Abstract
Increasing numbers of women veterans using Department of Veterans Affairs (VA) services has contributed to the need for equitable, high-quality care for women. The VA has evaluated performance measure data by gender since 2006. In 2008, the VA launched a 5-year women’s health redesign, and, in 2011, gender disparity improvement was included on leadership performance plans. We examined data from VA Office of Analytics and Business Intelligence quarterly gender reports for trends in gender disparities in gender-neutral performance measures from 2008 to 2013. Through reporting of data by gender, leadership involvement, electronic reminders, and population management dashboards, VA has seen a decreasing trend in gender inequities on most Health Effectiveness Data and Information Set performance measures.
Since 2000, the number of women veterans using Department of Veterans Affairs (VA) services has doubled.1 With the unprecedented increase in women seeking care in a health care system previously dedicated to men, it is imperative for VA to provide equitable, high-quality care to women veterans.
In 2006, VA began analyzing performance measure data by gender. Although VA outperforms the private sector in many quality measures for men and women, within the VA, significant gender disparities were initially noted.
In 2008, the VA’s Women’s Health Services launched a 5-year women’s health care redesign plan to ensure that women veterans receive comprehensive primary care from skilled providers, performance measures are reported by gender to VA leadership, and feedback is given to providers. In 2011, gender disparity improvement was included as a performance measure in the Healthcare Leadership Annual Performance Plan.
Provision of equitable, high-quality care to women includes both gender-specific and gender-neutral care. We examined trends in disparities in a subset of gender-neutral VA performance measures from 2008 to 2013 after implementation of a strategic plan focusing on VA women’s health care and increased leadership attention to gender disparities in performance measures.
METHODS
We examined data from VA Office of Analytics and Business Intelligence quarterly gender reports for trends in gender disparities in gender-neutral performance measures from 2008 to 2013.2 Information included in these reports are gathered by the VA’s External Peer Review Program, a database used for analysis and internal and external comparison of clinical care. The External Peer Review Program data are obtained from a random monthly sampling of medical records of veterans in VA care. The denominator for each clinical measure varies considerably because of the number of veterans eligible for each measure out of the sample pulled (dominator range: 1820 to 107 659). For each clinical measure, the percentage of veterans that satisfied this measure and denominators for veterans that qualified for the measure were reported. On the basis of previous methodology, we viewed differences of plus or minus 5 points as clinically significant.3
The VA Office of Analytics and Business Intelligence tracked 23 gender-neutral clinical measures as either part of the Health Effectiveness Data and Information Set or, in the case of behavioral health, part of established VA–Department of Defense clinical practice guidelines. These included measures of screening rates for mental health and substance abuse and quality of chronic disease management such as hypertension, and low-density lipoprotein (LDL) cholesterol levels in veterans with diabetes or ischemic heart disease. We focused on these measures: depression screening, posttraumatic stress disorder (PTSD) screening, LDL less than 100 milligrams per deciliter in veterans with diabetes, and LDL less than 100 milligrams per deciliter in veterans with ischemic heart disease. We analyzed national data from 2008 to 2013 for trends in gender disparities on these specified measures.
RESULTS
In 2008, 81% of women (n = 12 516) and 87% of men (n = 30 644) were screened for depression with the Patient Health Questionnaire (PHQ)-2 or PHQ-9 screen; a gap of 6% was noted. By 2009, rates of depression screening improved for both women (91.5%; n = 16 619) and men (95.4%; n = 41 176) but a 4-point gap still existed (Figure 1). By 2011, no difference was seen in depression screening rates. Likewise, in 2008, the percentage of women screened for PTSD at required intervals was lower than the percentage of men that received the same screening (women 78.7%; n = 8604; men 84.5%; n = 15 735). These gaps in PTSD screening were virtually eliminated in 2011 through 2013 (2013: women 97.9%; n = 28 057; men 98.5%; n = 107 659; Figure 1).
FIGURE 1—
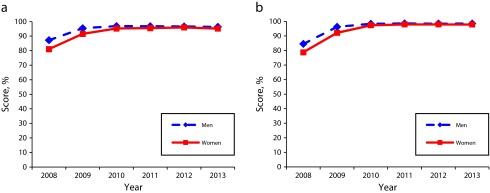
Gender differences among veterans in behavioral health screenings for (a) depression and (b) posttraumatic stress disorder: US Department of Veterans Affairs, 2008–2013.
Although notable reductions in gender disparity have occurred for other cardiovascular risk factors such as hypertension and diabetes control, the largest and most persistent gender disparities were in cholesterol management for veterans with diabetes and ischemic heart disease. In 2008, of veterans with ischemic heart disease, 48% of women (n = 842) and 66% of men (n = 18 711) had an LDL less than 100 milligrams per deciliter; for veterans with diabetes, 52% of women (n = 5977) and 68% of men (n = 31 827) had an LDL less than 100 milligrams per deciliter. In 2011, 55% of women (n = 1820) and 71.5% of men (n = 41 055) with ischemic heart disease had an LDL less than 100 milligrams per deciliter, and 55% of women (n = 4651) and 69% of men (n = 59 860) with diabetes had an LDL less than 100 milligrams per deciliter. In 2012, the LDL-less-than-100 milligrams per deciliter measure was changed so the measure could also be met by being on a moderate-dose statin. This change resulted in an increase of both women and men meeting the measure and a slight narrowing of the gender gap but overall a disparity of more than 5 points still existed in 2013 in patients with ischemic heart disease (women 79.47%; n = 1538; men 88.89%; n = 34 975) and diabetes (women 79.34%; n = 3974; men 85.67%; n = 45 952; Figure 2).
FIGURE 2—
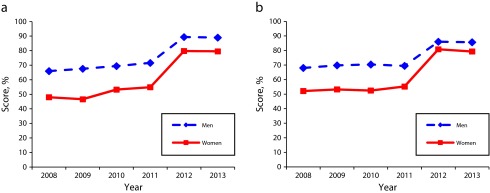
Gender differences in low-density lipoprotein < 100 mg/dL among veterans with (a) ischemic heart disease and (b) diabetes: US Department of Veterans Affairs, 2008–2013.
Note. Measure included use of moderate-dose statin in 2012–2013.
DISCUSSION
Since 2008, the VA has seen a decreasing trend in gender inequities on most Health Effectiveness Data and Information Set performance measures, with near elimination of the disparity for depression and PTSD screening. Gender inequities are still notable for LDL less than 100 milligrams per deciliter or use of a moderate-dose statin in female veterans with diagnosis of ischemic heart disease or diabetes.
The VA’s data reporting by gender, leadership involvement, electronic reminders, and population management dashboards have likely had an impact on improving gender inequities by drawing attention to the gender disparities in clinical performance. However, continued attention to provision of equitable, high-quality health care to women veterans remains crucial.
Human Participant Protection
The data reported here were collected as part of normal operational procedures and were therefore exempt from institutional review board review.
References
- 1.Frayne SM, Phibbs CS, Friedman SA . Sourcebook: Women Veterans in the Veterans Health Administration. Sociodemographics and Use of VHA and Non-VA Care (Fee) Vol 2. Washington, DC: Department of Veterans Affairs; 2012. [Google Scholar]
- 2.Performance measurement gender report. Washington, DC: Department of Veterans Affairs; 2013. VA Office of Analytics and Business Intelligence. [Google Scholar]
- 3.Wright SM, Schaefer J, Reyes-Harvey E, Francis J. Washington, DC: Department of Veterans Affairs; 2012. Comparing the care of men and women veterans in the Department of Veterans Affairs, VA Office of Analytics and Business Intelligence. [Google Scholar]


