Abstract
Objectives. We compared the strength of association between average 5-year county-level mortality rates and area-level measures, including air quality, sociodemographic characteristics, violence, and economic distress.
Methods. We obtained mortality data from the National Vital Statistics System and linked it to socioeconomic and demographic data from the Census Bureau, air quality data, violent crime statistics, and loan delinquency data. We modeled 5-year average mortality rates (1998–2002) for all-cause, cancer, heart disease, stroke, and respiratory diseases as a function of county-level characteristics using ordinary least squares regression models. We limited analyses to counties with population of 100 000 or greater (n = 458).
Results. Demographic and socioeconomic characteristics, particularly the percentage older than 65 years and near poor, were top predictors of all-cause and condition-specific mortality, as were a high concentration of construction and service workers. We found weaker associations for air quality, mortgage delinquencies, and violent crimes. Protective characteristics included the percentage of Hispanics, Asians, and married residents.
Conclusions. Multiple factors influence county-level mortality. Although county demographic and socioeconomic characteristics are important, there are independent, although weaker, associations of other environmental characteristics. Future studies should investigate these factors to better understand community mortality risk.
Community characteristics have been linked to mortality risks. Previous research has documented associations between area-level poverty, education, and racial residential segregation with all-cause and condition-specific mortality rates.1–4 Although these studies highlight the relationship between social context and mortality, they typically focus on a limited set of indicators. Furthermore, these studies rarely examine social factors in conjunction with other area-level factors.
For example, a distinct line of research has emerged on the role of air quality in health and mortality. These studies have found significant associations between airborne carbon monoxide, ozone, and fine particulate matter (PM) with cardiovascular symptoms, cancer, and deaths. For instance, the probability of emergency department admissions for cardiovascular disease increases 0.96% for every 1 part-per-billion increase in peak daily carbon monoxide.5 A 10 part-per-billion increase in ozone levels for 1 week increases cardiovascular and respiratory mortality by 0.64%.6 Additionally, a 10-microgram increase in airborne fine PM has been shown to increase admissions for respiratory and cardiovascular conditions by similar magnitudes.7 Finally, there are characteristics, such as financial distress, that have demonstrated associations with health outcomes at the individual level,8–11 but their roles as independent community-level predictors of mortality have not been examined.
We address this gap in the literature by simultaneously modeling and examining the relative strength of association between average 5-year mortality rates and a diverse set of county-level characteristics, including air quality, sociodemographics, violence, and housing distress, that have emerged from different lines of research that typically do not intersect.
METHODS
We drew on national data from federal agencies, including the Environmental Protection Agency, the Federal Bureau of Investigation, and the Federal Reserve as well as the Census Bureau and the National Vital Statistics System.
Dependent Variables
The dependent variables were derived from 5 years of annual mortality data reported to the National Vital Statistics System from 1998 to 2002 for counties with populations of 100 000 or greater (n = 458). Using information on causes of death available from the National Vital Statistics System, we calculated average 5-year all-cause mortality rates as well as mortality rates for 4 leading causes of death (cancer, heart disease, stroke, and respiratory diseases).
As we examined county age distribution as a predictor in our models, we did not use age-adjusted mortality rates as the study outcome. More details are available from http://www.cdc.gov/nchs/deaths.htm.
Independent Variables
Sociodemographic characteristics.
We obtained county-level information from Summary Files 1 and 3 released by the US Census Bureau for the 2000 Census on the sociodemographic and economic makeup of the 458 counties in our analysis. These included the proportion of residents of different age categories, race and ethnicity, educational attainment, poverty level, and occupation for each county. Educational attainment for residents aged 25 years and older included less than high school, high school graduate, some college, and college or more. We categorized poverty levels within the counties as poor (income-to-poverty ratio < 1.00), near poor (income-to-poverty ratio ≥ 1.00 and < 2.00), and nonpoor (income-to-poverty ratio ≥ 2.00). We calculated the poverty ratio using the federal poverty level standards specified by the Office of Management and Budget for 2000. We categorized occupations as management, business, financial, or other professional; sales, office, or administration; service; farming, fishing, or forestry; construction, extraction, maintenance and production, transportation, or material moving; and other. Details are available from http://www.census.gov/prod/2001pubs/mso-01icdp.pdf.
Air quality.
We obtained county-level data for 2000 on 6 common air pollutants—ground-level ozone; PM2.5, representing particles with diameters less than or equal to 2.5 micrograms; PM10, representing particles with diameters between 2.5 and 10 micrograms; carbon monoxide (CO); nitrogen dioxide (NO2); and sulfur dioxide (SO2)—from the US Environmental Protection Agency.12 We decided not to include the Air Quality Index because the reported Air Quality Index score for each county can reflect different combinations of the 6 criterion pollutants. We also excluded 4 individual pollutants, CO, NO2, PM10, and SO2, with more than 25% missing because of concerns regarding the validity of the imputed value when levels of missing values reached 50% to 60%.
Violent crime.
We obtained data on violent crime activity per county from the Federal Bureau of Investigation’s Uniform Crime Reporting system, which the Inter-University Consortium for Political and Social Research maintains and cleans.13 Violent crimes consisted of murder, rape, robbery, aggravated assault, burglary, larceny, and motor vehicle theft. We divided the count of violent crimes in each county by its population in 2000 to compute the violent crime rate per 1000 residents.
We imputed values for counties with information for only part of the year by annualizing the available months of data when at least 3 months of data were available. For cases in which less than 3 months of crime data were reported for a county, we imputed missing values using data from neighboring counties. Less than 6 months of data were available for 14% of the counties in our sample.
Economic distress.
We obtained county-level data on mortgage, credit card, and automobile loan delinquencies from the Federal Reserve Bank of New York.14 This data set included the percentage of a county’s population with loans more than 90 days in arrears on the basis of a 5% sample of individuals who had credit reports with EquiFax, one of the major national credit bureaus.
Delinquency data were reported only for counties with at least 10 000 consumers with credit reports as of December 2000. We used the average of delinquency data for each category of loans in our models.
Analysis
We performed all analyses in our study at the county level. We limited the analysis to counties with a population of 100 000 or greater because the reliability of mortality rates for these counties is more robust. To identify potentially important contextual factors, we examined the bivariate association of each independent variable with mortality rates for death from all causes and the top 4 causes of death (cancer, heart disease, respiratory conditions, and stroke). If we observed multiple measures for a particular domain (air quality and economic distress) to be significantly associated with mortality outcomes, we modeled county mortality rates as a function of significant variables using multiple linear regression to determine whether independent relationships existed and if not to identify the best representative indicator.
Finally, we combined significant measures from these bivariate and domain-specific regression models into a final set of models to compare the relative influence of different county-level sociodemographic, economic, and environmental characteristics. We have presented the difference in the number of deaths for counties at the 75th percentile of each characteristic compared with counties at the 25th percentile to facilitate comparison between characteristics with different scales. The final set of models examined education, occupation, and poverty in separate models because of the strong collinear relationship of these socioeconomic variables. To correct for heteroskedacity in errors, we weighted observations by the square root of a county’s population, after finding that SEs were approximately inversely proportional to population size. We performed all analyses on Stata 11.0 (StataCorp LP, College Station, TX). We used a P < .05 level to indicate statistical significance and provided 95% confidence intervals (CIs) for estimates.
Except for the 4 air pollutants, missing data at the county level were not common for variables included in our analyses. We imputed values for 87 counties with missing data on fine PM (PM2.5) and 11 counties that did not report any violent crime statistics for 2000. Our imputation technique treated air quality as correlated with observed county-level sociodemographic variables. We used the empirical correlation between these variables for counties with complete air quality to specify a multivariate normal distribution and simulated draws from this distribution to impute missing air quality data. We compared this imputation method to an alternative approach that calculated missing observations as a spatially weighted average of nearby counties’ pollution data. Because average associations were broadly similar in both imputation techniques, we have presented our results using multiple imputation,15 because this approach conservatively adjusts SEs upward to account for imputation uncertainty.16
RESULTS
Table 1 presents descriptive statistics of mortality, sociodemographic, economic, and environmental characteristics for the 458 counties, with each county weighted equally. The average all-cause mortality rate was 843 per 100 000 persons. Deaths from heart conditions, cancer, respiratory conditions, and stroke were 242, 197, 83, and 45, respectively, per 100 000 residents. On average, 12.4% of county residents were aged 65 years or older, with 12.0% Black, 9.5% Hispanic, and 3.3% Asian residents. More than a quarter of residents were in or near poverty level. An average of 27.0% of residents were employed in sales or administrative occupations, with another 23.5% employed in construction-related work. Fifty-two percent of county residents were married. The average level of fine PM (PM2.5) was 41 (representing good air quality), and the average number of violent crimes per 1000 residents was 44. Across all counties, 1.1% of mortgages were more than 90 days delinquent in 2000.
TABLE 1—
Sociodemographic, Economic, and Environmental Characteristics of Included Counties (n = 458): US Counties With Population ≥ 100 000, 2000
| Characteristic | Mean (95% CI) | Min | Max |
| Causes of death/100 000a | |||
| All causes | 842.8 (823.8, 861.8) | 371.0 | 1587.9 |
| Heart disease | 241.5 (234.6, 248.5) | 85.8 | 518.7 |
| Cancer | 197.0 (192.5, 201.5) | 76.1 | 412.1 |
| Respiratory conditions | 82.9 (80.8, 85.0) | 25.6 | 169.7 |
| Stroke | 45.4 (44.1, 46.6) | 16.3 | 99.2 |
| Age, y, % | |||
| 0–17 | 25.4 (25.2, 25.7) | 14.5 | 36.2 |
| 18–24 | 10.0 (9.7, 10.3) | 4.5 | 32.0 |
| 25–44 | 30.1 (29.8, 30.3) | 18.8 | 43.5 |
| 45–64 | 22.1 (21.9, 22.3) | 12.7 | 29.7 |
| 65–79 | 9.2 (8.9, 9.4) | 3.8 | 26.2 |
| ≥ 80 | 3.2 (3.1, 3.3) | 0.9 | 8.9 |
| Race/ethnicity, % | |||
| White | 73.8 (72.1, 75.5) | 4.9 | 97.4 |
| Black | 12.0 (10.8, 13.2) | 0.2 | 67.3 |
| Asian | 3.3 (2.8, 3.7) | 0.3 | 58.2 |
| Hispanic | 9.5 (8.3, 10.7) | 0.4 | 94.3 |
| Native American or other | 1.5 (1.2, 1.7) | 0.2 | 38.6 |
| Married resident, % | 52.1 (51.5, 52.8) | 22.8 | 70.8 |
| Education, % | |||
| < high school | 17.4 (16.8, 18.0) | 5.1 | 49.5 |
| Completed high school | 29.0 (28.4, 29.6) | 11.7 | 49.9 |
| Some college | 28.3 (27.9, 28.7) | 15.8 | 40.3 |
| Poverty status,b % | |||
| In poverty | 11.3 (10.8, 11.7) | 2.6 | 35.9 |
| Near poverty | 16.2 (15.7, 16.6) | 5.8 | 29.8 |
| Employment, % | |||
| Management or professional occupations | 33.7 (33.1, 34.3) | 20.3 | 61.3 |
| Sales or administration | 27.0 (26.8, 27.2) | 18.1 | 32.4 |
| Construction | 23.5 (23.0, 24.0) | 8.3 | 43.9 |
| Service occupations | 15.1 (14.9, 15.4) | 8.7 | 30.3 |
| Farming or agriculture | 0.7 (0.5, 0.8) | 0.1 | 13.2 |
| Average fine particulate matterb | 41.2 (40.2, 42.1) | 4.2 | 73.5 |
| Percentage of mortgages > 90-d delinquent | 1.1 (1.0, 1.1) | 0.1 | 3.9 |
| No. of violent crimes/1000 persons | 43.7 (41.9, 45.4) | 10.4 | 145.5 |
Note. CI = confidence interval.
5-year average (1998–2002).
We calculated the poverty ratio using the federal poverty level standards specified by the Office of Management and Budget for 2000.
Particles with diameters ≤ 2.5 µg. On the basis of 370 counties with data on particulate matter.
Community Characteristics and All-Cause Mortality
Table 2 presents the bivariate correlation between county characteristics and all-cause mortality. As expected, counties with older populations or higher percentages of residents with lower educational attainment or lower household income had higher mortality rates. Counties with higher percentages of married residents or Hispanic or Asian residents tended to have lower mortality rates.
TABLE 2—
Pearson Correlation of County Characteristics in 2000 and Average 5-Year All-Cause Mortality (1998–2002): US Counties With Population ≥ 100 000
| Characteristics | R (95% CI) |
| Age, y | |
| 0–17 | −0.5146*** (−0.6062, −0.4230) |
| 18–24 | −0.2932*** (−0.3848, −0.2016) |
| 25–44 | −0.6303*** (−0.7219, −0.5387) |
| 45–64 | 0.4563*** (0.3647, 0.5479) |
| 65–79 | 0.8478*** (0.7562, 0.9394) |
| ≥ 80 | 0.8584*** (0.7668, 0.9500) |
| Race/ethnicity | |
| White | 0.2173*** (0.1257, 0.3089) |
| Black | 0.1368*** (0.0452, 0.2284) |
| Asian | −0.2909*** (−0.3825, −0.1993) |
| Hispanic | −0.3112*** (−0.4028, −0.2196) |
| Native American or other | −0.0888 (−0.1804, 0.0028) |
| Education | |
| < high school | 0.2403*** (0.1487, 0.3319) |
| High school graduate | 0.5863*** (0.4947, 0.6779) |
| Some college | −0.2644*** (−0.3560, −0.1728) |
| Employment | |
| Service | 0.3944*** (0.3028, 0.4860) |
| Sales or administration | 0.0130 (−0.0786, 0.1046) |
| Farming | −0.0838 (−0.1754, 0.0078) |
| Construction | 0.3226*** (0.2310, 0.4142) |
| Poverty status | |
| Poverty | 0.1612*** (0.0696, 0.2528) |
| Near poverty | 0.3067*** (0.2151, 0.3983) |
| Married resident | −0.2913*** (−0.3829, −0.1997) |
| PM2.5 | 0.1291* (0.0273, 0.2309) |
| Mortgage delinquency | 0.3580*** (0.2664, 0.4496) |
| Violent crime | 0.1300** (0.0373, 0.2227) |
Note. CI = confidence interval; PM2.5 = particulate matter with diameters ≤ 2.5 µg. We calculated the poverty ratio using the federal poverty level standards specified by the Office of Management and Budget for 2000.
*P < .05; **P < .01; ***P < .001.
Counties with higher percentages of residents who were White or Black or employed in service occupations and construction had higher mortality rates. Counties with more economic distress, as measured by higher mortgage delinquencies, also had higher mortality rates. In terms of air pollutants and crime, higher levels of fine PM and violent crime were associated with higher all-cause mortality. Based on the multiple linear regression model, Figure 1 presents the difference in number of deaths from all causes per 100 000 persons between counties at the 25th percentile and counties at the 75th percentile of each county characteristic. Overall, counties with higher proportions of elderly residents, particularly those aged 65 years and older, had the largest difference in mortality. Although weaker than those for age, county socioeconomic characteristics also had strong, independent associations with mortality. Counties with high percentages of residents with low educational attainment or near poverty also had substantially higher numbers of deaths.
FIGURE 1—
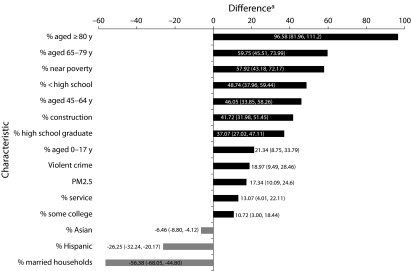
Magnitude of significant county characteristics association with all-cause mortality: US counties with population ≥ 100 000: 1998–2002.
Note. PM2.5 = particulate matter with diameters ≤ 2.5 µg. We calculated the poverty ratio using the federal poverty level standards specified by the Office of Management and Budget for 2000.
aNumber of deaths from all causes per 100 000 persons between counties at the 25th percentile and counties at the 75th percentile of each characteristic. All associations were statistically significant at p< 0.01. Reference categories for regression models: Percent Bachelors Plus; management, business, financial operations, and professional occupations; 25-44 years of age; Percent White; Poverty ≥ 200%. Values in parentheses indicate 95% confidence intervals.
Interestingly, the percentage of residents in poverty in a county was not significantly associated with mortality. The association of occupation with mortality was generally comparable to those observed for education. The difference in mortality from the 25th to 75th percentile counties ranged between 13.1 (percentage service workers) and 41.7 (percentage construction workers) for occupation and between 10.7 (percentage some college) and 48.7 (percentage < high school) for education. Of the significant relationships we found, the difference in the number of deaths between 25th and 75th percentile counties associated with rates of violent crime and level of fine PM was smallest but remained substantial at 19.0 and 17.3, respectively.
Three characteristics, the percentage of Hispanics, Asians, and married residents in a county were associated with reductions in all-cause mortality. The reduction ranged between 56.4 (percentage married) and 6.5 (percentage Asian) for counties at the 25th and 75th percentile of these sociodemographic characteristics.
Community Characteristics and Higher Cause-Specific Mortality
Table 3 presents the county characteristics ranked by the difference in the number of condition-specific deaths per 100 000 persons between counties at the 25th and 75th percentile of each characteristic. As with all-cause mortality, county age and socioeconomic characteristics—particularly the percentage of elderly residents and residents of low income and low educational attainment—were robust predictors of cause-specific mortality. Of the occupation categories we examined, the percentage of construction workers in a county was consistently associated with greater mortality for all 4 causes, although the ranking of its influence varied by condition, being strongest for heart disease and weakest for respiratory conditions. We also observed significant associations of service, sales, and farming, mining, or fishing occupations with greater mortality, but we did not consistently observe these associations across conditions.
TABLE 3—
The Estimated Increase in Death per 100 000 Persons (5-Year Average, 1998–2002) for Selected Leading Causes of Death for Difference From 25th to 75th percentile of County Characteristics in 2000: US Counties With Population ≥ 100 000
| Heart Disease |
Cancer |
Respiratory Condition |
Stroke |
|||||
| Ranka | Characteristic | Estimate, % (95% CI) | Characteristic | Estimate, % (95% CI) | Characteristic | Estimate, % (95% CI) | Characteristic | Estimate, % (95% CI) |
| 1 | Aged ≥ 80 y | 44.36*** (35.88, 52.84) | Aged 65–79 y | 22.94*** (19.40, 26.44) | Near poverty | 10.05*** (7.16, 12.95) | Aged ≥ 80 y | 9.55*** (7.47, 11.62) |
| 2 | High school graduate | 19.92*** (14.12, 25.80) | Aged ≥ 80 y | 13.64*** (10.10, 17.33) | Aged 65–79 y | 9.20*** (6.10, 12.31) | Near poverty | 7.22*** (5.37, 9.07) |
| 3 | Employed in construction | 16.07*** (10.77, 21.45) | Aged 45–64 y | 9.27*** (6.24, 12.29) | < high school | 7.23*** (4.87, 9.52) | Aged 45–64 y | 5.10*** (3.38, 6.82) |
| 4 | Near poverty | 14.50** (5.92, 23.07) | High school graduate | 7.35*** (4.82, 9.80) | Aged 45–64 y | 6.30*** (3.66, 8.93) | < high school | 4.94*** (3.41, 6.47) |
| 5 | < high school | 14.32*** (8.13, 20.51) | < high school | 6.88*** (4.17, 9.52) | Aged ≥ 80 y | 5.38** (2.19, 8.58) | Employed in construction | 3.72*** (2.53, 4.99) |
| 6 | Aged 65–79 y | 12.61** (4.35, 20.88) | Employed in construction | 5.07*** (2.69, 7.36) | Aged 0–17 y | 4.80** (2.03, 7.53) | Violent crime | 3.16*** (1.84, 4.48) |
| 7 | Aged 45–64 y | 12.01** (4.99, 19.00) | Near poverty | 3.95* (0.31, 7.59) | Employed in construction | 3.64*** (1.66, 5.54) | Some college | 2.28*** (1.17, 3.39) |
| 8 | Employed in service | 10.73*** (5.77, 15.68) | Aged 0–17 y | 3.64* (0.51, 6.76) | Some college | 2.83** (1.11, 4.50) | Aged 18–24 y | 2.18*** (1.10, 3.25) |
| 9 | Mortgage delinquency | 9.27*** (4.56, 13.94) | Employed in service | 2.97** (0.82, 5.15) | PM2.5 | 2.21** (0.62, 3.69) | PM2.5 | 1.97*** (0.98, 3.08) |
| 10 | PM2.5 | 9.23*** (5.17, 13.28) | PM2.5 | 2.58** (0.62, 4.43) | Employed in service | 1.86* (0.03, 3.68) | Employed in farming | 0.34** (0.11, 0.57) |
| 11 | Employed in sales or administration | 5.36* (0.78, 9.93) | ||||||
Note. CI = confidence interval; PM2.5 = particulate matter with diameters ≤ 2.5 µg. Only statistically significant effects are shown. Ranking is on the basis of number of additional deaths. Lower ranking indicates a more detrimental effect (greater number of additional deaths). Reference categories for multivariate models: percentage bachelor’s degree or higher; management, business, financial operations, and professional occupations; aged 25–44 years; percentage White; poverty ≥ 200%. We calculated the poverty ratio using the federal poverty level standards specified by the Office of Management and Budget for 2000.
Listed from largest to smallest significant magnitude.
*P < .05; **P < .01; ***P < .001.
It is worth noting the variation in factors that appear influential on cause-specific deaths compared with factors that were associated with all-cause mortality. For example, mortgage delinquency and employment in sales and farming were significant predictors of cause-specific mortality but not of all-cause mortality. Also notable was the significant independent influence of the less traditionally examined community predictors such as air quality, mortgage delinquency, and violent crime. Although the difference in deaths was more modest than was that for county age and socioeconomic characteristics, fine PM was associated with each of the 4 cause-specific deaths we examined. Counties at the 75th percentile for mortgage delinquencies and violent crime were associated with more deaths owing to heart disease and stroke, respectively. However, these 2 indicators did not significantly contribute to deaths for the other causes.
Community Characteristics and Lower Cause-Specific Mortality
Most of the statistically significant associations with cause-specific mortality were detrimental, but several sociodemographic characteristics were associated with lower mortality rates (Table 4). A higher percentage of Hispanic residents was associated with fewer deaths for all conditions, except heart disease.
TABLE 4—
The Estimated Reduction in Death per 100 000 Persons (5-Year Average, 1998–2002) for Selected Leading Causes of Death for Difference From 25th to 75th Percentile of County Characteristics in 2000: US Counties With Population ≥ 100 000
| Cancer |
Respiratory Conditions |
Stroke |
||||
| Ranka | Characteristic | Estimate, % (95% CI) | Characteristic | Estimate, % (95% CI) | Characteristic | Estimate, % (95% CI) |
| 1 | Married | −12.60*** (−15.47, −9.64) | Married | −11.24*** (−13.78, −8.71) | Hispanic | −2.62*** (−3.46, −1.77) |
| 2 | Hispanic | −6.24*** (−7.76, −4.73) | Black | −8.16*** (−10.27, −5.91) | Mortgage delinquency | −1.24* (−2.40, −0.08) |
| 3 | Asian | −1.17*** (−1.76, −0.59) | Hispanic | −4.73*** (−5.99, −3.38) | ||
| 4 | Asian | −0.98*** (−1.49, −0.46) | ||||
Note. CI = confidence interval. Only statistically significant effects are shown. Ranking is on the basis of the number of fewer deaths. Lower ranking indicates more protective effect (more deaths averted). No significant factor is found for heart disease. Reference categories for regression models are percentage bachelor’s degree or higher; management, business, financial operations, and professional occupations; younger than 65 years; percentage White; poverty ≥ 200%.
Listed from largest to smallest significant magnitude.
*P < .05; **P < .01; ***P < .001.
Counties with higher percentages of married residents and Asian residents had fewer deaths from cancer and respiratory conditions, whereas counties with higher percentages of Black residents had fewer deaths owing to respiratory conditions. One unexpected finding was the association of greater mortgage delinquency rates with reduced stroke mortality, although the statistical significance of this effect (P = .04) was not as strong as were the other predictors.
DISCUSSION
We have described the relative strength of the independent associations of a diverse set of county-level characteristics with mortality. We observed the expected strong links of mortality rates with county demographic and socioeconomic characteristics. The percentages of elderly residents older than 65 years and of the near poor were the top predictors of all-cause mortality. The proportion of residents with less than a high school education, aged 45 to 64 years, or employed in construction also demonstrated a substantial, but more modest, association with all-cause mortality. The associations between air quality, mortgage delinquencies, and violent crimes were significant but among the weakest of the county characteristics we examined. We observed similar results with condition-specific mortality, with strong associations of older age and lower socioeconomic status and weaker, but significant, associations for air quality, mortgage delinquencies, and violent crime. Higher percentages of Hispanics, Asians, and married residents were generally protective, with significant associations with reduced mortality observed for both all-cause and cause-specific mortality.
After age, county socioeconomic characteristics exhibited the strongest association with mortality. Education demonstrated the expected relationship with mortality, with lower educational attainment associated with greater numbers of deaths. Selected occupations are also linked with higher mortality. Counties with higher percentages of construction workers had consistently greater all-cause and condition-specific mortality. Employment in service, sales, or farming also had a significant association with mortality, although these associations were weaker and less consistent than was the association with employment in construction. Previous research suggests that the link between occupation and mortality derives from the risks and exposures associated with specific occupations.
The numerous dangers directly associated with construction work, including falls, are well documented in the literature.17–19 Furthermore, construction workers are often exposed to hazardous materials and chemicals, which pose longer-term risks to mortality from cancer20 and respiratory diseases.21 The greater mortality associated with a greater concentration of service and sales or office workers may be linked to hazards associated with subcategories of these occupations. For example, protective services, which include firefighting and law enforcement, are inherently dangerous occupations.22 Wholesale and retail workers are often at a higher risk of death from traffic accidents and assaults and violent acts, with highest fatality rates at gasoline stations, convenience stores, and used car dealerships.23 Aside from occupation-related exposures, sales or office and service workers, respectively, had 24 and 43 higher adjusted odds of being current smokers than did professional and management occupations,24 which may contribute to their association with condition-specific mortality.
It is surprising that the percentage of the near poor (100%–200% federal poverty level) but not the percentage of the poor (< 100% federal poverty level) was associated with greater mortality. However, this finding may reflect the fragility of the health and social services safety net for the working poor. Programs such as food stamps, housing subsidies, and Medicaid increase health care access25 and provide needed support for the poorest and most vulnerable.26 However, the near poor have not been as well supported.27 Many low-wage and part-time workers lack employer-based health insurance and other benefits28 but do not qualify for such programs as Medicaid and state-supported child care.29
The burden of cost sharing and the lack of affordable coverage options for these workers have contributed to reduced utilization of preventive services and poorer medication adherence even among the insured.30–32 Furthermore, the lack of affordable housing and the instability of low-wage employment33,34 likely create chronic stress among the near poor that interacts with unhealthy behaviors to increase mortality risk.35 The Medicaid expansion under the Affordable Care Act should improve health access for the near poor in participating states, which can in turn improve health outcomes and reduce mortality risks. However, more comprehensive measures, such as “living wage” legislation,36 are needed to address the higher mortality risk observed in counties with large proportions of the near poor.
Few studies have simultaneously modeled community-level air quality, public safety, and financial distress after controlling for a robust set of demographic and socioeconomic characteristics. Our findings indicate that the associations of these characteristics with mortality are independent but weaker than are those for county demographic and socioeconomic characteristics. Our results are broadly consistent with the literature. Numerous studies have already linked fine PM to greater all-cause mortality and cardiovascular and respiratory outcomes.37–40 Rettenmaier and Wang used the County Health Ranking data set to examine county-level associations of 24 behavioral, clinical care, socioeconomic, and environmental factors with mortality.41 The authors also identified significant effects of violent crime with premature mortality. However, their study, which used a different definition of air quality (i.e., number of unhealthy days) and included numerous county-level behavioral factors, did not find, as we did, a relationship between fine PM and premature mortality.
The relationship between community-level financial distress and mortality has not been well studied. The few existing studies, grounded on individual-level analyses, have reported poorer health, including nonadherence to treatment, greater odds of no insurance, and higher prevalence of hypertension, heart disease, and depression and lower self-rated health among individuals experiencing debt-related strain.8–11 Our study suggests mortgage-related distress is also associated with deaths owing to heart disease at the county level.
Although the ecological associational design of our study precludes causal inference, we were able to describe the relative strength of the associations for a diverse set of county-level characteristics on all-cause and condition-specific mortality. Our study confirms the expected importance of county demographic and socioeconomic characteristics. However, we also highlighted the independent association of fine PM, community violence, and mortgage distress with important mortality outcomes. These variables are rarely examined jointly with community demographic and socioeconomic characteristics. Our results highlight the need for studies that investigate factors from separate lines of research to better understand the key drivers of community mortality risk.
Acknowledgments
This study was made possible by a grant from a large US insurer.
We thank Gerard Andersen for helpful comments on an earlier draft of the article.
Human Participant Protection
The Johns Hopkins Bloomberg School of Public Health institutional review board reviewed and approved the study protocol.
References
- 1.Gebreab SY, Diez Roux AV. Exploring racial disparities in CHD mortality between Blacks and Whites across the United States: a geographically weighted regression approach. Health Place. 2012;18(5):1006–1014. doi: 10.1016/j.healthplace.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greer S, Casper M, Kramer M et al. Racial residential segregation and stroke mortality in Atlanta. Ethn Dis. 2011;21(4):437–443. [PubMed] [Google Scholar]
- 3.Major JM, Doubeni CA, Freedman ND et al. Neighborhood socioeconomic deprivation and mortality: NIH–AARP diet and health study. PLoS ONE. 2010;5(11):e15538. doi: 10.1371/journal.pone.0015538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galea S, Tracy M, Hoggatt KJ, Dimaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101(8):1456–1465. doi: 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bell ML, Peng RD, Dominici F, Samet JM. Emergency hospital admissions for cardiovascular diseases and ambient levels of carbon monoxide: results for 126 United States urban counties, 1999–2005. Circulation. 2009;120(11):949–955. doi: 10.1161/CIRCULATIONAHA.109.851113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bell ML, McDermott A, Zeger SL, Samet JM, Dominici F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA. 2004;292(19):2372–2378. doi: 10.1001/jama.292.19.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peng RD, Bell ML, Geyh AS et al. Emergency admissions for cardiovascular and respiratory diseases and the chemical composition of fine particle air pollution. Environ Health Perspect. 2009;117(6):957–963. doi: 10.1289/ehp.0800185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pollack CE, Lynch J. Health status of people undergoing foreclosure in the Philadelphia region. Am J Public Health. 2009;99(10):1833–1839. doi: 10.2105/AJPH.2009.161380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cannuscio CC, Alley DE, Pagán JA et al. Housing strain, mortgage foreclosure, and health. Nurs Outlook. 2012;60(3):134–142. doi: 10.1016/j.outlook.2011.08.004. 142.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alley DE, Lloyd J, Pagán JA, Pollack CE, Shardell M, Cannuscio C. Mortgage delinquency and changes in access to health resources and depressive symptoms in a nationally representative cohort of Americans older than 50 years. Am J Public Health. 2011;101(12):2293–2298. doi: 10.2105/AJPH.2011.300245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drentea P, Lavrakas PJ. Over the limit: the association among health, race and debt. Soc Sci Med. 2000;50(4):517–529. doi: 10.1016/s0277-9536(99)00298-1. [DOI] [PubMed] [Google Scholar]
- 12. US Environmental Protection Agency. AirData website download data page. 2013. Available at: http://www.epa.gov/airquality/airdata/ad_data.html. Accessed October 2, 2013.
- 13. Federal Bureau of Investigation. Uniform Crime Reporting Program data [United States]: county-level detailed arrest and offense data. 2000. Available at: https://www.icpsr.umich.edu/icpsrweb/NACJD/studies/3451. Accessed October 7, 2013.
- 14. Federal Reserve Bank of New York. Available at: http://www.newyorkfed.org/research/national_economy/householdcredit/county_report_by_year.xlsx. Accessed October 2, 2013.
- 15.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8(1):3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 16.Marchenko Y. Multiple-imputation analysis using Stata’s MI command. 2009. Available at: http://biostat.mc.vanderbilt.edu/wiki/pub/Main/QingxiaChen/MI_stata.pdf. Accessed June 30, 2013.
- 17.van der Molen HF, Lehtola MM, Lappalainen J et al. Interventions to prevent injuries in construction workers. Cochrane Database Syst Rev. 2012;12:CD006251. doi: 10.1002/14651858.CD006251.pub3. [DOI] [PubMed] [Google Scholar]
- 18.Jackson SA, Loomis D. Fatal occupational injuries in the North Carolina construction industry, 1978–1994. Appl Occup Environ Hyg. 2002;17(1):27–33. doi: 10.1080/104732202753306122. [DOI] [PubMed] [Google Scholar]
- 19.Janicak CA. Occupational fatalities due to electrocutions in the construction industry. J Safety Res. 2008;39(6):617–621. doi: 10.1016/j.jsr.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Rachiotis G, Drivas S, Kostikas K, Makropoulos V, Hadjichristodoulou C. Respiratory tract mortality in cement workers: a proportionate mortality study. BMC Pulm Med. 2012;12:30. doi: 10.1186/1471-2466-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bang KM, Weissman DN, Wood JM, Attfield MD. Tuberculosis mortality by industry in the United States, 1990–1999. Int J Tuberc Lung Dis. 2005;9(4):437–442. [PubMed] [Google Scholar]
- 22.Fronczek P, Johnson P. Occupations: 2000. Census Bureau brief C2KBR-25. 2003. Available at: http://www.census.gov/prod/2003pubs/c2kbr-25.pdf. Accessed May 29, 2014.
- 23.Anderson VP, Schulte PA, Sestito J, Linn H, Nguyen LS. Occupational fatalities, injuries, illnesses, and related economic loss in the wholesale and retail trade sector. Am J Ind Med. 2010;53(7):673–685. doi: 10.1002/ajim.20813. [DOI] [PubMed] [Google Scholar]
- 24.Chahine T, Subramanian SV, Levy JI. Sociodemographic and geographic variability in smoking in the U.S.: a multilevel analysis of the 2006–2007 Current Population Survey, Tobacco Use Supplement. Soc Sci Med. 2011;73(5):752–758. doi: 10.1016/j.socscimed.2011.06.032. [DOI] [PubMed] [Google Scholar]
- 25.Long SK, Coughlin T, King J. How well does Medicaid work in improving access to care? Health Serv Res. 2005;40(1):39–58. doi: 10.1111/j.1475-6773.2005.00341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ratcliffe C, McKernan S-M, Zhang S. How much does the Supplemental Nutrition Assistance Program reduce food insecurity? Am J Agric Econ. 2011;93(4):1082–1098. doi: 10.1093/ajae/aar026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu C-F, Eamon MK. Need for and barriers to accessing public benefits among low-income families with children. Child Youth Serv Rev. 2010;32(1):58–66. [Google Scholar]
- 28.Bernstein J, Hartmann H. The Low-Wage Labor Market: Challenges and Opportunities for Economic Self-Sufficiency. Washington, DC: Urban Institute; 1999. Defining and characterizing the low-wage labor market; pp. 17–39. [Google Scholar]
- 29.Hildebrandt E, Stevens P. Impoverished women with children and no welfare benefits: the urgency of researching failures of the Temporary Assistance for Needy Families Program. Am J Public Health. 2009;99(5):793–801. doi: 10.2105/AJPH.2006.106211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guy GP., Jr The effects of cost sharing on access to care among childless adults. Health Serv Res. 2010;45(6, pt 1):1720–1739. doi: 10.1111/j.1475-6773.2010.01162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng T. Leaving Medicaid without health insurance: TANF policies and recipients’ vulnerabilities. J Health Care Poor Underserved. 2007;18(3):609–619. doi: 10.1353/hpu.2007.0056. [DOI] [PubMed] [Google Scholar]
- 32.Fung V, Reed M, Price M et al. Responses to Medicare drug costs among near-poor versus subsidized beneficiaries. Health Serv Res. 2013;48(5):1653–1668. doi: 10.1111/1475-6773.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Quigley JM, Raphael S. Is housing unaffordable? Why isn’t it more affordable? J Econ Perspect. 2004;18(1):191–214. [Google Scholar]
- 34.Stewart MB. The interrelated dynamics of unemployment and low-wage employment. J Appl Econ. 2007;22(3):511–531. [Google Scholar]
- 35.Krueger PM, Chang VW. Being poor and coping with stress: health behaviors and the risk of death. Am J Public Health. 2008;98(5):889–896. doi: 10.2105/AJPH.2007.114454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhatia R, Katz M. Estimation of health benefits from a local living wage ordinance. Am J Public Health. 2001;91(9):1398–1402. doi: 10.2105/ajph.91.9.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Puett RC, Hart JE, Yanosky JD et al. Chronic fine and coarse particulate exposure, mortality, and coronary heart disease in the Nurses’ Health Study. Environ Health Perspect. 2009;117(11):1697–1701. doi: 10.1289/ehp.0900572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eftim SE, Samet JM, Janes H, McDermott A, Dominici F. Fine particulate matter and mortality: a comparison of the six cities and American Cancer Society cohorts with a Medicare cohort. Epidemiology. 2008;19(2):209–216. doi: 10.1097/EDE.0b013e3181632c09. [DOI] [PubMed] [Google Scholar]
- 39.Pope CA, 3rd, Burnett RT, Thurston GD et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109(1):71–77. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- 40.Pope CA, III, Burnett RT, Thun MJ et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287(9):1132–1141. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rettenmaier AJ, Wang Z. What determines health: a causal analysis using county level data. Eur J Health Econ. 2013;14(5):821–834. doi: 10.1007/s10198-012-0429-0. [DOI] [PubMed] [Google Scholar]


