Abstract
Occult thyroid carcinoma is very common in the clinic and is generally divided into four groups. Here, we proposed two types of occult thyroid carcinoma as the fifth group. The first type was locoregional lymph node metastases from thyroid carcinoma, and the second type was distant organ metastases from thyroid carcinoma. The unique aspect of the fifth group was that the primary carcinoma of the fifth group was not finally found by pathological examination. To better understand the fifth group, we reported a typical case. Furthermore, we discussed the diagnostic criteria and procedures and the management of the fifth group of occult thyroid carcinoma.
Keywords: Occult thyroid carcinoma, thyroid cancer, thyroid microcarcinoma
Introduction
Occult thyroid carcinoma (OTC) has different identifications but is similar to papillary thyroid microcarcinoma (PTMC) [1]. Boucek et al divided OTC into four groups [2]. The first group is incidentally found in the thyroid gland after total thyroidectomy (TT) for benign disease [3] or at autopsy [4]. The second group is incidentally detected PTMC, mainly by ultrasonography [5], or by fine needle aspiration biopsy (FNAB) [6]. The third group is found with clinically apparent metastases of thyroid carcinoma, where the primary carcinoma is not detectable before surgery but found in the final histological specimen [7-9]. The fourth group is patients with ectopic thyroid tissue with clinical symptoms or with apparent metastases [10,11]. The differences between the four groups of OTC are the initial presentation and final detection of primary mass (Table 1). Besides these four groups, we propose another group of OTC (the fifth group). For the fifth group of OTC, thyroid gland is diagnosed benign disease according to pathological and imaging evaluations. However, the locoregional lymph nodes (the first type) or distant organs (the second type) are metastases from thyroid carcinoma, and the diagnostic procedures for these two types of OTC in the fifth group are proposed as follows: For the first type, thyroid is diagnosed as benign lesions after TT, and then central lymph nodes with metastases from thyroid carcinoma is detected after central lymph node dissection (CLND). Central lymph nodes are the most common metastasis region in the neck. It is easier to perform CLND than lateral lymph node dissection [12,13]. Thus central lymph nodes are taken as representatives of locoregional lymph nodes (Figure 1A). In the second type, a distant metastatic mass is presented before a primary mass of thyroid carcinoma. Therefore, the first step of the second type is to diagnose a distant mass as metastasis from thyroid carcinoma, and the second step is to diagnose thyroid as benign lesions or normality after TT (Figure 1B).
Table 1.
Comparison of five groups of occult thyroid carcinoma
| Groups | Subtypes | Initial presentation or diagnosis | Final detection of primary mass |
|---|---|---|---|
| First group | First type | Thyroidectomy for benign disease | Yes, by pathology |
| Second type | Autopsy | Yes, by pathology | |
| Second group | Imaging examination | Yes, by FNAB | |
| Third group | Apparent metastases | Yes, by FNAB or pathology | |
| Fourth group | Ectopic thyroid tissue with clinical symptoms or with apparent metastases | Yes, by FNAB or pathology | |
| Fifth group | First type | Benign thyroid lesion and lymph node metastases | Not found |
| Second type | Distant organs metastases | Not found |
Figure 1.
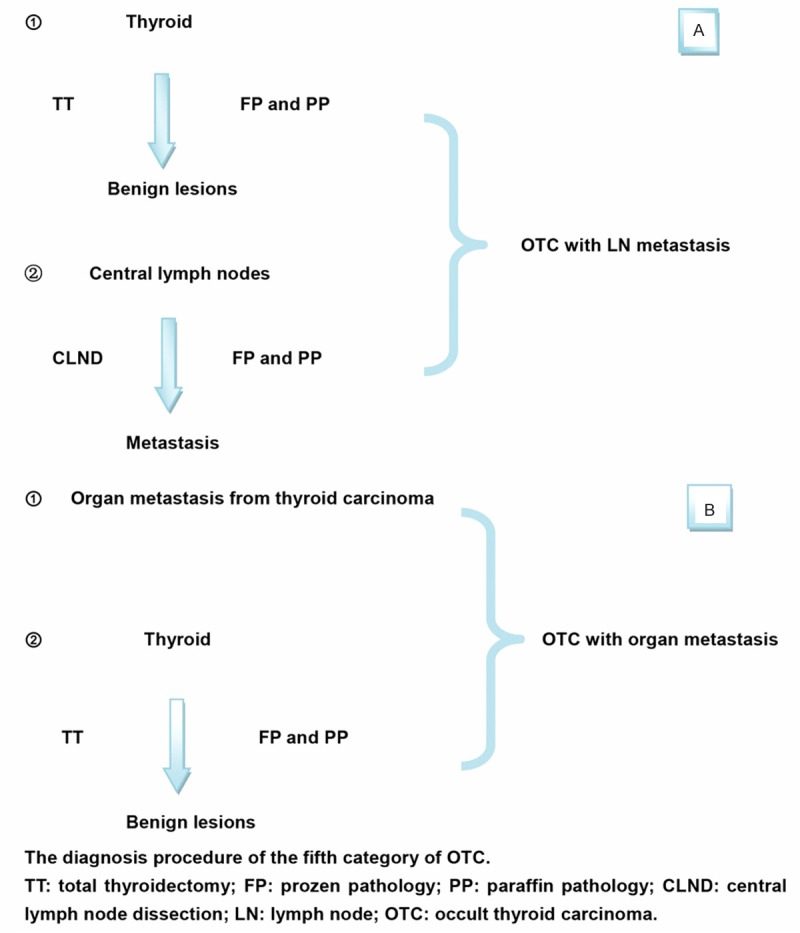
The diagnostic procedures for the fifth group of occult thyroid carcinoma. Part A is for the first type of the fifth group. The first step is to diagnose thyroid as benign lesions after TT; the second step is to prove central lymph nodes with metastases from thyroid carcinoma after CLND. Part B is for the second type. The first step is to diagnose a distant mass as metastasis from thyroid carcinoma; the second step is to diagnose thyroid as benign lesions or normality after TT.
Case report
According to literature, there is no case report meeting the diagnostic criterion of the fifth group of OTC. However, two cases of the first type of OTC with locoregional lymph nodes metastases were found in our hospital. Here we presented one case as an example. A 47-year-old man was admitted into our hospital for a big mass in the front of the neck. Preoperative thyroid ultrasonography showed that the right lobe was normal (Figure 2A), but in the left lobe several nodules were obvious and the biggest one was about 5×4×4 mm with several light spotting hyperechoic (Figure 2B). Intraoperative and postoperative pathological diagnosis showed that all of thyroid nodules were nodular goiters (Figure 2C), and an incidental resection lymph node near the left lobe metastasized from papillary thyroid carcinoma (Figure 2D). Two experienced pathologists examined serial sections of all nodules intraoperation and postoperation, but found no primary carcinoma. Therefore, we judged it as a typical case of the fifth group of OTC.
Figure 2.
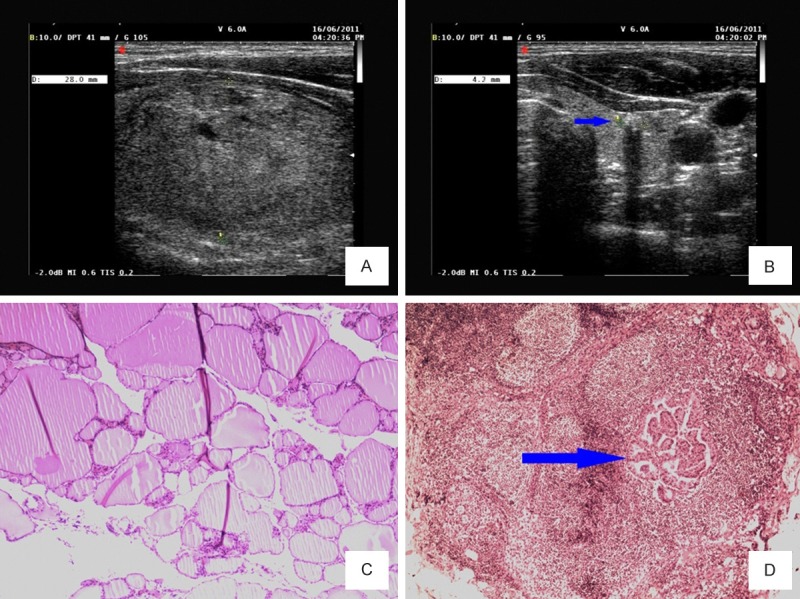
Ultrasonography and pathological images of a case diagnosed as the fifth group of occult thyroid carcinoma. A. The ultrasonography with a large nodule in the right lobe of thyroid. B. The ultrasonograph with a small nodule marked by the arrow in the left lobe. C. The pathological staining of nodular goiters. D. The pathological staining of lymph node with papillary thyroid carcinoma metastasis marked by the arrow.
Discussion
In this case report, we presented a typical case of the fifth group of OTC. We also postulated the second type of OTC with distant organs metastases. A few case reports showed that some OTC cases presented with distant organs metastases at first [7-9]. The difference between the third group of OTC proposed by Boucek and the second type of the fifth group is the final pathological diagnosis of the primary mass. The primary carcinoma of the third group is found in the final histological specimen, but the fifth group is not (Table 1). The process of metastasis takes some time [14]. It is usually easy to find the mass of primary thyroid carcinoma by pathological examination after distant metastases. Therefore, the second type of OTC is rare in the clinic. In summary, the fifth group of OTC must meet two criteria. First, the thyroid glands are benign disease according to pathological examination. Second, locoregional lymph nodes or distant organs are proved metastases from thyroid carcinoma according to pathological examination.
Why do we propose the fifth group of OTC in the clinic? First of all, because of limited time to examine serial frozen sections during operation, OTC is prone to be misdiagnosed. Second, differentiated thyroid carcinoma is easy to metastasis at early stage, 38-45% patients are identified with metastases undergoing prophylactic lymph node dissection [15,16]. The rate of lymph node metastasis could be 90% based on pathological and molecular examination [12]. However, in some cases, the primary carcinoma is still a small foci and easy to be missed by pathological examination. Therefore, it is very important to reduce false negatives of the fifth group of OTC by improving pathological and diagnostic methods. Cyclin D1 protein was overexpressed in 90.9% of metastasizing PTMC, but only in 8% of nonmetastasizing PTMC [17]. Immunohistochemistry analysis of cyclin D1 may be a valuable diagnosis tool of PTMC, which is likely to be the fifth group of OTC. In addition, the overexpression of S100A4 protein was associated with metastasis of PTMC [18,19]. Therefore, these molecular markers may provide a new way to improve the diagnosis of the fifth group of OTC.
For the management of the fifth group of OTC, if central lymph nodes dissection (CLND) is performed, and the lymph nodes are diagnosed without metastasis, the lymph node dissection is overtreatment and the complication will do harm to the patients. However, if CLND is not performed, the fifth group of OTC is easy to be misdiagnosed and the patients will suffer a lot because of inappropriate treatment and incorrect follow-up.
Central lymph nodes also known as VI lymph nodes lie in the paratracheal and front of the trachea [20]. The complications of CLND include: 1. the injury of recurrent laryngeal nerve; 2. the hypoparathyroidism because of incidental resection or damage to the blood supply of parathyroid. A retrospective study of 1,087 patients with PTC and clinical negative central lymph nodes showed no significant differences in the rate of transient and permanent recurrent laryngeal nerve injury among three groups (Group A, TT; Group B, TT and ipsilateral CLND; Group C, TT and bilateral CLND), but a higher rate of transient hypoparathyroidism in Group B and C and a higher rate of permanent hypoparathyroidism in Group C [21]. However, Shan et al reported no increased risk of recurrent laryngeal nerve injury and permanent hypocalcemia when CLND was performed in addition to TT [22]; 3. lymphatic leakage. Lorenz et al analyzed postoperative lymphatic leakage in 5800 cases after thyroid surgery, only 29 cases had lymph fistulas and 19 of them were successfully treated by fasting diet and medical treatment [23].
What are the benefits of CLND? First, CLND may reduce the false negatives for the diagnosis of the fifth group of OTC. Hughes et al reported that bilateral CLND upstaged 28.6% of PTC patients over the age of 45 to stage III disease [24]. Correct diagnosis and prognosis evaluation will benefit patients with appropriate treatment and follow-up. Second, CLND can decrease the risk of locoregional lymph nodes recurrence and the complications of reoperation [25]. Furthermore, Wong et al reported that prophylactic CLND for low-risk PTC became cost-effective 9 years after initial surgery and became cost-saving at 20 years if postoperative radioiodine use and/or permanent surgical complications were kept to a minimum [26].
In conclusion, we took a typical case as an example to propose the diagnostic criteria and procedures for the fifth group of OTC, and we discussed the cons and pros of CLND in the treatment of them. The complications of CLND are avoidable and acceptable. TT with CLND will not bring much more harm to patients than TT alone. On the other hand, CLND is helpful for the diagnosis, treatment and follow-up of the fifth group of OTC. Therefore, in our opinions, CLND should be performed together with TT. However, the incidence and characteristic of the fifth group of OTC is unclear and more studies are needed to better understand them.
Disclosure of conflict of interest
None.
References
- 1.Sobin L, Wittekind C. TNM Classification of Malignant Tumours. 6 edition. New York: Wiley-Liss; 2002. [Google Scholar]
- 2.Boucek J, Kastner J, Skrivan J, Grosso E, Gibelli B, Giugliano G, Betka J. Occult thyroid carcinoma. Acta Otorhinolaryngol Ital. 2009;29:296–304. [PMC free article] [PubMed] [Google Scholar]
- 3.Fink A, Tomlinson G, Freeman JL, Rosen IB, Asa SL. Occult micropapillary carcinoma associated with benign follicular thyroid disease and unrelated thyroid neoplasms. Mod Pathol. 1996;9:816–20. [PubMed] [Google Scholar]
- 4.Yamamoto Y, Maeda T, Izumi K, Otsuka H. Occult papillary carcinoma of the thyroid. A study of 408 autopsy cases. Cancer. 1990;65:1173–9. doi: 10.1002/1097-0142(19900301)65:5<1173::aid-cncr2820650524>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 5.Yuen AP, Ho AC, Wong BY. Ultrasonographic screening for occult thyroid cancer. Head Neck. 2011;33:453–7. doi: 10.1002/hed.21462. [DOI] [PubMed] [Google Scholar]
- 6.Kwak JY. Indications for Fine Needle Aspiration in Thyroid Nodules. Endocrinol Metab (Seoul) 2013;28:81–5. doi: 10.3803/EnM.2013.28.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pardal-de-Oliveira F, Vieira F. Occult papillary carcinoma of the thyroid gland with extensive osseous metastases-a case report with review of the literature. Pathol Res Pract. 1999;195:711–4. doi: 10.1016/S0344-0338(99)80065-X. discussion 5-6. [DOI] [PubMed] [Google Scholar]
- 8.Cavazza A, Roggeri A, Zini M, Rossi G, Zucchi L. Lymphangioleiomyomatosis associated with pulmonary metastasis from an occult papillary carcinoma of the thyroid: report of a case occurring in a patient without tuberous sclerosis. Pathol Res Pract. 2002;198:825–8. doi: 10.1078/0344-0338-00342. [DOI] [PubMed] [Google Scholar]
- 9.Lecumberri B, Alvarez-Escolá C, Martín-Vaquero P, Nistal M, Martín V, Riesco-Eizaguirre G, Sosa G, Pallardo LF. Solitary hemorrhagic cerebellar metastasis from occult papillary thyroid microcarcinoma. Thyroid. 2010;20:563–7. doi: 10.1089/thy.2010.0062. [DOI] [PubMed] [Google Scholar]
- 10.Kushwaha JK, Sonkar AA, Goel MM, Gupta R. Papillary carcinoma of thyroid arising from ectopic thyroid tissue inside branchial cleft cyst: a rare case. BMJ Case Rep. 2012:2012. doi: 10.1136/bcr.02.2012.5783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu JJ, Kwan K, Fung K. Papillary thyroid carcinoma in a lateral neck cyst: primary of ectopic thyroid tissue versus cystic metastasis. J Laryngol Otol. 2013;127:724–7. doi: 10.1017/S0022215113001205. [DOI] [PubMed] [Google Scholar]
- 12.Fritze D, Doherty GM. Surgical management of cervical lymph nodes in differentiated thyroid cancer. Otolaryngol Clin North Am. 2010;43:285–300. viii. doi: 10.1016/j.otc.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Nixon IJ, Shaha AR. Management of regional nodes in thyroid cancer. Oral Oncol. 2013;49:671–5. doi: 10.1016/j.oraloncology.2013.03.441. [DOI] [PubMed] [Google Scholar]
- 14.Klein CA. Selection and adaptation during metastatic cancer progression. Nature. 2013;501:365–72. doi: 10.1038/nature12628. [DOI] [PubMed] [Google Scholar]
- 15.Sywak M, Cornford L, Roach P, Stalberg P, Sidhu S, Delbridge L. Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery. 2006;140:1000–5. doi: 10.1016/j.surg.2006.08.001. discussion 5-7. [DOI] [PubMed] [Google Scholar]
- 16.Pereira JA, Jimeno J, Miquel J, Iglesias M, Munné A, Sancho JJ, Sitges-Serra A. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery. 2005;138:1095–100. doi: 10.1016/j.surg.2005.09.013. discussion 100-1. [DOI] [PubMed] [Google Scholar]
- 17.Khoo ML, Ezzat S, Freeman JL, Asa SL. Cyclin D1 protein expression predicts metastatic behavior in thyroid papillary microcarcinomas but is not associated with gene amplification. J Clin Endocrinol Metab. 2002;87:1810–3. doi: 10.1210/jcem.87.4.8352. [DOI] [PubMed] [Google Scholar]
- 18.Zou M, Al-Baradie RS, Al-Hindi H, Farid NR, Shi Y. S100A4 (Mts1) gene overexpression is associated with invasion and metastasis of papillary thyroid carcinoma. Br J Cancer. 2005;93:1277–84. doi: 10.1038/sj.bjc.6602856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Min HS, Choe G, Kim SW, Park YJ, Park do J, Youn YK, Park SH, Cho BY, Park SY. S100A4 expression is associated with lymph node metastasis in papillary microcarcinoma of the thyroid. Mod Pathol. 2008;21:748–55. doi: 10.1038/modpathol.2008.51. [DOI] [PubMed] [Google Scholar]
- 20.Iyer NG, Shaha AR. Central compartment dissection for well differentiated thyroid cancer and the band plays on. Curr Opin Otolaryngol Head Neck Surg. 2011;19:106–12. doi: 10.1097/MOO.0b013e328343af58. [DOI] [PubMed] [Google Scholar]
- 21.Giordano D, Valcavi R, Thompson GB, Pedroni C, Renna L, Gradoni P, Barbieri V. Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid. 2012;22:911–7. doi: 10.1089/thy.2012.0011. [DOI] [PubMed] [Google Scholar]
- 22.Shan CX, Zhang W, Jiang DZ, Zheng XM, Liu S, Qiu M. Routine central neck dissection in differentiated thyroid carcinoma: a systematic review and meta-analysis. Laryngoscope. 2012;122:797–804. doi: 10.1002/lary.22162. [DOI] [PubMed] [Google Scholar]
- 23.Lorenz K, Abuazab M, Sekulla C, Nguyen-Thanh P, Brauckhoff M, Dralle H. Management of lymph fistulas in thyroid surgery. Langenbecks Arch Surg. 2010;395:911–7. doi: 10.1007/s00423-010-0686-2. [DOI] [PubMed] [Google Scholar]
- 24.Hughes DT, White ML, Miller BS, Gauger PG, Burney RE, Doherty GM. Influence of prophylactic central lymph node dissection on postoperative thyroglobulin levels and radioiodine treatment in papillary thyroid cancer. Surgery. 2010;148:1100–6. doi: 10.1016/j.surg.2010.09.019. discussion 1006-7. [DOI] [PubMed] [Google Scholar]
- 25.White ML, Gauger PG, Doherty GM. Central lymph node dissection in differentiated thyroid cancer. World J Surg. 2007;31:895–904. doi: 10.1007/s00268-006-0907-6. [DOI] [PubMed] [Google Scholar]
- 26.Wong CK, Lang BH. A Cost-Utility Analysis for Prophylactic Central Neck Dissection in Clinically Nodal-Negative Papillary Thyroid Carcinoma. Ann Surg Oncol. 2014;21:767–77. doi: 10.1245/s10434-013-3398-3. [DOI] [PubMed] [Google Scholar]


