Abstract
Patient: Female, 74
Final Diagnosis: Recurrent cholangitis
Symptoms: —
Medication: —
Clinical Procedure: —
Specialty: Gastroenterology and Hepatology
Objective:
Unusual clinical course
Background:
Cholangitis may result from biliary obstruction (e.g., biliary or anastomotic stenosis, or foreign bodies) or occur in the presence of normal biliary drainage. Although reflux of intestinal contents into the biliary tree after hepaticojejunostomy appears to be a rare complication, it is important to emphasize that there are few available surgical therapeutic techniques.
Case Report:
A 74-year-old woman presented to our hospital after 17 years of episodes of cholangitis. The patient had undergone a pancreatoduodenectomy (Whipple procedure) 18 years earlier due to pancreatic adenocarcinoma. The reconstruction was achieved through the sequential placement of pancreatic, biliary, and retrocolic gastric anastomosis into the same jejunal loop. The postoperative course was uneventful and the patient received adjuvant chemotherapy. Approximately 6 months after the initial operation, the patient started having episodes of cholangitis. Over the next 17 years she experienced several febrile episodes presumed to be secondary to cholangitis. A computing tomography (CT) scan of the abdomen revealed intrahepatic bile ducts partially filled with orally administered contrast material (Gastrografin). Magnetic resonance cholangiopancreatography (MRCP) showed dilatation of the left intrahepatic bile ducts. A percutaneous transhepatic cholangiography showed that the bilioenteric anastomosis was normal, without stenosis. Based on these findings, a diagnosis of a short loop between the hepaticojejunostomy and the gastrojejunostomy permitting the reflux of intestinal juice into the biliary tree was made. During the re-operation, a new hepaticojejunal anastomosis in a 100-cm long Roux-en-Y loop was performed to prevent the reflux of the intestinal fluid into the biliary tree. The patient was discharged on postoperative day 10. One year after the second procedure, the patient enjoys good health and has been free of fever and abdominal pain and has not received any antibiotic therapy.
Conclusions:
Lengthening the efferent Roux-en-Y limb should be considered as a therapeutic option when treating a patient with recurrent episodes of cholangitis after hepaticojejunostomy.
MeSH Keywords: Anastomosis, Roux-en-Y – methods; Cholangitis – therapy; Pancreatic Neoplasms – pathology; Pancreatic Neoplasms – surgery
Background
Cholangitis may result from biliary obstruction (e.g., biliary or anastomotic stenosis, or foreign bodies) or occur in the presence of normal biliary drainage. Although reflux of intestinal contents into the biliary tree after hepaticojejunostomy appears to be a rare complication, it is important to emphasize that there are few available surgical therapeutic techniques.
Case Report
A 74-year-old woman presented to our hospital after 17 year of episodes of cholangitis.
The patient had undergone a pancreatoduodenectomy (Whipple procedure) 18 years earlier due to pancreatic adenocarcinoma. The reconstruction was achieved through the sequential placement of pancreatic, biliary, and retrocolic gastric anastomosis into the same jejunal loop. According to the pathology report, the tumor was a well differentiated pancreatic head adenocarcinoma invading the duodenal wall but without lymph node involvement (pT3N0M0) (Figure 1). The postoperative course was uneventful and the patient received adjuvant chemotherapy with 5 FU + Leucovorin (ESPAC I). Approximately 6 months after the initial operation, the patient started having episodes of cholangitis (sudden onset of rigors, abdominal pain, and fever). Over the next 17 years, she experienced several febrile episodes presumed to be secondary to cholangitis. During this period she was admitted to 3 hospitals on 7 separate occasions with fever, rigors, and abdominal pain. Blood cultures were performed on only 1 occasion and grew E. coli sensitive to Amoxicillin/Clavulanic acid, Loracarbef, Aztreonam, Imipenem/Cilastatin, Cefaclor, Cefprozil, Ciprofloxacin, and Trimethoprim + Sulfomethoxazol.
Figure 1.
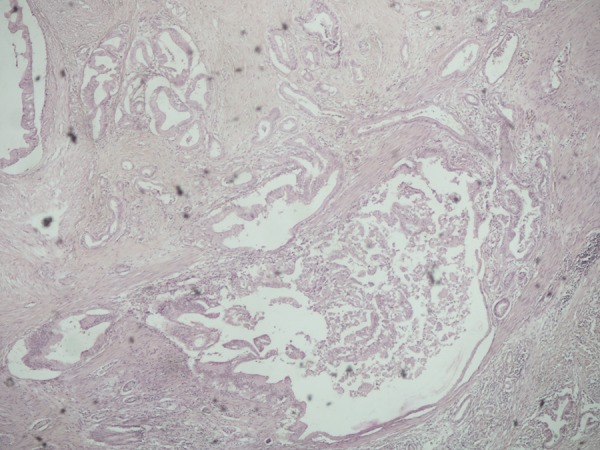
Pathology of the pancreatic tumor.
Results of laboratory studies were mostly normal except for a transiently increased alkaline phosphatase, and jaundice was absent.
In addition to these hospitalizations, the patient experienced several episodes of presumed cholangitis that were managed at an outpatient clinic with oral antibiotics. Repeatedly, she was placed on chronic suppressive oral antibiotic therapy with quinolones and/or amoxicillin/clavulanic acid, cycling every 1–2 months.
Fifteen years before this admission, the patient underwent an abdominal computed tomography (CT) scan, which revealed intrahepatic bile ducts partially filled with orally administered contrast material (Gastrografin). This finding was confirmed in a recent CT scan (Figure 2). Magnetic resonance cholangiopancreatography (MRCP) showed dilatation of the left intrahepatic bile ducts (Figure 3).
Figure 2.
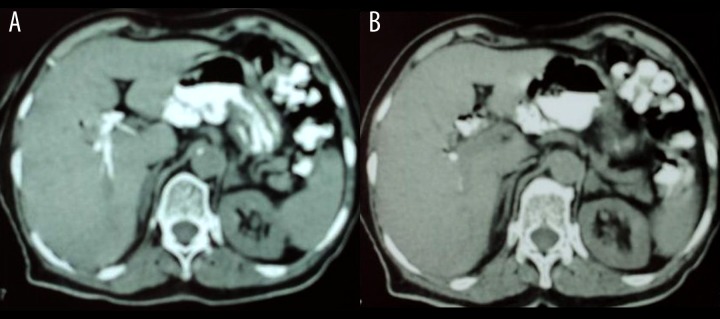
(A, B) CT scan of the patient showing the presence of orally administered Gastrografin into the biliary tree.
Figure 3.
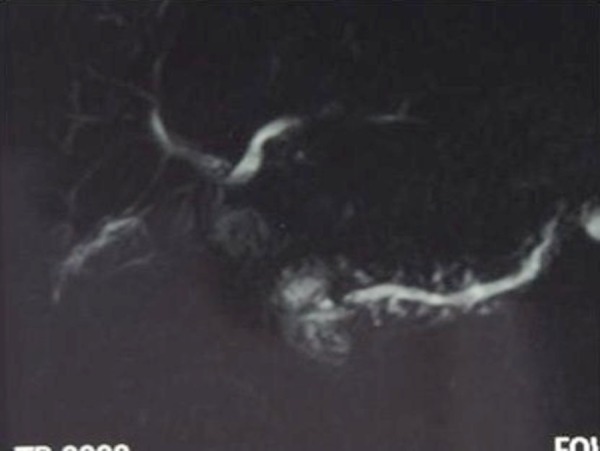
MRCP showing a possible dilatation of the left hepatic duct.
A percutaneous transhepatic cholangiography was performed to evaluate the biliary tract anatomy and place a stent in the anastomosis (Figure 4). This showed that the bilioenteric anastomosis was normal, without stenosis. Based on these findings a diagnosis of a short loop between the hepaticojejunostomy and the gastrojejunostomy permitting the reflux of intestinal juice into the biliary tree was made.
Figure 4.
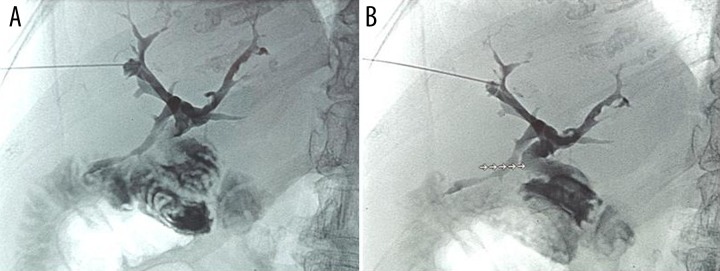
(A, B) Percutaneous transhepatic cholangiography revealing a hepaticojejunal anastomosis without stenosis (dotted arrow).
Operation
The operation was performed by a surgeon experienced in bilioenteric anastomosis. During the re-operation, no severe adhesions were found in the upper abdomen, the liver was fibrotic, and a suspicious lesion in the segment IV of the liver was sent for frozen section and it was found to be negative for tumor presence. The distance between the hepaticojejunostomy and the gastrojejunostomy was 30 cm and the hepaticojejunal anastomosis was normal, without stenosis. The hepaticojejunal anastomosis was taken down and the jejunal loop was cut 20 cm after the gastrointestinal anastomosis. A new hepaticojejunal anastomosis in a 100-cm long Roux-en-Y loop was performed to prevent the reflux of the intestinal fluid into the biliary tree (Figure 5). The patient was discharged on postoperative day 10.
Figure 5.
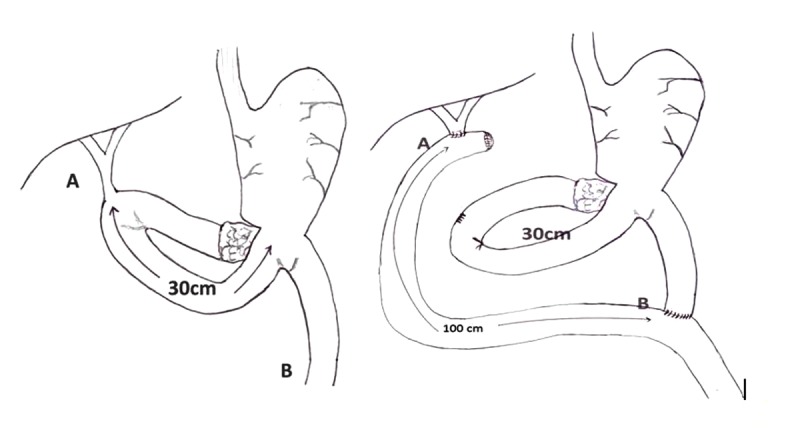
Hepaticojejunal anastomosis in a 100-cm long Roux-en-Y.
One year after the second procedure, the patient enjoys good health and has been free of fever and abdominal pain and has not received any antibiotic therapy. Her liver function test results are normal.
Discussion
Cholangitis may result from biliary obstruction (biliary or anastomotic stenosis, foreign bodies) or occur in the presence of normal biliary drainage [1,2].The incidence of anastomotic stricture following hepaticojejunostomy in experienced centers is 4–10% [3–5]. Anastomotic strictures account for the majority of long-term complications like hepatolithiasis, liver abscess, secondary biliary cirrhosis, and portal hypertension if left untreated. Infections in the setting of normal biliary drainage are rare. Orlando et al. [6] reported a single case of recurrent cholangitis after orthotopic liver transplantation (OLT) with a normal hepaticojejunal anastomosis. They proposed that a motility disorder might arise in the mobilized Roux-en-Y loop, allowing the intestinal contents to reflux, and performed an antireflux procedure that prevented further infections. Similarly Ducrotte et al. [7] described the motor patterns found in 2 patients with recurrent cholangitis episodes after Roux-en-Y hepaticojejunostomy. In the first patient, cholangitis was due to a stenosis of the anastomosis between the limb and the left intrahepatic bile duct, but motility of the limb, duodenum, and distal jejunum was normal. In the second patient, no anatomical explanation was found for cholangitis attacks. However, although the duodenal motor activity was normal, the motility of the limb and of the jejunum below the jejunojejunal anastomosis was grossly abnormal: permanent minute rhythm, phase Ills absent or rare and slowly propagated, which are all motor abnormalities that could promote bacterial overgrowth in the limb. Vrochides et al. reported on a patient with recurrent episodes of cholangitis in the presence of a normal hepaticojejunostomy after OLT [8]. The patient was successfully treated by lengthening the Roux-en-Y limb from 30 cm to 90 cm. They concluded that the episodes of cholangitis were the result of reflux of the gastrointestinal juice into the biliary tree.
Conclusions
In the present case, prior studies and PTC showed the absence of bile duct strictures. Particularly, the filling of the intrahepatic bile ducts with Gastrografin on CT scans confirmed the reflux of the intestinal contents into the biliary tree. The patient had been evaluated at 3 prior hospitals. Surgical intervention was not judged to be beneficial and symptomatic treatment followed by suppressive therapy with antibiotics was recommended. After the evaluation of the patient at our institution, particularly after the PTC findings, we were convinced that the episodes of cholangitis are due to reflux of intestinal contents into the biliary tree.
In this patient, the 30-cm long loop between the hepaticojejunostomy and the gastroenterostomy was inadequate to prevent the reflux of intestinal contents into the biliary tree. In a series of 41 patients with a 60-cm long Roux-en-Y jejunal loop after a variety of reconstructions, Collard and Romagnoli demonstrated the presence of refluxed bile in 17 (41%) patients [9]. They cured 2 patients with severe symptomatic bile re-flux by lengthening the Roux-en-Y loop from 60 cm to 110 cm. Although this cause of cholangitis appears to be a rare complication after hepaticojejunostomy, it is important to emphasize that there are available surgical therapeutic techniques. Lengthening the efferent Roux-en-Y limb should be considered as a therapeutic option when treating a patient who has recurrent episodes of cholangitis after hepaticojejunostomy.
Acknowledgments
The authors would like to thank the patient on whom this case report is based.
Footnotes
Competing interests
The authors declare that they have no competing interests.
References:
- 1.Chuang JH, Lee SY, Chen WJ, et al. Changes in bacterial concentration in the liver correlate with that in the hepaticojejunostomy after bile duct reconstruction: implication in the pathogenesis of postoperative cholangitis. World J Surg. 2001;25:1512–18. doi: 10.1007/s00268-001-0162-9. [DOI] [PubMed] [Google Scholar]
- 2.Lasnier C, Kohneh-Shahri N, Paineau J. Dysfonctionnement des anastomoses biliodigestives: à propos d’unesériechirurgicale de 20 cas. Revue de la littérature. Ann de Chirourgie. 2005;130:566–72. doi: 10.1016/j.anchir.2005.05.009. [in French] [DOI] [PubMed] [Google Scholar]
- 3.Stewart L, Way LW. Bile duct injuries during laparoscopic cholecystectomy.Factors that influence the results of treatment. Arch Surg. 1995;130:1123–29. doi: 10.1001/archsurg.1995.01430100101019. [DOI] [PubMed] [Google Scholar]
- 4.Casendes A, Navarrete C, Burdiles P, Yarmuch J. Treatment of common bile duct injuries during laparoscopic cholecystectomy: endoscopic and surgical management. World J Surg. 2001;25:1346–51. doi: 10.1007/s00268-001-0121-5. [DOI] [PubMed] [Google Scholar]
- 5.Davids PH, Tanka AK, Rauws EA, et al. Benign biliary strictures. Surgery or endoscopy? Ann Surg. 1993;217:237–43. doi: 10.1097/00000658-199303000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orlando G, Blairvacq JS, Otte JB, et al. Successfultreatmentof recurrent cholangitis after adult liver transplantation with a Tsuchidaantireflux valve. Transplantation. 2004;77:1307–8. doi: 10.1097/00007890-200404270-00033. [DOI] [PubMed] [Google Scholar]
- 7.Ducrotte P, Peillon C, Guillemot F, et al. Could recurrent cholangitis after Roux-en-Y hepaticojejunostomy be explained by motor intestinal anomalies? A manometric study. Am J Gastroenterol. 1991;86(9):1255–58. [PubMed] [Google Scholar]
- 8.Vrochides D, Fischer SA, Soares G, Morrissey PE. Successful treatment of recurrent cholangitis complicating liver transplantation by Roux-en-Y limb lengthening. Transpl Infect Dis. 2007;9(4):327–31. doi: 10.1111/j.1399-3062.2007.00221.x. [DOI] [PubMed] [Google Scholar]
- 9.Collard JM, Romagnoli R. Roux-en-Yjejunal loopandbilereflux. Am J Surg. 2000;179:298–303. doi: 10.1016/s0002-9610(00)00326-3. [DOI] [PubMed] [Google Scholar]


