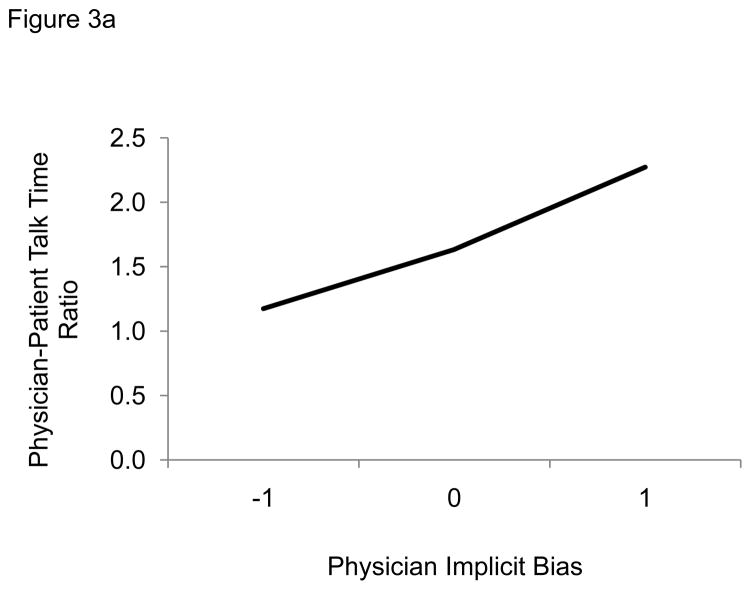
Overall physicians talked more than patients. In addition, as expected, we (Hagiwara et al., 2013) found that physicians’ implicit, but not explicit, levels of racial bias influenced the physician-patient talk time ratio. The higher the level of physicians’ implicit racial bias, the more they talked relative to physicians with lower levels of implicit bias (see Figure 3a). That is, more implicitly prejudiced physicians dominated the medical interaction more verbally. Cooper et al. (2012) reported convergent findings for a separate sample of medical interactions. Hagiwara et al. (2013) speculated that physicians with higher levels of implicit bias harbor negative attitudes toward and stereotypes about Black patients (as discussed earlier, they may see Black patients as less compliant and trustworthy), which might lead them to want to exert more control during interactions with them. This is manifested in the association between their implicit bias and how much they talked relative to their patients.
Figure 3.
Figure 3a Physician Implicit Bias and Ratio and Patient to Physician Talk Time Ratio*. Copyright © 2013 Elsevier. Racial attitudes, social control, and adherence in racially discordant medical interactions. Hagiwara, N. et al., Social Science and Medicine, 87, 123–131.
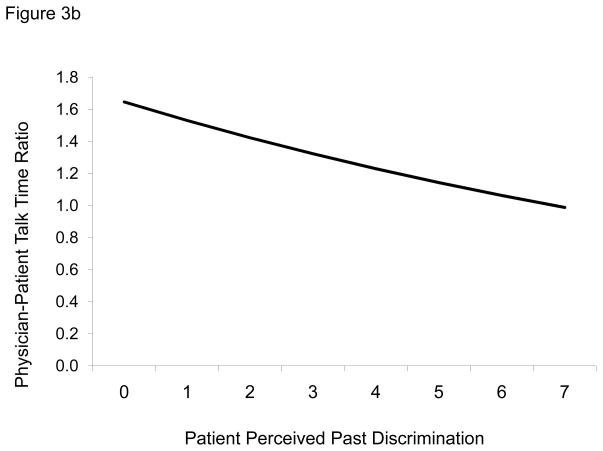
Figure 3b Patient Perceived Past Discrimination and Patient to Physician Talk-Time Ratio*. Copyright © 2013 Elsevier. Racial attitudes, social control, and adherence in racially discordant medical interactions. Hagiwara, N. et al., Social Science and Medicine, 87, 123–131.
Figure 3 Caption Overall physicians talked more tan patients (ratio >1); the larger this ratio, the more physicians talked relative to patients.
In the same study, we also examined the impact of patients’ reports of previous experiences of discrimination by Whites on physician-patient talk time ratio. As seen in Figure 3b, the greater perceived past discrimination patients reported, the smaller was the physician-patient talk time ratio; that is, participants who reported experiencing high levels of previous discrimination talked more than those who reported experiencing low levels of discrimination. The same pattern was observed for trust—the less the trust, the more the patients talked. At first glance, these findings seem inconsistent with a patient-centered perspective on medical interactions (Epstein & Street, 2007; Hahn, 2009). In attempting to explain this inconsistency, Hagiwara et al. argued that greater patient talk time may not always reflect positive patient reactions to medical interactions. Specifically, we proposed that in racially discordant medical interactions Black patients may fear that, based on their prior experiences with bias and mistrust of the physician, they may become the victims of discrimination. They therefore attempt to assert more control in their medical interactions to achieve higher quality care. Indeed, consistent with this interpretation of greater talk-time among Black patients, we found that the smaller the ratios (i.e., more patient talk time relative to the physicians), the less they subsequently adhered to physician recommendations (see Hagiwara et al., 2013).
We acknowledge that patient-centeredness is a valid and desired goal for all medical interactions, but propose that the behaviors associated with patient-centeredness may differ between racially concordant and racially discordant medical interactions. As, Shelton, West, and Trail (2009) have shown, sometimes exactly the same behaviors may be viewed in different, frequently opposite, ways in same-race interactions and different-race interactions. Thus, our research further highlights the importance of recognizing and understanding how the distinctive dynamics of racially concordant and discordant interactions can affect medical encounters and outcomes.
Physicians’ racial prejudice, implicit and explicit, can have a direct negative impact on the experience of Blacks in medical encounters, and ultimately on the quality of care that Blacks receive. For example Cooper et al. (2012) found that higher implicit physician bias was associated with less positive affect and poorer ratings of interpersonal care from Black patients. Similarly, Blair et al. (2013) found that higher physician implicit bias was significantly associated with lower patient-centered care as reported by Black patients. (Interestingly this relationship was not found among Latino patients.)
In our own work, we have examined how the interaction between explicit and implicit bias may affect Black patients’ reactions in racially discordant medical interactions. This study again uses data from participants in the primary care clinic, specifically the 15 physicians who completed the measures of explicit and implicit racial bais and the patients they saw. This work was based on Aversive Racism Theory (Dovidio & Gaertner, 2004; Gaertner & Dovidio, 1986). Aversive racism theory proposes that racial majorities often hold positive explicit, conscious thoughts about and feelings toward racial minorities that are consistent with their egalitarian values. However, at the same time they also hold negative implicit, nonconscious thoughts about and feelings toward these minorities, resulting in discomfort from the dissociation between their explicit egalitarian values and their implicit negative feelings toward racial minorities and their fear of appearing to be a racist.
In order to alleviate their discomfort and fear, individuals characterized by aversive racism (i.e., low explicit-high implicit bias) tend to avoid or disengage from racially discordant interactions, often without conscious awareness of the reasons for their behavior (Dovidio & Gaertner, 2004; Gaertner & Dovidio, 1986). However, people often cannot avoid certain racially discordant interactions. Once engaged in these interactions, people who fit the profile of an aversive racist may display inconsistent behaviors because they can self-regulate deliberate behaviors that are usually associated with explicit attitudes (e.g., verbal behaviors) while they have difficulties self-regulating automatic behaviors that are usually associated with implicit attitudes (e.g., nonverbal behaviors). These inconsistent behaviors may elicit negative reactions from members of racial minority groups (Dovidio et al., 2008). Although the phenomenon of aversive racism was first demonstrated in the context of White Americans’ response to Blacks, it has subsequently been found with other target minorities in countries such as Canada, the UK, and the Netherlands (Hodson, Hooper, Dovidio, & Gaertner, 2005; Kleinpenning & Hagendoorn, 1993; Son Hing, Chung-Yan, Hamilton, & Zanna, 2008).
The negative consequences of aversive racism may be especially relevant to racially discordant medical interactions, because for legal and ethical reasons, physicians cannot typically avoid racially discordant medical interactions. Research on Blacks’ reactions to racially discordant social interactions (Dovidio et al., 2008; Hebl & Dovidio, 2005) led us to examine whether physicians who fit the profile of an aversive racist may elicit negative reactions from racial minority patients. In this study (Penner et al. 2010b), we used the scores on the explicit and implicit racial bias measures described above (i.e., the racial attitudes scale and the IAT) to identify physicians who, relative to other physicians, showed the aversive racism profile – that is, low explicit and high implicit bias. We also computed a composite measure of patients’ perceptions of the patient-centeredness of the interaction, including the items about patient satisfaction and perceived doctor warmth. We then compared differences in patients’ experiences in the interactions with physicians reflecting the four configurations of explicit and implicit physician bias: (a) high explicit/high implicit (i.e., high prejudiced physicians), (b) high explicit/low implicit, (c) low explicit/high implicit (i.e., aversive racists), and (d) low explicit/low implicit (i.e., low prejudiced physicians).
We found that physician explicit bias affected their own perceptions of being on a team with the patients (i.e., higher bias, less perceived teamness), but had no impact on patient reactions. However, as can be seen in Figure 4, Black patients who interacted with the aversive racist physicians were less satisfied with the interaction and felt less positive about and close to their physicians than Black patients who interacted with other physicians, including physicians who were high on both explicit and implicit bias. We have also found, using just the patients who completed the trust measures, that patients trusted the “aversive racist” physicians significantly less than the other physicians.
Figure 4.
Physician Aversive Racism and Black Patients’ Positive Reactions to Medical Interaction*. Copyright © 2010 Elsevier. Aversive racism and medical interactions with Black patients: A field study. Penner, L. A., et al., Journal of Experimental Social Psychology, 46, 436–440.
*Figure 4 Caption Patient reactions is a composite of patient satisfaction and perceptions of their physician (e.g., warm, friendly).
Turning to the issue of the role of patient attitudes, we know that patient behavior affects how physicians communicate with them; for example, contentious patients elicit contentious communication from their physician (Street et al., 2007). We know of no published work on how patient race-related attitudes/beliefs may affect physician reactions to them; however a subsequent analysis of our original patient-physician data (Hagiwara et al., under review) suggests there may be such a relationship. In this analysis of physician-patient interdependence in the racially discordant medical interactions, we examined the impact of patients’ experience with discrimination on their physician’s reactions to the interaction. We found the more past discrimination patients reported, the less likely their physicians were see the two of them as a team.
To summarize, at the interpersonal level, racially discordant, relative to racially concordant, medical interactions are typically characterized by poorer communication and more negative affect. Social identity theory may provide a general theoretical framework in which to place many of these negative outcomes. Social identity processes can influence the quality of racially discordant medical interactions through several paths. People tend to engage in ingroup favoritism and/or outgroup derogation, which may explain why racial majorities are more likely than racial minorities to have positive medical interactions. Theories of how individuals self-regulate their behaviors to achieve interaction goals as well as how individuals cope with the stress associated with interracial interactions may provide further insight into why these interactions often have less than positive outcomes even in the absence of obvious intergroup bias. Contemporary research on explicit and implicit racial attitudes suggests that these attitudes affect the quality of these interactions and, indeed, our own work provides substantial support for this. Perhaps the most intriguing finding in this regard is that although we currently do not know exactly what behaviors they are reacting to, Black patients are very good at detecting implicit bias among their physicians and react negatively to it. Their dissatisfaction and distrust are directly negatively linked to the likelihood they will adhere to the treatment recommendations their physicians make (Hagiwara et al., 2013; Penner et al., 2013) and thus how much they may benefit from a medical interaction.
Thus, as was true with intrapersonal processes, social psychological theories of processes that occur at the interpersonal (or face-to-face intergroup) level seem to be quite useful in understanding racial healthcare disparities. In the final section of this article we consider how these theories may be used to develop effective interventions to reduce these disparities.
Social Psychological Approaches to the Reduction of Healthcare Disparities
In this section we consider ways to address healthcare disparities at the intrapersonal and interpersonal levels. We acknowledge that interventions at the societal level (e.g., increasing the number of racial minority physicians) are critical and necessary to fully address healthcare disparities. However, discussion of these societal-level interventions is beyond this review’s scope. Following a key distinction in our model (depicted in Figure 1), this section is divided into interventions at the intrapersonal and interpersonal levels. In other words, we consider interventions based on social psychological theory and research that may effectively improve the quality of racially discordant medical interactions. At the outset, we must acknowledge the relative dearth of interventions that specifically target racially discordant medical interactions. We shall present these and where appropriate also discuss possible interventions that draw on social psychological theory and research. We discuss two general kinds of interventions. One kind is interventions that target negative stereotypes and attitudes towards all members of some racial minority. The goals of such interventions we describe are to produce general changes in physicians and patients that might affect healthcare disparities. The other kind is interventions that target a specific racially discordant interaction. Their goal is to improve the outcome of these interactions by reducing the impact of negative race-related thoughts and feelings of the specific patient and/or physician participating in the interaction. One might hope that these effects might generalize beyond this interaction, but our primary goal is much more modest. We simply want to reduce healthcare disparities in that interaction.
Intrapersonal Level Processes
In this section we focus on potential interventions that target the race-related thoughts and feelings patients and physicians may bring to racially discordant medical interactions. First we consider the racial minority patients.
Racial minority patients
Interventions with racial minority patients have focused on both cognitive and motivational processes. Specifically, these interventions have addressed patients’ expectations of bias and the health consequences of identity-based motivations.
Members of both racial majority and minority groups approach interracial interactions guardedly and with negative expectations (Mallett, Wilson, & Gilbert, 2008). When racial minority members expect to be treated unfairly by a majority group member in racially discordant interactions, they experience negative moods and/or interaction anxiety and may become defensive during the interactions (Butz & Plant, 2006; Shelton et al., 2005). Therefore, one target for interventions is to reduce the impact of these expectations on racially discordant medical interactions.
As noted earlier, Burgess and colleagues (2010) proposed that one manifestation of racial minority patients expecting to be the target of prejudice and discrimination is the activation of stereotype threat, wherein minority group patients may worry that their physicians may negatively stereotype them. Thus, minority patients may not fully and actively participate in the interaction, lest they engage in behaviors that might reinforce these stereotypes. Recently, Havranek et al. (2013) tested the impact of an intervention intended to reduce stereotype threat among minority patients on the patients’ reactions to racially discordant medical interactions. In this study, patients were randomly assigned to either a treatment group, in which they engaged in a values-affirmation exercise shortly before they met with their physician, or to a control group. Values-affirmation exercises encourage people to identify personal values that are important to them. Such exercises have been shown to reduce stereotype threat, presumably due to the positive impact on the self (Burson, Crocker, & Mischkowski, 2012). The interactions were audio recorded. Patients who engaged in the values affirmation exercise asked for more information about their medical condition during the interactions and reported a less negative mood after the interactions, as compared to patients in the control group. Additionally, independent coders rated these patients as more friendly and responsive during the interactions.
The goals of medical interactions extend beyond accurate diagnosis and the best treatments. Today, most medical facilities also emphasize steps that people can take to prevent diseases. Indeed, there is already a very large public health and communication literature on persuasive messages that target and attempt to change health-related beliefs and behavior (Thompson, Dorsey, Miller, & Parrott, 2008). Recently, communication researchers have proposed that health messages should be tailored based on the target’s social identity (McQueen & Kreuter, 2010). This approach is based primarily on classic models of persuasive communication (e.g., increasing source credibility and/or the relevance of the persuasive message).
We would suggest another approach based on Oyserman and colleagues’ report of their efforts to change identity-based motivations in middle school students. Oyersman, Bybee, and Terry (2006) targeted racial minority students’ self-concepts, social identity, and academic achievement. They developed classroom exercises aimed at connecting students’ “possible selves” (i.e., how they see themselves in the future) and their social identity. Specifically, the classroom exercises encouraged minority students to see their “possible selves” as congruent with a social identity that was associated with academic success. The primary means to do this was to have students think about another student and/or adult with whom they identified, who provided a model of their academically successful possible self. This intervention was successful and had substantial long-term academic consequences for the students. For example, relative to comparable students who did not receive the intervention, the targeted students had fewer school absences and higher grades and scores on standardized tests. Moreover, these effects persisted over time. It would seem useful to explore whether similar interventions that target self-concept and social identity might be developed for health-related behaviors among racial minorities.
Physicians
At both explicit and implicit levels, non-minority physicians tend to harbor negative feelings towards members of racial minorities and hold negative stereotypes about minority patients. Thus, interventions that target these attitudes and beliefs might serve to reduce healthcare disparities.
These interventions target people’s general stereotypes and attitudes that affect reactions to some target group, including their thoughts, feelings, and actions when they interact with members of that group. Burgess and colleagues (Burgess, van Ryn, Dovidio, & Saha, 2007) argued that changes in physician training will reduce the impact of ingroup bias and race-related stereotypes and attitudes on healthcare. Most medical schools (at least in the US) now require training in “cultural competency”—“a set of attitudes, skills, behaviors and policies enabling individuals to establish effective interpersonal and working relationships that supersede cultural differences” (Price et al., 2005, p. 578). The term cultural competency training covers a host of different approaches, but in the training models that have been empirically evaluated, do not directly address intergroup relations or racial bias (Lie, Lee-Ray, Gomez, Bereknyei, & Braddock, 2010). Burgess et al. (2007) recommended teaching medical trainees about the nature of stereotyping, thus increasing their understanding that even negative stereotypes are a pervasive social phenomenon that can unintentionally shape medical decision making and interactions. This type of training should help them to devise strategies to counteract stereotypes rather than try to deny or suppress them. At a conceptual level, we would agree that such an approach has value. In fact, this approach is consistent with findings from the social psychological literature showing that, with some practice, people can develop strategies to counteract the influence of implicit racial bias on their explicit thoughts, feelings, and actions (e.g., Monteith, Arthur, & Flynn, 2010). However, given the other demands on medical education to prepare trainees for the current rapidly-changing healthcare environment, these kinds of programs will need to be integrated into already crowded medical curricula, which may make them less feasible or effective.
Although it may be difficult to directly address medical trainees’ race-related thoughts and feelings through special training, it might be possible to modify the training experience in ways that reduce racial stereotypes and the anxiety and uncertainty that often accompanies interracial interactions. Allport’s (1954) classic contact hypothesis suggests some strategies. Repeated positive and constructive contact between ingroup and outgroup members can often reduce implicit and explicit negative attitudes and beliefs about members of an outgroup, as well as negative affective reactions (e.g., anxiety, discomfort, uncertainty) that often accompany interacting with members of the outgroup; and thus improve intergroup relations (Brewer & Miller, 1984, Tausch & Hewstone, 2010; Voci & Hewstone, 2003). So, one way to reduce physicians’ negative race-related feelings during racially discordant medical interactions is to provide them with multiple opportunities to interact with minority patients during their training. This could be done in the context of a widely used training tool in medical schools--interactions with “standardized patients” (i.e., actors hired to play the role of patients). That is, one possible way to give medical students experience with minority patients is simply to increase the diversity of the standardized patients they see, and provide feedback that specifically addresses those aspects of the interaction that concern intergroup relations.
It might also be useful to provide students with behavioral scripts before these interactions. This approach is suggested by a study by Avery, Richeson, Hebl, and Ambady (2009) that found providing Whites with behavioral scripts to follow before their interactions with Blacks significantly reduced their anxiety during the interactions. This might serve to desensitize non-minority physicians to minority patients early in their medical training.
It would also be beneficial to provide non-minority medical students with naturally occurring contact with equal or higher status individuals from racial minorities, such as minority medical students or medical school faculty. However, only a small portion of medical students are from racial minorities, and minorities are also substantially under represented on medical school faculties (Nunez-Smith et al., 2012). One possible reason is for this is that, at least in the US, minority medical school faculty members have significantly lower promotion rates than White faculty (Nunez-Smith et al., 2012). This limits the opportunities for White students and faculty to have contact with equal or higher status minority group members.
Other interventions might attempt to reduce physicians’ reliance on racial stereotypes when they interact with racial minority patients. For example, one might attempt to reduce the cognitive load of physicians whose practices involve a high percentage of racial minority patients. Laboratory studies of racially discordant interactions suggest that Whites under low cognitive load are less likely to engage in social categorization and more able to individuate their interaction partner than those under high cognitive load (Bodenhausen & Wyer, 1985). Thus, interventions might be developed to increase physicians’ cognitive resources by reducing the stress and anxiety associated with their clinical practice. This might involve organizational interventions, such as reducing patient caseloads through the use of nurses or other physician “extenders.” Of course, given the fiscal realities of medical practice in the 21st century in almost all countries, it seems that such changes in organizational practice will not be easy to achieve.
Interpersonal Level Processes
We have argued that one major reason for the less productive and positive communication in racially discordant medical interactions involves the social biases that physicians bring, often without conscious awareness, to these formal encounters. Basic social psychological research and theory can help guide the development of interpersonal-level interventions to reduce healthcare disparities. In this section, we consider strategies for structuring racially discordant medical interactions and reshaping social categorization processes to enhance the effectiveness of racially discordant medical interactions.
Creating equal status in racially discordant medical interactions
A meta-analysis conducted by Pettigrew and Tropp (2006; see also Pettigrew & Tropp, 2011) testing Contact Theory reveals that intergroup contact, and particularly under conditions of equal status, common goals, acquaintance potential, and support of authorities, has beneficial effects on intergroup attitudes. Within medical contexts, the Patient-Centered Communication Model of physician communication (Stewart et al., 2000), which is widely taught in North American and European medical schools (Mead & Bower, 2000), may serve to promote these facilitating conditions, especially equal-status relations. Whereas physician-patient interactions have traditionally reflected marked status distinctions, the Patient-Centered Communication Model stresses the need for physicians to understand the patient’s perspective, consider the patient’s psychological and social context, reach a shared understanding of the patient’s problem and its treatment, and offer patients meaningful involvement in treatment decisions (Epstein & Street, 2007). A central goal of patient-centered physician communication is to empower patients to participate actively in medical interactions. Research shows that patient-centered medical interactions produce more patient involvement and more positive outcomes (Epstein & Street, 2007).
However, as we have already noted, the effects of patient-centered communication have not been systematically examined in the context of racially discordant medical interactions. Moreover, our own research suggests that greater patient participation may not always reflect physicians empowering patients. Recall that Hagiwara et al., (2013) found that Black patients who perceived greater past discrimination and reported less trust talked more in their medical interactions with non-Black physicians. This suggests that this behavior may have reflected negative rather than positive affect. As a consequence, in these racially-discordant interactions, greater talk-time by patients predicted less subsequent adherence to the doctor’s recommendations. Thus, while patient-centered communication may have value in improving the outcomes of racially discordant medical interactions, it needs to be empirically evaluated before being implemented as a remedy for the problems associated with these interactions.
One intriguing, but as yet untested, idea for an intervention to create optimal conditions for racially discordant medical interactions is to try interventions modeled on Aronson’s Jigsaw Technique (see Aronson, 2008). The Jigsaw Technique was designed to reduce intergroup conflict in small groups and emphasizes the importance of each individual’s participation and of the information each has in the solution of a problem of mutual interest. This technique can create equal status among the participants. Although this technique was originally developed to improve diverse classroom environments, it might be meaningfully modified for medical interactions. For example, framing the medical interaction as one in which each party has valuable information that the other one needs to solve the “problem” (i.e., find the correct diagnosis and best treatment plan) might engender a more equal status, cooperative interaction than is the norm in racially discordant interactions. It would seem worthwhile to explore this approach to improving racially discordant medical interactions.
The optimal conditions identified by Contact Theory and the dynamics of the Jigsaw Technique operate to reduce intergroup bias by altering the ways people in these interactions socially categorize others2. As already discussed, because of the importance of race and ethnicity in social relations generally, people automatically and often unconsciously respond to others primarily based on their race or ethnicity, which can negatively affect racially discordant medical interactions. Thus, one possible avenue to prevent such outcomes in interactions is to reduce the likelihood that participants automatically categorize themselves as members of two different groups. Specifically, positive intergroup contact and cooperative interdependence, as identified by Contact Theory and the Jigsaw Technique, can alter physician and patient perceptions of membership in an ingroup and in an outgroup based on race/ethnicity to more individuated perceptions of one another and/or to recognition of a shared identity within the context of a specific medical interaction.
To the extent that social categorization processes are a critical factor biasing perceptions and interpersonal-level processes in racially discordant medical encounters, interventions targeted more directly at changing the nature of social categorization can help eliminate healthcare disparities. In the remainder of this section, we discuss interventions designed to create more individuated impressions or common-group representations (versus different racial/ethnic categories) in medical encounters.
Individuation of participants in racially discordant medical interactions
Several models of intergroup relations (e.g., Brewer, 1988; Fiske, et al., 1999) posit that people do not categorize others into specific social categories when they are provided with rich individuating information about target individuals. For instance, Turner, Hewstone, and Voci (2007) have shown that self-disclosure among members of different groups is associated with an increase in positive attitudes and more heterogeneous perceptions of members of the outgroup. Consistent with these research findings, Burgess and colleagues (2007) specifically argued that individuation of a minority patient is an effective way to reduce the impact of race-related thoughts/feelings on physician reactions to that patient.
We are currently testing an intervention (Eggly et al., 2013) that is partially intended to help individuate racial minority cancer patients in the eyes of their oncologists. Prior to meeting the oncologist, minority patients are provided with a list of questions they might ask their non-minority oncologists during discussions of their treatment and given advice on the best way to ask them. We believe that patients asking more questions about their specific condition and treatment will activate more individuated impressions of minority patients during the interactions. In addition, asking these questions provides an example of an engaged, interested patient that contrasts with documented physician expectations that minority patients are unintelligent, uninterested or uncooperative (Green et al. 2007; Sabin, et al., 2008; van Ryn & Burke, 2008). The patient may be seen as an exception to the social category, thus diminishing the impact of pre-existing stereotypes on the oncologists’ views of the patient. As a result, treatment decisions will be more likely to be based on the particular characteristics of this patient than stereotypes about the group to which he/she belongs.
In the same vein, previous research reveals that minority cancer patients typically receive less information from their oncologist (Eggly et al., 2011), which may reinforce minority patients’ stereotypes about nonminority physicians as not interested in or biased against them (Johnson et al., 2004). Thus, we posit that this intervention will have cascading positive influences on racially discordant medical interactions. Helping patients to ask more questions is expected to elicit greater responsiveness from oncologists, which, in turn, should (based on the psychological literature) undermine patients’ negative stereotypic perceptions, at least with respect to this particular healthcare provider. That is, greater responsiveness in the encounter by oncologists may serve to individuate the oncologists to the patients and thus reduce the impact of the patients’ race-related thoughts and feelings on the interaction itself and the treatment decisions patients make. Note that this intervention would not really address the general attitudes and stereotypes that either oncologists or patients bring to the interactions, but it might reduce the relevance of these feelings and thoughts to communication during their immediate interactions and the decisions each party makes.
Of course, one could simply provide physicians and patients with large amounts of information about one another prior to the interactions, which might also serve to individuate them. However, promoting individuation by providing patients and physicians detailed information about one another may not be practical. Physicians may not be willing or able to invest great amounts of their very limited time exchanging individuating information with their patients; similarly, patients may not be willing or able to learn about their physicians as individuals. Furthermore, the stressful aspects of racially discordant interactions (Richeson & Shelton, 2007) and the time pressures and heavy workload for many physicians who treat minority patients may increase the cognitive load on such physicians.
Under these conditions attempts at individuation via increased information may actually have counterproductive effects. For example, Phillips, Northcraft and Neale (2006) studied homogeneous and diverse groups working on a complex problem. They found that individuating members of diverse groups with information about similar attitudes and values did not increase attraction among them and, in fact, actually resulted in poorer performance relative to diverse groups that did not receive this information3. These findings suggest that one might be cautious in providing large amounts of individuating information during already cognitively taxing racially discordant medical interactions because this information may further increase the cognitive load. Under such circumstances, physicians may actually fall back onto racial stereotypes to reduce the cognitive load.
Creating a common identity in medical interactions
Another, possibly more productive, way to improve the outcomes of racially discordant medical interactions might be to try to change patients’ and physicians’ perceptions of one another as “us” versus “them.” Social psychological research has shown that it possible to do this by creating a common group identity, in which members of disparate groups are induced to focus on their common interests and goals they share in common (e.g., Gaertner & Dovidio, 2009; Gaertner, Dovidio, & Houlette, 2010). The creation of a common group identity has been found to reduce intergroup bias and increase intergroup trust.
In a recent study (Penner et al., 2013), we attempted to improve the outcomes of racially discordant medical interactions by creating an intervention to promote common group identity between the low SES Black patients and their non-Black physicians in our samples in the Detroit clinic. Prior to their appointment with their primary care physicians, 72 Black patients completed all the baseline measures described above (e.g., general trust, adherence) and then were randomly assigned to a treatment group or control group. The 42 patients in the treatment group received written instructions that introduced the concept of being on a team with their doctor. They were asked to sign a contract stating that they would be “partners in a team that is working to solve your medical problems.” To reinforce this message, treatment-group patients were given buttons and pens with the team name and team colors. Patients also received 10 suggestions for being part of a team, which were posted on the wall of the room in which the treatment-condition patients saw their physician. The 30 patients in the control group received their usual standard of care. The 7 physicians randomly assigned to the treatment condition received similar instructions at the beginning of the study and wore the same kind of buttons during the interactions. Each physician interacted with multiple patients across the course of the study. Patients completed the measure of physician specific trust and the two team items immediately after the interaction; 4 and 16 weeks later they completed the trust measures again and the adherence measures. In all the tests of treatment- control differences, we controlled for baseline trust and adherence measures.
As illustrated in Figure 5, we found that relative to the control group, patients who received the common identity manipulation showed increased trust in their physicians and in physicians in general at four and 16 weeks after the interactions. Perhaps more importantly, 16 weeks after the interactions, members of the intervention group adhered to physician recommendations significantly more than did members of the control group. These findings reveal the important role of changing the way physicians and patients think of each other during their medical interactions – from “us” and “them” based on their racial or ethnic group memberships to “we” in terms of their relationship in this medical context – on healthcare success. Understanding the psychological mechanisms that underlie intergroup bias can thus help guide the development of interventions to improve the effectiveness of medical encounters in ways that particularly benefit minority-group patients, thereby reducing healthcare disparities.
Figure 5.
Effects of Common Ingroup Identity Intervention on Patient Trust* Journal of General Internal Medicine.
Copyright © 2013 Springer. A social psychological approach to improving the outcomes of racially discordant medical interactions. Penner, L. A., et al., General Internal Medicine (e-pub ahead of print).
*Figure 5 Caption: Black Patients’ Trust of Physicians at baseline and then 4 and 16 weeks after medical interactions.
As we close this section, we might consider which of the two kinds of interventions holds the greatest promise for reducing healthcare disparities. Ultimately, of course, it is those interventions that target general negative race-related thoughts and feelings. However, for the immediate future it may well be most practical and efficacious to target specific medical interactions and focus attention on improving interactions between racial minority patients and their physicians. Thus, the most practical and realistic goal is to reduce the impact of race-related thoughts and feelings on how patients and physicians interact with one another and, thus improve the outcome of these interactions.
Summary and conclusions
Around the world, members of racial/ethnic minorities almost invariably experience poorer mental and physical health than do racial/ethnic majorities. Racial/ethnic disparities in healthcare play an important role in these disparities in the health of different racial/ethnic groups. Societal, intrapersonal, and interpersonal level processes involving race-related thoughts, feelings, and actions play important roles in healthcare disparities. We presented a social psychological analysis in the exposition of the healthcare disparities model. To do this, we focused more on processes at intrapersonal and interpersonal levels than on the societal level, and primarily considered the impact of these processes on racially discordant medical interactions. At both levels, we saw that a social psychological analysis provides considerable insight into the reasons why these interactions are typically less positive and productive than racially concordant interactions. While healthcare disparities have a long history and are pervasive throughout the world, they are not inevitable and can be reduced, if not eliminated.
Social psychological theories have much to offer in this regard. Some healthcare disparity interventions, directly derived from social psychological theories, have already been tested and seem to hold great promise of improving both communication during and the outcomes of racially discordant medical interactions. Moreover, there are other untested interventions, also derived from social psychological theory that hold promise as means to address healthcare disparities. We believe there is a special benefit to developing such theory-driven interventions. Presently, many of the interventions directed at healthcare disparities are largely atheoretical and may often simply apply an intervention that was shown to be effective in one context to another context, without much consideration of why it was successful. One important practical drawback of such approaches is that if the intervention succeeds (or fails), it is very difficult to identify the mechanisms responsible for the outcomes. Thus, the investigator has little guidance on how to improve the intervention or apply it to other settings. However, theory-driven interventions which specify and test the presumed causes of the expected outcome and the mediational processes associated with the outcomes, are likely to provide valuable heuristic and practical information for future efforts, whether or not the specific intervention is successful.
We note that there are two excellent reasons for bridging social psychological theory and racial and ethnic disparities in health and healthcare. First, this pervasive social problem provides an exciting natural laboratory in which to test theories of intergroup relations and racial bias. At the same time, psychologists have a potentially important role to play in applied, practical research intended to reduce health disparities. Thus, this article represents an argument for a melding of basic and applied research. Thus, addressing the problem of healthcare disparities may be another example of Kurt Lewin’s (1951) well-known axiom, “Nothing is as practical as a good theory.”
Acknowledgments
The authors gratefully acknowledge the following sources of support for their research reported in this article and the writing of this article. NICHD (1R21HD050445001A1) and Society for Psychological Study of Social Issues Sages awards to the first author; an NCI (R03CA130588) award to the second author and an NCI Program Award, (1U54CA153606-01), to the fifth author; an NIH RO1HL 0856331-0182 and 1R01DA029888-01 award to the last author
Footnotes
Because so much of the research to be reviewed focuses on healthcare disparities among Black patients, we will primarily use the term, racial minority, for the remainder of this paper. Racial minority, as it is used here, describes a social construction of race as a meaningful category rather than a description of a group’s genetic characteristics.
We thank the editor for suggesting the potential usefulness of the Jigsaw Technique in interventions that address healthcare disparities.
We thank an anonymous reviewer for pointing out the relevance of Philips et al. (2006) to our argument.
References
- Abrams D, Hogg MA. Social identity and self-categorization. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The Sage handbook of prejudice, stereotyping and discrimination. New York: Sage; 2010. pp. 179–193. [Google Scholar]
- Agyemang C, Seeleman C, Suurmond J, Stonks K. Racism in health and healthcare in Europe: Where does the Netherlands stand? European Journal of Public Health. 2007;17:240–241. doi: 10.1093/eurpub/ckm040. [DOI] [PubMed] [Google Scholar]
- Albrecht TL, Eggly S, Gleason M, Harper F, Foster T, Peterson A, Orom H, Penner L, Ruckdeschel JC. The influence of clinical communication on patients decision making about clinical trials. Journal of Clinical Oncology. 2008;26:2666–2273. doi: 10.1200/JCO.2007.14.8114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allport G. The nature of prejudice. Massachusetts: Addison-Wesley; 1954. [Google Scholar]
- Aronson E. The social animal. 10. New York: Worth/Freeman; 2008. [Google Scholar]
- Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O’Malley K, …Street RL., Jr Racial and ethnic disparities in the use of health services. Journal of General Internal Medicine. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avery DR, Richeson J, Hebl M, Ambady N. It doesn’t have to be uncomfortable: The role of behavioral scripts in interracial interactions. Journal of Applied Psychology. 2009;94:1382–1393. doi: 10.1037/a0016208. [DOI] [PubMed] [Google Scholar]
- Bargh JA. The cognitive monster: The case against controllability of automatic stereotype effects. In: Chaiken S, Trope Y, editors. Dual process theories in social psychology. New York: Guilford; 1999. [Google Scholar]
- Bécares L, Stafford M, Nazroo J. Fear of racism, employment and expected organizational racism: their association with health. European Journal of Public Health. 2009;19:504–510. doi: 10.1093/eurpub/ckp071. [DOI] [PubMed] [Google Scholar]
- Benkert R, Peters RM, Clark R, Keves-Foster K. Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. Journal of National Medical Association. 2006;98:1532–1540. [PMC free article] [PubMed] [Google Scholar]
- Berger M, Lund MJ, Brawley OW. Racial disparities in lung cancer. Current Problems in Cacner. 2007;31:202–210. doi: 10.1016/j.currproblcancer.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Bergsieker HB, Shelton JN, Richeson JA. To be liked versus respected: Divergent goals in interracial interactions. Journal of Personality and Social Psychology. 2010;99:248–264. doi: 10.1037/a0018474. [DOI] [PubMed] [Google Scholar]
- Bhopal RA. Racism in health and healthcare in Europe: Reality or mirage? European Journal of Public Health. 2007;17:238–241. doi: 10.1093/eurpub/ckm039. [DOI] [PubMed] [Google Scholar]
- Blair IV, Steiner JF, Havranek EP. Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Annals of Family Medicine. 2013;11:43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blascovich J, Mendes WB, Hunter SB, Lickel B, Kowai-Bell N. Perceiver threat in social interactions with stigmatized others. Journal of Personality and Social Psychology. 2001;80:253–267. doi: 10.1037/0022-3514.80.2.253. [DOI] [PubMed] [Google Scholar]
- Bodenhausen GV, Wyer RS. Effects of stereotypes on decision making and information-processing strategies. Journal of Personality and Social Psychology. 1985;48:267–282. [PubMed] [Google Scholar]
- Bogart LM, Catz SL, Kelly JA, Benotsch EG. Factors influencing physicians’ judgments of adherence and treatment decisions for patients with HIV disease. Medical Decision Making. 2001;21:28–36. doi: 10.1177/0272989X0102100104. [DOI] [PubMed] [Google Scholar]
- Bogart LM, Wagner G, Galvan FH, Banks D. Conspiracy beliefs about HIV are related to antiretroviral treatment nonadherence among African American men with HIV. Journal of Acquired Immune Deficiency Syndromes. 2010;53:648–655. doi: 10.1097/QAI.0b013e3181c57dbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldry JG, Gaertner L, Quinn J. Measuring the measures: A meta-analytic investigation of the measures of outgroup homogeneity. Group Processes and Intergroup Relations. 2007;10:147–178. [Google Scholar]
- Boulware LE, Copper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the healthcare system. Public Health Reports. 2003;118:358–365. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P. Health disparities and health equity: Concepts and measurement. Annual Review of Public Health. 2006;27:167–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- Braveman P. Health disparities and health equity: Concepts and measurement. Annual Review of Public Health. 2006;27:167–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- Brewer MB. A dual process model of impression formation. In: Srull T, Wyer R, editors. Advances in s social cognition. Vol. 1. Mahwah, NJ: Erlbaum; 1988. pp. 1–36. [Google Scholar]
- Brewer MB, Miller N. Beyond the contact hypothesis: Theoretical perspectives on desegregation. In: Miller N, Brewer MB, editors. Groups in contact: The psychology of desegregation. New York: Academic Press; 1984. pp. 281–302. [Google Scholar]
- Brondolo E, Hausmann LR, Jhalani J, Pencille M, Atencio-Bacayon J, Kumar A, Schwatz J. Dimensions of perceived racism and self-reported health: Examination of racial/ethnic differences and potential mediators. Annals of Behavioral Medicine. 2011;42:14–28. doi: 10.1007/s12160-011-9265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R, Hewstone M. An integrative theory of intergroup contact. In: Zanna M, editor. Advances in experimental social psychology. San Diego, CA: Academic Press; 2005. pp. 255–343. [Google Scholar]
- Brown TS. Measuring self-perceived racial and ethnic discrimination in social surveys. Sociological Spectrum. 2001;21:377–391. [Google Scholar]
- Burgess DJ, van Ryn M, Crowley-Matoka M, Malat J. Understanding the provider contribution to race/ethnicity disparities in pain treatment: Insights from dual process models of stereotyping. Pain Medicine. 2006;7:119–134. doi: 10.1111/j.1526-4637.2006.00105.x. [DOI] [PubMed] [Google Scholar]
- Burgess D, van Ryn M, Dovidio JF, Saha S. Reducing racial bias among healthcare providers: Lessons from social-cognitive psychology. Journal of General Internal Medicine. 2007;8:882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Warren J, Phelan S, Dovidio JF, van Ryn M. Stereotype threat and health disparities: What medical educators and future physicians need to know. Journal of General Internal Medicine. 2010;25(Suppl 2):S169–177. doi: 10.1007/s11606-009-1221-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burson A, Crocker J, Mischkowski D. Two types of value affirmation: Implications for self-control following social exclusion. Social Psychological and Personality Science. 2012;3:510–516. [Google Scholar]
- Butz DA, Plant EA. Perceiving outgroup members as unresponsive: Implications for approach-related emotions, intentions, and behavior. Journal of Personality and Social Psychology. 2006;91:1066–1079. doi: 10.1037/0022-3514.91.6.1066. [DOI] [PubMed] [Google Scholar]
- Byrd WM, Clayton LA. An American health dilemma: Race, medicine, and healthcare in the United States 1900–2000. New York: Routledge; 2000. [Google Scholar]
- Byrd WM, Clayton LA. An American health dilemma: A medical history of African Americans and the problem of race. New York: Routledge; 2002. [Google Scholar]
- Carpenter WR, Godley PA, Clark JA, Talcott JA, Finnegan T, Mishel M, Mohler JL. Racial differences in trust and regular source of patient care and the implications for prostate cancer screening use. Cancer. 2009;115:5048–5059. doi: 10.1002/cncr.24539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casas JA, Dachs JN, Bambas A. Equity and Health. Washington, DC: Pan American Health Organization; 2001. Disparities in Latin America and the Caribbean: The role of social and economic determinants; pp. 22–49. [Google Scholar]
- Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. Journal of General Internal Medicine. 2007;22 :389–395. doi: 10.1007/s11606-006-0057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Medicine. 71:1182–1188. [Google Scholar]
- Chase R. The physical basis of mental illness. New Brunswick, NJ: Transaction Publishers; 2012. [Google Scholar]
- Chen M, Bargh JA. Nonconscious behavioral confirmation processes: The self-fulfilling nature of automatically-activated stereotypes. Journal of Experimental Social Psychology. 1997;33:541–560. [Google Scholar]
- Chen FM, Fryer GE, Phillips RL, Wilson E, Pathman DE. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Annals of Family Medicine. 2005;3:139–143. doi: 10.1370/afm.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW. Social regulation of human gene expression. Current Directions in Psychological Science. 2009;18:132–137. doi: 10.1111/j.1467-8721.2009.01623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. Journal of General Internal Medicine. 2002;17:477–486. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Crandall CS, Eshleman A. A justification-suppression model of the expression and experience of prejudice. Psychological Bulletin. 2003;129:414–446. doi: 10.1037/0033-2909.129.3.414. [DOI] [PubMed] [Google Scholar]
- Daponte-Codina A, Bolívar-Muñoz J, Toro-Cárdenas S, Ocaña-Riola R, Benach-Rovira J, Navarro-López V. Area deprivation and trends in inequalities in self-rated health in Spain, 1987–2001. Scandinavian Journal of Public Health. 2008;36:504–515. doi: 10.1177/1403494807088454. [DOI] [PubMed] [Google Scholar]
- De Lew N, Weinick RM. An overview: Eliminating racial, ethnic, and SES disparities in health care. Health Care Financing Review. 2000;21:1–7. [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services. Mental Health: Culture Race and Ethnicity a Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Government Printing office; 2001. [PubMed] [Google Scholar]
- Dilley JA, Simmons KW, Boysun MJ, Pizacari BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: Health disparities in the Pacific NW. American Journal of Public Health. 2010;100:460–467. doi: 10.2105/AJPH.2007.130336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: A pilot study. International Journal of Quality in Healthcare. 2007;19:60–67. doi: 10.1093/intqhc/mzl069. [DOI] [PubMed] [Google Scholar]
- Dorling D, Mitchell R, Pearce J. The global impact of income inequality on health by age: An observational study. British Medical Journal. 2007;335:833–834. doi: 10.1136/bmj.39349.507315.DE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF. On the nature of contemporary prejudice: The third wave. Journal of Social Issues. 2001;57:829–849. [Google Scholar]
- Dovidio JF, Brown CE, Keating CF, Heltman K, Ellyson SL. Power displays between women and men in discussions of gender-linked tasks: A multichannel study. Journal of Personality and Social Psychology. 1988;55:580–587. doi: 10.1037//0022-3514.54.2.233. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Fazio RH. New technologies for the direct and indirect assessment of attitudes. In: Tanur J, editor. Questions about questions: Inquiries into the cognitive bases of surveys. New York: Russell Sage Foundation; 1992. pp. 204–237. [Google Scholar]
- Dovidio JF, Gaertner SL. Aversive racism. In: Zanna MP, editor. Advances in experimental social psychology. San Diego, CA: Academic Press; 2004. pp. 1–52. [Google Scholar]
- Dovidio JF, Gaertner SL. Intergroup bias. In: Fiske ST, Gilbert D, Lindzey G, editors. Handbook of social psychology. New York: Wiley; 2010. pp. 1084–1121. [Google Scholar]
- Dovidio JF, Kawakami K, Gaertner SL. Implicit and explicit prejudice and interracial interaction. Journal of Personality and Social Psychology. 2002;82:62–68. doi: 10.1037//0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and healthcare. Social Science & Medicine. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Services Research. 2005;5:64. doi: 10.1186/1472-6963-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan SL. Differential social perception and attribution of intergroup violence: Testing the lower limits of stereotyping of blacks. Journal of Personality and Social Psychology. 1976;56:5–18. doi: 10.1037//0022-3514.34.4.590. [DOI] [PubMed] [Google Scholar]
- Dunham Y. An angry = outgroup effect. Journal of Experimental Social Psychology. 2011;47:668–671. [Google Scholar]
- Earnshaw V, Bogart L, Dovidio JF, Williams D. Stigma and racial/ethnic HIV disparities. American Psychologist. 2013;68:225–236. doi: 10.1037/a0032705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggly S, Barton E, Winckles A, Penner L, Albrecht T. A disparity of words: A comparison of offers to participate in cancer clinical trials by patient race. Health Expectations in press. [Google Scholar]
- Eggly S, Harper FWK, Penner LA, Gleason MJ, Foster T, Albrecht TL. Variation in question asking during cancer clinical interactions: A potential source in access to information. Patient Education and Counseling. 2011;82:63–68. doi: 10.1016/j.pec.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggly S, Tkatch R, Penner LA, Mabunda L, Hudson J, Chapman R, Albrecht TL. Development of a question prompt list as a communication intervention to reduce racial disparities in cancer treatment. Journal of Cancer Education. 2013 doi: 10.1007/s13187-013-0456-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfenbein HA, Ambady N. On the universality and cultural specificity of emotion recognition: A meta-analysis. Psychological Bulletin. 2002;128:203–235. doi: 10.1037/0033-2909.128.2.203. [DOI] [PubMed] [Google Scholar]
- Elster A, Jarosik J, VanGeest J, Fleming M. Racial and ethnic disparities in health care for adolescents. Archives of Pediatrics & Adolescent Medicine. 2003;157:867–874. doi: 10.1001/archpedi.157.9.867. [DOI] [PubMed] [Google Scholar]
- Engle RW, Conway ARA, Tuholski SW, Shisler RJ. A resource account of inhibition. Psychological Science. 1995;6:122–125. [Google Scholar]
- Epstein RM, Street RL. Patient-centered communication in cancer care: Promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute; 2007. [Google Scholar]
- Fazio RH. Multiple processes by which attitudes guide behavior: The MODE model as an integrative framework. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 23. New York: Academic Press; 1990. pp. 75–109. [Google Scholar]
- Fernandez A, Schillinger D, Warton EM, Adler N, Moffet HH, Schenker Y, Karter AJ. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: The diabetes study of northern California (DISTANCE) Journal of General Internal Medicine. 2010;26:170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske ST, Lin MH, Neuberg SL. The continuum model: Ten years later. In: Chaiken S, Trope Y, editors. Dual process theories in social psychology. New York: Guilford; 1999. pp. 231–254. [Google Scholar]
- Foddy M, Platow MJ, Yamagishi H. Group-based trust in strangers: The role of stereotypes and expectations. Psychological Science. 2009;20:419–422. doi: 10.1111/j.1467-9280.2009.02312.x. [DOI] [PubMed] [Google Scholar]
- Franks P, Muennig P, Lubetkin E, Jia H. The burden of disease associated with being African-American in the United States and the contribution of socioeconomic status. Social Science and Medicine. 2006;62:2469–2478. doi: 10.1016/j.socscimed.2005.10.035. [DOI] [PubMed] [Google Scholar]
- Frohlich KL, Ross N, Richmond C. Health disparities in Canada today: Some evidence and a theoretical framework. Health Policy. 2006;79:132–143. doi: 10.1016/j.healthpol.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Evans GW, Ong AD. Poverty and health: The mediating role of perceived discrimination. Psychological Science. 2012;23:734–739. doi: 10.1177/0956797612439720. [DOI] [PubMed] [Google Scholar]
- Gaertner SL, Dovidio JF. The aversive form of racism. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination and racism: Theory and research. Orlando, FL: Academic Press; 1986. pp. 61–89. [Google Scholar]
- Gaertner SL, Dovidio JF. A Common Ingroup Identity: A categorization-based approach for reducing intergroup bias. In: Nelson T, editor. Handbook of prejudice. Philadelphia, PA: Taylor & Francis; 2009. pp. 489–506. [Google Scholar]
- Gaertner SL, Dovidio JF, Houlette MA. Social categorization. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The Sage handbook of prejudice, stereotyping and discrimination. New York: Sage; 2010. pp. 526–543. [Google Scholar]
- Garcia JA, Paterniti DA, Romano PS, Kravitz RL. Patient preferences for physician characteristics in university-based primary care clinics. Ethnicity and Disease. 2003;13:259–267. [PubMed] [Google Scholar]
- Gerber JS, Prasad PA, Localio R, Fiks AG, Grundmeier RW, Bell LM, Zaoutis TE. Racial differences in antibiotic prescribing by primary care pediatricians. Pediatrics. 2013;131:677–684. doi: 10.1542/peds.2012-2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon HS, Street RL, Sharf BF, Kelly PA, Souchek J. Racial differences in trust and lung cancer patients’ perceptions of physician communication. Journal of Clinical Oncology. 2006;24:904–909. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, Vallerand AH. The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Medicine. 2003;4:277–294. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. The presence of implicit bias in physicians and its predictions of thrombolysis decisions for Black and White patients. Journal of General Internal Medicine. 2007;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, Banaji MR. Implicit social cognition: Attitudes, self-esteem, and stereotypes. Psychological Review. 1995;102:4–27. doi: 10.1037/0033-295x.102.1.4. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Greer TM. Perceived racial discrimination in clinical encounters among African American hypertension patients. Journal of Healthcare for the Poor and Underserved. 2010;21:251–263. doi: 10.1353/hpu.0.0265. [DOI] [PubMed] [Google Scholar]
- Griggs JJ, Sorbero ME, Stark AT, Heininger SE, Dick AW. Racial disparity in the dose and dose intensity of breast cancer adjuvant chemotherapy. Breast Cancer Research and Treatment. 2003;81:21–31. doi: 10.1023/A:1025481505537. [DOI] [PubMed] [Google Scholar]
- Hagiwara N, Kashy DA, Penner LA. A new analytical strategy for patient-physician communication researcher: The one-with-many design. Annals of Family Medicine. doi: 10.1016/j.pec.2014.03.017. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara N, Penner LA, Gonzalez R, Albrecht TL. Within-group health disparities among Blacks: The effects of Afrocentric features and unfair treatment. Cultural Diversity and Ethnic Minority Psychology. doi: 10.1037/a0032566. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara N, Penner LA, Gonzalez R, Eggly S, Dovidio JF, Gaertner SL, West T, Albrecht TL. Racial attitudes, social control, and adherence in racially discordant medical interactions. Social Science and Medicine. 2013;87:123–131. doi: 10.1016/j.socscimed.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn SR. Patient-centered communication to assess and enhance patient adherence to glaucoma medication. Ophthalmology. 2009;116:S37–42. doi: 10.1016/j.ophtha.2009.06.023. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Armstrong K, Gandy OH, Shaker L. Racial differences in trust in healthcare providers. Archives of Internal Medicine. 2006;166:896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- Hall JA, Roter DL, Katz NR. Meta-analysis of correlates of provider behavior in medical encounters. Medical Care. 1988;26:657–675. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- Harris DE, Andrews R, Elixhauser A. Racial and gender differences in the use of procedures for black and white hospitalized adults. Ethnicity and Disease. 1997;7:91–102. [PubMed] [Google Scholar]
- Harris R, Tobias M, Jeffreys M, Waldegrave K, Karlsen S, Nazroo J. Racism and health: The relationship between experience of racial discrimination and health in New Zealand. Social Science & Medicine. 2006;63:1428–1441. doi: 10.1016/j.socscimed.2006.04.009. [DOI] [PubMed] [Google Scholar]
- Hartley LR, Adams RG. Effect of noise on the Stroop test. Journal of Experimental Psychology. 1974;102:62–66. doi: 10.1037/h0035695. [DOI] [PubMed] [Google Scholar]
- Havranek EP, Hanratty R, Tate C, Dickinson M, Steiner J, Cohen G, Blair I. The effects of values affirmation on race-discordant patient provider communication. Archives of Internal Medicine. 2012;17:1662–1667. doi: 10.1001/2013.jamainternmed.258. [DOI] [PubMed] [Google Scholar]
- Hays RD, Kravitz RL, Mazel RM, Sherbourne CD, DiMatteo MR, Rogers WH, Greenfield S. The impact of patient adherence on health outcomes for patients with chronic disease in the Medical Outcomes Study. Journal of Behavioral Medicine. 1994;17:347–360. doi: 10.1007/BF01858007. [DOI] [PubMed] [Google Scholar]
- Hebl MR, Dovidio JF. Promoting the “social” in the examination of social stigma. Personality and Social Psychology Review. 2005;9:156–182. doi: 10.1207/s15327957pspr0902_4. [DOI] [PubMed] [Google Scholar]
- Hirsh AT, Jensen MP, Robinson ME. Evaluation of nurses’ self-insight into their pain assessment and treatment decisions. Journal of Pain. 2010;11:454–461. doi: 10.1016/j.jpain.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodson G, Hooper H, Dovidio JF, Gaertner SL. Aversive racism in Britain: Legal decisions and the use of inadmissible evidence. European Journal of Social Psychology. 2005;35:437–448. [Google Scholar]
- Hugenberg K, Bodenhausen GV. Ambiguity in social categorization: The role of prejudice and facial affect in racial categorization. Psychological Science. 2004;15:342–345. doi: 10.1111/j.0956-7976.2004.00680.x. [DOI] [PubMed] [Google Scholar]
- Smedley BE, Stith AY, Nelson AR, editors. Institute of Medicine. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Islam MR, Hewstone M. Dimensions of contact as predictors of intergroup anxiety, perceived outgroup variability, and outrgroup attitudes: An integrative model. Personality and Social Psychology Bulletin. 1993;19:700–710. [Google Scholar]
- John-Baptiste A, Naglie G, Tomlinson G, Alibhai SMH, Etchells E, Cheung A, Krahn M. The effect of English language proficiency on length of stay and in-hospital mortality. Journal of General Internal Medicine. 2004;19:221–228. doi: 10.1111/j.1525-1497.2004.21205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in healthcare. Journal of General Internal Medicine. 2004;19:101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd CM, Park B, Yzerbyt V, Gordijn EH, Muller D. Attributions of intergroup bias and outgroup homogeneity to ingroup and outgroup others. European Journal of Social Psychology. 2005;35:677–704. [Google Scholar]
- Kelly PA, Haidet P. Physician overestimation of patient literacy: A potential source of healthcare disparities. Patient Education and Counseling. 2007;66:119–122. doi: 10.1016/j.pec.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Schneier M. The 12-month prevalence and correlates of serious mental illness (SMI) Rockville, MD: Center for Mental Health Services; 1996. [Google Scholar]
- Kinder DR, Sears DO. Prejudice and politics: Symbolic racism versus racial threats to the good life. Journal of Personality and Social Psychology. 1981;40:414–431. [Google Scholar]
- Kirby JB, Taliaferro G, Zuvekas SH. Explaining racial and ethnic disparities in healthcare. Medical Care. 2006;44:164–712. doi: 10.1097/01.mlr.0000208195.83749.c3. [DOI] [PubMed] [Google Scholar]
- Kleinpenning G, Hagendoorn L. Forms of racism and the cumulative dimension. Social Psychology Quarterly. 1993;56:21–36. [Google Scholar]
- Lahelma E, Lunberg O. Health inequalities in European welfare states. European Journal of Public Health. 2009;19:445–446. doi: 10.1093/eurpub/ckp120. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Nuru-Jeter A, Jones KE. The association of doctor-patient race concordance with health services utilization. Journal of Public Health Policy. 2003;24:312–323. [PubMed] [Google Scholar]
- Lee AJ, Gehlbach S, Hosmer RM, Baker CS. Medicare treatment differences for blacks and whites. Medical Care. 1997;35:1173–1189. doi: 10.1097/00005650-199712000-00002. [DOI] [PubMed] [Google Scholar]
- Lewin K. In: Field theory in social science: Selected theoretical papers. Cartwright D, editor. New York: Harper & Row; 1951. [Google Scholar]
- Lie DA, Lee-Rey E, Gomez A, Bereknyei S, Braddock CH., III Does cultural competency training of health professionals improve patient outcomes? A systematic review and proposed algorithm for future research. Journal of General Internal Medicine. 2010;26:317–325. doi: 10.1007/s11606-010-1529-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CC, Virgo KS. Association between the availability of medical oncologists and initiation of chemotherapy for patients with stage III colon cancer. Journal of Oncological Practice. 2013;9:27–33. doi: 10.1200/JOP.2012.000627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan C, Walsh PN, van Schrojenstein Lantman-de Valk HMJ, Kerr MP, Dawson F. Are people with intellectual disabilities represented in European public health surveys? Journal of Applied Research in Intellectual Disabilities. 2009;22:409–420. [Google Scholar]
- Linsky A, McIntosh N, Cabral H, Kazis LE. Patient-provider language concordance and colorectal cancer screening. Journal of General Internal Medicine. 2010 doi: 10.1007/s11606-010-1512-9. Retrieved from http://www.springerlink.com/content/f283462461lk5608/fulltext.pdf. [DOI] [PMC free article] [PubMed]
- Macrae CN, Milne AB, Bodenhausen GV. Stereotypes as energy-saving devices: A peek inside the cognitive toolbox. Journal of Personality and Social Psychology. 1994;66:33–47. [Google Scholar]
- Major B, Mendes WB, Dovidio JF. Intergroup relations and health disparities: A social psychological perspective. Health Psychology. 2013 doi: 10.1037/a0030358. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major B, Townsend SSM. Coping with bias. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The Sage handbook of prejudice, stereotyping and discrimination. New York: Sage; 2010. pp. 410–425. [Google Scholar]
- Mallett RK, Wilson TD, Gilbert DT. Expect the unexpected: Failure to anticipate similarities when predicting the quality of an intergroup interaction. Journal of Personality and Social Psychology. 2008;94:265–277. doi: 10.1037/0022-3514.94.2.94.2.265. [DOI] [PubMed] [Google Scholar]
- Mallinger JB, Lamberti SJ. Racial differences in the use of adjunctive psychotropic medications for patients with schizophrenia. Journal of Mental Health Policy and Economics. 2007;10:15–22. [PubMed] [Google Scholar]
- Mast MS. Dominance as expressed and inferred through speaking time. Human Communication Research. 2002;28:420–450. [Google Scholar]
- McConahay JB. Modern racism, ambivalence, and the modern racism scale. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination, and racism. Orlando, FL: Academic Press; 1986. pp. 99–125. [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: An application to mental health care. Health Service Research. 2006;41:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQueen A, Krueter MW. Women’s cognitive and affective reactions to breast cancer survivor stories: A structural equation analysis. Patient Education and Counseling. 2010;81:S15–S21. doi: 10.1016/j.pec.2010.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead N, Bower P. Patient-centredness: A conceptual framework and review of the empirical literature. Social Science and Medicine. 2000;51:1087–1100. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- Mendoza-Denton R, Downey G, Purdie VJ, Davis A, Pietrzak J. Sensitivity to status-based rejection: Implications for African American students’ college experience. Journal of Personality and Social Psychology. 2002;83:896–918. doi: 10.1037//0022-3514.83.4.896. [DOI] [PubMed] [Google Scholar]
- Merton RK. The self-fulfilling prophecy. Antioch Review. 1948;8:193–210. [Google Scholar]
- Mobaraki AE, Söderfeldt B. Gender inequality in Saudi Arabia and its role in public health. Eastern Mediterranean Health Journal. 2010;16:113–118. [PubMed] [Google Scholar]
- Monteith MJ, Arthur SA, Flynn SM. Self-regulation and bias. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. Handbook of prejudice, stereotyping, and discrimination. Thousand Oaks, CA: Sage; 2010. pp. 493–507. [Google Scholar]
- Morris AM, Billingsley KG, Hayanga AJ, Matthews B, Baldwin LM, Birkmeyer JD. Residual treatment disparities after oncology referral for rectal cancer. Journal of the National Cancer Institute. 2008;100:738–744. doi: 10.1093/jnci/djn396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz D, Thom DH, Guzman D, Penko J, Miaskowski C, Kushel M. Is primary care providers’ trust in socially marginalized patients affected by race? Journal of General Internal Medicine. 2011;26:846–851. doi: 10.1007/s11606-011-1672-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz GB, Stone J, Childs A. Implicit stereotyping and medical decisions: Unconscious stereotype activation in practitioners’ thoughts about African Americans. American Journal of Public Health. 2012;102:996–1001. doi: 10.2105/AJPH.2011.300591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullen B, Dovidio JF, Johnson C, Copper C. In-group-out-group differences in social projection. Journal of Experimental Social Psychology. 1992;28:422–440. [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychological Bulletin. 2000;126:247–259. doi: 10.1037/0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- Nakash O, Saguy T, Levav I. The effects of social identities of service-users and clinicians on mental health disparities: A review of theory and facts. The Israel Journal of Psychiatry and Related Sciences. 2012;49:202–210. [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 201: With special feature on socioeconomic status and health. Hyattsville, MD: U.S. Government Printing Office; 2011. [PubMed] [Google Scholar]
- Nazroo JY, Karlsen S. Ethnic inequalities in health: Social class, racism, and identity: ESRC research findings 10 from the health variation programme. Lancaster: Lancaster University; 2001. [Google Scholar]
- New Zealand Ministry of Health. Reducing inequalities in health. 2002 Sep; Retrieved from http://owl.english.purdue.edu/owl/resource/560/10/
- Nielsen-Bohlman L, Panzer AM. Health literacy: A prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Norredam M, Krasnik A, Sorensen TM, Keiding N, Michaelsen JJ, Nielsen AS. Emergency room utilization in Copenhagen: A comparison of immigrant groups and Danish-born residents. Scandinavian Journal of Public Health. 2004;32:53–59. doi: 10.1080/14034940310001659. [DOI] [PubMed] [Google Scholar]
- Nunez-Smith M, Ciarleglio M, Sandoval-Minero T, Elumn J, Castillo-Page L, Peduzzi P, Bradley E. Medical school faculty promotion in the United States: Is there institutional variation by race/ethnicity? American Journal of Public Health. 2012;102:852–858. doi: 10.2105/AJPH.2011.300552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obeidat NA, Pradel FG, Zuckerman IH, Trovato JA, Palumbo FB, DeLisle S, Mullins CD. Racial/ethnic and age disparities in chemotherapy selection for colorectal cancer. American Journal of Managed Care. 2010;16:515–522. [PubMed] [Google Scholar]
- Oliver MN, Goodwin MA, Gotler RS, Gregory PM, Stange KC. Time use in clinical encounters: are African-American patients treated differently? Journal of the National Medicical Association. 2001;93:380–385. [PMC free article] [PubMed] [Google Scholar]
- O’Reilly KB. Black men increasingly hard to find in medical schools. American Medical News. 2013 Feb 25; (url: http://amednews.com/article/20130225/profession/130229975/2/ Retrieved April 14, 2013)
- Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS. Health literacy: An overlooked factor in understanding HIV health disparities. American Journal of Preventive Medicine. 2007;33:374–378. doi: 10.1016/j.amepre.2007.07.022. [DOI] [PubMed] [Google Scholar]
- Otten S, Moskowitz GB. Evidence for implicit evaluative ingroup bias: Affect-biased spontaneous trait inference in a minimal group paradigm. Journal of Experimental Social Psychology. 2000;36:77–89. [Google Scholar]
- Oyserman D, Bybee D, Terry K. Possible selves and academic outcomes: How and when possible selves impel action. Journal of Personality and Social Psychology. 2006;91:188–204. doi: 10.1037/0022-3514.91.1.188. [DOI] [PubMed] [Google Scholar]
- Oyserman D, Fryberg SA, Yoder N. Identity-based motivation and health. Journal of Personality and Social Psychology. 2007;93:1011–1027. doi: 10.1037/0022-3514.93.6.1011. [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. Journal of General Internal Medicine. 2005;20:175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Albrecht TL, Orom H, Coleman DK, Underwood W., III . Health and healthcare disparities. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The Sage handbook of prejudice, stereotyping and discrimination. New York: Sage; 2010. pp. 472–490. [Google Scholar]
- Penner LA, Dovidio JF, Edmondson D, Dailey RK, Markova T, Albrecht TL, Gaertner SL. The experience of discrimination and Black-White health disparities in medical care. Journal of Black Psychology. 2009;35:180–203. doi: 10.1177/0095798409333585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, West TW, Gaertner SL, Albrecht TL, Dailey RK, Markova T. Aversive racism and medical interactions with Black patients: A field study. Journal of Experimental Social Psychology. 2010b;46:436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Eggly S, Harper FWK, Albrecht TL, Ruckdeschel JC. Patient attributes and information provided about clinical trials. Proceedings of the American Association for Cancer Research Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved. 2007 Nov;95 [Google Scholar]
- Penner LA, Eggly S, Griggs J, Orom H, Underwood W., III Life-threatening disparities: The roles of ethnicity and social class in the treatment of cancer. Journal of Social Issues. 2012;68:328–357. doi: 10.1111/j.1540-4560.2012.01751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Gaertner S, Dovidio JF, Hagiwara N, Petrocelli J, Markova T, Albrecht TL. A social psychological approach to improving the outcomes of racially discordant medical interactions. Journal of General Internal Medicine. 2013 doi: 10.1007/s11606-013-2339-y. e-pub ahead of publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Hagiwara N. Racism and health. In: Ryan JM, editor. The Wiley-Blackwell encyclopedia of health, illness, behavior, and society. Hoboken, NJ: Wiley-Blackwell; in press. [Google Scholar]
- Penner LA, Orom, Albrecht T, Franks M, Foster T, Ruckdeschel JC. Camera-related behaviors during video recorded medical interactions. Journal of Nonverbal Behavior. 2007;31:99–117. [Google Scholar]
- Perloff RM, Bonder B, Ray GB, Ray EB, Siminoff LA. Doctor-patient communication, cultural competence, and minority health. American Behavioral Scientist. 2005;49:835–852. [Google Scholar]
- Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology. 2006;90:751–783. doi: 10.1037/0022-3514.90.5.751. [DOI] [PubMed] [Google Scholar]
- Pettigrew TF, Tropp LR. When groups meet: The dynamics of intergroup contact. Philadelphia, PA: Psychology Press; 2011. [Google Scholar]
- Phillips KW, Northcraft GB, Neale MA. Surface-level diversity and decision-making in groups: When does deep-level similarity help? Group Processes and Intergroup Relations. 2006;9:467–482. [Google Scholar]
- Pinel EC. Stigma Consciousness: The Psychological Legacy of Social Stereotypes. Journal of Experimental Social Psychology. 1999;76:114–128. doi: 10.1037//0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- Pope JH, Aufderheide TP, Selker HP. Missed diagnoses of acute cardiac ischemia in the emergency department. The New England Journal of Medicine. 2000;342:1163–1170. doi: 10.1056/NEJM200004203421603. [DOI] [PubMed] [Google Scholar]
- Price EG, Beach MC, Cooper LA. A systematic review of the methodological rigor of studies evaluating cultural competence training of health professionals. Academic Medicine. 2005;80:578–586. doi: 10.1097/00001888-200506000-00013. [DOI] [PubMed] [Google Scholar]
- Reid A, Dovidio JF, Ballester E, Johnson B. HIV prevention interventions to reduce 3exual risk for African Americans: The influence of community-level stigma and psychological processes. Invited revision, Social Science and Medicine. 2013 doi: 10.1016/j.socscimed.2013.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richeson JA, Shelton JN. Negotiating interracial interactions: Costs, consequences, and possibilities. Current Directions in Psychological Science. 2007;16:316–320. [Google Scholar]
- Richeson JA, Trawalter S. Why do interracial interactions impair executive function? A resource depletion account. Journal of Personality and Social Psychology. 2005;88:934–947. doi: 10.1037/0022-3514.88.6.934. [DOI] [PubMed] [Google Scholar]
- Richeson JA, Trawalter S, Shelton JN. African Americans’ racial attitudes and the depletion of executive function after interracial interactions. Social Cognition. 2005;23:336–352. [Google Scholar]
- Robbins JM, Krueger JI. Social projection to ingroups and outgroups: A review and meta-analysis. Personality and Social Psychology Review. 2005;9:32–47. doi: 10.1207/s15327957pspr0901_3. [DOI] [PubMed] [Google Scholar]
- Rostila M. Birds of a feather flock together – and fall ill? Migrant homophily and health in Sweden. Sociology of Health & Illness. 2010;32:382–399. doi: 10.1111/j.1467-9566.2009.01196.x. [DOI] [PubMed] [Google Scholar]
- Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. American Journal of Public Health. 2012;102:988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Nosek BA, Greenwald AG, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. Journal of Healthcare for the Poor and Underserved. 2009;20:896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Medical Care. 2008;46:678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. American Journal of Public Health. 2003;93:1713–1719. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Jacobs EA, Moore RD, Beach MC. Trust in physicians and racial disparities in HIV care. AIDS Patient Care and STDs. 2010;24:415–420. doi: 10.1089/apc.2009.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saldana-Ruiz N, Clouston SA, Rubin MS, Colen CG, Link BG. Fundamental causes of colorectal cancer mortality in the United States: Understanding the importance of socioeconomic status in creating inequality in mortality. American Journal of Public Health. 2013;103:99–104. doi: 10.2105/AJPH.2012.300743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers VL, Brown M, Klabunde CN, Potosky AL, Davis W, Moul JW, Fahey A. Race/Ethnicity and the intensity of medical monitoring under ‘watchful waiting’ for prostate cancer. Medical Care. 2004;42:239–250. doi: 10.1097/01.mlr.0000117361.61444.71. [DOI] [PubMed] [Google Scholar]
- Shavers VL, Fagan P, Jones D, Klein WM, Boyington J, Moten C, Rorie E. The state of research on racial/ethnic discrimination in the receipt of health care. American Journal of Public health. 2012;102:953–966. doi: 10.2105/AJPH.2012.300773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton JN, Richeson JA. racially discordant interactions: A relational approach. Advances in Experimental Social Psychology. 2006;38:121–181. [Google Scholar]
- Shelton JN, Richeson JA, Salvatore J, Trawalter S. Ironic effects of racial bias during racially discordant interactions. Psychological Science. 2005;16:397–402. doi: 10.1111/j.0956-7976.2005.01547.x. [DOI] [PubMed] [Google Scholar]
- Shelton JN, West TV, Trail TE. Concerns about apeparing prejudiced: Implications for anxiety during daily interracial interactions. Group Processes and Intergroup Relations. 2010;13:329–344. [Google Scholar]
- Shirom A, Nirel N, Viuokar A. Overload, autonomy, and burnout as predictors of physicians’ quality of care. Journal of Occupational Health psychology. 2006;11:328–342. doi: 10.1037/1076-8998.11.4.328. [DOI] [PubMed] [Google Scholar]
- Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors. Patient Education and Counseling. 2006;62:355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Sims M, Diez-Roux AV, Taylor HA. Perceived discrimination and hypertension among African Americans in the Jackson Heart Study. American Journal of Public Health. 2012;102:S258–265. doi: 10.2105/AJPH.2011.300523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden LR. Bias in mental health assessment and intervention: Theory and evidence. American Journal of Public health. 2003;93:239–243. doi: 10.2105/ajph.93.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son Hing LS, Chung-Yan GA, Hamilton LK, Zanna MP. A two-dimensional model that employs explicit and implicit attitudes to characterize prejudice. Journal of Personality and Social Psychology. 2008;94:771–987. doi: 10.1037/0022-3514.94.6.971. [DOI] [PubMed] [Google Scholar]
- Stephan WG, Stephan CW. Intergroup anxiety. Journal of Social Issues. 1985;41:157–175. [Google Scholar]
- Stewart MA, Brown JB, Donner A, McWhinney I, Oates J, Weston W, Jordan J. The impact of patient-centered care on outcomes. Journal of Family Practice. 2000;49:796–804. [PubMed] [Google Scholar]
- Street RL, Gordon HS, Haidet P. Physicians’ communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Social Science & Medicine. 2007;65:586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street RL, Jr, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: Personal and ethnic dimensions of shared identity. Annals of Family Medicine. 2008;6:198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sue S, Zane N, Young K. Research on Psychotherapy on Culturally Diverse Populations. In: Bergin A, Garfield S, editors. Handbook of psychotherapy and behavior change. New York, NY: Wiley; pp. 783–817. [Google Scholar]
- Sujoldžić A, Peternel L, Kulenvoić T, Terzić R. Social determinants of health – A comparative study of Bosnian adolescents in different cultural contexts. Collegium Antropologicum. 2006;30:703–711. [PubMed] [Google Scholar]
- Sussman LK, Robins LN, Earls F. Treatment-seeking for depression by black and white Americans. Social Science & Medicine. 1987;24:187–196. doi: 10.1016/0277-9536(87)90046-3. [DOI] [PubMed] [Google Scholar]
- Swedish National Institute of Public Health. Frykman J, editor. Discrimination: A threat to public health. 2006 Retrieved from http://www.fhi.se/PageFiles/4465/r200622_diskrimination_eng.pdf.
- Swim JK, Hyers LL. Excuse me-What did you just say?!: Women’s public and private responses to sexist remarks. Journal of Experimental Social Psychology. 1999;35:68–88. [Google Scholar]
- Tajfel H, Turner J. An integrative theory of intergroup conflict. In: Austin WG, Worchel S, editors. The social psychology of intergroup relations. Monterey, CA: Brooks/Cole; 1979. pp. 33–48. [Google Scholar]
- Tausch N, Hewstone M. Intergroup contact. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The Sage handbook of prejudice, stereotyping and discrimination. New York: Sage; 2010. pp. 544–560. [Google Scholar]
- Thompson TL, Dorsey A, Miller K, Parrott R. Handbook of Health Communication. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The group-based Medical Mistrust Scale: Psychometric properties and association with breast cancer screening. Preventive Medicine. 2004;38:209–218. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- Thorburn S, Bogart LM. African American women and family planning services: Perception of discrimination. Women & Health. 2005;42:23–39. doi: 10.1300/J013v42n01_02. [DOI] [PubMed] [Google Scholar]
- Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Annals of Emerging Medicine. 2000;35:11–16. doi: 10.1016/s0196-0644(00)70099-0. [DOI] [PubMed] [Google Scholar]
- Todd KH, Lee T, Hoffman JR. The effect of ethnicity on physician estimates of pain severity in patients with isolated extremity trauma. Journal of the American Medical Association. 1994;271:925–928. [PubMed] [Google Scholar]
- Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. Journal of the American Medical Association. 1993;269:1537–1539. [PubMed] [Google Scholar]
- Trawalter S, Hoffman KM, Waytz A. Racial bias in perceptions of pthers’ pain. PLoS One. 2012;7:e48546. doi: 10.1371/journal.pone.0048546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trawalter S, Richeson JA, Shelton JN. Predicting behavior during interracial interactions: A stress and coping approach. Personality and Social Psychology Review. 2009;13:243–268. doi: 10.1177/1088868309345850. [DOI] [PubMed] [Google Scholar]
- Turner RN, Hewstone M, Voci A. Reducing explicit and implicit outgroup prejudice via direct and extended contact: The mediating role of self-disclosure and intergroup anxiety. Journal of Personality and Social Psychology. 2007;93:369–388. doi: 10.1037/0022-3514.93.3.369. [DOI] [PubMed] [Google Scholar]
- Underwood W, De Monner S, Ubel P, Fagerlin A, Sanda MG, Wei JT. Racial/ethnic disparities in the treatment of localized/regional prostate cancer. Journal of Urology. 2004;171:1504–1507. doi: 10.1097/01.ju.0000118907.64125.e0. [DOI] [PubMed] [Google Scholar]
- van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Medical Care. 2002;40:140–151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- van Ryn M, Burgess D, Malat J, Griffin J. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. American Journal of Public Health. 2006;96:351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science & Medicine. 2000;50:813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- Voci A, Hewstone M. Intergroup contact and prejudice towards immigrants in Italy: The mediational role of anxiety and the moderational role of group salience. Group Processes and Intergroup Relations. 2003;6:37–54. [Google Scholar]
- Vogelstein B, Kinzler KW. The genetic basic of human cancer. 2. McGraw-Hill; 2002. [Google Scholar]
- Vorauer JD. An information search model of evaluative concerns in intergroup interaction. Psychological Review. 2006;113:862–886. doi: 10.1037/0033-295X.113.4.862. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund PA, Kessler RC. Recent Care of Common Mental Disorders in the United States. Journal of General Internal Medicine. 2000;15:284–292. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD, Davies AR. Developing and testing the MOS 20-item short-form health survey: A general population application. In: Stewart AL, Ware JE, editors. Measuring functioning and well-being: The Medical Outcomes Study approach. Durham, NC: Duke University Press; 1992. pp. 277–290. [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Sciences. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson TD, Lindsey S, Schooler TY. A model of dual attitudes. Psychological Review. 2000;107:101–126. doi: 10.1037/0033-295x.107.1.101. [DOI] [PubMed] [Google Scholar]
- Young SG, Hugenberg K. Mere social categorization modulates identification of facial expressions of emotion. Journal of Personality and Social Psychology. 2010;99:964–977. doi: 10.1037/a0020400. [DOI] [PubMed] [Google Scholar]
- Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry. 2001;58:55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- Zhang AY, Snowden LR, Sue S. Differences between Asian- and White-Americans’ help-seeking and utilization patterns in the Los Angeles area. Journal of Community Psychology. 1998;26:317–326. [Google Scholar]