Abstract
Objectives. We evaluated the effect of a weight gain prevention intervention (Shape Program) on depression among socioeconomically disadvantaged overweight and obese Black women.
Methods. Between 2009 and 2012, we conducted a randomized trial comparing a 12-month electronic health–based weight gain prevention intervention to usual primary care at 5 central North Carolina community health centers. We assessed depression with the Patient Health Questionnaire (PHQ-8). We analyzed change in depression score from baseline to 12- and 18-month follow-up across groups with mixed models. We used generalized estimating equation models to analyze group differences in the proportion above the clinical threshold for depression (PHQ-8 score ≥ 10).
Results. At baseline, 20% of participants reported depression. Twelve-month change in depression scores was larger for intervention participants (mean difference = −1.85; 95% confidence interval = −3.08, −0.61; P = .004). There was a significant reduction in the proportion of intervention participants with depression at 12 months with no change in the usual-care group (11% vs 19%; P = .035). All effects persisted after we controlled for weight change and medication use. We saw similar findings at 18 months.
Conclusions. The Shape Program, which includes no mention of mood, improved depression among socioeconomically disadvantaged Black women.
Depression is one of the most common and disabling, yet treatable, mental health conditions in the United States.1,2 Women are twice as likely as men to be affected,3 and more than 1 in 7 (14.9%) Black women will experience major depression in their lifetime.4 Observational evidence suggests that, although the prevalence of major depression is lower among Blacks than Whites, its severity is greater for Blacks.5 This is likely a result of racial disparities in access to depression treatment.6 Indeed, compared with their White counterparts, Black adults with depression are less likely to receive treatment for depression (39.7% vs 54.0%).6 Of those who do seek treatment, Blacks are less likely than Whites to receive care that corresponds to clinical practice guidelines.6,7 These racial disparities are magnified by socioeconomic disadvantage.8 Depression is 3 times more common for those with incomes below the federal poverty level, compared with those with higher incomes.9 As a consequence, the challenge remains how to effectively treat socioeconomically disadvantaged Black women with depression.
Obesity is also disproportionately prevalent among Black women relative to other racial/ethnic groups.10 The high burden of obesity among Black women not only indicates a higher prevalence of obesity-related chronic diseases (e.g., diabetes, heart disease),11 but it may also have an impact on psychosocial outcomes such as depression.12 As such, interventions focusing on behavioral weight control may present a useful opportunity to address both obesity and depression.
Behavioral weight loss interventions typically include frequent contact with a weight loss counselor; self-monitoring of diet, exercise, and weight; and lessons that cover various topics such as problem solving, relapse prevention, and stress management. Indeed, across numerous studies, behavioral weight loss interventions have been shown to promote reductions in depression.13,14 Such findings are generally believed to be related to weight loss15 and mediated by improvements in body satisfaction; that is, for many, weight loss might enhance body satisfaction and, thus, improve depression outcomes.16,17 However, this finding has most frequently been demonstrated in predominantly socioeconomically advantaged White women, who tend to exhibit strong relations between body size and mood.16,18 In contrast, Black women have greater social acceptance of overweight, less body weight dissatisfaction, and higher body weight ideals compared with White women.19–22 Thus, it is unclear whether Black women would experience a similar reduction in depression as a result of obesity treatment.
Although weight loss is indicated for those with obesity, promoting clinically meaningful weight change among Black women has been a major challenge.23 Across various studies, Black women achieve less weight loss relative to White women.24–26 The reason for this racial disparity in weight loss outcomes is unclear, but may be influenced in part by differences in sociocultural norms related to weight, diet, and physical activity.27 As a result, interventions that focus on preventing weight gain may be a useful alternative treatment approach among overweight and obese Black women.27
We recently conducted a study titled the Shape Program, a 12-month randomized controlled trial with follow-up at 18 months, evaluating an electronic health weight gain prevention intervention among Black women compared with usual care in the primary care setting.27 The Shape intervention was found to be effective in staving off weight gain at 12 and 18 months.28 It is unclear whether a weight gain prevention approach, as was tested in Shape, would be helpful for treating depression among Black women. As such, we sought to examine the potential spillover benefits produced by this “maintain, don’t gain” approach on depression, compared with usual care.
METHODS
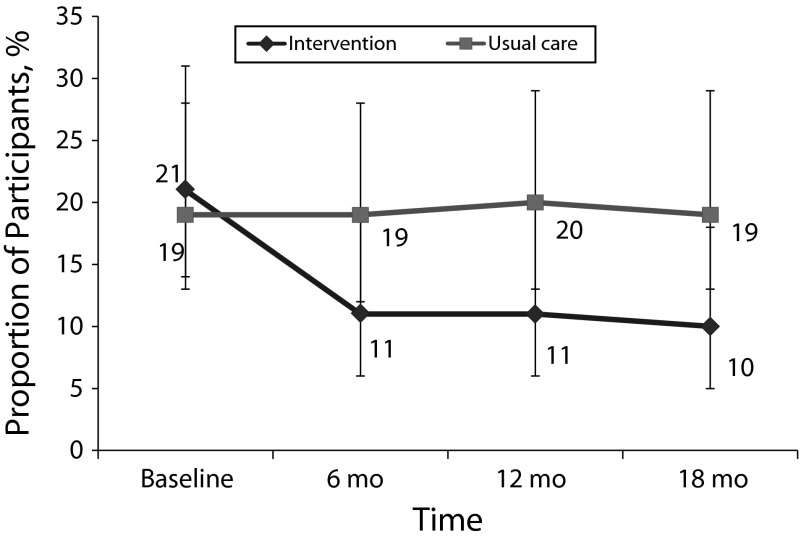
As described elsewhere,27 the Shape Program was a randomized controlled trial that compared a 12-month weight gain prevention intervention to usual care in the primary care setting. Following eligibility screening and baseline measures, we randomized participants (n = 194) to the Shape intervention (n = 97) or to usual care (n = 97). As shown in Figure 1, we excluded 9 participants after randomization. We re-evaluated all remaining participants (n = 185) at 6 and 12 months, with an additional follow-up visit at 18 months after randomization (Figure 1).
FIGURE 1—
Participant enrollment and retention in the Shape Program vs usual care among overweight and obese Black women in North Carolina community health centers: 2009–2012.
Participants
Eligibility criteria included Black women, aged 25 to 44 years, with a body mass index (BMI; defined as weight in kilograms divided by the square of height in meters [kg/m2]) of 25 to 34.9 kg/m2. We recruited participants from 5 community health centers operated by Piedmont Health Inc (PHS), a federally qualified community health center system that serves predominantly socioeconomically disadvantaged patients in central North Carolina. Additional inclusion criteria consisted of at least 1 visit to a Piedmont Health center in the previous 24 months and the ability to read and write in English.
Exclusion criteria included current pregnancy, being less than 12 months postpartum, a history of myocardial infarction or stroke in the previous 2 years, and profound cognitive, developmental, or psychiatric disorders (Axis II–III). As assessed by the electronic health record, exclusion for cognitive or psychiatric disorders included schizophrenia, bipolar disorder, borderline personality disorder, developmental delay or brain trauma.
Intervention
The Shape Program intervention has been described in detail elsewhere.27,28 Briefly, the year-long intervention included 5 primary components:
1. 3 personally tailored behavior change goals,
2. self-monitoring of these goals via weekly interactive voice response phone calls,
3. tailored skills training materials,
4. 12 monthly individual counseling calls with a registered dietitian, and
5. a 12-month YMCA membership.
The intervention was designed to achieve weight gain prevention. As such, we did not recruit those with high weight loss motivation, and intervention messages did not mention weight loss; rather, the primary intervention message concerned maintaining one’s weight and shape.
The intervention was delivered remotely and utilized the Interactive Obesity Treatment Approach,29–31 which uses a computer algorithm to prescribe a series of behavior change goals (e.g., 5 or more fruits and vegetables per day, no fast food, no sugar-sweetened beverages, walking 10 000 steps per day). The intervention emphasized achieving the behavioral goals as a means of creating a small caloric deficit to stave off weight gains. The algorithm considers self-efficacy, readiness, and the potential of the goal to produce a caloric deficit. We assigned 3 goals at baseline and updated them every 2 months. All intervention participants received walking up to 10 000 steps per day as one of their goals. Participants self-monitored their adherence to the behavior change goals on weekly, 2- to 4-minute, automated, interactive voice response telephone calls that were issued by a computer database. After self-monitoring, participants received immediate, automated feedback regarding their progress and skills training tips from the interactive voice response system. Self-monitoring data, in part, informed the monthly coaching calls that were conducted by PHS registered dietitians. The 20-minute coaching calls used principles of motivational interviewing to help elicit patient-directed motivation for meeting behavioral goals.
Usual care group participants received routine standard of care for obesity from providers at PHS. Usual care group participants also received semiannual newsletters that covered health topics other than weight, nutrition, or physical activity. They also received the National Heart, Lung, and Blood Institute’s “Aim for a Healthy Weight” brochure at the baseline visit. Otherwise, we made no efforts to impact their weight, or the care they received in the health center.
Measures
We assessed depression by using the 8-item Patient Health Questionnaire (PHQ-8).32 The PHQ-8 reflects the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for depression33 and was initially developed for use in primary care.34 The PHQ-8 has been tested in diverse samples and has been shown to be a valid measure for depression in various racial/ethnic populations.35 This questionnaire uses a 4-point Likert scale and asks the frequency, within the past 2 weeks, with which a respondent has experienced depressive symptoms. Response options range from “not at all” to “nearly every day” with values of 0 to 3 assigned to each response. Examples of symptoms include “feeling down,” “depressed or hopeless,” “poor appetite,” and “little interest or pleasure in doing things.” We calculated total scores, which ranged from 0 to 24. Scores of 10 and above on the PHQ-8 reflect moderate to severe depression and have 88% sensitivity and 88% specificity for predicting a major depression diagnosis.32,34 Scores greater than or equal to 15 reflect more severe depression. Reductions from the clinical threshold of PHQ-8 of 10 and higher to scores of less than 5 are thought to reflect remission in depression.34 Likewise, achieving at least a 5-point reduction in PHQ-8 score among those with depression (PHQ-8 ≥ 10) is considered clinically meaningful.36
Trained staff measured participant heights to the nearest 0.1 centimeter by using a calibrated wall-mounted stadiometer (Seca model 214, Hamburg, Germany).37 They measured weights to the nearest 0.1 kilogram with an electronic scale (Seca model 876, Hamburg, Germany).37
At 18 months, we collected self-reported medication use (i.e., “In the past 18 months, has a doctor or medical professional prescribed a medication for you? If yes, which medication(s)?”). We coded any self-reported use of tricyclic antidepressants, monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, or serotonin and norepinephrine reuptake inhibitors as depression medication use. Although we only collected medication data at 18 months, we assumed that medication use was stable throughout the study period.
Statistical Analysis
We used χ2 and analysis of variance models to examine differences in baseline characteristics and attrition between treatment arms. We calculated the proportion of participants with PHQ-8 scores greater than or equal to 10 and greater than or equal to 15. We imputed up to 1 missing PHQ-8 item by using the mean of the participant’s other 7 items. If a participant was missing more than 1 item on the PHQ-8, we set the total score for that observation to missing at random. To examine the effect of treatment group on continuous outcomes over time, we conducted intent-to-treat analyses by using linear mixed models with random intercept and maximum likelihood estimates. We used generalized estimating equation models to examine group differences over time for dichotomous outcomes. For both approaches, we included all participants, with the assumption that missing values were missing at random.
We also tested the same models, with control for weight change and medication use, to determine the effect of the treatment on depression beyond any effect that is attributable to change in weight and medication use. We conducted all analyses in 2013 with SPSS version 19 for Mac (IBM, Somers, NY), with an α < 0.05 to assess statistical significance.
RESULTS
Baseline characteristics have been reported in detail elsewhere.27,28 Briefly, participants (n = 185) had a mean age of 35.4 (±5.5) years and most (80%) had less than a college degree. The majority (71%) were currently employed and 74% reported an annual income of less than $30 000. At baseline, 20% reported depressive symptomatology consistent with moderate to severe depression and 10% with more severe depression (Table A, available as a supplement to the online version of this article at http://www.ajph.org). There were no significant differences in baseline characteristics between study groups. We retained 96% of participants at 12 months and 18 months after randomization (Figure 1), and there were no statistically significant differences in attrition between groups.
Shape Program study outcomes have been presented in detail elsewhere.28 Relative to usual care, the intervention was successful in mitigating weight gain over 12 months (−0.97 ±0.51 kg vs 0.48 ±0.49 kg; mean difference = −1.45 kg; 95% confidence interval [CI] = −2.84, 0.05; P = .04) and 18 months (−0.91 ±0.58 kg vs 0.83 ±0.55 kg; mean difference = −1.74 kg; 95% CI = −3.31, 0.15; P = .03) after randomization. In addition, at 12 months, a larger proportion of intervention participants (62%) were at or below their baseline weight, compared with those in usual care (45%; P = .02). We observed similar findings at 18 months,28 when 12% (n = 23) of all participants reported taking any depression medication over the past 18 months—14 participants in the usual care group and 9 participants in the intervention group.
Baseline sociodemographic characteristics among all participants by depression status at baseline are reported in Table 1. Compared with those without, participants with moderate to severe depression (PHQ-8 ≥ 10) had significantly higher PHQ-8 total scores (mean = 14.2; SD = 3.2 vs mean = 4.1; SD = 2.7; P < .001), were more obese (mean BMI = 31.2 kg/m2; SD = 2.5 vs mean BMI = 29.9 kg/m2; SD = 2.5; P = .004) and had lower levels of employment (55.3% vs 75.5%; P = .01). Almost half of participants (48.7%) with depression reported an annual household income less than $10 000, compared with 13% of those without (P < .001). Similarly, one third (32.4%) of those with depression had less than high-school education compared with only 4.9% among those without (P < .001).
TABLE 1—
Baseline Characteristics of Study Participants by Baseline Depression Status in the Shape Program vs Usual Care Among Overweight and Obese Black Women in North Carolina Community Health Centers: 2009–2012
| Characteristics | PHQ-8 ≥ 10 (n = 38),a No. (%) or Mean ±SD | PHQ-8 < 10 (n = 146),a No. (%) or Mean ±SD | P |
| Age, y | 35.45 ±5.42 | 35.35 ±5.51 | .92 |
| Body mass index, kg/m2 | 31.22 ±2.45 | 29.90 ±2.49 | .004 |
| Depression symptoms, total score | 14.2 ±3.2 | 4.1 ±2.7 | < .001 |
| Household income per year, $ | < .001 | ||
| < 10 000 | 18 (48.7) | 19 (13.1) | |
| 10 000–19 999 | 8 (21.6) | 44 (30.3) | |
| 20 000–29 999 | 8 (21.6) | 38 (26.2) | |
| ≥ 30 000 | 3 (8.1) | 44 (30.3) | |
| Education | < .001 | ||
| < high school | 12 (32.4) | 7 (4.9) | |
| High school | 7 (18.9) | 37 (25.7) | |
| Vocational or trade school after high school | 3 (8.11) | 13 (9.0) | |
| Some college | 13 (35.1) | 52 (36.1) | |
| ≥ college | 2 (5.41) | 35 (24.3) | |
| Employment status | .01 | ||
| Employed | 21 (55.3) | 108 (75.5) | |
| Not employed | 17 (44.7) | 35 (24.5) | |
| Marital status | .15 | ||
| Married | 6 (16.7) | 41 (28.5) | |
| Not married | 30 (83.3) | 103 (71.5) |
Note. PHQ-8 = 8-item Patient Health Questionnaire.
Subgroup numbers may not sum to sample total because of missing data.
As shown in Table 2, relative to the usual care group, participants randomized to the intervention reported significantly greater changes in depression at 6 months (−1.74 ±0.45 vs −0.43 ±0.44; mean difference = −1.31; 95% CI = −2.55, −0.08; P = .04), 12 months (−2.23 ±0.45 vs −0.38 ±0.44; mean difference = −1.85; 95% CI = −3.08, −0.61; P = .004), and 18 months (−2.21 ±0.45 vs −0.42 ±0.44; mean difference = −1.79; 95% CI = −3.02, −0.55; P = .005). These effects, although attenuated, persisted even after adjustment for weight change and medication use at 12 and 18 months (Table 2).
TABLE 2—
Change in 8-Item Patient Health Questionnaire Score by Study Group (N = 185) in the Shape Program vs Usual Care Among Overweight and Obese Black Women in North Carolina Community Health Centers: 2009–2012
| Change From Baseline, Mean (SE) or Mean (95% CI) |
||||
| Outcome Variable and Group | Baseline Score, Mean (SE) or Mean (95% CI) | 6 Months | 12 Months | 18 Months |
| Total PHQ-8 score (unadjusted model) | ||||
| Intervention | 6.23 (0.49) | –1.74 (0.45) | –2.23 (0.45) | –2.21 (0.45) |
| Usual care | 6.15 (0.48) | –0.43 (0.44) | –0.38 (0.44) | –0.42 (0.44) |
| Difference between armsa | 0.08 (–1.25, 1.42) | –1.31 (–2.55, –0.08) | –1.85 (–3.08, –0.61) | –1.79 (–3.02, –0.55) |
| Total PHQ-8 score (adjusted model)b | ||||
| Intervention | 7.48 (0.58) | –1.65 (0.46) | –2.17 (0.46) | –2.13 (0.45) |
| Usual care | 7.15 (0.55) | –0.49 (0.44) | –0.47 (0.44) | –0.56 (0.44) |
| Difference between armsa | 0.33 (–1.00, 1.66) | –1.16 (–2.41, 0.09) | –1.71 (–2.96, –0.46) | –1.57 (–2.81, –0.33) |
Note. CI = confidence interval; PHQ-8 = 8-item Patient Health Questionnaire.
Adjusted for weight change and medication use.
95% CIs that do not include zero indicate statistical significance at the P < .05 level.
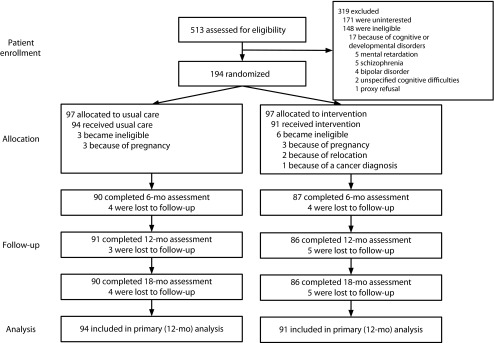
In a similar way, the intervention led to a reduction in the proportion of participants above the moderate severity clinical threshold (PHQ-8 ≥ 10; Figure 2). At baseline, 19% (n = 18) of intervention participants and 21% (n = 20) of usual care participants reported moderate to severe depression. At 12 months, a significantly smaller proportion of intervention participants were at or above that threshold, compared with those in usual care (11% vs 19%; P = .035). This equates to an almost 50% reduction in the proportion of intervention participants with moderate to severe depression, with no meaningful change among the usual care group. Intervention effects on depression were maintained at 18 months with fewer participants in the intervention reporting depression relative to controls (10% vs 19%; P = .039). The effect of the intervention on the proportion of participants with depression persisted even after we adjusted for weight change and medication use (data not shown).
FIGURE 2—
Change in proportion with moderate to severe depression by treatment arm among overweight and obese Black women in North Carolina community health centers: 2009–2012.
Few participants (n = 18) in either arm reported severe depression, defined as PHQ-8 greater than or equal to 15. At baseline, 9% of intervention and 10% of usual care participants were above this threshold. There were no significant differences between arms in the proportion of participants over time with severe depression (PHQ ≥ 15). However, within the intervention arm, the proportion of severely depressed patients dropped from 9% at baseline to 1% at 6 months (P = .03) and 2% at both 12 months (P = .06) and 18 months (P = .06). There was no significant change over time within the usual-care arm. We also examined group differences in depression remission (PHQ-8 < 5 at follow-up) among those above the clinical threshold for moderate to severe depression (PHQ-8 ≥ 10) at baseline. At 6 months, a significantly larger proportion of intervention participants (40%) achieved depression remission than those in usual care (0%; P = .004). This trend continued at 12 months (47% vs 18%; P = .083) and 18 months (50% vs 18%; P = .075) after randomization.
We further explored group differences in PHQ-8 score among those with depression at baseline (n = 38) and similarly found greater changes in depression among intervention participants relative to usual care at 6 months (−6.30 ±1.12 vs −2.16 ±1.28; mean difference = −4.14; 95% CI = −7.61, −0.68; P = .02), 12 months (−7.25 ±1.23 vs −4.25 ±1.28; mean difference = −3.00; 95% CI = −6.52, 0.51; P = .09), and 18 months (−7.95 ±1.23 vs −3.32 ±1.30; mean difference = −4.64; 95% CI = −8.19, −1.09; P = .01). All effects persisted among those with baseline depression after we adjusted for weight change and medication use.
DISCUSSION
We found that a 12-month weight gain prevention intervention produced large reductions in depression among socioeconomically disadvantaged, obese Black women, relative to usual care. At baseline, approximately 20% of participants in both groups reported experiencing symptoms consistent with moderate to severe depression. At both 12 months and 18 months, only 10% and 11% of intervention participants reported experiencing these symptoms, while the usual care group exhibited no change. Weight change did not explain the impact of the intervention on depression outcomes among Shape participants. It was also potentially evident irrespective of self-reported depression medication use. Among those with depression at baseline, we found large effect sizes and clinically meaningful changes among intervention participants.
These findings are notable for several reasons. Levels of baseline depression in Shape (20%) were larger than those that have been historically observed in weight management trials. For example, 10.3% of participants in the Diabetes Prevention Program (DPP)38 and 17.5% in the Look AHEAD Study14 reported baseline depression. These lower levels of depression are surprising because these trials were comprised primarily of obese White women who are often found to have higher rates of depression than their obese Black female counterparts.39,40 The higher prevalence of depression in our study might be attributable to our somewhat less restrictive mental health exclusion criteria compared with these trials; however, it is more likely a result of greater strain and stress experienced in this population41 because of greater socioeconomic disadvantage.8 Indeed, we found that participants who reported moderate to severe depression at baseline had lower rates of employment and education, and lower annual household income than those who were not depressed. It was interesting that we found that the depressed were also more obese. This finding is consistent with some previous observational evidence indicating that obese Black women have greater depression than normal-weight Black women.42
Both the DPP and Look AHEAD trials reported similar improvements in depressive symptoms as was seen in Shape. However, drivers of the improvements in depression are inconsistent. Among DPP participants, antidepressant medication use increased over time, concurrent with reductions in depression.38 This suggests that improvements in depressive symptoms could be attributed to medication use, rather than to the DPP intervention. In the Look AHEAD trial, reductions in depression were associated with significantly greater weight loss within the intervention arm.14 As noted earlier, the common hypothesized mediator for the improvements in depression in the Look AHEAD trial is higher body satisfaction. In Shape, reductions in depression were independent of weight change, suggesting that the mediator of body satisfaction that explains changes in depression rates among predominantly White samples might not be a factor in explaining how the intervention reduced depression outcomes in Shape.
Regarding the effects of a weight control intervention in primary care setting, the POWER trial43 similarly evaluated the impact of a primary care–based weight loss intervention on depression, as measured by the PHQ-8.44 However, the population characteristics differed from those in Shape; POWER participants were more socioeconomically advantaged, predominantly White, and had a higher prevalence of chronic disease at baseline.43 In contrast to our findings, they found nonsignificant primary treatment effects on depression. After adjustment for weight change, they reported significantly less depression among control participants suggesting that weight change did not improve, but actually increased, depression outcomes among intervention participants. They speculated that this might have resulted from the burden associated with intervention participation or intervention participants’ lack of satisfactory weight loss results.44 Although Shape was also conducted in primary care, it was a weight gain prevention trial that did not emphasize weight loss; nevertheless, we still found improvements in depression outcomes that were sustained even after we controlled for weight change.
Although the Shape Program was effective at reducing depressive symptoms overall, the intervention included multiple components and our study design does not allow us to dismantle their independent effects on depression. However, we can speculate about potential mechanisms.
First, the Shape intervention was quite different from classic approaches to behavioral weight control. Behavioral weight control interventions have typically been conducted among more advantaged White populations that have a strong connection between mood and weight. These interventions are designed to address the role that emotions play in weight control and include topics such as addressing negative thoughts, problem solving, stress management, managing barriers, and relapse prevention.45 As a result, improvements in depressive symptoms might be expected if the intervention is successful in producing weight loss.
By contrast, Shape included a population that has been shown to have fewer connections between mood and weight. In fact, this “maintain, don’t gain” approach was designed specifically because members of this population often have a greater tolerance of overweight and class I obese body shapes.27 As a result, the intervention was intended to support participants’ efforts to maintain their current body shapes. Thus, weight loss was neither explicitly discussed nor encouraged. Moreover, despite the high prevalence of depression and socioeconomic strain at baseline, the intervention did not explicitly address topics such as stress management or problem solving that are common in other weight-control interventions and might be expected to exert an intervention effect on depression.
Second, it is possible that the attention directed to intervention participants might explain these findings. The Shape intervention offered participants’ support via monthly coaching calls with a PHS registered dietitian. Given the poor access to depression treatment generally experienced among socioeconomically disadvantaged populations like the women in Shape, it may be that contact in general was influential in reducing depression.
As previously reported, 82% of coaching calls were completed and there was no association between coaching call completion and weight change.28 However, we found an inverse association between coaching call completion and depression levels at both 6 months (Spearman r = −0.29; P = .006) and 12 months (Spearman r = −0.23; P = .034). Furthermore, depression scores at 6 months were marginally lower in the highest versus the lowest tertile of coaching call completion (mean difference = −2.46; 95% CI = −4.92, −0.001; P = .05). There were no significant differences at any time point between coaching call completion and the proportion of intervention participants with moderate to severe depression. The improvements in depression without concurrent weight losses or medication use suggest that the attention via the coaching calls may have driven our findings. In addition to general attention and contact, we hypothesize that the social support, skills building, and self-monitoring feedback received during these calls may have affected depression outcomes. This is supported by previous literature assessing the critical role of social support and contact in mental health treatment.46 This indicates that there is potential for low-intensity social support delivered via phone coaching to make a difference in lowering rates of depression in high-risk populations.
We further speculate that an increase in physical activity, which was emphasized in Shape, might partially explain the large reductions in depression. There is strong evidence linking physical activity with improvements in depression.47,48 In exploratory analyses, we did not find significant between-groups differences in physical activity as measured by accelerometry. In addition, we found that minutes of moderate to vigorous physical activity did not mediate the intervention effects on depression. Likewise, within the intervention arm, there were no differences in physical activity by depression status.
Finally, another possibility is that our intervention might have acted in a manner consistent with behavioral activation. Behavioral activation theory emphasizes the role of context on mood and posits that depression occurs when a person engages in passive behavior and avoids active situations that may be perceived as aversive.49,50 Treatment using behavioral activation focuses on evaluating environmental sources of depression51 and structuring daily activities to include those typically avoided.52 Thus, the intervention may have also prompted behavioral activation through goal attainment, which then led to a cascade effect on other behaviors. Similarly, some of the behavioral goals included changing personal environments. Achieving goals such as “no fast food” and “no more than 2 hours of TV each day” may have led to changes in both the external and home environments, which then activated additional behavior changes. Because this finding was unexpected, we did not include measures that allowed us to directly assess whether behavioral activation was driving the effects on depression. More work is needed to determine whether the changes brought on as a result of the intervention may have prompted behavioral activation and thus led to a reduction in depression.
Strengths and Limitations
Shape was conducted in the primary care setting among a socioeconomically disadvantaged population that has limited access to treatment of depression. Although this is a strength of this study, the findings may not generalize to other populations in different circumstances. Additional strengths include multiple measurements over an 18-month time period and the use of an experimental design, which allows for a better understanding of causal inference. We found that reductions in depression at 12 months were maintained through 18 months, suggesting maintenance of effects after treatment. That our findings are independent of weight change or depression medication use further strengthens the potential for an intervention effect on depression.
A limitation of this study is the use of a limited, self-report assessment of medication use. We collected medication data only at 18 months and our statistical models conservatively assumed that medication use was consistent at all evaluation points. This assumption may misclassify the interaction between medication use and intervention effect. Similarly, another potential limitation is that we did not measure or include the use of additional medications that might be associated with depression or obesity in the analysis. Although there was a trend toward an intervention effect on depression remission at 12 and 18 months, our limited sample size of those with depression at baseline (n = 38) likely limited our ability to detect significant differences between groups. An additional limitation is that we were not fully able to explain our findings through the exploratory analyses we conducted. Because the primary aim of this article was to examine group differences in depression outcomes, it is important for future studies to more robustly examine the potential mechanisms.
Conclusions
In summary, we found that a weight gain prevention intervention among socioeconomically disadvantaged Black women led to significant reductions in depressive symptoms over 12 and 18 months. To our knowledge, this is the first study to examine the spillover effects of a weight control intervention on depression among Black women. It was interesting that the magnitude of our study findings compare favorably with those of standard treatments for depression (e.g., counseling, medication).53,54 We found that, among Shape intervention participants with depression at baseline, 40% met the criteria for remission by 6 months and about half achieved remission by 12 and 18 months.
The clinical implications of these findings are unclear, but these data suggest that Shape has a broader set of clinical benefits, well beyond weight gain prevention. This is particularly important in a patient population that receives comparatively less treatment of depression, a finding that is magnified by the profound socioeconomic disadvantage. In light of increasing recognition of the value of patient-centered medical outcomes,55 it is possible that Shape’s ability to improve mood might be received more favorably by patients, likely because of fewer barriers such as lack of access to treatment or cost. More research is needed, however, to examine the potential impacts of a “maintain, don’t gain” weight-management approach on depression and other patient-centered outcomes.
Acknowledgments
This trial is funded by grant R01DK078798 from the National Institute for Diabetes and Digestive and Kidney Diseases. G. G. Bennett was supported by grant K22CA126992 from the National Cancer Institute.
We express deep gratitude to the administration and staff of Piedmont Health for their continued collaboration and participation in the Shape Program. Most importantly, we would especially like to thank the women who participated in Shape.
Human Participant Protection
The Duke University institutional review board and the Piedmont Health Board of Advisors approved all study procedures.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 4.McKnight-Eily LR, Presley-Cantrell L, Elam-Evans LD, Chapman DP, Kaslow NJ, Perry GS. Prevalence and correlates of current depressive symptomatology and lifetime diagnosis of depression in Black women. Womens Health Issues. 2009;19(4):243–252. doi: 10.1016/j.whi.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Williams DR, Gonzalez HM, Neighbors H et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and non-Hispanic Whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 6.González HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res. 2010;44(15):1043–1051. doi: 10.1016/j.jpsychires.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alegría M, Chatterji P, Wells K et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 9.Pratt LA, Brody DJ. Depression in the United States household population, 2005–2006. NCHS Data Brief. 2008;(7):1–8. [PubMed] [Google Scholar]
- 10.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 11.Field AE, Coakley EH, Must A et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161(13):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 12.Needham BL, Epel ES, Adler NE, Kiefe C. Trajectories of change in obesity and symptoms of depression: the CARDIA study. Am J Public Health. 2010;100(6):1040–1046. doi: 10.2105/AJPH.2009.172809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fabricatore AN, Wadden TA, Higginbotham AJ et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes (Lond) 2011;35(11):1363–1376. doi: 10.1038/ijo.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faulconbridge LF, Wadden TA, Rubin RR et al. One-year changes in symptoms of depression and weight in overweight/obese individuals with type 2 diabetes in the Look AHEAD study. Obesity (Silver Spring) 2012;20(4):783–793. doi: 10.1038/oby.2011.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foster GD, Wadden TA, Vogt RA. Body image in obese women before, during, and after weight loss treatment. Health Psychol. 1997;16(3):226–229. doi: 10.1037//0278-6133.16.3.226. [DOI] [PubMed] [Google Scholar]
- 16.Gavin AR, Simon GE, Ludman EJ. The association between obesity, depression, and educational attainment in women: the mediating role of body image dissatisfaction. J Psychosom Res. 2010;69(6):573–581. doi: 10.1016/j.jpsychores.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Markowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clin Psychol Sci Pract. 2008;15(1):1–20. [Google Scholar]
- 18.Simon GE, Ludman EJ, Linde JA et al. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008;30(1):32–39. doi: 10.1016/j.genhosppsych.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell AD, Kahn AS. Racial differences in women’s desires to be thin. Int J Eat Disord. 1995;17(2):191–195. doi: 10.1002/1098-108x(199503)17:2<191::aid-eat2260170213>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 20.Stevens J, Kumanyika SK, Keil JE. Attitudes toward body size and dieting: differences between elderly Black and White women. Am J Public Health. 1994;84(8):1322–1325. doi: 10.2105/ajph.84.8.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Striegel-Moore RH, Wilfley DE, Caldwell MB, Needham ML, Brownell KD. Weight-related attitudes and behaviors of women who diet to lose weight: a comparison of Black dieters and White dieters. Obes Res. 1996;4(2):109–116. doi: 10.1002/j.1550-8528.1996.tb00522.x. [DOI] [PubMed] [Google Scholar]
- 22.Flynn KJ, Fitzgibbon M. Body images and obesity risk among Black females: a review of the literature. Ann Behav Med. 1998;20(1):13–24. doi: 10.1007/BF02893804. [DOI] [PubMed] [Google Scholar]
- 23.Kumanyika SK, Gary TL, Lancaster KJ et al. Achieving healthy weight in African-American communities: research perspectives and priorities. Obes Res. 2005;13(12):2037–2047. doi: 10.1038/oby.2005.251. [DOI] [PubMed] [Google Scholar]
- 24.West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of Black, White, and Hispanic men and women in the Diabetes Prevention Program. Obesity (Silver Spring) 2008;16(6):1413–1420. doi: 10.1038/oby.2008.224. [DOI] [PubMed] [Google Scholar]
- 25.Yancey AK, Kumanyika SK, Ponce NA et al. Population-based interventions engaging communities of color in healthy eating and active living: a review. Prev Chronic Dis. 2004;1(1):A09. [PMC free article] [PubMed] [Google Scholar]
- 26.Osei-Assibey G, Kyrou I, Adi Y, Kumar S, Matyka K. Dietary and lifestyle interventions for weight management in adults from minority ethnic/non-White groups: a systematic review. Obes Rev. 2010;11(11):769–776. doi: 10.1111/j.1467-789X.2009.00695.x. [DOI] [PubMed] [Google Scholar]
- 27.Foley P, Levine E, Askew S et al. Weight gain prevention among Black women in the rural community health center setting: the Shape Program. BMC Public Health. 2012;12:305. doi: 10.1186/1471-2458-12-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennett GG, Foley PB, Levine EL et al. Behavioral treatment for weight gain prevention among Black women in the community health center setting: a randomized controlled trial. JAMA Intern Med. 2013;173(19):1770–1777. doi: 10.1001/jamainternmed.2013.9263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bennett GG, Warner ET, Glasgow RE et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med. 2012;172(7):565–574. doi: 10.1001/archinternmed.2012.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greaney ML, Quintiliani LM, Warner ET et al. Weight management among patients at community health centers: the “Be Fit, Be Well” study. Obes Weight Manag. 2009;5(5):222–228. [Google Scholar]
- 31.Bennett GG, Herring SJ, Puleo E, Stein EK, Emmons KM, Gillman MW. Web-based weight loss in primary care: a randomized controlled trial. Obesity (Silver Spring) 2010;18(2):308–313. doi: 10.1038/oby.2009.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 33.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21(6):547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):1–7. [Google Scholar]
- 37.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey Protocol. Hyattsville, MD: US Department of Health and Human Services; 2007. [Google Scholar]
- 38.Rubin RR, Knowler WC, Ma Y et al. Depression symptoms and antidepressant medicine use in Diabetes Prevention Program participants. Diabetes Care. 2005;28(4):830–837. doi: 10.2337/diacare.28.4.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gavin AR, Rue T, Takeuchi D. Racial/ethnic differences in the association between obesity and major depressive disorder: findings from the Comprehensive Psychiatric Epidemiology Surveys. Public Health Rep. 2010;125(5):698–708. doi: 10.1177/003335491012500512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hicken MT, Lee H, Mezuk B, Kershaw KN, Rafferty J, Jackson JS. Racial and ethnic differences in the association between obesity and depression in women. J Womens Health (Larchmt) 2013;22(5):445–452. doi: 10.1089/jwh.2012.4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kubzansky LD, Bordelois P, Jun HJ et al. The weight of traumatic stress: a prospective study of posttraumatic stress disorder symptoms and weight status in women. JAMA Psychiatry. 2014;71(1):44–51. doi: 10.1001/jamapsychiatry.2013.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heo M, Pietrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in US adults: comparison and moderation by sex, age, and race. Int J Obes (Lond) 2006;30(3):513–519. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- 43.Appel LJ, Clark JM, Yeh HC et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rubin RR, Peyrot M, Wang NY et al. Patient-reported outcomes in the practice-based opportunities for weight reduction (POWER) trial. Qual Life Res. 2013;22(9):2389–2398. doi: 10.1007/s11136-013-0363-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brownell K. The LEARN Program for Weight Management. Dallas, TX: American Health Publishing Company; 2004. [Google Scholar]
- 46.Mirowsky J, Ross CE. Social Causes of Psychological Distress. New York, NY: Transaction Publishers; 2003. [Google Scholar]
- 47.Babyak M, Blumenthal JA, Herman S et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62(5):633–638. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 49.Ferster CB. A functional analysis of depression. Am Psychol. 1973;28(10):857–870. doi: 10.1037/h0035605. [DOI] [PubMed] [Google Scholar]
- 50.Veale D. Behavioural activation for depression. Adv Psychiatr Treat. 2008;14(1):29–36. [Google Scholar]
- 51.Martell CR, Addis ME, Jacobson NS. Depression in Context: Strategies for Guided Action. New York, NY: WW Norton & Co; 2001. [Google Scholar]
- 52.Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: returning to contextual roots. Clin Psychol Sci Pract. 2001;8(3):255–270. [Google Scholar]
- 53.Schulberg HC, Katon W, Simon GE, Rush AJ. Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry. 1998;55(12):1121. doi: 10.1001/archpsyc.55.12.1121. [DOI] [PubMed] [Google Scholar]
- 54.Unützer J, Katon W, Callahan CM et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 55.Stewart M, Brown JB, Donner A et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]