Abstract
Context:
The Falmouth Road Race is unique because of the environmental conditions and relatively short distance, which allow runners to maintain a high intensity for the duration of the event. Therefore, the occurrence of exertional heat illnesses (EHIs), especially exertional heat stroke (EHS), is 10 times higher than in other races.
Objective:
To summarize the occurrence and relationship of EHI and environmental conditions at the Falmouth Road Race.
Design:
Descriptive epidemiologic study.
Setting:
An 11.3-km (7-mile) road race in Falmouth, Massachusetts.
Patients or Other Participants:
Runners who sustained an EHI while participating in the Falmouth Road Race.
Main Outcome Measure(s):
We obtained 18 years of medical records and environmental conditions from the Falmouth Road Race and documented the incidence of EHI, specifically EHS, as related to ambient temperature (Tamb), relative humidity, and heat index (HI).
Results:
Average Tamb, relative humidity, and HI were 23.3 ± 2.5°C, 70 ± 16%, and 24 ± 3.5°C, respectively. Of the 393 total EHI cases observed, EHS accounted for 274 (70%). An average of 15.2 ± 13.0 EHS cases occurred each year; the incidence was 2.13 ± 1.62 cases per 1000 runners. Regression analysis revealed a relationship between the occurrence of both EHI and EHS and Tamb (R2 = 0.71, P = .001, and R2 = 0.65, P = .001, respectively) and HI (R2 = 0.76, P < .001, and R2 = 0.74, P < .001, respectively). Occurrences of EHS (24.2 ± 15.5 cases versus 9.3 ± 4.3 cases) and EHI (32.3 ± 16.3 versus 13.0 ± 4.9 cases) were higher when Tamb and HI were high compared with when Tamb and HI were low.
Conclusions:
Because of the environmental conditions and race duration, the Falmouth Road Race provides a unique setting for a high incidence of EHS. A clear relationship exists between environmental stress, especially as measured by Tamb and HI, and the occurrence of EHS or other EHI. Proper prevention and treatment strategies should be used during periods of high environmental temperatures as the likelihood of runners experiencing EHS is exacerbated in these harsh conditions.
Key Words: heat stress, thermoregulation
Key Points
The Falmouth Road Race provides a unique setting for the recognition and treatment of exertional heat stroke: the incidence rate during this race is 10 times that of other races.
Environmental measures of ambient temperature and heat index contribute to a significant relationship between environmental stress and the occurrence of exertional heat stroke.
Severe hyperthermia is an inherent risk of endurance exercise. Evidence supports the notion that dangerous levels of hyperthermia can be prevented with the use of self-mediated pacing strategies. An individual's pacing strategy is determined by underlying physiologic regulation based on perceptual feedback and on prior experience.1 In other words, athletes may voluntarily cease exercise when they perceive high heat stress or decrease their intensity to allow them to work for a longer period. A similar model proposes a critical core body temperature (Tcore) that, when reached, is the defining limit at which humans will voluntarily stop exercising.2 However, these internal cues are sometimes ignored during times of competition, which can often result in exertional heat illness (EHI).
The umbrella term of EHI has recently been under scrutiny regarding its terminology and ability to define previously identified heat illnesses.3 Terms such as heat exhaustion and heat cramps have been questioned because of the physiologic causes and lack of distinguishing diagnostic criteria. Regardless of this dispute, exertional heat stroke (EHS) has been uniformly acknowledged as the most serious form of EHI and is characterized by central nervous system (CNS) dysfunction and a Tcore greater than 40°C. Mitigating the rate of increase in Tcore primarily depends on the body's ability to dissipate endogenous heat production, which is a direct result of exercise intensity. Heat dissipation is maximized with high ratios of (1) Tcore to skin temperature and (2) skin temperature to air temperature. The primary heat-dissipation mechanism during exercise is sweating, though heat loss only occurs if that sweat can evaporate off the skin. However, when humidity is high, the ability to dissipate heat in this manner is hindered.4 Humidity becomes especially problematic when an ambient temperature (Tamb) is high because once Tamb rises above skin temperature, cooling by radiation and convection is lost and Tamb now contributes to heat gain as opposed to heat loss.4 Therefore, when metabolic heat production is high and environmental conditions are hot and humid, the thermoregulatory response becomes less effective as it loses the capacity to dissipate heat. As a result, Tcore begins to rise quickly and increases the likelihood of EHS.
Several groups5–13 have examined the influence of environmental conditions on running performance. Some6,8,9,13 have tried to quantify the optimal range of environmental conditions at which running performance can be maximized, but it is generally accepted that running performance progressively decreases as wet-bulb globe temperature (WBGT) increases. However, although some6 have concluded that as temperatures increase, performance slows in a predictable and quantifiable manner, others9 have argued that a linear model based on the WBGT index is not feasible because of the variations in different races. These differences not only include varying environmental conditions due to the geographical location of the race but also individual differences, such as heat acclimatization, hydration status, fitness level, pacing strategy, and sex. In addition, debate continues as to which environmental factors (eg, WBGT, dry-bulb temperature, relative humidity [rH]) are most appropriate to quantify this relationship.11–13
The relationship between environmental conditions and running performance has been extensively studied,5–13 yet few authors10,14,15 have examined the association of environmental conditions and the incidence of EHS. One of the most extensive studies examining this relationship was done by Roberts,15 who evaluated the incidence of EHS over 12 years of the Twin Cities Marathon. Exercise-associated collapse resulting from hyperthermia occurred in 3 per 10 000 entrants (EHS accounted for 1–2 per 10 000 finishers). Furthermore, heat and humidity contributed to 72% of the risk for moderate to severe exercise-associated collapse in this running population.15 In a separate study, Roberts10 showed that the number of participants who “successfully complete” a marathon decreases as the heat stress increases. In contrast to the relatively low overall incidence of EHS (1–2 cases per 10 000 entrants) during the Twin Cities Marathon, 1–2 EHS cases per 1000 entrants have been reported at the Falmouth Road Race, accounting for 40% of the total patients seen in the medical tent.14 This 10-fold increase in the incidence of EHS indicates that other factors contribute to the likelihood of acquiring EHS during competitive running.
Although extreme environmental conditions decrease performance and increase the risk of acquiring EHS, it is important to consider other factors that can exaggerate the risk of EHI. We describe 18 years of EHI and EHS cases during the Falmouth Road Race, which takes place every year in the middle of August. In addition to this large data set for EHI and EHS cases, our study is unique in that the Falmouth Road Race produces some of the highest occurrences of EHS compared with other races, averaging 10–12 cases per year. The purposes of this study were to (1) observe the incidence rates of EHI and EHS at the Falmouth Road Race, (2) examine the relationship between environmental conditions and EHI or EHS during the Falmouth Road Race, and (3) examine the effect of environmental conditions on the occurrence of EHI and EHS. Our hypotheses were that (1) the incidence of EHS at the Falmouth Road Race would be high because this short-duration race is run in the middle of the summer; (2) cases of EHI and EHS would be highly correlated with environmental conditions, especially Tamb and HI; and (3) the occurrence of EHI and EHS would be higher in those years with higher environmental conditions (Tamb, heat index [HI], rH).
METHODS
Study Design
We studied environmental factors and cases of EHI and EHS at the Falmouth Road Race. This race is a 7-mi (11.26-km) point-to-point race held annually on the second Sunday of August in Falmouth, Massachusetts (41° 52′ N, 70° 67′ W). The average weather conditions, according to METAR reports from the Cape Cod Coast Guard Air Station, for the race days studied were an Tamb of 23°C, an rH of 70%, and a National Weather Service HI of 24°C. The race begins at 10:00 am, and there are approximately 10 000 runners ranging from elite to novice status.
Race-Participant Data
Medical tent records from the EHI treatment areas were obtained for the following years: 1984, 1989, 1992–1994, 1996–1998, 2001, and 2003–2011 (18 years total). After triage, patients presenting with signs and symptoms of EHI were directed to the EHI treatment area, where rectal temperature was assessed using rectal thermometry. We acknowledge the ongoing debate regarding proper EHI terminology, as mentioned previously, but for the purpose of this study, we chose to include the following conditions in our classification of EHI: EHS and any episode of exercise-associated collapse near, at, or beyond the finish line that resulted in syncope or collapse because of orthostatic hypotension, presentation of CNS dysfunction, or both. Exertional heat stroke was diagnosed when a rectal temperature ≥40°C was associated with signs of CNS dysfunction (ie, the runner had altered mental status, was unconscious, was unable to lucidly answer questions). Incidence is calculated as cases per 1000 finishers for the years after 1996 (12 years in total), as finisher information was not available for the 6 years before 1996 (Table 1). Permission to use medical record data was given by the university's institutional review board.
Table 1.
Finisher Data and Exertional Heat Illness and Exertional Heat Stroke Incidence Rates for the Falmouth Road Race
| Year |
Finishers, No. |
Exertional Heat Illness IncidenceRate |
Exertional Heat Stroke IncidenceRate |
| 1997 | 7752 | 2.71 | 2.19 |
| 1998 | 7219 | 2.22 | 1.11 |
| 2001 | 7774 | 2.32 | 0.77 |
| 2003 | 8058 | 7.57 | 6.58 |
| 2004 | 8171 | 1.59 | 1.10 |
| 2005 | 7532 | 4.38 | 3.19 |
| 2006 | 8242 | 1.94 | 0.97 |
| 2007 | 8926 | 4.37 | 2.91 |
| 2008 | 8743 | 3.32 | 2.63 |
| 2009 | 8864 | 1.92 | 1.58 |
| 2010 | 9653 | 1.55 | 1.14 |
| 2011 | 10930 | 1.74 | 1.37 |
| Mean ± SD | 8489 ± 1029 | 2.97 ± 1.76 | 2.13 ± 1.62 |
Weather Data
Weather data were obtained from METAR records for the Cape Cod Coast Guard Air Station. Daily averages for Tamb, rH, and HI during the time of the race (between 10:00 am and 12:00 pm) on the race days studied were used for regression analysis and are presented in Table 2. Additionally, to test the hypothesis that EHI and EHS occurrence would be higher when environmental conditions were higher, data for each environmental factor (Tamb, rH, and HI) were divided into thirds, and a group comparison was performed for the highest and lowest thirds for each variable. The HI calculations were performed using the National Weather Service's HI model.16
Table 2.
Falmouth Road Race Environmental Conditions
| Year |
Ambient Temperature, °C |
Relative Humidity, % |
Heat Index, °C |
| 1984 | 22.2 | 55 | 22 |
| 1989 | 23.9 | 79 | 24 |
| 1992 | 17.2 | 92 | 17 |
| 1993 | 19.6 | 61 | 19 |
| 1994 | 24.2 | 82 | 25 |
| 1996 | 24.0 | 75 | 24 |
| 1997 | 26.7 | 70 | 28 |
| 1998 | 24.5 | 69 | 25 |
| 2001 | 23.3 | 98 | 25 |
| 2003 | 27.7 | 87 | 33 |
| 2004 | 22.0 | 57 | 22 |
| 2005 | 26.0 | 87 | 28 |
| 2006 | 21.3 | 47 | 21 |
| 2007 | 25.3 | 57 | 26 |
| 2008 | 23.7 | 65 | 24 |
| 2009 | 22.3 | 49 | 22 |
| 2010 | 22.7 | 53 | 22 |
| 2011 | 23.0 | 78 | 23 |
| Mean ± SD | 23.3 ± 2.5 | 70 ± 16 | 24 ± 3.5 |
Statistical Analysis
Descriptive statistics are presented as mean ± SD. We calculated regression analyses to determine goodness of fit and the Shapiro-Wilk test of normality to ensure that conditions of the statistical test were met. Additionally, independent-samples t tests were used to determine group differences between the highest third and lowest third of each independent variable. Significance was set a priori at an α level of P < .05. Statistical analyses were performed using PASW Statistics (version 18.0 for Mac; SPSS Inc, Chicago, IL).
RESULTS
Incidence
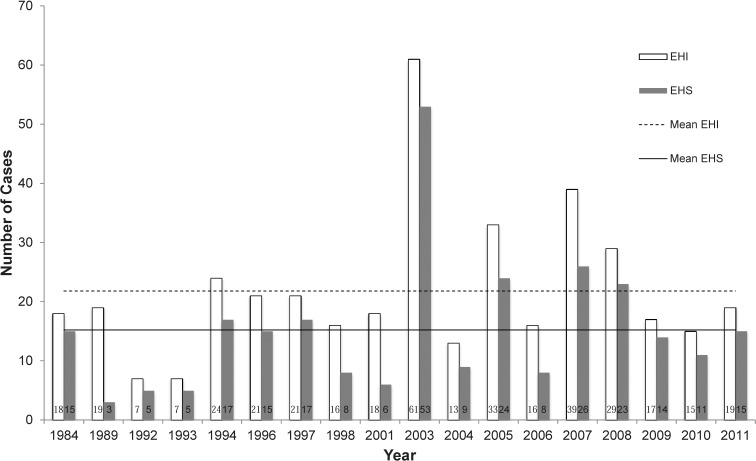
A total of 393 EHI cases were studied, and EHS accounted for 274 (70%) of these. The total number of EHIs per year is presented in Figure 1. In the years studied, an average of 15.2 ± 13.0 EHS cases occurred per year. An overall incidence of 2.13 ± 1.62 EHS cases per 1000 runners was calculated. The year with the most cases was 2003, when 61 EHIs were observed, including 53 cases of EHS. In both 1992 and 1993, only 7 EHI cases were recorded, including 5 cases of EHS per year.
Figure 1.
Number of cases of exertional heat illness (EHI; white bars) and exertional heat stroke (EHS; gray bars) for 18 years of the Falmouth Road Race.
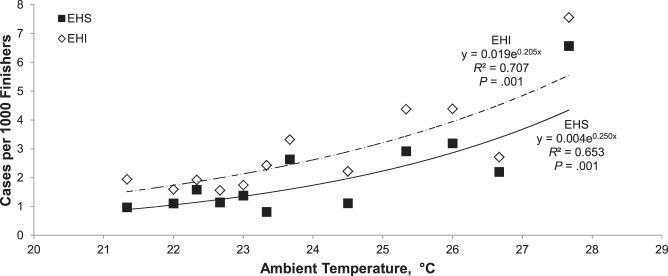
Ambient Temperature
Daily average Tamb was 23.3 ± 2.5°C (range, 17.2°C–27.7°C). Plots of the incidences of EHI and EHS against Tamb are shown in Figure 2. Analyses revealed a significant relationship between an increased Tamb and incidence of both EHI and EHS (each P = .001). When comparing those years with the highest Tamb versus those with the lowest Tamb (25.7 ± 1.3°C versus 20.8 ± 2.0°C, respectively), we found the total number of cases was higher in hot conditions than in cool conditions for both EHI (32.3 ± 16.3 cases versus 13.0 ± 4.9 cases, P = .02) and EHS (24.2 ± 15.5 cases versus 9.3 ± 4.3 cases, P = .04).
Figure 2.
Relationship of the incidence rate (per 1000 finishers) of exertional heat illness (EHI; white diamonds, dashed line) and exertional heat stroke (EHS; black squares, solid line) versus ambient temperature during the Falmouth Road Race.
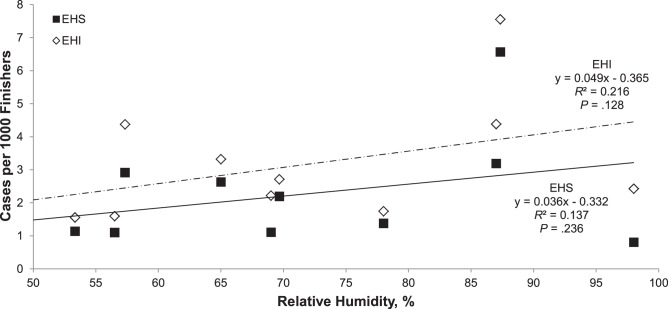
Relative Humidity
Daily average rH was 70% ± 16% (range, 47%–98%). Plots of the incidences of EHI and EHS against rH are shown in Figure 3. No significant interaction was demonstrated by regression analysis (P = .236, P = .128). When we compared those years with the highest rH versus those with the lowest rH (87.5% ± 6.8% versus 53.7% ± 5.2%, respectively), the total number of cases was similar (P > .05) for both EHI (27.0 ± 18.7 cases versus 19.7 ± 9.6 cases) and EHS (18.0 ± 19.0 cases versus 13.8 ± 6.6 cases).
Figure 3.
Relationship of the incidence rate (per 1000 finishers) of exertional heat illness (EHI; white diamonds, dashed line) and exertional heat stroke (EHS; black squares, solid line) versus relative humidity during the Falmouth Road Race.
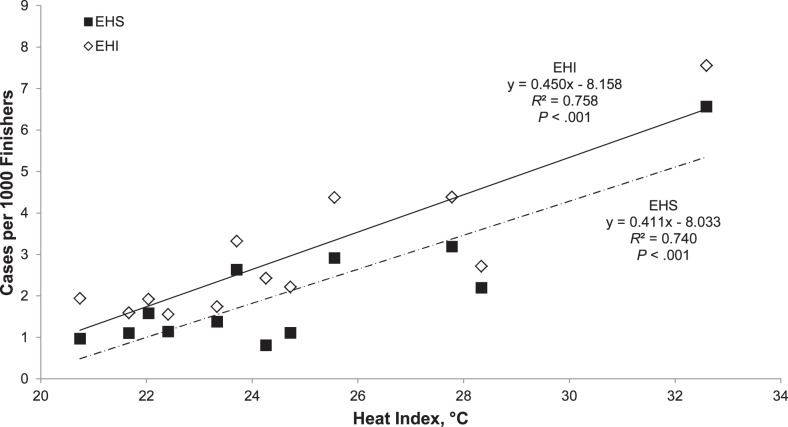
Heat Index
Daily average HI was 24°C ± 3.5°C (range, 17°C–33°C). Plots of the incidences of EHI and EHS against HI are shown in Figure 4. Positive relationships were noted between HI and the incidences of both EHI and EHS (each P < .001). When comparing those years with the highest HI versus those with the lowest HI (27.5°C ± 3.0°C versus 20.7°C ± 2.2°C, respectively), the total number of cases was higher in hot conditions than in cool conditions for both EHI (32.3 ± 16.3 cases versus 13.0 ± 4.9 cases, P = .02) and EHS (24.2 ± 15.5 cases versus 9.3 ± 4.3 cases, P = .04).
Figure 4.
Relationship of the incidence rate (per 1000 finishers) of exertional heat illness (EHI; white diamonds, dashed line) and exertional heat stroke (EHS; black squares, solid line) versus heat index during the Falmouth Road Race.
DISCUSSION
The purposes of this study were to (1) observe the incidence rates of EHI and EHS at the Falmouth Road Race, (2) assess the relationship between environmental conditions and the incidences of EHI and EHS from 18 years of data at the Falmouth Road Race, and (3) examine the effect of environmental conditions on the occurrences of EHI and EHS. Although we emphasize environmental conditions as a primary predisposing factor to acquiring EHS, we also address the potential influence from other factors (eg, exercise intensity, exercise duration, heat acclimatization). One key finding was that the incidence rate of EHS during the studied 18-year span of the Falmouth Road Race was considerably high. Previous authors reported an average incidence of approximately 1–2 cases of EHS per 10 000 runners10,15; such is the case with a 12-year profile of injury and illness from the Twin Cities Marathon.15 The average Tamb at the start of this race was 5°C (range, −4°C to 16°C), and the average Tamb at the 4-hour mark of this race was 13°C (range, 5°C to 20°C).15 Additionally, the average rH at the start of the race was 84%, but it dropped to an average of 57% at the 4-hour mark.15 These environmental conditions were mild compared with those in the current study, but it is reasonable to assume they played a primary role in the relatively low incidence rate of EHS. However, the contribution of Tamb to EHS was similar to that found by Roberts15 (approximately 70%; Figure 2). Therefore, it is likely that another factor led to the higher incidence of EHS at the Falmouth Road Race.
In addition to the higher temperatures present in the current study, another hallmark difference is the shorter distance of the race compared with that of the marathon (7 miles versus 26.2 miles). This shorter distance allowed the runners to maintain a high exercise intensity, thereby likely driving a greater increase in Tcore given the higher metabolic heat production.17,18
Although it seems clear that environmental conditions, especially as measured by Tamb and HI, play an integral role in the incidence of EHS, it is important to note that EHS can also occur in conditions that are generally considered safe for running. This was reported by Roberts,19 who described a case study of an EHS suffered in mild environmental conditions (WBGT = 7.9°C at the time of collapse). Given that the mild environmental conditions would have maximized the ability for heat dissipation and that common predisposing factors were ruled out, it is clear that another factor was the primary culprit in this runner's EHS. The author concluded that the primary factor leading to EHS was the runner's pacer for the last 16 km of the race.19 As a result, the runner likely ignored his internal cues of a dangerous level of hyperthermia and ran at a higher intensity than if the pacer had not been present. Roberts highlighted the importance of intensity level during exercise and agreed with previous reports20–22 that exercise intensity is the greatest influence on the rate of rise of Tcore.
Because the Falmouth Road Race consists of a significantly shorter race distance than a marathon, some may argue that the EHS incidence rate would be higher during the longer-distance event. However, this is likely not the case, primarily because of the difference in exercise intensity endured by runners in the 2 events. For example, a runner is able to maintain a higher intensity for a 7-mi (11-km) run compared with a 26-mi (42-km) run. Thus, the runner will have much higher metabolic heat production during a 7-mile race than during a marathon. Given the retrospective nature of this study, we could not examine exercise intensity, so we could not use it in the regression analysis to identify its true contribution to the development of EHS. However, the speculative high intensity level, coupled with the harsh environmental conditions that are often present during the middle of August, likely provide a unique and favorable setting for developing EHS.
As previously reported5 and examined20–22 in the literature, the rate of metabolic heat production is a function of running speed. In addition, the high Tcore achieved by athletes in shorter-distance races has been used to defend the notion that metabolic rate is most predictive of a rise in Tcore during exercise.5 To showcase this, Noakes et al20 examined the influence of several variables to determine the primary factor predicting postrace Tcore in marathon runners. Their results showed that, in fact, metabolic rate was the principal determinant of postrace Tcore.20 Furthermore, this correlation was heightened during the pace maintained in the last half of the race, which parallels the case study19 described earlier showing the influence of a pacer in the last 16 km of the marathon.
As previously stated, limited research10,14,15 exists regarding the direct relationship between environmental conditions and the incidence of EHI or EHS. Therefore, we sought to examine if the occurrences of EHI and EHS would change with varying environmental conditions. In the years with the highest Tamb and HI, there were significantly more cases of EHS and EHI compared with those years when Tamb and HI were low. However, this finding did not hold for the relationship between EHI or EHS and rH. In other words, cases of EHI and EHS were not different in years when rH was high compared with years when rH was low.
Roberts10 reported that when the WBGT at the start of a marathon was >13°C, the number and rate of finish-line medical encounters and on-course marathon dropouts began to rise. More specifically, when WBGT was <13°C, EHS cases averaged 0–1 per race but rose to 11–12 cases per race when the WBGT was >22°C. Similarly, we observed that in 8 of the 11 years (73%) when the HI >22°C, the number of EHS cases was also at or above the 18-year average (Table 2 and Figure 1). Although the HI does not account for solar radiation as does WBGT, these values were similar to our regression analysis findings that HI significantly explained the variability in EHS incidence (R2 = 0.74, P < .001; Figure 4).
Predictions of running performance and HI followed a similar trend.6,11–13 This relationship has primarily been studied in the marathon population, in whom marathon performance decreased as HI increased. For example, a moderate correlation (r = .739) was shown between WBGT and finishing times at the Boston marathon.11 Additionally, Ely et al7 demonstrated a progressive lowering of marathon performance as WBGT increased from 5°C to 25°C. These results agree with our findings that HI was a valid predictor of environmental stress, as has been previously described (see Figure 4).
Although reports of the relationship between environmental conditions and EHS are limited, numerous authors5–13 have examined the relationship between environmental conditions and running performance. The overwhelming majority concluded that performance (as measured by race time) decreases as environmental conditions become more extreme. Furthermore, these researchers attempted to distinguish this relationship based on specific environmental factors, such as Tamb,8,12–13 rH,11–13 and HI.6,11–13 When considering Tamb as a predictor, Frederick,8 Zhang et al,13 and Vihma12 all found decreases in marathon performance as Tamb increased. More specifically, Frederick8 reported that for every 5°C that Tamb was above 12°C, marathon time slowed by 3 minutes. Interestingly, this threshold of 12°C was similar to that reported by Roberts,10 who noted that the marathon dropout rate rose significantly when temperatures were >13°C. Unfortunately, we could not further explore a possible link of this temperature with our data because Tamb was above 13°C every year the data were analyzed. However, our results did support the notion that Tamb is a good measure of environmental heat stress for EHS (R2 = 0.65, P = .001; Figure 2) and EHI (R2 = 0.71, P = .001; Figure 3). Of the 10 years that Tamb was higher than the 18-year average, 7 of those years also resulted in an above-average incidence of EHS (Table 2 and Figure 1). Interestingly, the 3 years (1989, 1998, and 2001) that failed to show this association were the same 3 years in which the HI and occurrence of EHS were not associated, as described earlier. Therefore, other factors may have contributed to the lower incidence of EHS in those years that could not be explained by Tamb or HI.
We found Tamb and HI to be good predictors of EHS and EHI, and these factors are generally considered to be valid indicators of environmental stress, but various reports11–13 have indicated that rH is not an appropriate environmental marker for explaining extremes in running performance. In 1 study,13 although marathon finishing times were similarly correlated with Tamb and WBGT, rH was an appropriate predictor only when Tamb was >28°C. In other words, these runners were able to maintain their pace and tolerate the thermoregulatory strain of rH when Tamb remained within a given range; however, when Tamb rose to extreme levels, rH became a significant contributor that might have overwhelmed the thermoregulatory system, potentially leading to EHS if the runner had not slowed the pace (as indicated by a decrease in performance). This relationship portrays the contributions of different heat-loss mechanisms and their roles when varying degrees of Tamb are present. When Tamb is low, convective heat loss is the primary heat-loss mechanism; however, when Tamb rises, evaporation becomes the dominant heat-loss mechanism, especially when Tamb rises above skin temperature.17,18 In this scenario, evaporative heat loss is both important and essential; otherwise, the body loses all heat- dissipation mechanisms and has no defense against a certain and rapid rise in Tcore.
We did not measure Tcore (only performance), so we cannot directly link thermoregulatory efficiency and rH. Given this, and acknowledging that the importance of the contribution of evaporative heat loss during high Tamb is well established, the reported decrease in performance13 suggests that the harsh environmental conditions likely drove up Tcore to a point at which the runners willingly chose to decrease their pace, thus decreasing their metabolic heat production and preventing a critically high Tcore. This rationale further supports the previously discussed theories of a self-mediated strategy in which pace is determined by underlying physiologic regulation based on perceptual feedback1 and a critical Tcore.2
Our results further verify this claim. The rH was not a predictor of EHI (R2 = 0.216, P = .128; Figure 3) or EHS (R2 = 0.137, P = .236; Figure 4) and was the only environmental indicator examined that failed to show this relationship. In support, in 2001, when the rH was the highest among all years studied (98% rH), only 6 cases of EHS were reported, well below the 18-year average (Table 2 and Figure 1). Interestingly, in 2003, when the highest number of cases of EHI (61 cases) and EHS (53 cases) were reported, the rH was also well above the 18-year average (Table 2). Furthermore, the Tamb that year was 27.7°C, approaching that found by Zhang et al13 (28°C) at which rH began to significantly affect marathon performance. In further support of this theory, the 1992 data set from our study showed a similar rH to that of 2003; however, Tamb was considerably lower (Table 2), resulting in only 5 EHS cases compared with the astonishing 53 cases (accounting for 87% of EHI) in 2003 (Figure 1). Not surprisingly, in 2003, both Tamb and HI were the highest values among the 18 years studied (27.7°C and 33°C, respectively), providing a probable explanation for the 53 EHS cases observed. This cohort of data offers further evidence to suggest that rH is not a strong predictor of EHS.
This study had inherent limitations with regard to the study design and associated results. As this was a retrospective study design evaluating many years of data from the Falmouth Road Race, it was not possible for us to gather demographic information from individual participants. For example, we did not know if the participants possessed other common predisposing factors of EHI and EHS, such as fitness status, heat-acclimatization status, hydration status, and so on. Therefore, it is possible that the regression analyses of these factors may have altered the contribution of environmental factors to the incidences of EHI and EHS.
CONCLUSIONS
Our findings highlight the uniqueness of the Falmouth Road Race, during which a substantial number of EHS cases are seen each year. This is likely due in large part to the often extreme environmental temperatures that are present when the race is run and to the short duration of the race, promoting higher intensities by runners. In addition, our results showed a clear relationship between the incidence of EHI and EHS and the amount of environmental stress present, especially as measured by Tamb and HI. We recommend that proper precautions and treatment strategies be put in place during athletic events regardless of the environmental condition, as EHS can occur in any environment. Additionally, we recommend that these strategies be amplified during periods of high environmental temperatures, as the likelihood of runners acquiring EHS increases in these harsh conditions.
REFERENCES
- 1.Tucker R, Noakes TD. The physiological regulation of pacing strategy during exercise: a critical review. Br J Sports Med. 2009;43(6):e1. doi: 10.1136/bjsm.2009.057562. [DOI] [PubMed] [Google Scholar]
- 2.Marino FE. Anticipatory regulation and avoidance of catastrophe during exercise-induced hyperthermia. Comp Biochem Physiol B Biochem Mol Biol. 2004;139(4):561–569. doi: 10.1016/j.cbpc.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Noakes TD. A modern classification of the exercise-related heat illnesses. J Sci Med Sport. 2008;11(1):33–39. doi: 10.1016/j.jsams.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Stearns RL, O'Connor FG, Casa DJ, Kenny GP. Exertional heat stroke. In: Casa DJ, editor. Preventing Sudden Death in Sport and Physical Activity. Sudbury, MA: Jones & Bartlett Learning; 2012. pp. 53–77. In. ed. [Google Scholar]
- 5.Cheuvront SN, Haymes EM. Thermoregulation and marathon running: biological and environmental influences. Sports Med. 2001;31(10):743–762. doi: 10.2165/00007256-200131100-00004. [DOI] [PubMed] [Google Scholar]
- 6.Ely MR, Cheuvront SN, Roberts WO, Montain SJ. Impact of weather on marathon-running performance. Med Sci Sports Exerc. 2007;39(3):487–493. doi: 10.1249/mss.0b013e31802d3aba. [DOI] [PubMed] [Google Scholar]
- 7.Ely MR, Martin DE, Cheuvront SN, Montain SJ. Effect of ambient temperature on marathon pacing is dependent on runner ability. Med Sci Sports Exerc. 2008;40(9):1675–1680. doi: 10.1249/MSS.0b013e3181788da9. [DOI] [PubMed] [Google Scholar]
- 8.Frederick EC. Hot times. Running. 1983;9:51–53. [Google Scholar]
- 9.McCann DJ, Adams WC. Wet bulb globe temperature index and performance in competitive distance runners. Med Sci Sports Exerc. 1997;29(7):955–961. doi: 10.1097/00005768-199707000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Roberts WO. Determining a “do not start” temperature for a marathon on the basis of adverse outcomes. Med Sci Sports Exerc. 2010;42(2):226–232. doi: 10.1249/MSS.0b013e3181b1cdcf. [DOI] [PubMed] [Google Scholar]
- 11.Trapasso LM, Cooper JD. Record performances at the Boston Marathon: biometeorological factors. Int J Biometeorol. 1989;33(4):233–237. doi: 10.1007/BF01051083. [DOI] [PubMed] [Google Scholar]
- 12.Vihma T. Effects of weather on the performance of marathon runners. Int J Biometeorol. 2010;54(3):297–306. doi: 10.1007/s00484-009-0280-x. [DOI] [PubMed] [Google Scholar]
- 13.Zhang S, Meng G, Wang Y, Li J. Study of the relationships between weather conditions and the marathon race, and of meteorotropic effects on distance runners. Int J Biometeorol. 1992;36(2):63–68. doi: 10.1007/BF01208915. [DOI] [PubMed] [Google Scholar]
- 14.Brodeur VB, Dennett SR, Griffin LS. Exertional hyperthermia, ice baths, and emergency care at the Falmouth Road Race. J Emerg Nurs. 1989;15(4):304–312. [PubMed] [Google Scholar]
- 15.Roberts WO. A 12-yr profile of medical injury and illness for the Twin Cities Marathon. Med Sci Sports Exerc. 2000;32(9):1549–1555. doi: 10.1097/00005768-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Steadman RG. The assessment of sultriness, part I: a temperature-humidity index based on human physiology and clothing science. J Appl Meteorol. 1979;18(7):861–873. [Google Scholar]
- 17.Armstrong LE. Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003. pp. 17–28. [Google Scholar]
- 18.Kenefick RW, Cheuvront SN, Sawka MN. Thermoregulatory function during the marathon. Sports Med. 2007;37((4–5)):312–315. doi: 10.2165/00007256-200737040-00010. [DOI] [PubMed] [Google Scholar]
- 19.Roberts WO. Exertional heat stroke during a cool weather marathon: a case study. Med Sci Sports Exerc. 2006;38(7):1197–1203. doi: 10.1249/01.mss.0000227302.80783.0f. [DOI] [PubMed] [Google Scholar]
- 20.Noakes TD, Myburgh KH, du Plessis J, et al. Metabolic rate, not percent dehydration, predicts rectal temperature in marathon runners. Med Sci Sports Exerc. 1991;23(4):443–449. [PubMed] [Google Scholar]
- 21.Rav-Acha M, Hadad E, Epstein Y, Heled Y, Moran DS. Fatal exertional heat stroke: a case series. Am J Med Sci. 2004;328(2):84–87. doi: 10.1097/00000441-200408000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Saltin B, Hermansen L. Esophageal, rectal, and muscle temperature during exercise. J Appl Physiol. 1966;21(6):1757–1762. doi: 10.1152/jappl.1966.21.6.1757. [DOI] [PubMed] [Google Scholar]