Abstract
Objectives. We examined whether and how an HIV prevention diffusion-based intervention spread throughout participants’ online social networks and whether changes in social network ties were associated with increased HIV prevention and testing behaviors.
Methods. We randomly assigned 112 primarily racial/ethnic minority men who have sex with men (MSM) to receive peer-delivered HIV (intervention) or general health (control) information over 12 weeks through closed Facebook groups. We recorded participants’ public Facebook friend networks at baseline (September 2010) and follow-up (February 2011), and assessed whether changes in network growth were associated with changes in health engagement and HIV testing.
Results. Within-group ties increased in both conditions from baseline to follow-up. Among the intervention group, we found a significant positive relation between increased network ties and using social media to discuss sexual behaviors. We found a positive trending relationship between increased network ties and likelihood of HIV testing, follow-up for test results, and participation in online community discussions. No significant differences were seen within control groups.
Conclusions. Among high-risk MSM, peer-led social media HIV prevention interventions can increase community cohesion. These changes appear to be associated with increased HIV prevention and testing behaviors.
African American and Latino individuals are at high risk for contracting HIV.1 In Los Angeles County, California, most of these cases are attributable to men who have sex with men (MSM), who currently account for more than 75% of all HIV cases.2,3 Researchers, and MSM themselves, have suggested use of novel approaches to increase HIV prevention and testing among at-risk populations.4,5
Peer leader interventions, based on diffusion theories, are community-based interventions that train community peers to spread HIV prevention information and change HIV prevention-related social norms.6–9 Successful peer-led interventions have resulted in decreasing anal intercourse up to 25% and increasing condom use up to 16%, with sustained behavior change up to 3 years later.10–12 Peer-delivered interventions have been found to be acceptable among MSM populations.13 Social network interventions have shown that information can rapidly diffuse throughout social networks to change health behaviors,14,15 suggesting that peer-delivered HIV interventions also might diffuse throughout social networks.
Growth in social media allows these technologies to be used for peer-led HIV testing interventions,4 and research supports that peer-led interventions delivered via social media can increase HIV testing.16 Social networking technologies, such as Facebook, allow users to connect and communicate with other network users by sharing pictures, messages, Web site links, and other multimedia information.17 High rates of online social networking, especially among groups disproportionately affected by HIV (e.g., MSM),18 make it important to evaluate whether and how interventions might diffuse throughout online social networks. Although social media can be used to increase HIV prevention,16,19,20a and health behaviors of (offline) social ties influence our own health behaviors20b, no known research has studied changes in social network ties during the course of an online social media community HIV intervention or whether and how HIV prevention information and behaviors might spread among group participants in a social media–based HIV testing intervention that is designed for network diffusion.
The Harnessing Online Peer Education (HOPE) intervention was a 12-week randomized controlled HIV prevention intervention designed to use peer-led Facebook groups to diffuse HIV information to increase testing among African American and Latino MSM. The study found that participants in the HIV intervention groups were more likely to request an HIV test than were those in the control groups,16 but whether changes in social network ties (i.e., participants within each group becoming Facebook friends with one another) played a role in these effects among intervention group participants is unknown. The current study used data from the HOPE study and was designed to evaluate the association between changes in online social network structure and HIV prevention and testing among HOPE network participants. Specifically, we have (1) described the change from baseline to follow-up in network ties among HOPE participants as a result of the intervention, (2) presented network visualizations to illustrate changes in network connections among intervention and control group participants, and (3) determined whether changes in social network ties from baseline to follow-up were associated with online community engagement, discussions about HIV prevention, and rates of HIV testing.
METHODS
Between September 2010 and February 2011, we recruited 122 (primarily African American and Latino) MSM participants and 18 peer leaders online and offline for a 12-week randomized controlled trial on Facebook. Six participants did not complete the baseline survey and were dropped from the analysis. Four participants were found to have completed multiple baseline surveys. The second of their responses was included, leaving 112 valid participants.
Peer leaders were recruited with the help of community-based organizations serving primarily African American and Latino MSM. Staff were asked to identify and distribute fliers to well-respected peer leaders who were eligible according to the following criteria: African American or Latino MSM, reported having sex with a man in the past 12 months, 18 years of age or older, living in Los Angeles, and interested in using social media for health outreach. Interested peer leaders were randomly assigned to an HIV prevention (intervention) or general health (control) group and asked to attend 3 in-person training sessions at University of California, Los Angeles (UCLA). Those in the intervention group were trained in HIV prevention fundamentals and epidemiology, use of social media for HIV prevention outreach, and study logistics. Those in the control group were trained in general health (excluding HIV prevention) fundamentals and epidemiology, use of social media for general health outreach, and study logistics. Two peer leaders did not complete the training sessions and were dropped from the study, leaving 16 peer leaders. Peer leaders were paid for their participation ($30 for the initial 4 weeks; $40 for the next 4 weeks; $50 for the final 4 weeks). Additional details about peer leader recruitment and training are available.21,22
We recruited intervention and control participants online (from banner and social media site advertisements); offline (from community organizations and clinics serving primarily African American and Latino MSM); and through participant referrals. Recruitment fliers distributed via community-based organizations stated that the HOPE UCLA study was looking for men who were living in Los Angeles, who were 18 years of age or older, who had had sex with a man in the past 12 months, and who had a Facebook account. A Facebook Connect technology application was used to verify Facebook user accounts and filter participants to allow only 1 unique username per study participant. Because verifying each Facebook username through Facebook Connect slowed recruitment, we first recruited 70% of the participants who were African American and Latino. After the first 70% of African American and Latino participants were recruited, enrollment was opened to other populations to avoid delay. More information about study recruitment can be found in previously published research that used the HOPE data set.16
Intervention
This study used data collected from the HOPE intervention study. Facebook was used to create 4 closed, invite-only groups: 2 HIV intervention groups and 2 control groups. Participants were randomly assigned to 1 of these groups and assigned to 2 peer leaders within that group. Based on the recommended ratio of peer leaders to participants,6 each group was designed to have approximately 4 peer leaders and 25 participants.
During the 12-week intervention, peer leaders in both groups attempted to communicate with their assigned participants both individually and as a group, through chat, wall posts, and personal messages. Participants were required to accept an invitation to join the group, but further group participation and communication were voluntary. Peer leaders in the intervention group were instructed to communicate with participants about HIV prevention, whereas those in the control group were instructed to communicate with participants about general health and well-being, such as diet, exercise, and ways to maintain a low-stress lifestyle. Communication style was determined by peer leaders but could include messages, chats, group forum posts, or links to Web sites providing educational material. Peer leaders were required to complete weekly response forms indicating whether participants responded to their communication attempts. Peer leaders also had individual weekly meetings online or over the telephone with a peer leader trainer who would advise them on how to improve communication with participants.
Measures
Every 4 weeks, participants in both groups were informed that they could receive a free home-based HIV testing kit.23 Each participant was able to receive 1 testing kit during the course of the intervention by e-mailing the study coordinator. Kits were mailed to participants and included a personal identification number that could be used to track whether participants had mailed the testing kit to the company for analysis. Home Access Health Corporation provided data on participants who completed the test and followed up for results.
At baseline and follow-up (12 weeks after baseline), participants completed a 92-item survey focused on demographic information, social media and Internet use, sexual risk behaviors, and HIV testing history. For example, after providing participants with a definition of social networking technologies, participants were asked about social network use, such as “In the past 3 months, how many times did you use social networks to discuss sexual behaviors and partners?” (numerical response). Other survey questions included the following: “In the past 3 months, about how much time did you spend each week on online social networks?”; “In the past 3 months, have you used online social networks to meet new sexual partners?”; and “In the past 3 months, how many times have you talked to someone about the following topics (including sex, HIV testing, and condom use) on an online social network?” Participants were paid $30 in online gift cards to complete the baseline survey and $40 to complete the follow-up survey.
To measure participant engagement and acceptability, we independently recorded whether participants posted on the Facebook group “wall” and contributed to community discussions during the 12-week intervention.20a Contribution to community discussions was defined as posting any content to the community group at least 1 time during the course of the intervention. Details about the content of group posts are available.20a,24
We also planned to assess changes in social network structure. At baseline and follow-up, we recorded participants’ total friend networks by taking screenshots of participants’ “friend lists.” Screenshots of friend lists allowed us to determine whether new online network connections between participants formed over the course of the intervention. Because each friend list includes a thumbnail-size profile picture of each friend, ties to other study participants could be accurately coded by matching the name and picture associated with profiles. Facebook friends who were not study participants were not collected. As such, this was a subset of each participant’s Facebook network but a complete picture of how the study population was connected to one another on Facebook. From these data, degree centrality was calculated in UCINET (Analytic Technologies, Harvard, MA). Degree centrality reports the number of network members to whom a participant is connected and is a measure of social prestige.25 Based on the main outcomes of the HOPE study,16 the main HIV outcomes variables for analyses included (1) requesting and returning an HIV kit, (2) following up for test results, (3) participating in group discussions, and (4) using social networks to discuss sexual behaviors.16 Having already found differences between conditions among HOPE study participants, this analysis was designed to study the 2 intervention groups and 2 control groups to assess whether changes in network ties were associated with HIV prevention-related main outcomes among participants in the intervention group clusters.
Analysis
Descriptions of network metrics and social network terminology are included in Table 1. Network data were imported into NETDRAW 2.09026 to generate network visualizations.27 Degree centrality was used in regression analyses to determine whether an increase in network connectivity was associated with increased HIV prevention outcome measures. For each of the 4 individual clusters, we evaluated the effects of increasing network ties on the variables established a priori as main outcomes.21 Multiple logistic regression analysis with log odds/logit output was used to measure the relation between an increase in degree centrality from baseline to follow-up and likelihood of receiving an HIV test and following up for test results and whether participants posted on the Facebook group wall. Ordinary least squares regression analysis was used to measure the relation between an increase in degree centrality from baseline to follow-up and number of times participants used social networks to talk about sexual behaviors and partners.
TABLE 1—
Social Network Metrics Used in the Present Analysis: Harnessing Online Peer Education (HOPE) Intervention; Los Angeles, CA; September 2010–February 2011
| Social Network Metric | Definition |
| Node | An individual actor in a network (i.e., men who have sex with men in the intervention and control groups) |
| Isolate | A node not connected to any other nodes in the network |
| Ties | Connections between nodes in a network (i.e., “friend” relationships through Facebook) |
| Degree centrality | Number of connections from participant to other network members; rough measure of prestige or status |
| Density | The volume of connections in the network calculated by taking the number of ties between all nodes and dividing that number by the total number of possible ties |
| Average path length | The average distance between all reachable pairs of nodes in the network; used to understand how quickly information can diffuse through a network |
| Distance-based cohesion | Range = 0–1; larger values indicate greater cohesiveness |
All analyses included baseline measures of degree centrality as a covariate. We used Stata version 12 (StataCorp LP, College Station, TX) to complete statistical analyses.
RESULTS
Of the 112 baseline participants, 105 (93.8%) completed the follow-up survey, allowing us to analyze data on 105 participants from their baseline and follow-up surveys, HIV testing, likelihood of posting on the Facebook group walls, and social network changes. Participants were MSM, approximately 90% of whom were Latino or African American with an average age of 31 years.18
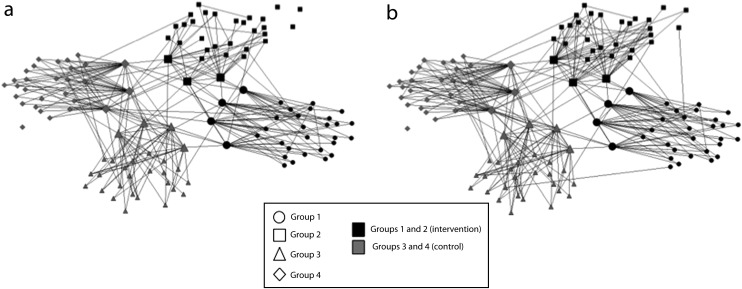
Figure 1 presents visual representations of each of the 4 groups at baseline and follow-up. A few features of these graphs are noteworthy. First, at baseline and follow-up, most ties within groups at both time points extend from peer leaders (represented by larger nodes) to participants (represented by smaller nodes). This was largely a result of study design. At baseline, study participants were “friended” by peer leaders, thereby establishing a connection to the study groups. However, there were more within-group ties both to peer leaders and to participants within groups at follow-up, indicating an increase in cross-participant connections and non–study-design-related connections between peer leaders and participants during the course of the intervention.
FIGURE 1—
Visual representations of each of the 4 social network groups at (a) baseline and (b) follow-up: Harnessing Online Peer Education (HOPE) intervention; Los Angeles, CA; September 2010–February 2011.
Note. Large nodes indicate that the individual was a peer leader. The sample size was n = 112.
A second feature of these networks was the interconnections among peer leaders both within groups and across groups and conditions. This was also an artifact of study design. The peer leaders were trained together within conditions, across groups. Moreover, trainings occurred across conditions at the same physical location at adjacent times of the day, allowing peer leaders in different conditions to meet and interact. The peer leaders were instructed not to disseminate intervention content across conditions during the study period, so these cross-condition ties do not represent opportunities for contamination.
Third, a few ties were documented between participants across groups and conditions at baseline. Most of the participants did not know one another, but some prestudy connections existed. The number of ties between conditions did increase slightly between baseline and follow-up. This may have introduced some pathways along which contamination could have occurred. Most between-groups ties, however, were between peer leaders and members of the other group in the same condition. Again, because these leaders were trained to not disseminate information across conditions, contamination seems unlikely.
Table 2 presents a comparison of network metrics across the 4 groups at baseline and follow-up. All peer leaders and most participants were retained within their groups from baseline to follow-up. Within-group ties increased across all 4 groups from baseline to follow-up; however, the magnitude of within-group ties was greatest in intervention group 2, in which ties increased from 69 at baseline to 117 at follow-up (70% increase). Average path length, the average distance between all reachable pairs in the network, decreased, indicating that the networks became more cohesive over time. These data mirror those from the network visualizations.
TABLE 2—
Comparison of Network Metrics Across Control and Intervention Groups at Baseline and Follow-Up: Harnessing Online Peer Education (HOPE) Intervention; Los Angeles, CA; September 2010–February 2011
| Intervention |
Control |
|||
| Metric | 1 | 2 | 3 | 4 |
| Baseline | ||||
| No. of isolates | 0 | 3 | 0 | 1 |
| No. of nodes | 31 | 31 | 28 | 29 |
| No. of peer leaders | 4 | 3 | 4 | 3 |
| No. of within-group ties | 97 | 69 | 88 | 77 |
| Density | 0.10 | 0.07 | 0.12 | 0.09 |
| Degree centrality | 0.12 | 0.08 | 0.13 | 0.14 |
| Average path lengtha | 2.241 | 2.319 | 2.229 | 2.047 |
| Distance-based cohesionb | 0.454 | 0.327 | 0.437 | 0.351 |
| Follow-up | ||||
| No. of isolates | 0 | 0 | 0 | 1 |
| No. of nodes | 31 | 30 | 28 | 29 |
| No. of peer leaders | 4 | 3 | 4 | 3 |
| No. of within-group ties | 106 | 117 | 103 | 115 |
| Density | 0.11 | 0.13 | 0.14 | 0.14 |
| Degree centrality | 0.13 | 0.14 | 0.15 | 0.15 |
| Average path lengtha | 2.184 | 2.009 | 2.037 | 1.856 |
| Distance-based cohesionb | 0.480 | 0.494 | 0.437 | 0.518 |
Note. All network metrics are normalized for comparison across networks. The sample size was n = 112.
For each pair of nodes, the algorithm finds the number of edges in the shortest path between them.
Range = 0–1; larger values indicate greater cohesiveness.
Table 3 shows the results of the relation between change in social network ties and the main outcome variables. Among the intervention group, we found a statistically significant positive relation between increase in network ties and use of social media to talk about sexual behaviors and partners (intervention group 2) and a positive trending relationship (P < .1) between increase in network ties and likelihood of testing for HIV (intervention group 1), follow-up for test results (intervention group 1), and participation in group discussions (intervention groups 1 and 2). We found no statistically significant differences among the control groups on any outcomes.
TABLE 3—
Relation Between Degree Centrality (Increased Social Network Ties) and Main HIV Outcomes Variables: Harnessing Online Peer Education (HOPE) Intervention; Los Angeles, CA; September 2010–February 2011
| Intervention |
Control |
|||
| Group 1 (n = 26), B (P) | Group 2 (n = 28), B (P) | Group 3 (n = 26), B (P) | Group 4 (n = 27), B (P) | |
| Tested and returned kita | 58.59 (.09) | 11.65 (.43) | . . . | . . . |
| Followed up for test resultsab | Predicts perfectly | . . . | . . . | . . . |
| Participated in group discussionsa | Predicts perfectly | 20.54 (.09) | 24.09 (.34) | −4.58 (.8) |
| Used social networks to talk about sexual behaviors | 7.18 (.48) | 4.86 (.003) | −7.34 (.56) | −4.41 (.69) |
Note. Analyses include baseline social network ties as a covariate. The sample size was n = 107.
Insufficient control group participants tested and returned kits and followed up for test results to calculate associations with increased degree centrality.
Predicts perfectly: every individual who had an increase in network degree followed up for test results and participated in group discussions, making statistical modeling impossible.
DISCUSSION
Among racial/ethnic minority MSM, peer-led online social media–based HIV prevention interventions can increase community cohesion, and these changes appear to be associated with important behavioral outcomes, such as increased HIV testing. The current results are important because they (1) describe the changing network characteristics (e.g., changes in number of connections) among racial/ethnic minority MSM participants in an online public health intervention; (2) present visualizations of participants’ changing network structure; (3) incorporate multiple sources of data, including self-reports, network data, and verifiable HIV testing endpoints; and (4) present an underlying framework suggesting that changes in online social network dynamics may affect the success of community-based interventions targeted toward MSM.
Participants in all 4 groups experienced an increase in the number of within-group ties, with intervention group 2 having the highest percentage of tie increases from baseline to follow-up (70%). Individuals who had changes in their network structures through increased ties generally were more likely to engage in HIV-related behavior change, including testing, follow-up for results, participation in community discussions, and use of social networks for sexual health communication. These trends were not found among control group communities. Although these findings were not statistically significant with a 2-tailed test, they suggested a positive relation between HIV prevention behavior change and change in social ties within an HIV prevention intervention. Figure 1 helps to present a few of these noteworthy changes in the network structures between time points. Initially, most of the ties were between only participants and their peer leaders, but at follow-up, additional ties were seen between participants.
Results suggest that content of communication matters when creating behavior change among online communities. In previous studies, we found that, as planned, HIV intervention participants engaged in a large number of HIV-related conversations and that those who discussed HIV prevention also were more likely to actually request an HIV test.20a These data build on those results by suggesting that HIV-related content might have spread as a function of increased participant social network ties, resulting in individual and group increases in HIV testing.
There has been increased interest in how social media and social networks can be used in the delivery of interventions and how these approaches can be leveraged toward improving intervention outcomes.14 Facebook and other social networking Web sites present a great opportunity for studying these processes because network connections in the form of “friends” are very explicit. Collecting data on these networks over time is far easier than in many field settings where verifying the identity of network ties can become very labor intensive and is often plagued by errors because of recall bias among participants.28 Network ties defined by friend status may lack some of the depth of content that other network studies use, such as “someone you go to for help or advice,” but their accuracy is high. As a result, we can have confidence in the changes observed over time in these structures and any associations such changes may have with health behaviors.
At an aggregate level, results suggest that online social networking communities can be more broadly used for public health interventions. Although this intervention was focused on HIV prevention and testing outcomes (and we therefore analyzed the relation between social network growth and HIV testing behaviors), we found that similar network growth appeared among both HIV intervention communities and general health–focused control group communities. For example, we found increased network cohesion (e.g., increased degree centrality, decreased average path length) among both intervention and control communities, suggesting that if we had analyzed the relation between network change and general health behaviors (i.e., outcomes related to the control group content), we might have found a relation among the control community participants. These results suggest that these findings might generalize outside of HIV prevention, such that social networking communities may be able to influence health behaviors in other areas of public health as well.
Limitations
The study had several limitations, primarily related to the small number of participants in each group. Initially, we had difficulties recruiting African American and Latino MSM into the study. We believe that this was a result of 2 main factors: (1) Facebook was just beginning to see rapid growth in racial/ethnic minority membership at the time of recruitment, and (2) our method for filtering duplicate respondents (nonunique usernames) reduced the sample size. Since the time of recruitment, social media technologies have rapidly grown in size among minority populations, making it easier to recruit at-risk participants. Additionally, although Internet studies have recruited large participant samples, many of these participants have been found to be duplicate respondents.29 To reduce duplicate respondents and increase data quality, we used Facebook Connect to ensure that participants were unique Facebook users. Although this filtering method increased the difficulty of recruiting participants and reduced the size of the sample, we believe that it is an important method in increasing data quality in Internet studies (for more detail on this approach, see Young4). Because this was a randomized controlled peer-led intervention among online communities, we created multiple intervention and control groups to reduce the possibility that a single peer leader might have accounted for differences within an intervention or a control condition. We therefore had limited data points and 1-tailed significance results on most regression analyses, because analyses were conducted within group rather than within condition. Although future research can evaluate best methods for analysis of online social network metrics, the results suggest the feasibility of this approach and present trends of a preliminary relation between increased online social network ties and HIV testing as a result of a diffusion of innovations intervention.
Data also were reduced as a result of intervention attrition from baseline to follow-up. However, we conducted an analysis that included both self-reported and objectively verifiable HIV testing endpoints and had very high rates of retention (more than 92% at follow-up), suggesting that this approach could lead to high data quality among larger participant samples. This study was the first to explore the influence of social network changes on behavior among an online community-based HIV prevention intervention; future research can address these limitations and build on the methods presented in this article.
Conclusions
Among racial/ethnic minority MSM, peer-led online social media HIV prevention interventions can increase community cohesion, and these network changes appear to be associated with increased HIV testing. Findings suggest that social media technologies can be used as platforms to rapidly spread HIV prevention information throughout participants’ social networks.
Acknowledgments
The authors wish to thank the National Institute of Mental Health for funding this study (S.D.Y.; K01 MH 090884), as well as UCLA CHIPTS and the UCLA AIDS Institute.
Human Participant Protection
This study was approved by the University of California, Los Angeles, and University of Southern California institutional review boards.
References
- 1.Hall HI, Song R, Rhodes P et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.HIV Epidemiology Program, Los Angeles County Department of Public Health. HIV/AIDS Surveillance Summary. January 2010:1–33. [Google Scholar]
- 3. HIV Epidemiology Program, Los Angeles County Department of Public Health. Special data run: Los Angeles. Los Angeles, CA: Los Angeles County Department of Public Health; 2008.
- 4.Young SD. Recommended guidelines on using social networking technologies for HIV prevention research. AIDS Behav. 2012;16:1743–1745. doi: 10.1007/s10461-012-0251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holloway IW, Cederbaum JA, Ajayi A, Shoptaw S. Where are the young men in HIV prevention efforts? Comments on HIV prevention programs and research from young men who sex with men in Los Angeles county. J Prim Prev. 2012;33(5-6):271–278. doi: 10.1007/s10935-012-0282-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogers E. Diffusion of Innovations. 4th ed. New York, NY: Free Press; 1995. [Google Scholar]
- 7.Maiorana A, Kegeles S, Fernandez P et al. Implementation and evaluation of an HIV/STD intervention in Peru. Eval Program Plann. 2007;30:82–93. doi: 10.1016/j.evalprogplan.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valente TW, Pumpuang P. Identifying opinion leaders to promote behavior change. Health Educ Behav. 2007;34(6):881–896. doi: 10.1177/1090198106297855. [DOI] [PubMed] [Google Scholar]
- 9.Kelly JA, St Lawrence JS, Diaz YE et al. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81(2):168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelly JA, Murphy DA, Sikkema KJ. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. Lancet. 1997;350(9090):1500–1505. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- 11.St Lawrence JS, Brasfield TL, Diaz YE, Jefferson KW, Reynolds MT, Leonard MO. Three-year follow-up of an HIV risk-reduction intervention that used popular peers. Am J Public Health. 1994;84(12):2027–2028. doi: 10.2105/ajph.84.12.2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amirkhanian YA, Kelly JA, Kabakchieva E et al. A randomized social network HIV prevention trial with young men who have sex with men in Russia and Bulgaria. AIDS. 2005;19(16):1897–1905. doi: 10.1097/01.aids.0000189867.74806.fb. [DOI] [PubMed] [Google Scholar]
- 13.Safren SA, O’Cleirigh C, Skeer MR et al. Demonstration and evaluation of a peer-delivered, individually-tailored, HIV prevention intervention for HIV-infected MSM in their primary care setting. AIDS Behav. 2011;15:949–958. doi: 10.1007/s10461-010-9807-8. [DOI] [PubMed] [Google Scholar]
- 14.Valente TW. Network interventions. Science. 2012;337:49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- 15.Smith KP, Christakis NA. Social networks and health. Annu Rev Sociol. 2008;34:405–429. [Google Scholar]
- 16.Young SD, Cumberland W, Sung-Jae L, Jaganath D, Szekeres G, Coates T. Social networking technologies as emerging tools for HIV prevention: a randomized controlled trial. Ann Intern Med. 2013;159:318–324. doi: 10.7326/0003-4819-159-5-201309030-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Facebook. 2012. Available at: http://www.facebook.com. Accessed December 12, 2012.
- 18.Young SD, Szekeres G, Coates T. The relationship between online social networking and sexual risk behaviors among men who have sex with men (MSM) PLoS One. 2013;8(5):e62271. doi: 10.1371/journal.pone.0062271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bull SS, Levine DK, Black SR, Schmiege SJ, Santelli J. A social media delivered sexual health intervention: a cluster randomized controlled trial. Am J Prev Med. 2012;43:467–474. doi: 10.1016/j.amepre.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20a.Young SD, Jaganath D. Online social networking for HIV education and prevention: a mixed-methods analysis. Sex Transm Dis. 2013;40(2):162–167. doi: 10.1097/OLQ.0b013e318278bd12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20b.Young SD, Jordan AH. The influence of social networking photos on social norms and sexual health behaviors. Cyberpsychol Behav Soc Netw. 2013;16(4):243–247. doi: 10.1089/cyber.2012.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaganath D, Gill HK, Cohen AC, Young SD. Harnessing Online Peer Education (HOPE): integrating C-POL and social media to train peer leaders in HIV prevention. AIDS Care. 2012;24(5):593–600. doi: 10.1080/09540121.2011.630355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young SD, Harrell L, Jaganath D, Cohen AC, Shoptaw S. Feasibility of recruiting peer educators for an online social networking-based health intervention. Health Educ J. 2013;72(3):276–282. doi: 10.1177/0017896912440768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. The Home Access HIV-1 Test System. 2012. Hoffman Estates, IL: Home Access Health Corporation.
- 24.Young SD, Jaganath D. Feasibility of using social networking technologies for health research among men who have sex with men: a mixed methods study. Am J Mens Health. 2014;8(1):6–14. doi: 10.1177/1557988313476878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borgatti SP. Centrality and network flow. Soc Networks. 2005;27(1):55–71. [Google Scholar]
- 26.Borgatti S. Cambridge, MA: Analytic Technologies; 2002. NETDRAW: Graph visualization software, version release 2.090. [Google Scholar]
- 27.Freeman LC. Visualizing social networks. J Soc Structure. 2000;1(1):4. [Google Scholar]
- 28.Rice E, Barman-Adhikari A, Milburn NG, Monro W. Position-specific HIV risk in a large network of homeless youths. Am J Public Health. 2012;102(1):141–147. doi: 10.2105/AJPH.2011.300295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pequegnat W, Rosser BRS, Bowen AM et al. Conducting Internet-based HIV/STD prevention survey research: considerations in design and evaluation. AIDS Behav. 2007;11:505–521. doi: 10.1007/s10461-006-9172-9. [DOI] [PubMed] [Google Scholar]