Abstract
Targeting the oxygen stress response pathway is considered a promising strategy to exert antineoplastic activity in a broad spectrum of tumor types. Supporting this view, we summarize the mechanism of action of Taurolidine and Piperlongumine, two antineoplastic agents with strikingly broad tumor selectivity. Taurolidine enhances the oxidative stress (ROS) selectively in tumor cells. Its cytotoxicity for various tumor cells in vitro and in vivo, which includes tumor stem cells, is based on the induction of programmed cell death, largely via apoptosis but also necroptosis and autophagy. The redox-directed mechanism of action of Taurolidine is apparent from the finding that reducing agents e.g., N-acetylcysteine or glutathione impair its cytotoxicity, while its effectiveness is enhanced by agents which inhibit the cellular anti-oxidant capacity. A similar redox-directed antineoplastic action is shown by Piperlongumine, a recently described experimental drug of plant origin. Taurolidine is particularly advantageous in surgical oncology as this taurine-derivative can be applied perioperatively or systemically with good tolerability as shown in initial clinical applications.
Keywords: antineoplastic agent, reactive oxygen species, apoptosis, autophagy, necroptosis
1. Introduction
A redox disequilibrium has been recognized in recent years as a specific vulnerability of various tumor cells (1–3). By exacerbating the oxidative stress, pro-oxidant drugs achieve antineoplastic activity in a multitude of cancer cells (1,4–6). Non-malignant cells, with their high anti-oxidant capacity, are largely resistant to the same degree of deviation from the redox equilibrium resulting in a high selectivity of such drugs for tumor cells (2,4–7). In the present review, Taurolidine is described as a redox-directed cancer therapeutic with a broad spectrum of antineoplastic action. In first clinical application in surgical oncology, Taurolidine was well tolerated in patients with glioblastoma and gastrointestinal cancers (8–13). In support of the ROS stress pathway being an effective target for broad antineoplastic action, the anticancer activity of Piperlongumine, a plant-derived experimental agent (14,15), is briefly outlined.
2. Redox-directed cancer therapeutics
Cancer arises through a multistep, mutagenic process (‘oncogene dependency’) whereby cancer cells acquire a common set of properties that enable tumor cells to proliferate and disseminate metastases (16). As an adaptive response, non-oncogenic pathways such as the oxidative stress response pathways, are also affected (1,2). Reactive oxygen species (ROS), the key mediators of cellular oxidative stress involved in cancer initiation and progression, have recently emerged as promising targets for anticancer drug development. Cancer cells have been reported to harbor elevated levels of ROS and the ability to cope with chronically elevated levels of cellular stress is compromised in a multitude of cancer cells (1–3,17). This specific vulnerability of various tumor cells was termed ‘non-oncogene dependency’ or ‘non-oncogene addiction’ (1,4,14). Importantly, this dependency may not be shared by many non-transformed cells (3–5,7). Their basal ROS levels are low and their anti-oxidant capacity is robust due to the activation of Nrf2, the master regulator of anti-oxidant responses which includes the induction of anti-oxidant enzymes such as catalase or glutathione-S-transferase (3,5,7).
In keeping with this hypothesis, small molecular weight pro-oxidant drugs, which enhance the oxidative stress in tumor cells, are considered as potential antineoplastic agents (2,3,6,15). In contrast, due to the lower basal ROS levels and elevated anti-oxidant capacity, the same pro-oxidant deviation from redox homeostasis would be tolerated by non-malignant cells leading to minimal side-effects (1–3,6,14).
In the age of molecularly targeted therapy, drugs with pleiotropic actions such as redox-directed agents, frequently find limited enthusiasm based on the expectation of off-target toxic effects. However, as exemplified in this review, at least some redox-directed agents appear to act selectively on tumor cells. In addition, recent research suggests that it is exactly the pleiotropic mode of action which seems to be uniquely tailored to overcome cancer cell drug resistance originating from a redundancy of oncogenic signaling and rapid mutation (3,6).
3. Broad-spectrum antineoplastic activity of Taurolidine
Taurolidine, first synthesized in the 1970s (18) as bis(1,1- dioxoperhydro-1,2,4-thiadizinyl-4)methane, was originally known for its antibacterial and anti-toxin (exo/endotoxin) activity and was tested clinically in the 1980’s in the treatment of severe surgical infections, abdominal sepsis and peritonitis (10,11,13). Its antineoplastic activity became apparent in colony forming assays, in which dissociated cells were seeded at very low density and incubated for 2 to 4 weeks. Taurolidine potently prevented cell proliferation (EC50, 1 to 7 μg/ml) as shown for glioma cell lines (19–21) as well as ex vivo human glioblastoma cells (19). In addition, at higher concentrations, Taurolidine induced acute cytotoxicity (EC50, 40 to 80 μg/ml), tested at 24–72 h incubation, as shown for a multitude of cultured tumor cell lines such as mesothelioma (22–24), prostate (21,25), glioblastoma (19,20,26,27), ovarian (21,28), leukemia (28), colon (21,29–36), melanoma (21,37,38), osteosarcoma (40,41), pancreatic (41), lung (21), esophageal (42) and fibrosarcoma (41,43) as partly summarized by Jacobi et al (44). The effectiveness of Taurolidine in vitro was largely confirmed in vivo using various tumor cell lines as xenografts such as mesothelioma (23), prostate (25), ovarian (21,45), colon (29–31,34,35) and melanoma (37,46) as well as melanoma cells in a metastatic tumor model (46).
4. ROS-dependent cytotoxicity of Taurolidine
As first demonstrated in glioblastoma cells (19), a ROS-dependent mechanism of Taurolidine-induced cell death became apparent in many tumor cell types. Taurolidine increased the level of ROS as shown in glioblastoma (19) and mesothelioma cells (22,24). The reducing agent N-acetylcysteine (NAC) was able to block or strongly reduce the cytotoxicity in nearly all tumor cells such as glioblastoma (20), mesothelioma cells (22,24), colon carcinoma HT29 cells (47) and Chang liver cells (47) although not in fibrosarcoma HT1080 cells (47). Addition of glutathione similarly prevented cytotoxicity as shown for mesothelioma cells (22). Conversely, a reduction of the glutathione level with DL-buthionin-(S,R)-sulfoximine (BSO) enhanced the ability of Taurolidine to induce cell death as shown for glioblastoma cells (20) as well as colon and pancreas carcinoma cells (47). These results underline the central role of ROS in triggering the Taurolidine-induced programmed cell death. Molecularly, Taurolidine may interfere with regulators of redox and ROS homeostasis such as glutathione-S transferase 1.
5. Taurolidine and cancer stem cells
In most tumors, the hierarchical model of tumor formation is thought to be operative with cancer stem cells (CSC) contributing to self-renewal and regrowth after debulking of tumor mass by surgery or radiation (16) e.g., in glioblastoma (48). Taurolidine exerted potent cytotoxic activity against murine and human glioma CSCs with ED50, 12±2 μg/ml and EC50, 13±2 μg/ml, respectively. The CSCs were isolated by the formation of neurospheres from either the murine SMA 560 glioma cell line or from tissue resected from newly diagnosed WHO grade IV glioblastoma patients (KF, unpublished data). These results extend the effectiveness of redox-directed cytotoxicity to CSCs and may strengthen the therapeutic potential of Taurolidine.
6. Sparing of normal cells by Taurolidine
Non-tumor cells in vitro such as bone marrow cells (28), NIH-3T3 fibroblasts (21), non-neoplastic mesothelial cells (22) were not affected by Taurolidine under conditions of tumor cell cytotoxicity. Similarly, in vivo, physiological cell proliferation such as leukopoiesis or erythropoiesis (28,31,44) were practically not affected by Taurolidine. The apparent selective induction of cytotoxicity in cancer cells distinguishes Taurolidine from other molecules that partly affect ROS levels, such as paclitaxel, bleomycin, cisplatin or the glutathione synthesis inhibitor BSO (6,49–53).
7. Good tolerability of Taurolidine in patients
Initially, Taurolidine was tested as an intraperitoneal and intravenous adjunct in the treatment of severe surgical infections (sepsis, peritonitis, pancreatitis), exploiting its activity against antibiotic-resistant bacteria and bacterial toxins. Taurolidine showed good tolerability (10,11,13). In the first clinical experiences with cancer patients in surgical oncology, Taurolidine was likewise well tolerated. In a first case report, a patient with gastric cancer re-recurrence was palliatively treated with 2% Taurolidine i.v. for 39 cycles, each cycle consisting of 7 days of treatment per month (300 mg/kg body weight per day). The patient was in good clinical condition as shown by the relevant blood parameters which included an undisturbed leukopoesis and thrombopoesis and no sign of toxicity (9). In a clinical experience with two patients with progressive, non-resectable glioblastoma and conventional therapy, the neurological condition and the quality of life improved in both patients with no sign of tumor progression (‘partial remission’) following two cycles of 21 days each with 2% Taurolidine i.v. (20 g/day) (8). In 11 patients with progresssive metastatic melanoma, co-administration of Taurolidine with high rIL-2 enhanced the tolerability of this regime (54). In a multicenter prospective randomized trial, patients with different resectable gastrointestinal (GI) cancers (20 patients each with colon, pancreas or stomach cancer) were treated with a perioperative lavage (2×10 min) consisting of 0.5% Taurolidine/heparin versus 0.25% povidone- iodine (control). Taurolidine resulted in a reduction of inflammatory cytokines (IL-1, IL-6, IL-10) at 2 and 6 h as measured in peritoneal fluid compared to pre-resection levels (12). There was no change in serum leukocytes and the perioperative complications did not differ. Up to now, the number of GI cancer patients in each group has remained insufficient for a statistical analysis of disease outcome following Taurolidine treatment (12). Nevertheless, in these oncological surgical interventions, Taurolidine did not interfere with post-operative wound healing, which was also demonstrated in a study on the use of Taurolidine in coronary artery bypass grafting in 60 patients (55). These findings confirmed previous findings in rats in which the scar tissue biopsies were examined macroscopically and histopathologically following Taurolidine treatment (56). The perioperative use of Taurolidine solution (2%) in surgical oncology (57) promises to be of special benefit as it is administered at the earliest possible therapeutic time window. Perioperatively, circulating tumor cells, which correlate negatively with disease free survival and overall survival (58), would be the prime targets for Taurolidine. By its ability to be cytotoxic to tumor cells and tumor stem cells, perioperative Taurolidine promises to reduce micrometastases and increase survival, as substantiated in a pancreatic cancer model (59). The majority of clinical studies relates to the intraperitoneal administration of Taurolidine, especially in the setting of peritonitis (11,13). In intravenous studies, vein irritation at high doses has been experienced, necessitating direct central administration or peripherally via a PICC line (57).
8. Potency of action and plasma levels in patients
Due to its short half-life in man (60) Taurolidine is usually administered by intravenous infusion (2% Taurolidine). When administered i.v. intermittently to glioblastoma patients, Taurolidine reached a maximal plasma level of 83±18 μg/ml (61), which is similar to peak values obtained in acutely treated healthy volunteers (60). This plasma concentration is expected to be clinically effective. It is about 20 times higher than the antiproliferative effective concentration of Taurolidine and is in the range of its cytotoxic potency.
9. Mechanisms of antineoplastic action
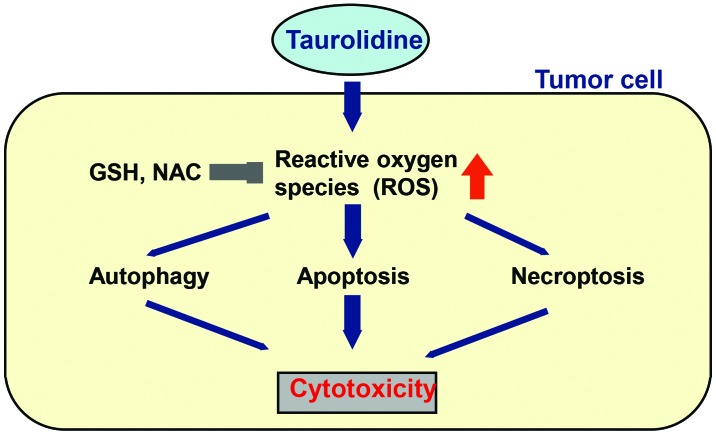
The ROS-dependent induction of programmed cell death by Taurolidine is based on a mixed type of cellular signaling, in particular the induction of caspase-independent apoptosis but also autophagy and programmed necrosis (necroptosis) (Fig. 1).
Figure 1.
The proposed antineoplastic action of Taurolidine. By increasing ROS, Taurolidine induces cytotoxicity in tumor cells largely by induction of apoptosis, but also autophagy and necroptosis. The degree to which these processes are involved may vary with the type of tumor cell. Reducing agents such as N-acetylcysteine (NAC) or glutathione (GSH) inhibit cytotoxicity, which supports the mechanism of redox-directed antineoplastic activity.
Apoptosis
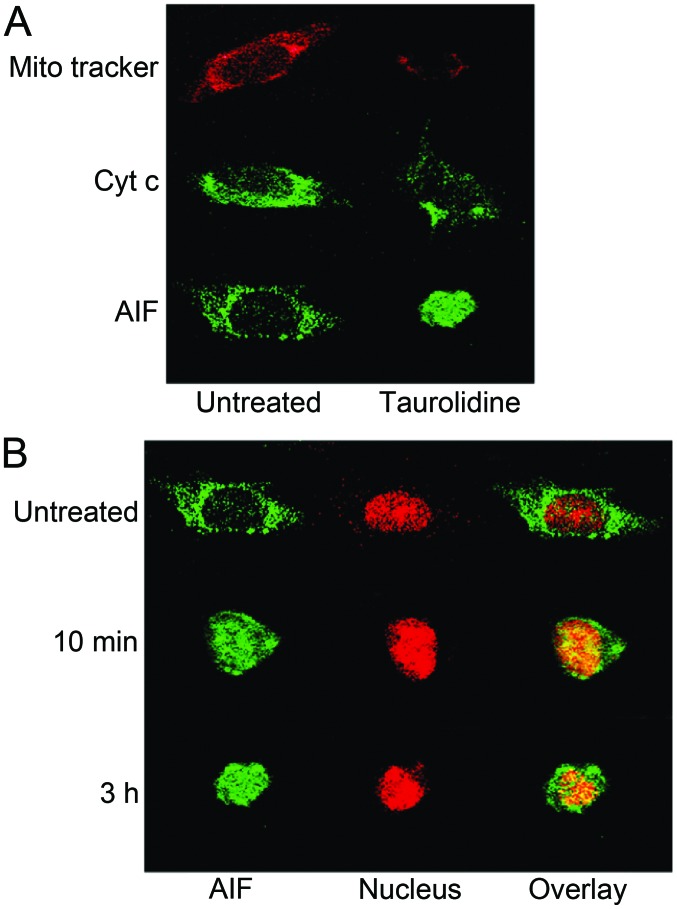
Induction of apoptosis by Taurolidine was first shown in ovarian tumor cells (21), also in mesothelioma cells (1,24) but was most extensively studied in glioma cells (19,20,26,27). Within minutes of incubation with Taurolidine, the ROS-induced mitochondrial stress signaling pathway was activated as shown by the depolarization and permeabilisation of the mitochondrial membrane of glioblastoma cells (Fig. 2). Concomitantly, as an inducer of apoptosis, the mitochondrial apoptosis-inducing factor (AIF) was transduced from the cytoplasm into the nucleus (Fig. 2) (19). In keeping with the redox-directed mechanism, this process was completely blocked by co-incubation with N-acetyl-cysteine (NAC) (19). This reducing agent prevented the Taurolidine-induced cell death in practically all tumor cells tested, as described above, supporting the view that induction of apoptosis is the main mechanism of Taurolidine-induced cytotoxicity (19,22,24,47). Other markers of apoptosis included condensation of chromatin, fragmentation of DNA, externalization of phosphatidylserine and blebbing of the plasma membrane (Fig. 3) (19–21,23,24,27).
Figure 2.
Initiation of the mitochondrial response pathway by Taurolidine (19). (A) Confocal microscopy images demonstrating Taurolidine-induced loss of mitochondrial membrane potential (red, visualized by MitoTracker) and translocation of Apoptosis-Inducing-Factor (AIF, green) from mitochondria to the nucleus in LN229 glioma cells after 2 h of Taurolidine treatment with 100 μg/ml. In contrast, cytochrome c (represented by the green punctate immunostaining) was not released. (B) Time dependency of the Taurolidine effect. AIF translocation, cell shrinkage, and nuclear condensation (chromatin stained red with PI) are detectable within 10 min after Taurolidine (100 μg/ml) treatment. For details see ref. 19.
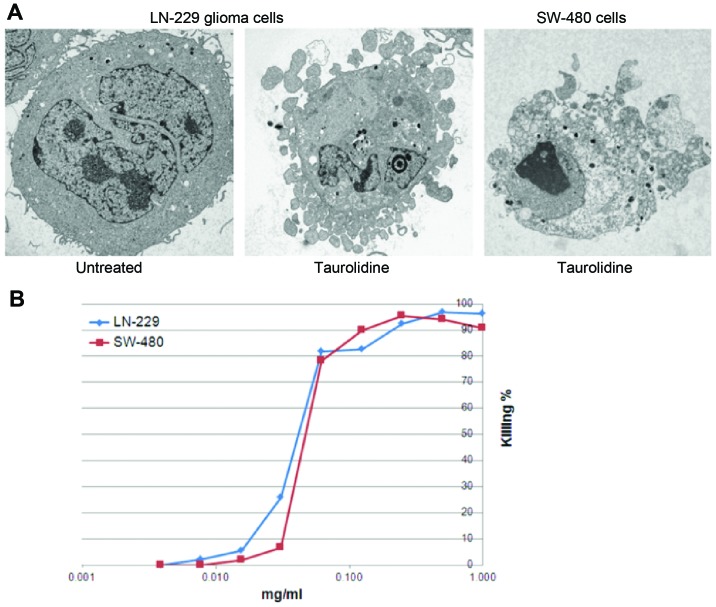
Figure 3.
(A) Ultrastructural evidence of Taurolidine (100 μg/ml, 12 h of treatment)-induced apoptosis in LN229 glioma cells and SW-480 colon adenocarcinoma cells as shown by blebbing of the plasma membrane and chromatin condensation. (B) Dose response of Taurolidine-induced cell death as shown for the human LN229 glioma and SW-480 colon adenocarcinoma cell lines. Electron microscopy and cytotoxicity were performed as described in ref. 20.
On the molecular level, the signaling pathways activated by Taurolidine, included the expression of pro-apoptotic transcription factors, the downregulation of the anti-apoptotoc regulator Bcl2, as well as the induction of genes involved in the ER stress response, in protein ubiquitination and in mitochondrial apoptotic pathways (42,62,63). Akt (but not Erk1,2) was inhibited (22). Taurolidine acted synergistically with TRAIL-induced apoptosis (42,63). In keeping with the ROS-dependent mechanism of action, Taurolidine was effective independent of whether p53 was mutated or not (19,20). A significant effect on DNA repair (PARP) was excluded, since PARP inhibition did not interfere with the cytotoxicity of Taurolidine (19,20).
Caspase-dependent pathways of apoptosis played a minor role. In glioblastoma cell lines, but not in ex vivo glioma cells, cytochrome c translocation was observed only to a very small extent (19,20). Nevertheless, after long-term incubation with Taurolidine (up to 48 h), some cytochrome c-dependent caspase activation (caspase 8 and 9) was apparent in prostate, colon and mesothelioma tumor cell lines since cytotoxicity was partly inhibited by a pan-caspase inhibitor (23,41,45). The primary molecular targets of Taurolidine remain to be identified.
Autophagy
States of cellular stress, including ROS formation, are known to be strong inducers of autophagy, a caspase-independent process of cell death. In this lysosomal process, cytoplasm and intracellular organelles are sequestered into autophagosomes and delivered to lysosomes for degradation. In glioblastoma cells, incubation with Taurolidine (6–24 h) induced autophagy in part of the cells as visualized by the sequestration and lysosomal degradation of intracellular oganelles using transmission electron microscopy (20,41). Autophagosomes were also detected by confocal microscopy (20). Inhibition by 3-methyl-adenine is likewise in keeping with autophagy (20). Autophagy represents an alternative mechanism of cytotoxicity in particular for apoptosis-resistant tumor cells (64).
Necrosis
The degree of Taurolidine-induced necrosis was variable. It was negligible in glioma cells but appeared more prevalent in pancreatic and fibrosarcoma cell lines (47). In glioma cell culture (LN229), Taurolidine within 24 h killed 90% of the cells as shown by the complete dissolution of the cell morphology (phase contrast microscopy before Annexin-V and PI staining). Of these cells, 53% were apoptotic, only 4.6% were necrotic (19,20). The latter was largely due to programmed necrosis (necroptosis) since pretreatment with necrostatin-1, a selective inhibitor of the receptor-interacting protein kinase RIP1, had some protective effect (about 40%) (20). The large number of unstained glioma cells (42%) may point to effects of Taurolidine beyond the induction of apoptosis and necrosis such as autophagy, as described above.
10. Supportive anti-angiogenic and anti-inflammatory activities of Taurolidine
Tumors are able to create a permissive microenvironment which includes the ability to induce neo-angiogenesis for maintaining the supply of oxygen and nutrients (16). Besides the induction of the programmed cell death, the antineoplastic activity of Taurolidine includes the inhibition of neo-angiogenesis. Taurolidine inhibited the adhesion of cultured endothelial cells (65), reduced the synthesis of VEGF but not of IL-6 (19,31) and potently inhibited the VEGF-induced formation of new blood vessels from human endothelial cells in vitro (lowest active concentration 1.25 μg/ml) (65). It remains to be seen, wether Taurolidine, besides its cytotoxic effect on tumor cells, may interfere with the neovascularization of tumors in vivo.
Taurolidine also showed anti-inflammatory activity as demonstrated early on by the suppression of E. coli endotoxin-induced endotoxemia (66) and the endotoxin-induced increase in IL-1β and TNFα synthesis in human peripheral blood monocytes (67) as well as the suppression of the stimulated release of IL-1β from peritoneal macrophages (34). There is a strong link between chronic inflammation and cancer, and NFκB is implicated as a key component in inflammation-induced tumorigenesis (68). In potentially attenuating this process, Taurolidine upregulated the NFκB inhibitor NFκBIA in fibrosarcoma and esophageal cancer cells (42,63). NFκB also regulates the release of the proinflammatory mediators IL-1, IL-6 and TNFα. The anti-inflammatory effect of Taurolidine was proposed to contribute, at least partially, to the attenuation of perioperative tumorigenesis by diminishing the surgery-related inflammation as shown in a rat melanoma model (46,57).
11. Piperlongumine, a broad-spectrum antineoplastic agent
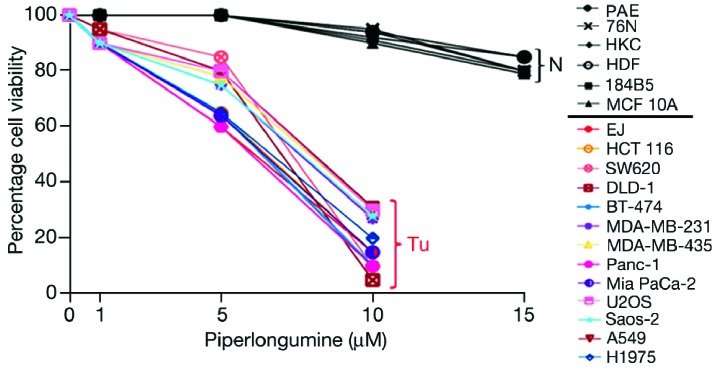
The plant alkaloid Piperlongumine (PL), which was previously reported to have antibacterial properties (69), was recently shown to display broad antineoplastic activity by targeting the ROS stress pathway in tumor cells. PL caused a marked increase in ROS selectively in cancer cells as shown in four cancer cell lines (incubation for 1 and 3 h) (14). PL dose-dependently induced cytotoxicity in all 13 different tumor cell lines tested with half maximal effects being reached at 6–8 μM (Fig. 4) (14). The increase in ROS in tumor cells and the cytotoxicity of PL was reduced by co-incubation with the enzyme catalase or blocked by the addition of NAC (14). PL is thought to interfere with redox and ROS homeostatic regulators such as glutathione-S transferase 1 or carbonyl reductase (14). PL, under comparable conditions, did not cause an increase of ROS or cytotoxicity in normal cells such as endothelial cells, breast epithelial cells, keratinocytes and skin fibroblasts (Fig. 4) (14). The PL-induced killing of a broad spectrum of tumor cell lines was based on a mixed type of cellular signaling based largely on the induction of apoptosis (70) but also of autophagy. The latter was triggered via the p38 protein kinase ROS stress response pathway (71). In prostate cells, inhibition of proliferation included the downregulation of the transcription factor NFκB (72). Thus, PL is an interesting broad-spectrum, redox-directed experimental antineoplastic agent.
Figure 4.
Piperlongumine treatment induces cell death in cancer cells but not in normal cells. Normal human cells (N), including aortic endothelial cells (PAE), breast epithelial cells (76N), keratinocytes (HKC) and skin fibroblasts (HDF), as well as two immortalized breast epithelial cell lines (184B5 and MCF 10A), were grown in 12-well or 24-well plates and treated with piperlongumine at 1–15 μM for 24 h. A variety of human cancer cell lines (Tu) were also treated with piperlongumine or DMSO (control) for 24 h. Cytotoxicity was measured by trypan blue exclusion staining (average of three independent experiments) (reproduced with permission from ref. 14).
12. Conclusions
Taurolidine is a representative of a novel class of redox-directed, broad-spectrum antineoplastic agents with tumor-selective cytotoxicity. It induces programmed cell death by targeting the oxidative stress response pathway which is compromised in many tumor cells. In initial applications in surgical oncology, Taurolidine i.v. was largely free of significant side-effects and merits further clinical evaluation. Applied perioperatively, Taurolidine promises to reduce circulating tumor cells, a negative predictor for disease-free survival. Taurolidine also inhibits VEGF-induced neo-angiogenesis and may therefore display a dual mode of antineoplastic action. Piperlongumine, an experimental plant-derived agent, is another redox-directed broad-spectrum antineoplastic agent with tumor cell selectivity.
References
- 1.Luo J, Solimini NL, Elledge SJ. Principles of cancer therapy: oncogene and non-oncogene addiction. Cell. 2009;136:823–837. doi: 10.1016/j.cell.2009.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trachootham D, Alexandre J, Huang P. Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discov. 2009;8:579–591. doi: 10.1038/nrd2803. [DOI] [PubMed] [Google Scholar]
- 3.Gorrini C, Harris IS, Mak TW. Modulation of oxidative stress as an anticancer strategy. Nat Rev Drug Discov. 2013;12:931–947. doi: 10.1038/nrd4002. [DOI] [PubMed] [Google Scholar]
- 4.Fruehauf JP, Meyskens FL., Jr Reactive oxygen species: a breath of life or death? Clin Cancer Res. 2007;13:789–794. doi: 10.1158/1078-0432.CCR-06-2082. [DOI] [PubMed] [Google Scholar]
- 5.Sporn MB, Liby KT. NRF2 and cancer: the good, the bad and the importance of context. Nat Rev Cancer. 2012;12:564–571. doi: 10.1038/nrc3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wondrak GT. Redox-directed cancer therapeutics: molecular merchanisms and opportunities. Antioxid Redox Signal. 2009;11:3013–3069. doi: 10.1089/ars.2009.2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kansanen E, Kuosmanen SM, Leinonen H, Levonen AL. The Keap1-Nrf2 pathway: mechanism of activation and dysregulation in cancer. Redox Biology. 2013;1:45–49. doi: 10.1016/j.redox.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stendel R, Picht T, Schilling A, Heidenreich J, Loddenkemper C, Jänisch W, Brock M. Treatment of glioblastoma with intravenous Taurolidine. First clinical experience. Anticancer Res. 2004;24:1143–1147. [PubMed] [Google Scholar]
- 9.Braumann C, Winkler G, Rogalla P, Menenakos C, Jacobi CA. Prevention of disease progression in a patient with a gastric cancer-recurrence. Outcome after intravenous treatment with the novel antineoplastic agent Taurolidine. Report of a case. World J Surg Oncol. 2006;4:34. doi: 10.1186/1477-7819-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCartney AC, Browne MK. Clinical studies on administration of taurolidine in severe sepsis: a preliminary study. Progr Clin Biol Res. 1988;272:361–371. [PubMed] [Google Scholar]
- 11.Staubach KH. Adjuvant therapy of peritonitis with taurolidine. Modulation of mediator liberation. Langenbecks Arch Chir. 1997;382:S26–S30. doi: 10.1007/pl00014640. [DOI] [PubMed] [Google Scholar]
- 12.Braumann C, Gutt CN, Scheele J, Menenakos C, Willems W, Mueller JM, Jacobi CA. Taurolidine reduces the tumor-stimulating cytokine IL 1beta in patients with resectable gastrointestinal cancer: a multicenter prospective randomized trial. World J Surg Oncol. 2009;7:32–45. doi: 10.1186/1477-7819-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wesch G, Petermann C, Linder MM. Drug therapy of peritonitis: 6-year experience with the chemotherapeutic agent and anti-endotoxin Taurolin. Fortschr Med. 1983;101:545–550. [PubMed] [Google Scholar]
- 14.Raj L, Ide T, Gurkar AU, Foley M, Schenone M, Li X, Tolliday NJ, Golub TR, Carr SA, Shamji AF, Stern AM, Mandinova A, Schreiber SL, Lee SW. Selective killing of cancer cells by a small molecule targeting the stress response to ROS. Nature. 2011;475:231–234. doi: 10.1038/nature10167. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Parkinson EI, Hergenrother PJ. Runaway ROS as selective anticancer strategy. Chem Med Chem. 2011;6:1957–1959. doi: 10.1002/cmdc.201100381. [DOI] [PubMed] [Google Scholar]
- 16.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 17.Szatrowski TP, Nathan CF. Production of large amounts of hydrogen peroxide by human tumor cells. Cancer Res. 1991;51:794–798. [PubMed] [Google Scholar]
- 18.Pfirrmann RW. In: Taurolin, ein neues Konzept zur antimikrobiellen Chemotherapie chirurgischer Infektionen. Brückner WL, Pfirrmann RW, editors. Urban and Schwarzenberg Verlag; 1985. (In German) [Google Scholar]
- 19.Rodak R, Kubota H, Ishihara H, Eugster HP, Könü D, Möhler H, Yonekawa Y, Frei K. Induction of reactive oxygen intermediates- dependent programmed cell death in human malignant ex vivo glioma cells and inhibition of the vascular endothelial growth factor production by Taurolidine. J Neurosurg. 2005;102:1055–1068. doi: 10.3171/jns.2005.102.6.1055. [DOI] [PubMed] [Google Scholar]
- 20.Stendel R, Biefer HR, Dékany M, Kubota H, Münz C, Wang S, Möhler H, Yonekawa Y, Frei K. The antibacterial substance Taurolidine exhibits anti-neoplastic action based on a mixed type of programmed cell death. Autophagy. 2009;5:194–210. doi: 10.4161/auto.5.2.7404. [DOI] [PubMed] [Google Scholar]
- 21.Calabresi P, Goulette FA, Darnowski JW. Taurolidine: cytotoxic and mechanistic evaluation of a novel antineoplastic agent. Cancer Res. 2001;61:6816–6821. [PubMed] [Google Scholar]
- 22.Aceto N, Bertino P, Barbone D, Tassi G, Manzo L, Porta C, Mutti L, Gaudio G. Taurolidine and oxidative stress: a rationale for local treatment of mesothelioma. Eur Respir J. 2009;34:1399–1407. doi: 10.1183/09031936.00102308. [DOI] [PubMed] [Google Scholar]
- 23.Nici L, Monfils B, Calabresi P. The effects of Taurolidine, a novel antineoplastic agent, on human malignant mesothelioma. Clin Cancer Res. 2004;10:7655–7661. doi: 10.1158/1078-0432.CCR-0196-03. [DOI] [PubMed] [Google Scholar]
- 24.Opitz I, Sigrist B, Hillinger S, Lardinois D, Stahel R, Weder W, Hopkins-Donaldson S. Taurolidine and povidone-iodine induce different types of cell death in malignant pleural mesothelioma. Lung Cancer. 2007;56:327–336. doi: 10.1016/j.lungcan.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 25.Darnowski JW, Goulette FA, Cousens LP, Chatterjee D, Calabresi P. Mechanistic and antineoplastic evaluation of Taurolidine in the DU145 model of human prostate cancer. Cancer Chemother Pharmacol. 2004;54:249–258. doi: 10.1007/s00280-004-0806-1. [DOI] [PubMed] [Google Scholar]
- 26.Stendel R, Stoltenburg-Didinger G, Brock M. Apoptotic changes in brain tumor cells induced by Taurolidine. J Cancer Res Clin Oncol. 2002;128:150. [Google Scholar]
- 27.Stendel R, Stoltenburg-Didinger G, Al Keikh CL, Wattroth M, Brock M. The effect of Taurolidine on brain tumor cells. Anticancer Res. 2002;22:809–814. [PubMed] [Google Scholar]
- 28.Ribizzi I, Darnowski JW, Goulette FA, Akhtar MS, Chatterjee D, Calabresi P. Taurolidine: preclinical evaluation of a novel, highly selective, agent for bone marrow purging. Bone Marrow Transplant. 2002;29:313–319. doi: 10.1038/sj.bmt.1703359. [DOI] [PubMed] [Google Scholar]
- 29.McCourt M, Wang JH, Sookhai S, Redmond HP. Taurolidine inhibits tumor cell growth in vitro and in vivo. Ann Surg Oncol. 2000;7:685–691. doi: 10.1007/s10434-000-0685-6. [DOI] [PubMed] [Google Scholar]
- 30.Nestler G, Schulz HU, Schubert D, Krüger S, Lippert H, Pross M. Impact of Taurolidine on the growth of CC531 coloncarcinoma cells in vitro and in a laparoscopic animal model in rats. Surg Endosc. 2005;19:280–284. doi: 10.1007/s00464-003-9301-8. [DOI] [PubMed] [Google Scholar]
- 31.Braumann C, Schoenbeck M, Menenakos C, Kilian M, Jacobi CA. Effects of increasing doses of a bolus injection and an intravenous long-term therapy of Taurolidine on subcutaneous (metastic) tumor growth in rats. Clin Exp Metastasis. 2005;22:77–83. doi: 10.1007/s10585-005-4695-4. [DOI] [PubMed] [Google Scholar]
- 32.Hoksch B, Rufer B, Gazdhar A, Bilici M, Beshay M, Gugger M, Schmid RA. Taurolidine in the prevention and therapy of lung metastases. Eur J Cardiothorac Surg. 2009;36:1058–1063. doi: 10.1016/j.ejcts.2009.04.065. [DOI] [PubMed] [Google Scholar]
- 33.Chromik AM, Daigeler A, Hilgert C, Bulut D, Geisler A, Liu V, Otte JM, Uhl W, Mittelkötter U. Synergistic effects in apoptosis induction by Taurolidine and TRAIL in HCT-15 colon carcinoma cells. J Investigat Surg. 2007;20:339–348. doi: 10.1080/08941930701772157. [DOI] [PubMed] [Google Scholar]
- 34.Jacobi C, Peter FJ, Wenger FA, Ordemann J, Müller JM. New therapeutic strategies to avoid intra- and extraperitoneal metastases during laparoscopy: results of a tumor model in the rat. Dig Surg. 1999;16:393–399. doi: 10.1159/000018754. [DOI] [PubMed] [Google Scholar]
- 35.Jacobi C, Sabat R, Ordemann J, Wenger F, Volk H, Müller J. Peritoneal instillation of taurolidine and heparin for preventing intraperitoneal tumor growth and trocar metastases in laparoscopic operations in the rat model. Langenbecks Arch Chir. 1997;382:S31–S36. doi: 10.1007/pl00014641. [DOI] [PubMed] [Google Scholar]
- 36.Jacobi CA, Ordemann J, Böhm B, Zieren HU, Sabat R, Müller JM. Inhibition of peritoneal tumor cell growth and implantation in laparoscopic surgery in a rat model. Am J Surgery. 1997;174:359–363. doi: 10.1016/s0002-9610(97)00099-8. [DOI] [PubMed] [Google Scholar]
- 37.Braumann C, Jacobi CA, Rogalla S, Menenakos C, Fuehrer K, Trefzer U, Hofmann M. The tumor suppressive reagent Taurolidine inhibits growth of malignant melanoma - a mouse model. J Surg Res. 2007;143:372–378. doi: 10.1016/j.jss.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 38.Sun BS, Wang JH, Liu LL, Gong SL, Redmond HP. Taurolidine induces apoptosis of murine melanoma cells in vitro and in vivo by modulation of the Bcl-2 family proteins. J Surg Oncol. 2007;96:241–248. doi: 10.1002/jso.20827. [DOI] [PubMed] [Google Scholar]
- 39.Walters DK, Muff R, Langsam B, Gruberer P, Born W, Fuchs B. Taurolidine: a novel anti-neoplastic agent induces apoptosis of osterosarcoma cell lines. Invest New Drugs. 2007;25:305–312. doi: 10.1007/s10637-007-9052-9. [DOI] [PubMed] [Google Scholar]
- 40.Marley K, Helfand SC, Edris WA, Mata JE, Gitelman AI, Medlock J, Séguin B. The effects of taurolidine alone and in combination with doxorubicin or carboplatin in canine osteosarcoma in vitro. BMC Veterinary Res. 2013;9:15–24. doi: 10.1186/1746-6148-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chromik AM, Daigeler A, Bulut D, Flier A, May C, Havati K, Roschinsky J, Sülberg D, Ritter PR, Mittelkötter U, Hahn SA, Uhl W. Comparative analysis of cell death induction by Taurolidine in different malignant human cancer cell lines. J Exp Clin Cancer Res. 2010;29:21–37. doi: 10.1186/1756-9966-29-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Daigeler A, Chromik AM, Geisler A, Bulut D, Hilgert C, Krieg A, Klein-Hitpass L, Lehnhardt M, Uhl W, Mittelkötter U. Synergistic apoptotic effects of taurolidine and TRAIL on squamous carcinoma cells of the esophagus. Int J Oncol. 2008;32:1205–1220. doi: 10.3892/ijo_32_6_1205. [DOI] [PubMed] [Google Scholar]
- 43.Daigeler A, Chromik AM, Haendschke K, Emmelmann S, Siepmann M, Hensel K, Schmitz G, Klein-Hitpass L, Steinau HU, Lehnhardt M, Hauser J. Synergistic effects of sonoporation and taurolidin/TRAIL on apoptosis in human fibrosarcoma. Ultrasound Med Biol. 2010;36:1893–1906. doi: 10.1016/j.ultrasmedbio.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 44.Jacobi CA, Menenakos C, Braumann C. Taurolidine - a new drug with anti-tumor and anti-angiogenic effects. Anticancer Drugs. 2005;16:917–921. doi: 10.1097/01.cad.0000176502.40810.b0. [DOI] [PubMed] [Google Scholar]
- 45.Volz J, Volz-Köster S, Kanis S, Klee D, Ahlert C, Melchert F. Modulation of tumor-induced lethality after pneumoperitoneum in a mouse model. Cancer. 2000;89:262–266. [PubMed] [Google Scholar]
- 46.Da Costa ML, Redmond HP, Bouchier-Hayes DJ. Taurolidine improves survival by abrogating the accelerated development and proliferation of solid tumors and development of organ metastases from circulating tumor cells released following surgery. J Surg Res. 2001;101:111–119. doi: 10.1006/jsre.2001.6250. [DOI] [PubMed] [Google Scholar]
- 47.Chromik AM, Daigeler A, Bulut D, Flier A, May C, Harti K, Roschinsky J, Sülberg D, Ritter PR, Mittelkötter U, Hahn SA, Uhl W. Comparative analysis of cell death induction by Taurolidine in different malignant human cancer cell lines. J Exp Clin Res. 2010;29:21–36. doi: 10.1186/1756-9966-29-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen L, Li Y, Yu TS, McKay RM, Burns DK, Kernie SG, Parada LF. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature. 2012;488:522–526. doi: 10.1038/nature11287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trachootham D, Zhou Y, Zhang H, Demizu Y, Chen Z, Pelicano H, Chiao PJ, Acxhanta G, Arlinghaus RB, Liu J, Hunag P. Selective killing of oncogenically trandformed cells through a ROS mediated mechanism by beta-phenylethyl isothiocyanate. Cancer Cell. 2006;10:241–252. doi: 10.1016/j.ccr.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 50.Huang P, Feng L, Oldham EA, Keating MJ, Plunkett W. Superoxide dismutase as a target for killing of cancer cells. Nature. 2000;407:390–395. doi: 10.1038/35030140. [DOI] [PubMed] [Google Scholar]
- 51.Shaw AT, Winslow MM, Magendantz M, Ouyang C, Dowdle J, Subramanian A, Lewis TA, Maglathin RL, Tolliday N, Jacks T. Selective killing of K-ras mutant cancer cells by small molecule inducers of oxidative stress. Proc Natl Acad Sci USA. 2011;108:8773–8778. doi: 10.1073/pnas.1105941108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dolam S, Lessnick SL, Hahn WC, Stockwell BR. Idebtificaton of genotype-selective antitumor agents using syntheticchemical screening in engineered human tumor cells. Cancer Cell. 2003;3:285–296. doi: 10.1016/s1535-6108(03)00050-3. [DOI] [PubMed] [Google Scholar]
- 53.Guzman ML, Rossi RM, Neelakantan S, Li X, Corbett CA, Hassane DC, Becker MW, Bennet JM, et al. An orally bioavailable parthenolide analog selectively eradicates acute myelogenous leukemia stem and progenitor cells. Blood. 2007;110:4427–4435. doi: 10.1182/blood-2007-05-090621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O’Brien G, Cahill R, Bouchier-Hayes D, Redmond P. Co-immunotherapy with interleukin-2 and taurolidine for progressive metastatic melanoma. Irish J Med Sci. 2006;175:10–14. doi: 10.1007/BF03168992. [DOI] [PubMed] [Google Scholar]
- 55.Doddakula KK, Neary PM, Wang JH, Sookhai S, O’Donnel A, et al. The antioxidant agent taurolidine potentially reduces ischemia/reperfusion injury through its metabolite taurine. Surgery. 2010;148:567–572. doi: 10.1016/j.surg.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 56.Braumann C, Guenther N, Pohlenz J, Pfirrmann RW, Menenakos C. Wound healing is not impaired in rats undergoing perioperative treatment with the antineoplastic agent taurolidine. Eur Surg Res. 2009;42:91–96. doi: 10.1159/000182817. [DOI] [PubMed] [Google Scholar]
- 57.Neary PM, Hallihan P, Wang JH, Pfirrmann R, Bouchier-Haves HP, Redmond HP. The evolving role of Taurolidine in cancer therapy. Ann Surg Oncol. 2010;17:1135–1143. doi: 10.1245/s10434-009-0867-9. [DOI] [PubMed] [Google Scholar]
- 58.Liberko M, Kolostova K, Bobek V. Essentials of circulating tumor cells for clinical research and practice. Cirtic Rev Hematol Oncol. 2013;88:338–356. doi: 10.1016/j.critrevonc.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 59.Kilian M, Gregor JI, Heukamp I, Braumann C, Guski H, Schimke I, Walz MK, Jacobi CA, Wenger FA. Impact of taurolidine and octreotide on liver metastasis and lipid peroxidation after laparoscopy in chemical induced ductal pancreatic cancer. Invest New Drugs. 2005;23:157–164. doi: 10.1007/s10637-005-5861-x. [DOI] [PubMed] [Google Scholar]
- 60.Gong L, Greenberg HE, Perhach JL, Waldman SA, Kraft WK. The pharmacokinetics of Taurolidine metabolites in healthy volunteers. J Clin Pharmacol. 2007;47:697–703. doi: 10.1177/0091270007299929. [DOI] [PubMed] [Google Scholar]
- 61.Stendel R, Scheurer L, Schlatterer K, Stalder U, Pfirrmann R, Fiss I, Möhler H, Bigler L. Pharmacokinetics of Taurolidine follwing repeated intravenous infusions measured by HPLC-ESI-MS/MS of the derivatives Taurultame and taurinamide in glioblastoma patients. Clin Pharmacokinetics. 2007;46:513–524. doi: 10.2165/00003088-200746060-00005. [DOI] [PubMed] [Google Scholar]
- 62.Chromik AM, Hahn SA, Daigeler A, Flier A, Bulut D, May C, Harati K, Roschinsky J, Sülberg D, Weyhe D, Mittelkötter U, Uhl W. Gene expression analysis of cell death induction by taurolidine in different malignant cell lines. BMC Cancer. 2010;10:595–608. doi: 10.1186/1471-2407-10-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Daigeler A, Brenzel Ch, Bulut D, Geisler A, Hilgert C, Lehnhardt M, Steinau HU, Flier A, Steinsträsser L, Klein-Hitpass L, Mittelkötter U, Uhl W, Chromik AM. TRAIL and Taurolidine induce apoptosis and decrease proliferation in human fibrosarcoma. J Exp Clin Cancer Res. 2008;27:82–102. doi: 10.1186/1756-9966-27-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rubinsztein DC, Codogno P, Levine B. Autophagy modulation as a potential therapeutic target for divers diseases. Nature Rev Drug Disc. 2012;11:709–730. doi: 10.1038/nrd3802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Möhler T, Willhauck-Fleckenstein M, Schwartz-Albiez R, Merling A, Möhler H. Inhibition of endothelial cell adhesion and in vitro angiogenesis by Taurolidine. Cancer Ther. 2008;6:623–628. [Google Scholar]
- 66.Egan BM, Bouchier-Hayes DJ, Condron C, Kelly CJ, Abdih H. Taurolidine attenuates the hemodynamic and respiratory changes associated with endotoxemia. Scock. 2002;17:308–311. doi: 10.1097/00024382-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 67.Bedrosian I, Sofia RD, Wolff SM, Dinarello CA. Taurolidine, an analogue of the amino acid taurine, suppresses interleukin 1 and tumor necrosis factor synthesis in human peripheral blood mononuclear cells. Cytokine. 1991;3:568–575. doi: 10.1016/1043-4666(91)90483-t. [DOI] [PubMed] [Google Scholar]
- 68.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Reddy PS, Jamil K, Madhusudhan P, Anjani G. Antibacterial activity of isolates of from Piper longum and Taxus baccata. Pharm Biol. 2001;39:236–238. [Google Scholar]
- 70.Adams DJ, Dai M, Pellegrino G, Wagner BK, et al. Synthesis, cellular evaluation and mechanism of action of piperlongumine anlogs. Proc Natl Acad Sci USA. 2012;109:15115–15120. doi: 10.1073/pnas.1212802109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang Y, Wang JW, Xiao X, Shan Y, Xue B, Jiang G, He Q, Chen J, Xu HG, Zhao RX, Werle KD, Cui R, Liang J, Li YL, Xu ZX. Piperlongumine induces autophagy by targeting p38. Cell Death Dis. 2013;4:e824. doi: 10.1038/cddis.2013.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ginzburg S, Golovine KV, Makhov PB, Uzzo RG, Kutikov A, Kolenko VM. Piperlongumine inhibits NFkappaB activity and attenuates aggressive growth characteristics of prostate cancer cells. Prostate. 2013;73:1–10. doi: 10.1002/pros.22739. [DOI] [PMC free article] [PubMed] [Google Scholar]