Abstract
Objective
To evaluate the participants in the Mayo Clinic Biobank for their representativeness to the entire Employee and Community Health (ECH) primary care population with regards to hospital utilization.
Patient and Methods
Participants enrolled in the Mayo Clinic Biobank from April 1, 2009, to December 31, 2010, were linked to ECH panels. Subjects were categorized into risk tiers (0–4) based on the number of health conditions as of December 31, 2010. Outcomes were ascertained through December 31, 2011. Hazard ratios (HR) and 95% confidence intervals (CI) for risk of hospitalization, ER visits, and 30-day re-hospitalization were estimated using Cox regression, accounting for age and sex.
Results
The 8,927 Biobank participants were part of an ECH panel (N=84,872). Compared to all of ECH, the Biobank-ECH participants were more likely to be female (64% vs 55%), older (median age of 58 years vs 47 years), and have a lower percentage in tier 0 (6% vs 24%). There were strong positive associations of tier (4 vs 0/1) with risk of hospitalization (HR=5.8; 95% CI, 4.6–7.5) and ER visits (HR=5.4; 95% CI, 4.2–6.8), among Biobank-ECH participants. Similar associations for risk of hospitalization (HR=8.5; 95% CI, 7.8–9.3) and ER visits (HR=6.9; 95%CI, 6.4–7.5) were observed for all of ECH.
Conclusion
Biobank-ECH participants were older and had more chronic conditions compared to the ECH panel. Nevertheless, the associations of risk tier with utilization outcomes were similar, supporting the use of the Biobank-ECH participants for assessing biomarkers for health care outcomes in the primary care setting.
INTRODUCTION
Clinicians, hospitals, and researchers are actively evaluating methods of reducing hospitalization and re-hospitalization within managed populations, particularly primary care populations.1 The design of health care exchanges within the Affordable Care Act will make the issues of risk stratification important as more patients are managed through a capitated payment system or have penalties for readmission.2,3 One of the most commonly used methods of risk stratification is the assignment of medical tiers involving a higher tier with an increasing number of comorbid health deficits.4,5 Risk stratification often uses data obtained from administrative billing data from an electronic medical record.6,7 While such approaches are fairly robust, they are limited to recorded diagnoses and do not integrate new biology and biomarkers that are rapidly being developed and translated to clinical practice.
Biobanks are critical for biomarker discovery and translation, but few are used in primary care. The Mayo Clinic Center for Individualized Medicine has initiated the Mayo Clinic Biobank, a prospective cohort of Mayo Clinic patients enrolled from multiple departments, irrespective of disease history at enrollment. A large number of participants in the Biobank are enrolled from primary care clinics. To identify and build an infrastructure for biomarker research in primary care populations, we identified participants in the Mayo Clinic Biobank who received their primary care at Mayo Clinic in Rochester as part of the Employee and Community Health (ECH) practice panel (Biobank-ECH). In order to assess their representativeness of the overall ECH population, we investigated whether risk stratification using Minnesota medical tiering8 predicted hospitalization and emergency department (ED) use in a similar manner. We hypothesized that the tiering model should perform well to predict hospitalizations and ER visits for the Biobank-ECH participants at a similar magnitude to the overall ECH panel. If established, this would enhance the validity of using this subset to assess the role of biomarkers in predicting outcomes within a primary care population.
METHODS
Study Participants and Setting
This study was reviewed and approved by the Mayo Clinic Institutional Review Board (IRB). The Mayo Clinic Biobank began enrollment on April 1, 2009, and by December 31, 2011, 22,916 participants had enrolled, mainly from internal and family medicine departments. Participants provided a “registry” consent that allowed use of their biological specimens, questionnaire data, and electronic medical record data for IRB-approved research studies conducted by Mayo Clinic investigators. ECH is the primary care practice at Mayo Clinic, which serves patients from Olmsted County, MN, and southeastern Minnesota. As part of ECH’s Minnesota Department of Health certification as a medical home,8 ECH patients were enrolled into provider panels and had Minnesota tiering applied to help determine the need for additional services such as case management. Only individuals who were empanelled as of December 31, 2010, and were aged 18 years and older were included in this study. Subjects were followed for health care outcomes through December 31, 2011. Of 90,409 patients within the ECH panel as of December 31, 2010, 84,872 (93.9%) gave consent for medical record review.
We linked all Biobank participants as of December 31, 2010 (n=16,576) to the ECH panel by Mayo Clinic patient medical record number in order to identify the subset of participants in the ECH panel.
Minnesota Tiering
The Minnesota tiering scores were calculated on December 31, 2010, for all ECH members. The Minnesota tiering method was based on the Johns Hopkins Adjusted Clinical Groups (ACG).9 Minnesota tiering is currently the standard for medical risk stratification for payment of care coordination for medical home patients within Minnesota.10 Based on the information obtained from ICD-9 codes from billing data for the 12 months previous, the model categorizes patients into 5 tiers defined as tier 0 (no chronic conditions), 1 (1–3 conditions), 2 (4–6 conditions), 3 (7–9 conditions) and 4 (10 or more conditions). The coding methodology is available from the State of Minnesota.11
Outcomes
The primary outcomes of this study were hospitalization and ER visits based on utilization as determined from institutional billing systems. Hospitalization included a stay that was overnight and excluded outpatient hospital services (i.e., colonoscopy and outpatient surgery). ER visits resulting in an inpatient stay were only counted as hospitalizations. The admission dates for hospitalization and ER visits served as event dates in the analysis. Thirty-day re-hospitalization after the date of discharge from the first hospitalization was also considered as an outcome of interest.
Statistical Analysis
Demographic characteristics and Minnesota tiering scores of the Biobank-ECH participants were summarized in percentages and compared with the overall ECH panel. The effects of sex on different tiering scores were assessed using the Pearson chi-square test for both the Biobank-ECH and overall ECH groups. Kruskal-Wallis tests were performed for the association between age and tiering scores.
Kaplan-Meier plots and Cox proportional hazards models (accounting for age and sex) were utilized to examine the association of tiering scores with the selected outcomes of interest (hospitalization, ER visits, and 30-day re-hospitalization after the first hospitalization). After evaluating the proportionality assumption of the Cox model, hazard ratios (HR) and their 95% confidence intervals (CI) for each risk tier were presented, with the lowest risk tiers (tier 0 and 1 combined) serving as the reference group.
RESULTS
Participant Characteristics
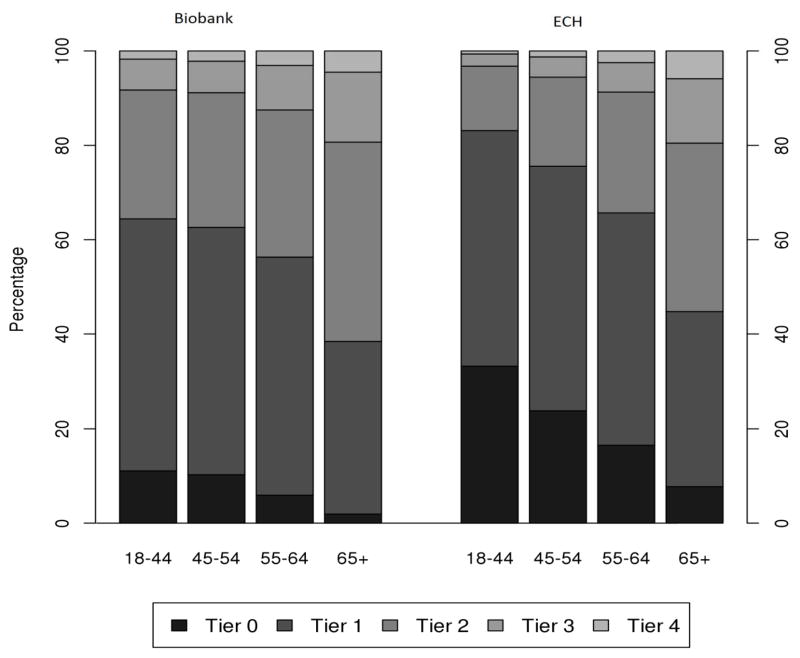
There were 8,927 Biobank participants enrolled in the ECH panel (i.e. Biobank-ECH) as of the end of December 2010. As shown in Table 1, Biobank-ECH participants were more likely to be female (64.3%) and older (median age 58 years) compared to the overall ECH panel (54.6% female and median age 47 years). The older age distribution is mainly driven by the lower percentage of people aged 18–39 years in the Biobank-ECH (17.0%) compared to the overall ECH panel (37.9%), and the higher percentage of people aged 70 years and older in the Biobank-ECH (24.1%) compared to the overall ECH panel (13.5%). Figure 1 highlights the differences in age distribution of the Biobank-ECH participants relative to the overall ECH panel.
TABLE 1.
Demographic characteristics and Minnesota tiering scores of Biobank participants in the ECH panel, compared to the whole ECH populationa
| Biobank-ECH (n=8,927) | ECH (n=84,872) | |
|---|---|---|
| Female sex (%) | 64.3 | 54.6 |
| Median age as of 12/31/2010 (25th and 75th percentiles) | 58 (46 – 69) | 47 (32 – 60) |
| Age groups (%) | ||
| <30 | 7.9 | 20.7 |
| 30 – 39 | 9.1 | 17.2 |
| 40 – 49 | 13.6 | 17.7 |
| 50 – 59 | 23.6 | 19.0 |
| 60 – 69 | 21.7 | 11.7 |
| 70 – 79 | 17.4 | 7.9 |
| 80+ | 6.7 | 5.6 |
| Minnesota medical home tiers (%) | ||
| Tier 0 | 6.4 | 24.0 |
| Tier 1 | 46.4 | 47.7 |
| Tier 2 | 33.9 | 20.7 |
| Tier 3 | 10.2 | 5.6 |
| Tier 4 | 3.1 | 2.0 |
ECH = Employee and Community Health
Figure 1.
Age distribution of Biobank participants in ECH panel and overall ECH panel.
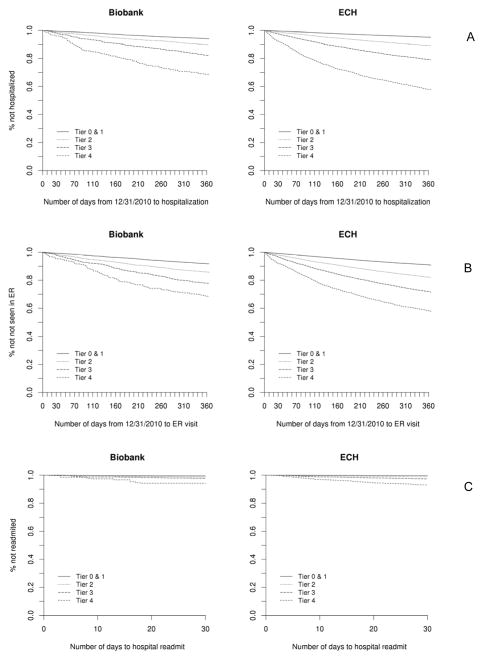
Based on Minnesota tiering (Table 1), Biobank-ECH participants were less likely to be in the healthiest tier (tier 0, 6.4%) compared to the overall ECH panel (24.0%); were similar for tier 1 (46.4% compared to 47.7%); were enriched for combined tiers 2 and 3 (44.1% compared to 26.3%); and were similar for tier 4 (3.1% compared to 2.0%). In comparing the absolute number of medical conditions, there were no significant differences between ECH patients and Biobank-ECH patients in each tier group. Figure 2 depicts the distribution of medical tiering within each age group and shows that older age is associated with a shift to higher tiers for both the Biobank-ECH and the overall ECH.
Figure 2.
Percentages of Minnesota tiering scores (tier 0–4) at each age group (18 – 44, 45 – 54, 55 – 64, and 65 or older) for Biobank in ECH panel and the overall ECH.
Tiering and Outcome
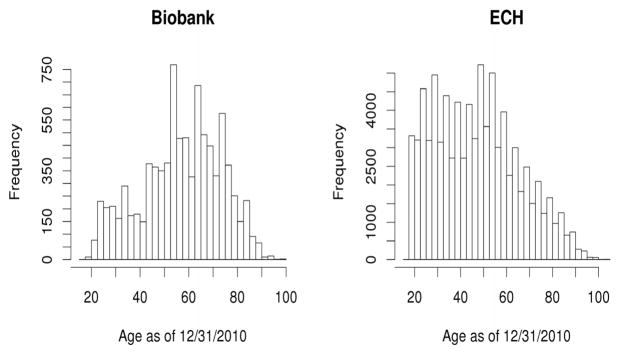
There was a significant positive association of medical tier with risk of hospitalization, ER visits, and 30-day re-hospitalization in the Biobank-ECH and the ECH overall groups as shown in Kaplan-Meier plots (Figure 3) and in age- and sex-adjusted Cox models (Tables 2 and 3). Specifically, among Biobank-ECH participants, risk tiering (tier 4 vs combined tiers 0 and 1) was strongly associated with risk of hospitalization (HR=5.8; 95% CI, 4.6–7.5), ER visits (HR=5.4; 95% CI, 4.2–6.8), and 30-day re-hospitalization (HR=9.0, 95% CI, 4.7–17.2). Similar, albeit stronger, associations for risk of hospitalization (HR=8.5; 95% CI, 7.8–9.3), ER visits (HR=6.9; 95% CI, 6.4–7.5), and 30-day re-hospitalization (HR=13.3; 95% CI, 10.4–16.9) were observed for all of ECH. However, lack of power prevented the detection of differences in risk of 30-day re-hospitalization. Of note, the HRs for tiers 2 and 3 were of similar magnitude for the 2 groups.
Figure 3.
Kaplan-Meier curves for comparing different tiering groups: (A) Hospitalization within 1-year; (B) ER visits within 1-year; and (C) 30-day re-hospitalization after the first hospitalization.
TABLE 2.
Minnesota tiering stratification of age and sex for Biobank participants in ECH panel, and age- and sex-adjusted HR and 95% CI of each outcome (hospitalization and ER visits within 1 year, and 30-day re-hospitalization)a
| Minnesota Medical Home tiers
|
||||||
|---|---|---|---|---|---|---|
| Tier 0 | Tier 1 | Tier 2 | Tier 3 | Tier 4 | P value | |
| Female sex (%) | 62.7 | 63.7 | 64.7 | 65.5 | 69.8 | 0.22b |
| Median age as of 12/31/2010 (y) | 48 | 55 | 63 | 66 | 65 | <0.001b |
| Hospitalization within one year (n) | 275 | 311 | 161 | 87 | <0.001c | |
| HR (95% CI)d | Reference | 1.7 (1.4–2.0) | 3.0 (2.4–3.6) | 5.8 (4.6–7.5) | ||
| ER visits within one year (n) | 389 | 435 | 201 | 88 | <0.001c | |
| HR (95% CI)d | Reference | 2.0 (1.7–2.3) | 3.4 (2.8–4.0) | 5.4 (4.2–6.8) | ||
| 30-day re-hospitalization (n) | 25 | 37 | 20 | 16 | <0.001c | |
| HR (95% CI)d | Reference | 2.0 (1.2–3.4) | 3.5 (1.9–6.3) | 9.0 (4.7–17.2) | ||
ECH = Employee and Community Health; ED = emergency department.
P values for overall tiering group differences on sex and age.
P values for overall tiering group effect on each outcome, adjusting for age and sex.
HRs and 95% CIs for comparing each tier group to the combined tiers 0 and 1, adjusting for age and sex.
TABLE 3.
Minnesota tiering stratification of age and sex for the overall ECH panel, and age- and sex-adjusted HR and 95% CI of each outcome (hospitalization and ER visits within 1 year, and 30-day re-hospitalization)a
| Minnesota Medical Home tiers
|
||||||
|---|---|---|---|---|---|---|
| Tier 0 | Tier 1 | Tier 2 | Tier 3 | Tier 4 | P value | |
| Female sex (%) | 42.6 | 55.3 | 63.4 | 64.4 | 64.4 | <0.001b |
| Median age as of 12/31/2010 (y) | 37 | 45 | 55 | 62 | 67 | <0.001b |
| Hospitalization within one year (n) | 2940 | 1903 | 980 | 710 | <0.001c | |
| HR (95% CI)d | Reference | 2.0 (1.9–2.1) | 3.8 (3.5–4.1) | 8.5 (7.8–9.3) | ||
| ER visits within one year (n) | 5549 | 3145 | 1321 | 695 | <0.001c | |
| HR (95% CI)d | Reference | 2.2 (2.1–2.3) | 3.9 (3.7–4.2) | 6.9 (6.4–7.5) | ||
| 30-day re-hospitalization (n) | 221 | 181 | 121 | 123 | <0.001c | |
| HR (95% CI)d | Reference | 2.3 (1.9–2.8) | 5.1 (4.0–6.4) | 13.3 (10.4–16.9) | ||
ECH = Employee and Community Health; ED = emergency department.
P values for overall tiering group differences on sex and age.
P values for overall tiering group effect on each outcome, adjusting for age and sex.
HRs and 95% CIs for comparing each tier group to the combined tiers 0 and 1, adjusting for age and sex.
DISCUSSION
We found that the subset of the Mayo Clinic Biobank who were part of a primary care panel were more likely to be older, female, and have more chronic conditions compared to the overall ECH primary care panel. This is not unexpected, since most participants were recruited into the Biobank through mailings in advance of prescheduled appointments at Mayo Clinic. This approach will enrich for people who seek medical care, including those who are older, female, and have more chronic conditions, which we observed. In particular, the Biobank-ECH group underrepresents people under the age of 40 years relative to the ECH panel. This age group is much less likely to need medical care and due to the recruitment strategy has a lower probability of being invited.12 Furthermore, participation rates are generally lower for this age group.13 As expected, with increasing age, there was a shift towards higher tiers in both the Biobank-ECH and the overall ECH panel, showing the clear association of chronic conditions with age. Of importance, at each age level, Biobank-ECH was enriched for people in tiers 2 and 3 (4–9 chronic conditions), deficient in tier 0 (no chronic conditions), and of similar magnitude for tiers 1 and 4 relative to the overall ECH.
While Biobank-ECH participants were older and had more chronic conditions compared to the overall ECH panel, the associations for Minnesota medical tiering with health outcomes showed similar, albeit weaker, associations with risk of hospitalization, ER visits, and 30-day re-hospitalization in the Biobank-ECH compared to all ECH participants. The participants in both the ECH and the Biobank-ECH groups had a similar absolute number of chronic conditions within each tier; thus, the medical burden was the same within a tier. These differences likely reflect the low number of tier 0 participants, and may also reflect the total number and severity of health conditions in tier 4. Patients with very poor health would have been unlikely to travel to the clinic in Rochester to enroll in the Biobank.
The systematic differences identified here will need to be considered when making any inferences about the primary care derived from studies using the Biobank-ECH sample. However, the enrichment of older persons and persons in higher tiers in the Biobank-ECH sample also enriches for outcomes, thereby increasing the study power. While the association of tiering with risk of hospitalization, ER visits, and 30-day re-hospitalization were slightly weaker for tier 4 in the Biobank-ECH, the overall patterns of association were similar and the HRs were similar for tiers 2 and 3. The evidence in support of using tiering to predict hospitalization or ER visits is limited; however, tiering is based on the ACG risk stratification system which has been widely studied. The ACG system has a good predictive value of hospitalization with an area under the curve of 0.80 with a sensitivity of 46% and specificity of 91%.14 Since the operating characteristics of tiering should be consistent regardless of population, new frailty indexes using comorbid health burden and new biomarkers can be defined and developed within a wide range of populations,5,15 including the Biobank-ECH group.
There are limitations to this study. For the outcomes of hospitalization and ER visits, if the participant sought care outside of the Mayo Clinic medical system, there was a potential for missing outcomes. However, all members of the ECH panel receive their primary care within the Mayo Clinic system; thus, the potential for missing data is minimized. Tiering is based upon medical billing diagnostic codes which could be miscoded or missing. The ability to generalize this information may be limited to similar populations in terms of race/ethnicity, insurance status, and availability of primary care.
In summary, Mayo Clinic Biobank participants in a primary care panel can serve as a laboratory to identify new biologic markers and merge clinical and genomic data for risk stratification for hospitalization and ER visits in the primary care setting. While the current tiering works reasonably well, there is a need to improve risk stratification for hospitalization in primary care.
Acknowledgments
Financial support
The Mayo Clinic Biobank is supported by the Mayo Clinic Center for Individualized Medicine.
Abbreviations and Acronyms
- ACG
adjusted clinical groups
- CI
confidence interval
- ECH
employee and community health
- ED
emergency department
- HR
hazard ratio
- IRB
institutional review board
Footnotes
Disclosure:
The authors have no conflict of interest to declare.
References
- 1.McKinney M. Preparing for impact. Many hospitals will struggle to escape or absorb penalty for readmissions. Modern healthcare. 2012;42:6–7. 16, 11. [PubMed] [Google Scholar]
- 2.Weiner JP, Trish E, Abrams C, Lemke K. Adjusting for risk selection in state health insurance exchanges will be critically important and feasible, but not easy. Health Affairs. 2012;31:306–315. doi: 10.1377/hlthaff.2011.0420. [DOI] [PubMed] [Google Scholar]
- 3.Navarro AE, Enguidanos S, Wilber KH. Identifying risk of hospital readmission among Medicare aged patients: an approach using routinely collected data. Home health care services quarterly. 2012;31:181–195. doi: 10.1080/01621424.2012.681561. [DOI] [PubMed] [Google Scholar]
- 4.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62:722–727. doi: 10.1093/gerona/62.7.722. [DOI] [PubMed] [Google Scholar]
- 5.Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27:17–26. doi: 10.1016/j.cger.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Crane SJ, Tung EE, Hanson GJ, Cha S, Chaudhry R, Takahashi PY. Use of an electronic administrative database to identify older community dwelling adults at high-risk for hospitalization or emergency department visits: the elders risk assessment index. BMC health services research. 2010;10:338. doi: 10.1186/1472-6963-10-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naessens JM, Stroebel RJ, Finnie DM, et al. Effect of multiple chronic conditions among working-age adults. Am J Manag Care. 2011;17:118–122. [PubMed] [Google Scholar]
- 8.Minnesota Department of Health. Health Care Homes: MHCP Fee-For Service Care Coordination Rate Methodology. 2013 http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_CONVERSION&RevisionSelectionMethod=LatestReleased&dDocName=dhs16_151292.
- 9.Weiner JP, Starfield BH, Steinwachs DM, Mumford LM. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care. 1991;29:452–472. doi: 10.1097/00005650-199105000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Health Care Homes 256B.0751. United States: Minnesota Legistature; 2011. https://www.revisor.mn.gov/statutes/?id=256B.0751. [Google Scholar]
- 11.Minnesota Department of Health. Care Coordinator Tier Assignment Tool, Version 1. http://www.health.state.mn.us/healthreform/homes/payment/HCHComplexityTierTool_March2010.pdf.
- 12.Schiller J, Lucas J, Peregoy J. Summary health statistics for US adults: National Health Interview Survey, 2011. Vol. 10. National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 13.Ridgeway JL, Han LC, Olson JE, et al. Potential Bias in the Bank: What Distinguishes Refusers, Non-responders and Participants in a Clinic-based Biobank? Public Health Genomics. 2013 doi: 10.1159/000349924. accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lemke KW, Weiner JP, Clark JM. Development and Validation of a Model for Predicting Inpatient Hospitalization. Med Care. 2012;50:131–139. doi: 10.1097/MLR.0b013e3182353ceb. [DOI] [PubMed] [Google Scholar]
- 15.Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24. doi: 10.1186/1471-2318-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]