Abstract
Objectives. We assessed HCV screening and prevalence among veterans and estimated the potential impact of complete birth cohort screening, accounting for the disparate HCV disease burden by race/ethnicity and gender.
Methods. We used the Department of Veterans Affairs (VA) Corporate Data Warehouse to identify birth dates, gender, race/ethnicity, and laboratory tests for veterans with at least 1 VA outpatient visit in 2012. We calculated HCV screening rates, prevalence, and HCV infection incident diagnosis.
Results. Among 5 499 743 veterans, 54.7% had HCV screening through the VA. In more than 2.9 million veterans screened, HCV prevalence was 6.1% overall and highest among Blacks (11.8%), particularly Black men born in 1945 to 1965 (17.7%). HCV infection incident diagnosis in 2012 was 5.9% for men and 2.3% for women. An estimated additional 48 928 male veterans, including 12 291 Black men, and 1484 female veterans would potentially be identified as HCV infected with full birth cohort screening.
Conclusions. HCV prevalence was markedly elevated among veterans born in 1945 to 1965, with substantial variation by race/ethnicity and gender. Full adoption of birth cohort screening may reveal substantial numbers of veterans with previously unknown HCV infection.
In the United States, it is estimated that 2.7 to 3.9 million persons are living with HCV infection, of whom 45% to 85% are unaware they are infected.1–4 Many have no symptoms until they develop severe liver damage and HCV-related complications, resulting in more than 15 000 deaths per year.5,6 To prevent transmission and to reduce the risk of disease progression in the millions of Americans who are infected but undiagnosed, more thorough screening for HCV infection is critical.
Recognizing this as a public health priority, the Centers for Disease Control and Prevention and the US Preventive Services Task Force now recommend one-time HCV screening, without prior ascertainment of HCV risk, for all persons born 1945 to 1965 in addition to continued risk-based screening.1 This recommendation efficiently targets screening to address the disproportionately high HCV prevalence in this birth cohort population.2,7 Although it is expected that birth cohort screening may identify 808 580 US persons with previously undiagnosed HCV infection, the recommendation for birth cohort screening and the resultant estimate for case finding is for all persons in the United States and does not take into account the disparate HCV disease burden by race/ethnicity or gender.8
Blacks, and to a lesser extent Hispanics, disproportionately bear a large burden of HCV infection in the United States, yet the role and importance of race/ethnicity has not been well characterized among the population of viral hepatitis–infected individuals and deserves special attention.9,10 Analyses of nationally representative National Health and Nutrition Examination Survey data from 2 separate evaluation periods have identified Blacks as having the highest prevalence of antibody to HCV (anti-HCV) at 3.0% among Blacks compared with 1.6% in the general population and compared with an even higher anti-HCV prevalence of 13.6% among Black men born between 1945 and 1965.2,7
Veterans have also been reported to have a higher prevalence of anti-HCV than does the general population.11 Previously, anti-HCV prevalence among veterans seen at Department of Veterans Affairs (VA) medical facilities was estimated from a cluster sample of VA users at 5.4% compared with the 1.5% estimated anti-HCV prevalence for the general US population at that time.1,11 However, more recent analyses using all available VA laboratory data indicate that the anti-HCV prevalence in the veteran population in current VA care is 8.4%.12 Within the VA, however, as in the general population, the prevalence of HCV infection is not the same across gender and race/ethnicity, and epidemiologic disparity exists.7,10,13,14
Recognition of the current burden of HCV in these disparate populations and the new emphasis on screening could lead to identification of those with previously undiagnosed infection and ultimately to effective treatment of HCV infection. Such screening thus would potentially prevent substantial HCV-related losses of health and life, provided those identified via screening received appropriate treatment.15
Several shortcomings have been noted with the existing HCV screening and prevalence literature, emphasizing a need for more representative population samples, appropriate use of diagnostic tests, and better stratification by gender and race/ethnicity.16 Because of these needs, the identified inequities, and the updated Centers for Disease Control and Prevention and US Preventive Services Task Force recommendations, we (1) assessed the extent to which veterans in recent VA care born 1945 to 1965 have been screened for HCV and, in particular, assessed the extent to which screening has varied by gender and race/ethnicity; (2) assessed the current disease burden by determining the HCV infection prevalence in the male and female veteran population currently in VA care among various race/ethnicity; and (3) estimated the potential clinical impact of complete birth cohort screening within these groups using the HCV infection prevalence from those screened most recently.
METHODS
We performed a retrospective population analysis using the VA’s Corporate Data Warehouse, which includes birth dates, gender, race/ethnicity, and VA laboratory tests from October 1, 1999, onward for veterans who have received VA care. Our analysis included all veterans who had at least 1 VA outpatient visit (including telehealth visits) in 2012. We identified all HCV antibody, viral load, and genotype tests. We considered individual test results “informative” if the result could be categorized as negative or positive for antibody tests, detectable or undetectable for viral load, and detectable for genotype tests if a recognized HCV genotype was reported.
HCV Screening and Prevalence
We determined if each veteran ever had VA HCV screening by December 31, 2012. Any HCV antibody, viral load, or genotype test recorded at any VA facility qualified as HCV screening.
To estimate HCV infection prevalence, we included the number of veterans with testing adequate to determine HCV infection status; specifically, this comprised those veterans with negative anti-HCV testing, positive anti-HCV testing with a negative recombinant immunoblot assay, informative viral load testing, or informative genotype testing. We excluded veterans with positive anti-HCV results but without RNA testing (either viral load or genotype testing), as we could not determine infection status. We determined HCV infection prevalence by dividing the total number of veterans with a detectable viral load or genotype by the total number of veterans with testing adequate to determine HCV infection status.
HCV Incident Diagnosis
For veterans in care in 2012, we used all informative antibody and RNA-based test results to identify the year of first incident diagnosis of HCV. We recorded the year of the first positive screening test in which the confirmatory test (HCV RNA or genotype) could occur at the same time or later.
For those without a positive test, we assigned the year from the date of the first-ever negative test. The population for this analysis comprised those veterans who had a first-ever test with an informative (positive or negative) result in that year.
Patient Characteristics
We calculated HCV screening rates, RNA testing rates, and HCV infection prevalence by gender and race/ethnicity stratified by 3 birth cohorts (before 1945, 1945–1965, and after 1965). We identified race/ethnicity classifications from the VA’s Corporate Data Warehouse. At VA registration, veterans are asked their race with options of American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, White, declined to answer, and unknown. At VA registration, veterans are also asked their ethnicity with options of Hispanic or Latino, not Hispanic or Latino, declined to answer, and unknown.
We classified patients with a reported ethnicity of Hispanic as Hispanic in the combined variable of race/ethnicity regardless of reported race. We classified those in which race and ethnicity were recorded as unknown or declined to answer or in which more than 1 race was reported as “mixed/other/unknown.” In a sensitivity analysis, we recalculated all results, assigning those with Hispanic ethnicity to their selected race category.
For veterans in care in 2012 diagnosed with HCV, we determined the rates of several comorbidities using the occurrence of International Classification of Diseases, 9th Revision17 code in the year. To determine advanced fibrosis or cirrhosis, we calculated their fibrosis-4 score with the standard formula (age × aspartate aminotransferase)/(platelets × sqr[alanine aminotransferase]) using age as of the end of 2012 and the most recent results for the necessary laboratory tests.
We have not reported statistical testing because the very large sample size makes extremely small numeric differences statistically significant even when such small differences are not clinically meaningful. For example, a difference of only 0.13% is statistically significant with a standard α of 0.05 and β of 0.2 when comparing screening rates for the 3 birth cohorts with an overall sample size of 5 400 000.
RESULTS
Overall, 5 500 392 veterans had a VA outpatient visit in 2012. Basic demographic information was remarkably complete, with only 30 veterans (0.0005%) missing gender and 619 (0.011%) missing birth date, leaving 5 499 743 veterans in our study. The cohort was 93.4% male (n = 5 138 887) and 6.6% female, representing a sizable population of 360 856 women. The cohort was 65.3% White (n = 3 593 668), 15.0% Black (n = 823 383), 11.8% mixed/other/unknown (n = 649 375), 5.7% Hispanic (n = 313 468), and less than 1.0% each for American Indian/Alaska Native (n = 38 586), Asian (n = 44 511), and Native Hawaiian/Pacific Islander (n = 36 752).
By birth cohort, 37.4% (n = 2 056 126) were born before 1945, 46.2% (n = 2 541 021) were born between 1945 and 1965, and 16.4% (n = 902 596) were born after 1965. We identified 6 622 782 HCV antibody, viral load, and genotype test results between October 1, 1999, and December 31, 2012, for the veterans in care in 2012. Informative values could be assigned to 6 009 302 (90.7%) of these test results (data not shown).
HCV Screening
For the entire cohort, 3 009 852 (54.7%) had VA HCV screening. HCV screening rates were higher in women (58.2%) than in men (54.5%). Screening rates were highest among Hispanics (68.6%) and Blacks (63.3%) followed by American Indian/Alaska Natives (61.8%), Native Hawaiian/Pacific Islanders (56.8%), Asians (55.5%), Whites (53.5%), and mixed/other/unknown (39.7%). By birth cohort, the HCV screening rate was 41.5% for those born before 1945, 64.2% for those born 1945–1965, and 58.0% for those born after 1965 (data not shown).
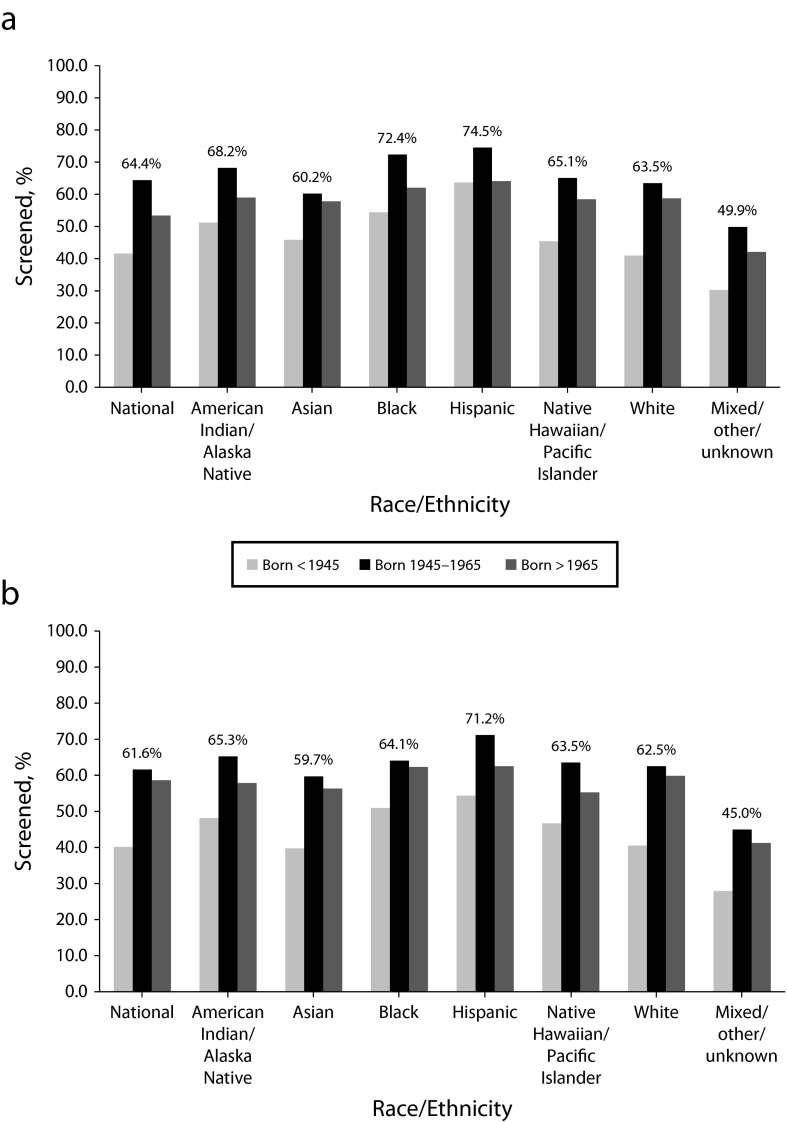
When considering race/ethnicity stratified by gender, HCV screening rates for both men and women among all race/ethnicity categories were highest in those born from 1945 to 1965, slightly lower in those born after 1965, and lowest in those born before 1945 (Figure 1). The 1 exception was male Hispanics, for whom the HCV screening rate was highest in those born 1945 to 1965 (74.5%), but the screening rates in those born before 1945 (63.7%) and after 1965 (64.1%) were nearly identical.
FIGURE 1—
HCV screening by race/ethnicity among veterans who were (a) male and (b) female: Department of Veterans Affairs Corporate Data Warehouse, United States, 2012.
HCV Infection Prevalence
Nationally, 95.1% of veterans identified with anti-HCV had RNA testing for HCV infection. HCV infection prevalence was 6.1% in the more than 2.9 million veterans tested. HCV infection prevalence differed strikingly by birth cohort, gender, and race/ethnicity. For men, HCV infection prevalence was 1.7% for those born before 1945, 10.3% for those born 1945 to 1965, and 1.2% for those born after 1965.
For women, HCV infection prevalence was 1.2% for those born before 1945, 4.7% for those born 1945 to 1965, and 0.7% for those born after 1965. HCV infection prevalence was highest among Blacks (11.8%), followed by Hispanics (6.4%) and American Indian/Alaska Natives (6.4%), Whites (4.8%), Native Hawaiian/Pacific Islanders (4.7%), mixed/other/unknown (3.3%), and Asians (1.8%; data not shown).
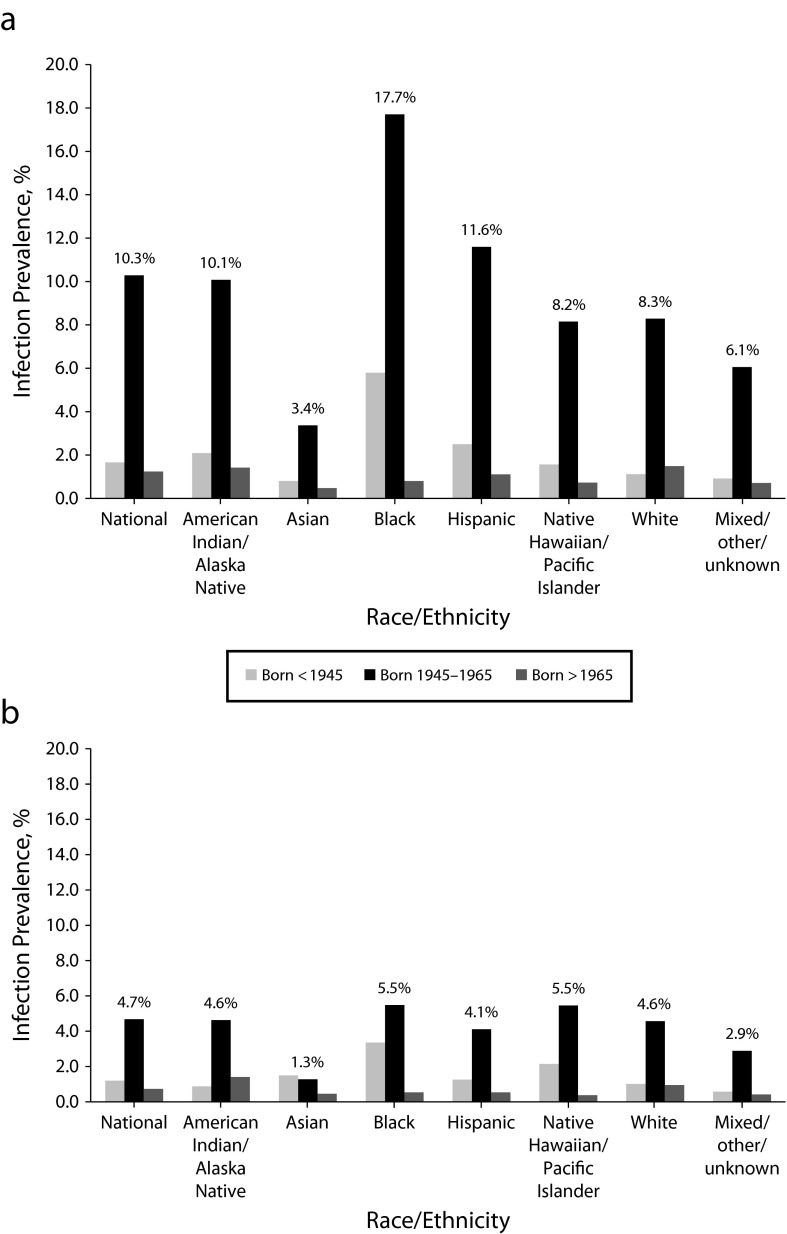
For all men grouped by race/ethnicity, HCV infection prevalence was highest in those born 1945 to 1965, much lower in those born before 1945, and generally lowest in those born after 1965 (Figure 2). Among men born 1945 to 1965, HCV infection prevalence varied widely among the various race/ethnicity subgroups—from 3.4% among Asians to 17.7% among Blacks. In women grouped by race/ethnicity, HCV infection prevalence was similarly highest in those born 1945 to 1965 (Figure 2).
FIGURE 2—
HCV infection prevalence by race/ethnicity among veterans who were (a) male and (b) female: Department of Veterans Affairs Corporate Data Warehouse, United States, 2012.
In the 1945 to 1965 birth cohort, HCV infection prevalence was appreciably lower among women than among men, with less variation by race/ethnicity (Figure 2). Although the prevalence in the 1945 to 1965 birth cohort was highest among Black and Native Hawaiian/Pacific Islander women (5.5%), the prevalence for women in other race/ethnicity subgroups in this birth cohort was generally similar to the marked exception of Asian women, among whom the prevalence was only 1.3% for those born 1945 to 1965.
HCV Incident Diagnosis
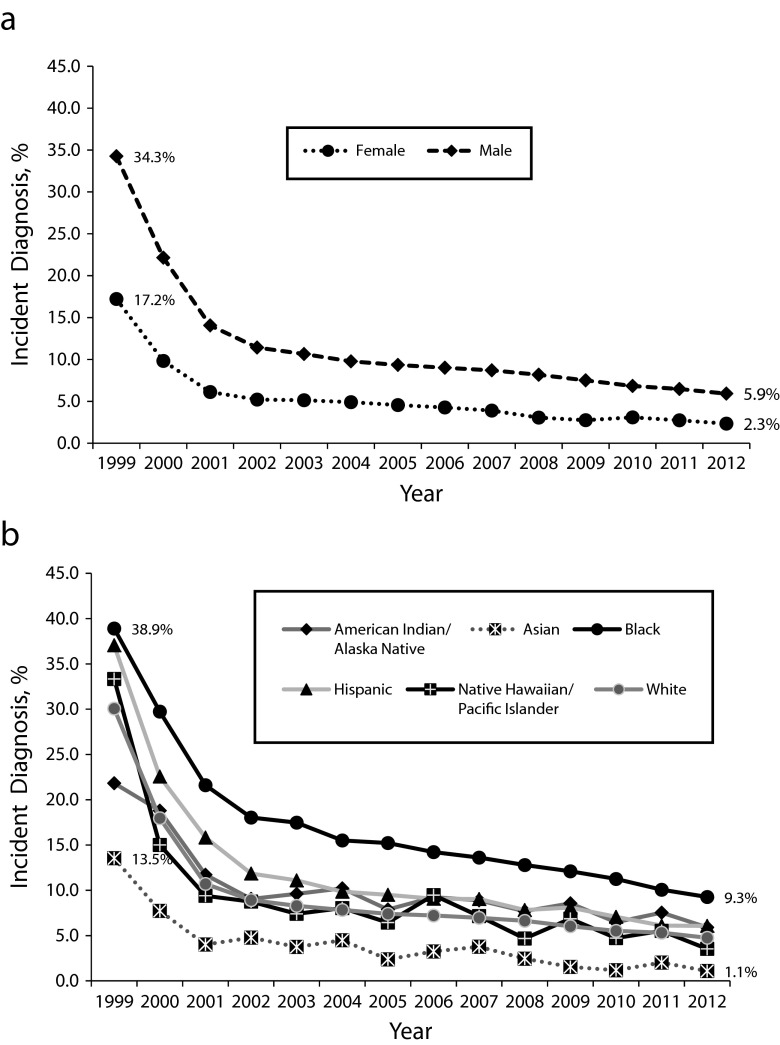
For both men and women in the 1945 to 1965 birth cohort in VA care in 2012, HCV infection incident diagnosis as determined by the year HCV screening first occurred declined sharply from 1999 to 2002 and then more gradually for those screened between 2003 and 2012 (Figure 3). For those first screened for HCV in 2012, the HCV infection incident diagnosis was 5.9% for men (down from 34.3% for those first screened in 1999) and 2.3% for women (down from 17.2% for those first screened in 1999).
FIGURE 3—
HCV incident diagnosis by year of first HCV screening among veterans born 1945–1965 by (a) gender and (b) race/ethnicity: Department of Veterans Affairs Corporate Data Warehouse, United States, 2012.
This same pattern of decline in HCV infection incident diagnosis as determined by year of first screening occurred for each race/ethnicity group (Figure 3). For those in the 1945 to 1965 birth cohort first screened in 2012, HCV infection incident diagnosis varied by race/ethnicity, from 1.1% among Asians to 9.3% among Blacks.
Among those in the 1945 to 1965 birth cohort first identified with HCV in 2012, 25% had advanced fibrosis or cirrhosis as determined by a fibrosis-4 score greater than 3.25, which matched the percentage among those in the birth cohort identified in prior years with HCV. Those most recently diagnosed with HCV had high rates of other comorbidities in 2012, including diabetes (17%), dyslipidemia (20%), alcohol use (26%), depression (26%), and hypertension (48%).
Rates of HIV and hepatitis B virus coinfection were 2% each. The rates in those first diagnosed in 2012 were generally, but not always, lower than were the rates for those in the birth cohort identified in prior years with HCV: diabetes (25%), dyslipidemia (28%), alcohol use (25%), depression (33%), hypertension (55%), HIV (3%), and hepatitis B virus (1%; data not shown).
Estimates of Additional Cases to Be Found
Table 1 includes the HCV infection incident diagnosis for those first screened in 2012 taking into account both gender and race/ethnicity. Table 1 also includes estimates of the number of additional veterans who would be identified with HCV infection with full birth cohort screening by gender and race/ethnicity using the most recent HCV infection incident diagnosis rate. If full birth cohort screening were adopted among veterans, an estimated 48 928 male veterans—including 12 291 Black men—and 1484 female veterans who did not know of their HCV infection would potentially be identified as HCV infected.
TABLE 1—
Estimates of the Number of Additional Male and Female Veterans Born 1945–1965 Who Would Be Identified With HCV Infection With Complete Birth Cohort Screening: Department of Veterans Affairs Corporate Data Warehouse, United States, 2012
| Male Veterans |
Female Veterans |
|||||
| Race/Ethnicity | 1945–1965 Birth Cohort Not Screened, No. | Incident Diagnosis in Those Screened in 2012, % | Additional Estimated Cases Found With Full Cohort Screening, No. | 1945–1965 Birth Cohort Not Screened, No. | Incident Diagnosis in Those Screened in 2012, % | Additional Estimated Cases Found With Full Cohort Screening, No. |
| American Indian/Alaska Native | 6044 | 6.3 | 381 | 577 | 1.1 | 6 |
| Asian | 6665 | 1.2 | 80 | 477 | 0.0 | 0 |
| Black | 122 908 | 10.0 | 12 291 | 16 999 | 2.8 | 476 |
| Hispanic | 34 543 | 6.3 | 2176 | 2030 | 1.2 | 24 |
| Native Hawaiian/Pacific Islander | 5424 | 3.5 | 190 | 454 | 3.4 | 15 |
| White | 548 896 | 4.9 | 26 896 | 33 631 | 2.3 | 774 |
| Mixed/other/unknown | 121 301 | 5.7 | 6914 | 9017 | 2.1 | 189 |
| Total | 48 928 | 1484 | ||||
In a sensitivity analysis, assigning those of Hispanic ethnicity to their selected race category did not appreciably change the results with regard to HCV screening rates, HCV prevalence rates, or the estimate of additional cases that would be found with expanded birth cohort testing.
DISCUSSION
This population-based evaluation provides important information about the current screening and prevalence of HCV infection in vulnerable groups of veterans. As shown in this population, although screening rates were high, a large disparate burden of disease exists, particularly among Black men born between 1945 and 1965. The HCV infection prevalence among Blacks born during this period first screened in 2012 remains substantially higher than does the prevalence for other race/ethnicity groups, although HCV infection incident diagnosis for all race/ethnicity subgroups in the VA are higher than is that of the general US population.1,18
If full Centers for Disease Control and Prevention and US Preventive Services Task Force recommended birth cohort testing were implemented in the VA—extrapolating the most recent incidence diagnosis estimates—there is the potential to identify almost 13 000 Black veterans currently in VA care with previously unrecognized HCV infection.
Screening rates were high in the target birth cohort, with nearly two thirds of all male and female veterans tested, regardless of race/ethnicity. As evidenced by the high screening rates in both male and female veterans among all race/ethnicities, the efforts that the VA has taken to promote HCV screening testing are having results. We observed even higher screening rates among those race/ethnicities in which others have reported inequities in screening, namely Blacks and Hispanics. Among those with positive screening tests, nearly 95% had appropriate supplementary RNA testing confirming the success of the VA’s effort to ensure that patients with positive antibody tests are appropriately tested for HCV infection.
In these comprehensive data, we found much higher screening rates than have other health care settings. Most prior studies have reported much lower HCV screening rates, leading to estimates that less than 40.0% of HCV-infected persons have been tested.1 In a study examining 4 large US private health care organizations, for example, HCV screening rates examined by age or race for those in care between 2006 and 2008 ranged from a low of 8.5% (those aged ≥ 80 years) to 22.4% (Black persons).4
In a study of patients with a clinic visit during 2 months in 2008 to a New York City academic medical center, 39.7% of patients had been tested overall. Among those with an identified risk (including the high-prevalence birth cohort), 48.6% had been HCV tested.19 The reported HCV infection prevalences in this high-risk urban population, which consisted mostly of Black and Hispanic women, were 4.6% and 7.7%, respectively. These HCV infection prevalences are similar to the 5.5% and 4.1% we have reported for Black and Hispanic women, respectively.
Despite the substantial decline in HCV infection incident diagnosis in those screened over the past 10 years compared with those screened between 1999 and 2002, the current incident diagnosis rate of 10% among Black male veterans is still higher than are any other reported HCV infection prevalence estimates among the general population.1,2,18
A recent evaluation of the National Health and Nutrition Examination Survey from 2001 through 2010 reported a prevalence of 2.2% among male Blacks in 2009 to 2010, down from approximately 3.3% in 2001 to 2002.18 This same study also reported a general US prevalence of 3.5% in those born 1945 to 1965 and noted a decreasing trend in prevalence on the basis of gender, with the most recent prevalence of 1.9% in men and 0.7% in women in 2009 to 2010. These HCV infection prevalence estimates are substantially lower than is the prevalence that we observed of 5.9% among male veterans and 2.3% among female veterans born 1945 to 1965 who were first screened in 2012.
Possible differences in the results between the National Health and Nutrition Examination Survey and our VA population-based study may be related to the methods used as well as the risk profile of the participants. Our analysis represents the entire population of veterans in VA care in 2012, including the homeless, the institutionalized, and those receiving hemodialysis. The multistage probability sampling design used by the National Health and Nutrition Examination Survey does not include such individuals.
In addition, prior work, which included questionnaire information about risk factors, concluded that the elevated prevalence of HCV in veterans reflected more exposure to traditional risk factors (i.e., transfusion or intravenous drug use) and to other potential risk factors (i.e., snorting drugs, incarceration, or 15 or more sexual partners).11
Although the VA HCV screening rates among disparate populations are much higher than are those reported in other health care organizations, a gap in care still remains; 28% of Black male and 36% of Black female veterans born 1945 to 1965 seemingly lack VA HCV screening. If the current HCV infection incident diagnosis estimates by race/ethnicity and gender in the 1945 to 1965 birth cohort are applied to those in the cohort without HCV screening, as many as 12 291 additional Black male veterans and 476 additional Black female veterans in VA care in 2012 may have unrecognized HCV infection that would be identified with complete screening of the birth cohort.
The high prevalence in this birth cohort and the underacknowledgment of risk makes it reasonable to use birth cohort screening as a simple, nonstigmatizing criterion to prompt providers to screen their patients for HCV. Because of the disparity of disease observed among Black male veterans, further refining the birth cohort recommendation to include those race/ethnicities with the highest prevalence may more accurately identify those who are likely to test positive.
Timely diagnosis becomes even more important because of the landmark changes occurring in the treatment of HCV infection, with cure rates approximating more than 90%, including those of Black patients, who have generally had lower treatment response rates with earlier HCV antiviral treatments.20 Without identification of HCV infection and subsequent HCV care and treatment, we will begin to see significantly more advanced liver disease, namely cirrhosis and hepatocellular carcinoma, of which mortality for Blacks is reported as 2 to 3 times greater than that for non-Hispanic Whites.21
A recent Institute of Medicine report identified 3 underlying factors impeding current efforts to combat HCV: (1) lack of knowledge and awareness among health care and social service providers; (2) lack of knowledge and awareness among at-risk populations, members of the public, and policymakers; and (3) insufficient understanding about the extent and seriousness of this public health problem.22 To realize improvements in outcomes, effective screening of male and female veterans born between 1945 and 1965, particularly Black men, needs to continue and can be facilitated with VA-wide promotion of awareness of HCV infection emphasizing the extensive burden in this population.
Limitations
Our study has several limitations. The HCV screening rates are likely underestimated for 2 reasons: (1) the VA’s Corporate Data Warehouse includes only VA laboratory data, preventing identification of veterans with HCV screening outside the VA; and (2) the VA’s Corporate Data Warehouse includes laboratory data only from October 1999 onward, preventing identification of veterans screened for HCV before October 1999.
If veterans with positive non-VA or positive pre-1999 results are more likely to be rescreened for HCV in the VA than are those with negative non-VA or negative pre-1999 results, this would lead to a slight overestimation of prevalence. However, because this cohort consists of veterans in care in 2012, the impact of the missing pre-1999 laboratory data is likely to be small. We did not consider sociodemographic and behavioral risk factors that may affect prevalence of HCV in vulnerable groups.
Finally, we do not have information about the severity of liver disease or comorbidities in those who have not yet been identified with HCV. We do, however, have information about those in the 1945 to 1965 birth cohort who were first identified with HCV in 2012. This group provides the closest approximation for those in the 1945 to 1965 birth cohort who might be identified with expanded birth cohort testing. If the high rate of advanced fibrosis or cirrhosis in those most recently diagnosed applies to those not yet identified, those identified with expanded birth cohort testing may also be more likely to have substantial liver complications from their HCV infection, which is consistent with the time course of disease progression. In addition, if the rates of comorbidities in those most recently diagnosed with HCV also apply to those not yet identified, those identified with expanded birth cohort testing are likely to have high rates of comorbidities that may affect and complicate the care and treatment of their HCV infection.
Conclusions
HCV infection prevalence in veterans is uneven and, coupled with the lack of recognition of HCV infection in vulnerable veteran populations, can lead to inequities in care and treatment. Knowledge of the current burden of HCV infection in disparate groups among veterans is critical for addressing the inequity of care. We have established national screening and prevalence data for veterans that can serve as a baseline moving forward to evaluate future screening and prevalence in these vulnerable populations because of the updated Centers for Disease Control and Prevention and US Preventive Services Task Force recommendations. These results should serve to increase public awareness of the current burden of disease in veterans differentiated by gender and race/ethnicity.
VA providers should be made aware that screening these populations is needed so that appropriate care and curative treatments can be provided, limiting consequences of undiagnosed HCV infection. Although curing HCV infection becomes increasingly likely for many individuals, it is less certain how these remarkable new treatments will affect those disparate populations in which infection has not yet been diagnosed unless greater efforts are undertaken to educate providers about this burden and screen those at highest risk.
Acknowledgments
This work was prepared independently, without financial support.
Human Participant Protection
This health care operations work is not considered human participant research so does not require institutional review board approval. Under the guidance of the VA Office of Research Oversight (ORO), the Office of Public Health/Population Health has the authority to perform the analyses as part of its mission to evaluate and improve health care operations. The guidance from ORO is available in detail in VHA Handbook 1058.05 (http://www.va.gov/ORO/ORO_Policy_Docum.asp).
References
- 1.Smith BD, Morgan RL, Beckett GA et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR Recomm Rep. 2012;61(RR-4):1–32. [PubMed] [Google Scholar]
- 2.Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144(10):705–714. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- 3.Roblin DW, Smith BD, Weinbaum CM, Sabin ME. HCV screening practices and prevalence in an MCO, 2000–2007. Am J Manag Care. 2011;17(8):548–555. [PubMed] [Google Scholar]
- 4.Spradling PR, Rupp L, Moorman AC et al. Hepatitis B and C virus infection among 1.2 million persons with access to care: factors associated with testing and infection prevalence. Clin Infect Dis. 2012;55(8):1047–1055. doi: 10.1093/cid/cis616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ly KN, Xing J, Klevens RM, Jiles RB, Ward JW, Holmberg SD. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Ann Intern Med. 2012;156(4):271–278. doi: 10.7326/0003-4819-156-4-201202210-00004. [DOI] [PubMed] [Google Scholar]
- 6.Rein DB, Wittenborn JS, Weinbaum CM, Sabin M, Smith BD, Lesesne SB. Forecasting the morbidity and mortality associated with prevalent cases of pre-cirrhotic chronic hepatitis C in the United States. Dig Liver Dis. 2011;43(1):66–72. doi: 10.1016/j.dld.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Alter MJ, Kruszon-Moran D, Nainan OV et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341(8):556–562. doi: 10.1056/NEJM199908193410802. [DOI] [PubMed] [Google Scholar]
- 8.Rein DB, Smith BD, Wittenborn JS et al. The cost-effectiveness of birth-cohort screening for hepatitis C antibody in U.S. primary care settings. Ann Intern Med. 2012;156(4):263–270. doi: 10.7326/0003-4819-156-4-201202210-00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forde KA, Tanapanpanit O, Reddy KR. Hepatitis B and C in African Americans: current status and continued challenges. Clin Gastroenterol and Hepatol. 2014;12(5):738–748. doi: 10.1016/j.cgh.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seeff LB, Miller RN, Rabkin CS et al. 45-year follow-up of hepatitis C virus infection in healthy young adults. Ann Intern Med. 2000;132(2):105–111. doi: 10.7326/0003-4819-132-2-200001180-00003. [DOI] [PubMed] [Google Scholar]
- 11.Dominitz JA, Boyko EJ, Koepsell TD et al. Elevated prevalence of hepatitis C infection in users of United States veterans medical centers. Hepatology. 2005;41(1):88–96. doi: 10.1002/hep.20502. [DOI] [PubMed] [Google Scholar]
- 12.Backus LI, Belperio PS, Loomis TP, Yip GH, Mole LA. Hepatitis C virus screening and prevalence among US veterans in Department of Veterans Affairs care. JAMA Intern Med. 2013;173(16):1549–1552. doi: 10.1001/jamainternmed.2013.8133. [DOI] [PubMed] [Google Scholar]
- 13.Pyrsopoulos N, Jeffers L. Hepatitis C in African Americans. J Clin Gastroenterol. 2007;41(2):185–193. doi: 10.1097/01.mcg.0000225689.60335.44. [DOI] [PubMed] [Google Scholar]
- 14.Butterfield MI, Bosworth HB, Stechuchak KM et al. Racial differences in hepatitis B and hepatitis C and associated risk behaviors in veterans with severe mental illness. J Natl Med Assoc. 2004;96(1):43–52. [PMC free article] [PubMed] [Google Scholar]
- 15.Liu S, Cipriano LE, Holodniy M, Goldhaber-Fiebert JD. Cost-effectiveness analysis of risk-factor guided and birth-cohort screening for chronic hepatitis C infection in the United States. PLoS ONE. 2013;8(3):e58975. doi: 10.1371/journal.pone.0058975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lavanchy D. Evolving epidemiology of hepatitis C virus. Clin Microbiol Infect. 2011;17(2):107–115. doi: 10.1111/j.1469-0691.2010.03432.x. [DOI] [PubMed] [Google Scholar]
- 17.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 18.Ditah I, Ditah F, Devaki P et al. The changing epidemiology of hepatitis C virus infection in the United States: National Health and Nutrition Examination Survey 2001 through 2010. J Hepatol. 2014;60(4):691–698. doi: 10.1016/j.jhep.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 19.Southern WN, Drainoni ML, Smith BD et al. Hepatitis C testing practices and prevalence in a high-risk urban ambulatory care setting. J Viral Hepat. 2011;18(7):474–481. doi: 10.1111/j.1365-2893.2010.01327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawitz E, Mangia A, Wyles D et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368(20):1878–1887. doi: 10.1056/NEJMoa1214853. [DOI] [PubMed] [Google Scholar]
- 21.Fleckenstein J. Chronic hepatitis C in African Americans and other minority groups. Curr Gastroenterol Rep. 2004;6(1):66–70. doi: 10.1007/s11894-004-0028-z. [DOI] [PubMed] [Google Scholar]
- 22.Institute of Medicine. Hepatitis and liver cancer: a national strategy for the prevention and control of hepatitis B and C. 2010. Available at: http://www.iom.edu/Reports/2010/Hepatitis-and-Liver-Cancer-A-National-Strategy-for-Prevention-and-Control-of-Hepatitis-B-and-C.aspx. Accessed May 1, 2014. [PubMed]