Abstract
Objectives. We examined gap length, characteristics associated with gap length, and number of enrollment periods among Medicaid-enrolled children in the United States.
Methods. We linked the 2004 National Health Interview Survey to Medicaid Analytic eXtract files for 1999 through 2008. We examined linkage-eligible children aged 5 to 13 years in the 2004 National Health Interview Survey who disenrolled from Medicaid. We generated Kaplan-Meier curves of time to reenrollment. We used Cox proportional hazards models to assess the effect of sociodemographic variables on time to reenrollment. We compared the percentage of children enrolled 4 or more times across sociodemographic groups.
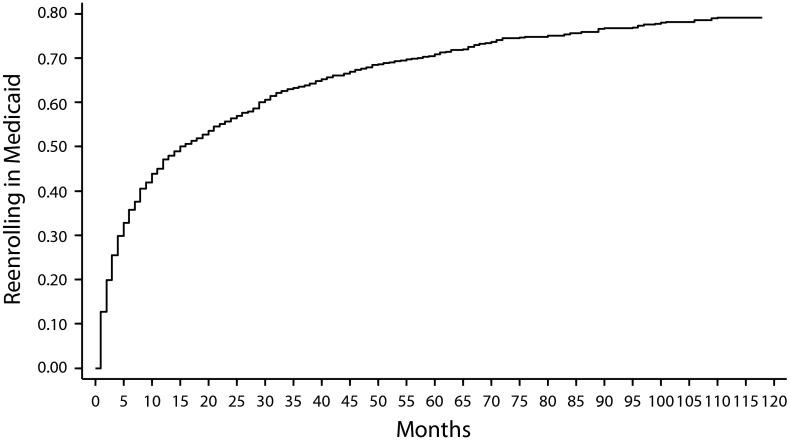
Results. Of children who disenrolled from Medicaid, 35.8%, 47.1%, 63.5%, 70.8%, and 79.1% of children had reenrolled in Medicaid by 6 months, 1, 3, 5, and 10 years, respectively. Children who were younger, poorer, or of minority race/ethnicity or had lower educated parents had shorter gaps in Medicaid and were more likely to have had 4 or more Medicaid enrollment periods.
Conclusions. Nearly half of US children who disenrolled from Medicaid reenrolled within 1 year. Children with traditionally high-risk demographic characteristics had shorter gaps in Medicaid enrollment and were more likely to have more periods of Medicaid enrollment.
Medicaid provided health insurance for approximately one third of children younger than 18 years in 2010.1 However, many children experience gaps in Medicaid enrollment. Some children have gaps in Medicaid enrollment because they gain health insurance coverage from another source, but more than half of children become uninsured during these gaps, despite half of those remaining eligible for Medicaid.2 Gaps in health insurance and in Medicaid coverage specifically have been shown to negatively affect child health3,4 as well as shift care from ambulatory settings to more costly emergency departments and inpatient days.5
Gaps in Medicaid enrollment among children have been previously described, although rarely using nationally representative data or even data from multiple states.6,7 Research using Medicaid data from 2005 to 2007 suggests that, among children enrolled in Medicaid at the beginning of 2005, 41.1% were continuously enrolled through 2007, 27.1% disenrolled and reenrolled, and 31.8% disenrolled and did not return to Medicaid by the end of 2007.7 Another recent study showed that, between 2000 and 2004, among children who disenrolled from Medicaid 6 months before, 28.1% had reenrolled in Medicaid and 28.9% had acquired other health insurance.8 However, although some studies have reported on gaps in Medicaid enrollment among children, the characteristics of children who have gaps and the characteristics of those with shorter as compared with longer gaps in Medicaid coverage have not been described. Similarly, other studies have examined the enrollment and disenrollment patterns of children for insurance in general2,9–12 and for Medicaid specifically.7 However, previous studies have not identified the characteristics of children with multiple entrances to and exits from Medicaid over a prolonged period.
There has been great interest in trying to develop policies to enroll and retain Medicaid-eligible children in the Medicaid programs.13 Understanding the lengths of Medicaid gaps—as well as the sociodemographic and health characteristics of children with continuous enrollment, shorter gaps, longer gaps, and frequent enrollments and disenrollments—could provide valuable information for states intending to design programs to retain Medicaid-eligible children in Medicaid programs and to reenroll Medicaid-eligible children who have become uninsured.
We used a nationally representative sample of children and tracked Medicaid enrollment patterns among children across 10 years to examine 2 specific issues. First, we examined sociodemographic and health characteristics for children with longer versus shorter gaps in Medicaid enrollment. Second, to identify children at greater risk for multiple enrollment periods, we examined the percentage of children with 4 or more enrollment periods in Medicaid within selected sociodemographic and health characteristic groups.
METHODS
We used the National Health Interview Survey (NHIS) and Medicaid Analytic eXtract (MAX) linked data files to examine Medicaid enrollment patterns over time in US children. We linked the 2004 NHIS person-file to the MAX files for 1999 through 2008.
The NHIS is a nationally representative, cross-sectional population health survey that the National Center for Health Statistics (NCHS) conducts annually. It is a multistage sample survey with primary sampling units of counties or adjacent counties, secondary sampling units of clusters of houses, tertiary sampling units of households, and finally persons within households.14 The response rate for the family interview, from which we derived our data, was 86.5%. A knowledgeable adult family member (aged 18 years or older) residing in the household provided the information about the children.15
The Centers for Medicare and Medicaid Services creates the MAX files. Each state provides Medicaid enrollee eligibility information and Medicaid claims paid to the Centers for Medicare and Medicaid Services through the Medicaid Statistical Information System. The Centers for Medicare and Medicaid Services extracts data from the Medicaid Statistical Information System to create the MAX files.
Respondents needed to match exactly on social security number and month and year of birth to be linked between the NHIS and MAX files. Details of the linkage algorithm can be found elsewhere.16 Of children aged 5 to 13 years in the 2004 NHIS, 51.3% were linkage eligible (n = 6749), meaning consent and sufficient information were provided to enable linkage.
We used the 2004 NHIS to identify children aged 5–13 years. We excluded children younger than 5 years because these children may not have been born during the earliest year of the MAX data linked to the NHIS (1999). We excluded children older than 13 years at the time of the NHIS interview because these children would become older than 17 years if observed until 2008. The NCHS Ethics Review Board prohibits linkage of Medicaid records beyond age 17 years for children sampled in the NHIS before their 18th birthday. Additionally, Medicaid enrollment criteria change greatly after an individual reaches age 19 years.
We determined enrollment in Medicaid during each month during the years 1999 through 2008 by linkage to the MAX files during that month of the year and indication within the MAX file that the child was enrolled in either the Medicaid program or in a Medicaid expansion Children’s Health Insurance Program (M-CHIP) rather than in a separately administered Children’s Health Insurance Program (separate CHIP). We did not consider separately administered CHIP programs, as data from separate CHIP programs are inconsistently reported within the MAX files. We obtained sociodemographic and health status variables from the NHIS, including age at time of first observed disenrollment from Medicaid, race/ethnicity, urban versus rural status, highest level of parental education, health status, and family income-to-poverty level ratio. For age at first disenrollment, we assigned children who did not disenroll before the end of the observation period their age at the end of the observation period.
Because this is an individual-level longitudinal analysis, the children we followed increased in age from 5 to 13 years in 2004 to 9 to 17 years in 2008. During 1999, the first year of the linked MAX files, the children we followed were aged 0 to 8 years.
Of children aged 5 to 13 years in the 2004 NHIS who were linkage eligible (n = 6749), 3381 were ever enrolled in Medicaid or M-CHIP during the 10-year observation period. We excluded 5 observations from the analysis because the MAX files indicated Medicaid or M-CHIP enrollment before the month of birth indicated by the NHIS, which seemed implausible. Of the remaining 3376 observations, the highest level of parental education was missing for 220 children (6.5%), health status was missing for 4 children (0.1%), and age at first observed disenrollment from Medicaid or M-CHIP was missing for 4 children (0.1%). Race/ethnicity was missing for 421 children (12.5%), but we used single imputation values provided by the NHIS for these missing observations. Income was missing for 639 observations (18.9%), but we used multiply imputed data for income-to-poverty ratio provided by the NHIS for these missing observations. The final study included 3149 children for whom data were available for all variables.
Analysis
We used survival analysis to examine the time from disenrolling in Medicaid or M-CHIP to reenrolling in Medicaid or M-CHIP (the length of the first gap in enrollment). For the first gap in Medicaid or M-CHIP coverage, we assessed bivariable and multivariable associations between longer gaps in Medicaid or M-CHIP and each sociodemographic and health status variable.
We were unable to determine the length of the initial Medicaid or M-CHIP enrollment because 52.6% (50.8% weighted) of children who were enrolled at any time during the 10-year period were already enrolled during the first month of the observation period, creating significant left-censoring. Because it is unknown when these respondents first became at risk for the outcome of disenrolling from Medicaid or M-CHIP, unbiased estimates for the length of the initial Medicaid or M-CHIP enrollment may be difficult to obtain.
The term “churning” is often used to describe Medicaid enrollees who enroll and disenroll multiple times, but to our knowledge, there is no specific definition of this phenomenon. We identified the number of times that children were enrolled in Medicaid or M-CHIP during the 10-year observation period and divided them into categories of once, twice, 3 times, and 4 or more times, similar to the categorization previously used in research on Medicaid gaps.7 We compared the percentage of children within sociodemographic and health status groups enrolled in Medicaid 4 or more times.
Statistical Analysis
We adjusted the sample weights in the 2004 NHIS to account for survey respondents who were not linkage eligible in the NHIS.17 We used a model-based calibration approach (WTADJUST procedures) in SUDAAN version 11.0.0 (RTI International, Research Triangle Park, NC) to reweight the data to preserve correct population totals within race/ethnicity, age, and gender cross-stratifications.18 We conducted analyses and adjusted for the complex survey design of the NHIS using Stata version 12.1 SE and the SVY suite of commands (StataCorp LP, College Station, TX). We analyzed multiply imputed data using the MI suite of commands.
We used Kaplan-Meier survival analysis to generate a survival curve for a child’s first observed gap in Medicaid or M-CHIP, with censoring of children who had not reenrolled in Medicaid or M-CHIP by the end of the observation period (2008). We used Cox proportional hazards models in bivariable and multivariable analyses to assess the effect of each independent variable on the hazard of reenrollment in Medicaid after the first gap. We used the Breslow method for ties in each case. We included sociodemographic and health status variables in multivariable analysis, as a similar group of variables have been used previously to examine continuity of insurance coverage.3 We did not include poverty-to-income ratio in initial multivariable analysis because of high correlation with highest level of parental education and because income is more time variant than are other variables. We conducted additional analyses that included poverty-to-income ratio to determine whether poverty-to-income ratio would have a significant independent effect, even after controlling for other highly correlated sociodemographic factors.
We conducted statistical comparisons of the percentage of children in each sociodemographic and health status group who were enrolled in Medicaid 4 or more times during the 10-year period using the Wald test of proportions. To compare percentages within the multiply imputed income-to-poverty ratio categories, we used the unrestricted fraction missing information model test. We considered estimates statistically unreliable if there were fewer than 30 observations or relative SEs were less than 30%. We did not make any adjustments for multiple comparisons.
RESULTS
Of those who were enrolled in Medicaid or M-CHIP at some point during the 10-year observation period (n = 3149), 2512 (80.0% weighted; 95% confidence interval [CI] = 78.0, 81.8) disenrolled at some point before the end of the 10-year observation period. The characteristics of the children who disenrolled from Medicaid or M-CHIP at some point before the end of the 10-year period are presented in Table 1.
TABLE 1—
Characteristics of Children Who Disenrolled From Medicaid During Observation Period: National Health Interview Survey, United States, 2004
| Unweighted No. |
||||
| Characteristic | Not Reenrolled, Censored (n = 718) | Reenrolled, Not Censored (n = 1794) | Total (n = 2512) | Weighted % (SE) |
| Age at first disenrollment, y | ||||
| < 6 | 177 | 764 | 941 | 37.2 (1.1) |
| 6–11 | 352 | 839 | 1191 | 47.6 (1.2) |
| ≥12 | 189 | 191 | 380 | 15.2 (0.9) |
| Gender | ||||
| Male | 365 | 914 | 1279 | 49.2 (1.1) |
| Female | 353 | 880 | 1233 | 50.8 (1.1) |
| Race | ||||
| Non-Hispanic White | 365 | 585 | 950 | 45.4 (1.6) |
| Non-Hispanic Black | 98 | 416 | 514 | 20.4 (1.2) |
| Non-Hispanic all others | 21 | 44 | 65 | 4.1 (0.6) |
| Hispanic | 234 | 749 | 983 | 30.2 (1.3) |
| Health status | ||||
| Excellent or very good | 573 | 1282 | 1855 | 74.6 (1.2) |
| Good, fair, or poor | 145 | 512 | 657 | 25.4 (1.2) |
| Highest level of parental education | ||||
| ≥ some college, associate degree, technical degree | 412 | 688 | 1100 | 47.7 (1.4) |
| High school | 194 | 601 | 795 | 31.8 (1.3) |
| < high school | 112 | 505 | 617 | 20.5 (1.1) |
| Income-to-poverty ratio,a % | ||||
| < 100 | 112 | 741 | 853 | 31.1 (1.4) |
| 100–149 | 150 | 441 | 592 | 22.9 (1.4) |
| 150–199 | 145 | 261 | 405 | 16.4 (1.2) |
| ≥ 200 | 311 | 351 | 662 | 29.6 (1.3) |
| MSA status | ||||
| In MSA, in central city | 197 | 681 | 878 | 31.8 (1.5) |
| In MSA, not in central city | 359 | 740 | 1099 | 45.5 (1.7) |
| Not in MSA | 162 | 373 | 535 | 22.7 (1.4) |
Note. MSA = metropolitan statistical area. Children were aged 5–13 years in 2004. Observation period was 1999–2008. Data are from the National Health Interview Survey, 2004 and Medicaid Analytic eXtract 1999–2008 linked data files.
Numbers of observations in each income-to-poverty ratio category are averages rounded to the nearest whole number across the 5 imputed values for these values. Because of rounding, censored and noncensored columns may not add exactly to total column. Similarly, numbers of observations in categories may not add exactly to column totals.
Of those who disenrolled in Medicaid or M-CHIP during the 10-year period, Kaplan-Meier estimates showed that by age 6 months, 1 year, 3 years, 5 years, and 10 years, 35.8%, 47.1%, 63.5%, 70.8%, and 79.1% of children, respectively, had reenrolled in Medicaid or M-CHIP (Figure 1). In bivariable analysis assessing the relative hazard of reenrollment in Medicaid or M-CHIP after disenrolling from Medicaid or M-CHIP the first time, children who were older at time of disenrollment had a lower likelihood of reenrolling (Table 2). Compared with non-Hispanic White children, non-Hispanic Black (hazard ratio [HR] = 1.66; 95% CI = 1.43, 1.92) and Hispanic (HR = 1.42; 95% CI = 1.23, 1.63) children had significantly greater likelihood of reenrolling in Medicaid or M-CHIP, as did children in good, fair, or poor health compared with those in excellent or very good health (HR = 1.26; 95% CI = 1.10, 1.47). Children with parents with lower levels of education and children in families with lower income-to-poverty ratios had a higher likelihood of reenrolling in Medicaid or M-CHIP. Finally, children living in a metropolitan statistical area (MSA) but not in a central city (HR = 0.73; 95% CI = 0.63, 0.84) and those not living in an MSA (HR = 0.82; 95% CI = 0.69, 0.97) had a lower likelihood of reenrolling in Medicaid or M-CHIP than did children living in a central city of an MSA.
FIGURE 1—
Kaplan–Meier failure function of time to reenrollment in Medicaid after first disenrollment during observation period of 1999–2008 for children aged 5–13 years in the 2004 National Health Interview Survey: United States.
TABLE 2—
Children’s Unadjusted and Adjusted Hazard Ratios for Reenrollment in Medicaid: National Health Interview Survey, United States, 2004
| Characteristic | UHR (95% CI) | AHR (95% CI) |
| Age at first disenrollment, y | ||
| < 6 (Ref) | 1.00 | 1.00 |
| 6–11 | 0.89* (0.80, 0.99) | 0.90 (0.81, 1.00) |
| ≥12 | 0.80* (0.67, 0.96) | 0.82* (0.69, 0.96) |
| Gender | ||
| Male (Ref) | 1.00 | 1.00 |
| Female | 1.01 (0.92, 1.12) | 1.01 (0.92, 1.12) |
| Race/ethnicity | ||
| Non-Hispanic White (Ref) | 1.00 | 1.00 |
| Non-Hispanic Black | 1.66*** (1.43, 1.92) | 1.52*** (1.31, 1.77) |
| Non-Hispanic all others | 1.07 (0.72, 1.59) | 0.96 (0.65, 1.44) |
| Hispanic | 1.42*** (1.23, 1.63) | 1.19* (1.02, 1.38) |
| Health status | ||
| Excellent or very good (Ref) | 1.00 | 1.00 |
| Good, fair, or poor | 1.26** (1.10, 1.47) | 1.13 (0.98, 1.31) |
| Highest level of parental education | ||
| ≥ some college, associate degree, or technical degree (Ref) | 1.00 | 1.00 |
| High school | 1.48*** (1.29, 1.70) | 1.41*** (1.24, 1.61) |
| < high school | 1.82*** (1.55, 2.13) | 1.67*** (1.42, 1.95) |
| Income-to-poverty ratio, % | ||
| < 100 | 3.01*** (2.53, 3.59) | NA |
| 100–149 | 1.94*** (1.58, 2.38) | NA |
| 150–199 | 1.43** 1.13, 1.81) | NA |
| ≥ 200 (Ref) | 1.00 | NA |
| MSA status | ||
| In MSA, in central city (Ref) | 1.00 | 1.00 |
| In MSA, not in central city | 0.73*** (0.63, 0.84) | 0.83** (0.73, 0.96) |
| Not in MSA | 0.82* (0.69, 0.97) | 0.94 (0.77, 1.14) |
Note. AHR = adjusted hazard ratio; CI = confidence interval; MSA = metropolitan statistical area; NA = not available; UHR = unadjusted hazard ratio. Characteristics are of children (aged 5–13 years in 2004) who reenrolled in Medicaid after first disenrollment during our observation period of 1999–2008. Data are from National Health Interview Survey, 2004 and Medicaid Analytic eXtract 1999–2008 linked data files.
P < .05; **P < .01; ***P < .001.
In general, the results of multivariable analysis were similar to those found in bivariable analysis (Table 2). However, effect sizes for some variables were attenuated, and some specific categories lost significance. Specifically, children in good, fair, or poor health no longer had a significantly greater risk of reenrollment than did children in excellent or very good health, and children living in a non-MSA were no longer at lower risk of reenrollment than were those living in a central city within an MSA. The addition of poverty-to-income ratio to the model (not shown) further attenuated the effect sizes of nearly all variables, although all categories found significant in the initial multivariable model remained significant with the exception of living in a MSA, but not in a central city, and being Hispanic. In this model, there was an increasing likelihood of reenrollment with decreasing income-to-poverty ratios; compared with those at 200% or greater, children in families with lower income-to-poverty ratio categories had higher likelihood of reenrollment: 150% to 199% (adjusted hazard ratio [AHR] = 1.35; 95% CI = 1.07, 1.71; P < .05), 100% to 149% (AHR = 1.84; 95% CI = 1.50, 2.26; P < .001), and less than 100% (AHR = 2.64; 95% CI = 2.20, 3.18; P < .001).
Of the children ever enrolled in Medicaid or M-CHIP during the 10-year observation period, 44.3% were enrolled only a single time, 28.2% were enrolled twice, 15.3% were enrolled 3 times, and 12.2% were enrolled 4 or more times (Table 3). The population for this analysis differs from that in the analysis of gap length in that it includes those who were enrolled in Medicaid or M-CHIP but did not disenroll from Medicaid or M-CHIP during the observation period. We included this group (n = 637) as having been enrolled only a single time, and it is therefore part of the 44.3% of children who were enrolled in Medicaid only a single time. The percentage of children enrolled in Medicaid 4 or more times was statistically greater for children younger than 6 years (23.3%) than for those aged 6 to 11 years; children who were non-Hispanic Black (14.6%) or Hispanic (15.1%) than for children who were non-Hispanic White (9.3%); children with parents whose highest level of educational attainment was less than high school (16.1%) or high school (15.1%) than for those with some college, associate degrees, or technical degrees or higher (8.4%); and children in families with income-to-poverty ratios of less than 100% (15.0%) or 100% to 149% (16.0%) than for those in families with income-to-poverty ratios of greater than 200% (7.3%).
TABLE 3—
Number of Times Children Were Enrolled in Medicaid Between 1999 and 2008: National Health Interview Survey, United States, 2004
| Enrollments in Medicaid, Mean (SE) |
|||||
| Characteristic | 1 (n = 1355) | 2 (n = 888) | 3 (n = 493) | ≥ 4 (n = 413) | Pa |
| Total | 44.3 (1.1) | 28.2 (1.1) | 15.3 (0.8) | 12.2 (0.7) | |
| Age at first disenrollment, y | |||||
| < 6 (n = 941; Ref) | 20.6 (1.6) | 31.1 (1.8) | 25.1 (1.7) | 23.3 (1.7) | |
| 6–11 (n = 1392) | 41.1 (1.6) | 32.0 (1.5) | 15.8 (1.2) | 11.2 (1.0) | ≤ .001 |
| ≥ 12 (n = 816) | 77.2 (1.7) | 18.3 (1.5) | 3.3 (0.7) | . . .b | |
| Gender | |||||
| Male (n = 1611; Ref) | 44.7 (1.5) | 28.9 (1.3) | 15.0 (1.1) | 11.4 (0.9) | |
| Female (n = 1538) | 43.9 (1.4) | 27.5 (1.3) | 15.6 (1.1) | 13.0 (1.0) | .17 |
| Race/ethnicity | |||||
| Non-Hispanic White (n = 1154; Ref) | 49.5 (1.9) | 26.9 (1.6) | 14.3 (1.3) | 9.3 (1.1) | |
| Non-Hispanic Black (n = 716) | 41.3 (2.3) | 30.5 (2.2) | 13.7 (1.6) | 14.6 (1.7) | < .01 |
| Non-Hispanic all others (n = 88) | 54.0 (6.0) | . . .b | . . .b | . . .b | |
| Hispanic (n = 1191) | 37.2 (1.8) | 29.2 (1.7) | 18.4 (1.6) | 15.1 (1.3) | < .001 |
| Health status | |||||
| Excellent or very good (n = 2274; Ref) | 44.8 (1.3) | 28.5 (1.2) | 15.0 (0.9) | 11.7 (0.9) | |
| Good, fair, or poor (n = 875) | 42.9 (2.2) | 27.4 (2.0) | 16.3 (1.8) | 13.5 (1.5) | .33 |
| Highest level of parental education | |||||
| ≥ some college, associate degree, or technical degree (n = 1338; Ref) | 50.2 (1.7) | 27.0 (1.5) | 14.4 (1.2) | 8.4 (1.0) | |
| High school (n = 981) | 39.4 (2.0) | 29.8 (2.0) | 15.7 (1.5) | 15.1 (1.5) | < .001 |
| < high school (n = 830) | 39.0 (2.2) | 28.3 (2.0) | 16.7 (1.8) | 16.1 (1.7) | < .001 |
| Income-to-poverty ratio,c % | |||||
| < 100 (n = 1198) | 38.3 (2.0) | 30.1 (1.6) | 16.6 (1.5) | 15.0 (1.4) | ≤ .001 |
| 100–149 (n = 692) | 35.8 (2.7) | 30.6 (2.5) | 17.6 (2.1) | 16.0 (1.9) | < .001 |
| 150–199 (n = 428) | 47.9 (3.4) | 28.4 (2.6) | 14.3 (2.0) | 9.4 (2.1) | ≥ .39 |
| ≥ 200 (n = 778; Ref) | 56.3 (2.4) | 23.9 (1.9) | 12.5 (1.6) | 7.3 (1.2) | |
| MSA status | |||||
| In MSA, in central city (n = 1135; Ref) | 40.1 (1.9) | 30.9 (1.8) | 16.1 (1.5) | 13.0 (1.2) | |
| In MSA, not in central city (n = 1356) | 47.2 (1.8) | 26.6 (1.6) | 15.2 (1.3) | 11.0 (1.1) | .23 |
| Not in MSA (n = 658) | 44.7 (2.2) | 27.3 (2.1) | 14.5 (1.7) | 13.5 (1.6) | .78 |
Note. MSA = metropolitan statistical area. Characteristics are of children aged 5–13 years in 2004. Data are from the National Health Interview Survey, 2004 and Medicaid Analytic eXtract 1999–2008 linked data files.
For comparison of percentages in ≥ 4 enrollments group.
Estimate is not statistically reliable because n < 30 or relative SE > 30%.
Numbers of observations in each income-to-poverty ratio category are averages rounded to the nearest whole number across the 5 imputed values for this variable.
DISCUSSION
Over a 10-year period, 80% of children enrolled in Medicaid or M-CHIP left the program at least once. After their initial disenrollment from Medicaid or M-CHIP, slightly less than half of children (47.0%) had reenrolled by 1 year, nearly two thirds (63.5%) had reenrolled by 3 years, and approximately 70.0% had reenrolled within 5 years. Understanding that a majority of children who disenroll from Medicaid return to the program may be useful for state and federal Medicaid program administrators because it suggests that, at some point in the future, they usually will again pay for the health care of these children. Future research to examine the health care and health trajectories of children during those gaps may also provide useful data for policymakers and administrators alike.
National estimates of gaps in Medicaid or M-CHIP are uncommon, but work by Czajka suggests that among children who disenrolled from Medicaid within a 3-year time frame (2005–2007), approximately 38% had reenrolled within a year.7 Because Czajka did not use survival analysis, his estimates may have been biased downward because they may not account for children who disenrolled within a year of the end of the observation period and those who were not observed to reenroll at all. Nonetheless, both studies suggest that many children who disenroll from Medicaid do reenroll within a year.
These estimates of gap lengths may be of great use to states considering enacting or changing their Medicaid or CHIP continuous eligibility policies. Continuous eligibility policies allow states to provide children who enroll in Medicaid or CHIP with up to 12 months of continuous insurance coverage, even if the family’s income changes during the period.19 One rationale that has been given for these programs is that they can reduce administrative costs by decreasing the number of disenrollments and reenrollments that states process when children disenroll and reenroll in Medicaid frequently.19 Whether continuous eligibility is provided, to whom, and for how many months varies between states.20 Knowledge of the length of gaps in Medicaid enrollment, as well as how frequently children return to Medicaid during childhood, provides states with needed information as they create or revise continuous eligibility policies.
We also examined sociodemographic differences that exist within the Medicaid population, rather than treating the Medicaid population as a single sociodemographic entity. As such, our data suggest that gap length differs by these sociodemographic differences, most notably by age at disenrollment, race/ethnicity, highest level of parental education, income-to-poverty ratio, and geography. By contrast, a study of Survey of Income and Program Participation data from 1992 to 1994 found that the characteristics of children with long periods of uninsurance were similar to those with short periods of uninsurance,2although that study examined gaps in insurance, whereas our study examined gaps in Medicaid or M-CHIP. We identified characteristics that may help predict which children will be likely to return to the Medicaid or M-CHIP program.
Additionally, our data show that, largely, the same set of sociodemographic factors are related to being enrolled in Medicaid 4 or more times during the 10-year period. Indeed, younger, poorer minority children with lower educated parents are not only more likely to have shorter gaps in Medicaid or M-CHIP but also more likely to have 4 or more enrollment periods.
Understanding the sociodemographic factors associated with longer and shorter gaps and multiple enrollment periods in the Medicaid program may be useful in trying to alleviate churning and unnecessary gaps in insurance. One assessment of evidence for different strategies to eliminate churning among eligible children suggested that states may need to use multiple strategies and that, in isolation, any given step may not be successful.21 In addition to continuous enrollment policies, 1 assessment of the evidence for different strategies to enroll and retain eligible children in Medicaid or CHIP programs suggested both community-based outreach and marketing techniques to increase awareness of these programs.22 To be sure, evidence on the success of marketing techniques is mixed, but some studies suggest that using marketing techniques can be useful.22 Furthermore, it has been suggested that more targeted marketing efforts are more successful than are broad marketing campaigns aimed at the general population.22 If states choose to adopt these strategies, sociodemographic descriptions of churners, as we have conducted, may be useful in creating targeted interventions.
This study has several limitations. Foremost, child demographic characteristics were collected in 2004, but some characteristics, such as family income-to-poverty ratio, may change across the study period, adding some uncertainty to the characterization of the children. In addition, Medicaid enrollment has increased since 2008,23 potentially affecting gap lengths or predictors of gap length.23
Only 51.3% of children in the 2004 NHIS were linkage eligible, which may introduce bias into our estimates. However, we reweighted the data to account, to the extent possible, for linkage eligibility. With the exception of age at first disenrollment that could not be assessed, the distributions of the variables we used in the analysis using the full sample of children and the distribution using the reweighted data were largely similar, with differences of 1.6% points or less in all categories (data not shown).
Finally, insurance status of children during their gaps in Medicaid or M-CHIP is unknown. Disenrollment and subsequent failure to reenroll may be because of loss of Medicaid or M-CHIP eligibility, acquisition of other private insurance, movement from Medicaid to separate CHIP programs, or failure to reenroll for other reasons. Shifts between CHIP and Medicaid, for example, may be substantial.24 In our sample, in the month following their first disenrollment from Medicaid, approximately 8.5% of children enrolled in an M-CHIP program (data not shown), although M-CHIP programs make up a smaller proportion of CHIP than do separate CHIP programs.25 Still, it is known that many children have been shown to be uninsured during gaps in Medicaid.2,8
These data show that among children who disenroll from Medicaid, nearly half will be reenrolled within a year, and nearly 70% will be reenrolled within 5 years. Also, younger, poorer minority children with parents of lower educational level have shorter gaps in Medicaid and are more likely to have several enrollment periods. These data may help state policymakers in efforts to enroll and retain eligible children in the Medicaid program.
Human Participant Protection
The National Health Interview Survey and the subsequent link with the Medicaid Analytic eXtract files were approved by the National Center for Health Statistics ethics review board.
References
- 1.Bloom B, Cohen RA, Freeman G. Summary health statistics for US children: National Health Interview Survey, 2010. Vital Health Stat 10. 2011;(250):1–80. [PubMed] [Google Scholar]
- 2.Czajka JL. Analysis of Children’s Health Insurance Patterns: Findings From the SIPP. Washington, DC: Mathematica Policy Research, Inc.; 1999. [Google Scholar]
- 3.Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005;353(4):382–391. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- 4.Bindman AB, Chattopadhyay A, Auerback GM. Medicaid re-enrollment policies and children’s risk of hospitalizations for ambulatory care sensitive conditions. Med Care. 2008;46(10):1049–1054. doi: 10.1097/MLR.0b013e318185ce24. [DOI] [PubMed] [Google Scholar]
- 5.Rimsza ME, Butler RJ, Johnson WG. Impact of Medicaid disenrollment on health care use and cost. Pediatrics. 2007;119(5):e1026–e1032. doi: 10.1542/peds.2006-2747. [DOI] [PubMed] [Google Scholar]
- 6.Fairbrother GL, Emerson HP, Partridge L. How stable is Medicaid coverage for children? Health Aff (Millwood) 2007;26(2):520–528. doi: 10.1377/hlthaff.26.2.520. [DOI] [PubMed] [Google Scholar]
- 7.Czajka JL. Medicaid Enrollment Gaps, 2005–2007. Washington, DC: Mathematica Policy Research, Inc.; 2012. [Google Scholar]
- 8.Sommers BD. Loss of health insurance among non-elderly adults in Medicaid. J Gen Intern Med. 2009;24(1):1–7. doi: 10.1007/s11606-008-0792-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Short PF, Graefe DR, Schoen C. Churn, Churn, Churn: How Instability of Health Insurance Shapes America’s Uninsured Problem. New York, NY: Commonwealth Fund; 2003. Issue brief no. 688. [PubMed] [Google Scholar]
- 10.Borck R, Cheh V, Lu L. Recent Patterns in Children’s Medicaid Enrollment: A National View. Washington, DC: Mathematica Policy Research, Inc.; 2011. [Google Scholar]
- 11.Satchell M, Pati S. Insurance gaps among vulnerable children in the United States, 1999–2001. Pediatrics. 2005;116(5):1155–1161. doi: 10.1542/peds.2004-2403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Short PF, Graefe DR, Swartz K, Uberoi N. New estimates of gaps and transitions in health insurance. Med Care Res Rev. 2012;69(6):721–736. doi: 10.1177/1077558712454195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cassidy A. Enrolling more kids in Medicaid and CHIP. Health Affairs. January 27, 2011. [Google Scholar]
- 14.National Center for Health Statistics. Design and estimation for the National Health Interview Survey, 1995–2004. Vital Health Stat 2. 2000;(130):1–31. [PubMed] [Google Scholar]
- 15.2004 National Health Interview Survey (NHIS), Public Use Data Release, NHIS Survey Description. Hyattsville, MD: National Center for Health Statistics; 2005. [Google Scholar]
- 16.Simon A, Driscoll A, Golden C . Documentation and Analytic Guidelines for NCHS Surveys Linked to Medicaid Analytic eXtract (MAX) files. Hyattsville, MD: National Center for Health Statistics; 2011. [Google Scholar]
- 17.Use of Survey Weights for Linked Data Files—Preliminary Guidance. Hyattsville, MD: National Center for Health Statistics; 2011. [Google Scholar]
- 18.Witt MB. Overview of software that will produce sample weight adjustments. Presented at: Joint Statistical Meetings; 2009; Washington, DC.
- 19.Horner D. Program Design Snapshot: 12-Month Continuous Eligibility. Washington, DC: Georgetown University Health Policy Institute; 2009. [Google Scholar]
- 20.The Henry J. Kaiser Family Foundation. Has 12-month continuous eligibility for children under Medicaid and separate CHIP programs. 2013. Available at: http://kff.org/medicaid/state-indicator/12-mo-continuous-eligibilitymedichip. Accessed December 15, 2013.
- 21.Summer L, Mann C. Instability of Public Health Insurance Coverage for Children and Their Families: Causes, Consequences, and Remedies. Washington, DC: Georgetown University Health Policy Institute; 2006. [Google Scholar]
- 22.Wachino V, Weiss AM. Maximizing Kids’ Enrollment in Medicaid and SCHIP: What Works in Reaching, Enrolling, and Retaining Eligible Children. Portland, ME: National Academy for State Health Policy; 2009. [Google Scholar]
- 23.Snyder L, Rudowitz R, Ellis E, Roberts D. Medicaid Enrollment: June 2011 Snapshot. Washington, DC: Kaiser Commission on Medicaid and the Uninsured and Health Management Associates; 2012. [Google Scholar]
- 24.Report to Congress on Medicaid and CHIP. Washington, DC: Medicaid and CHIP Payment and Access Commission; 2012. [Google Scholar]
- 25.Report to the Congress on Medicaid and CHIP. Washington, DC: Medicaid and CHIP Payment and Access Commission; 2011. [Google Scholar]