Abstract
Background
The relationship between procedural relative value units (RVUs) for surgical procedures and other measures of surgeon effort are poorly characterized. We hypothesized that RVUs would poorly correlate with quantifiable metrics of surgeon effort.
Methods
Using the 2010 ACS-NSQIP database, we selected 11 primary CPT codes associated with high volume surgical procedures. We then identified all patients with a single reported procedural RVU who underwent non-emergent, inpatient general surgical operations. We used linear regression to correlate length of stay, operative time, overall morbidity, frequency of serious adverse events (SAEs), and mortality with RVUs. We used multivariable logistic regression using all pre-operative NSQIP variables to determine other significant predictors of our outcome measures.
Results
Among 14,481 patients, RVUs poorly correlated with individual length of stay (R2=0.05), operative time (R2=0.10), and mortality (R2=0.35). There was a moderate correlation between RVUs and SAEs (R2 =0.79), and RVUs and overall morbidity (R2=0.75). However, among low to mid-level RVU procedures (11 to 35) there was a poor correlation between SAEs (R2=0.15), overall morbidity (R2=0.05), and RVUs. On multivariable analysis, RVUs were significant predictors of operative time, length of stay, and SAEs (OR 1.06, 95%CI: 1.05–1.07), but RVUs were not a significant predictor of mortality (OR 1.02, 95%CI: 0.99–1.05)
Conclusion
For common, index general surgery procedures, the current RVU assignments poorly correlate with certain metrics of surgeon work, while moderately correlating with others. Given the increasing emphasis on measuring and tracking surgeon productivity, more objective measures of surgeon work and productivity should be developed.
Keywords: relative value units, operative time, length of stay, adverse events, morbidity and mortality
Introduction
Since the development of a fee-for-service model for determining Medicare reimbursement (1), relative value units (RVUs) have become a metric of physician work and productivity. Currently, the assignment of RVUs is under the discretion of a select committee known as the RUC (Relative Value Scale Update Committee) which has substantial influence in determining RVU levels. Moreover, this committee is constrained by Medicare budgetary restrictions which effectively force them to decrease the RVU levels of some services when it recommends raising the RVU level of other services. Consequently, the process of assigning RVUs is highly subjective and predisposed to significant external forces (2). Moreover, there is concern that RVU levels may not accurately reflect a surgeon's work, productivity, or "value" to his or her department, hospital or community.
Given the increasing emphasis on measuring and tracking surgeon productivity, we sought to determine if primary procedure RVUs among general surgical operations would correlate with other markers of surgeon work. As our main outcome variables we chose to analyze operative time, length of stay (LOS), and morbidity and mortality rates, since these are proxies for the physical and cognitive time invested by surgeons in the care of their patients. We hypothesized that there would be poor correlation between primary procedure RVUs and these endpoints.
Methods
The 2010 ACS-NSQIP database was queried for all patients who underwent non-emergent, inpatient, general surgical operations as defined by a LOS greater than or equal to one day. We identified frequently represented primary procedural RVUs to arrive at eleven commonly performed general surgical procedures that represented the full breadth of surgical complexity. As depicted in Table 1, in order to sample as diverse a group of procedures as possible across the RVU continuum, we included laparoscopic and open procedures, oncologic and non-oncologic procedures, and visceral vs. non-visceral procedures. To avoid skewing our data toward high volume, low RVU procedures, we chose to exclude appendectomy and cholecystectomy since these procedures appeared to dominant the dataset and therefore diluted the results and significance of other procedures. In addition, these two procedures were excluded to avoid possible heterogeneity in patient and procedure risk factors associated with emergent operations compared to elective procedures.
Table 1.
Case mix, operative time, length of stay (LOS), morbidity, and serious adverse events (SAE) by RVUs. Only patients with a single RVU coded were included (N=14481).
| RVU | CPT | Procedure | N(%) |
*Median LOS (IQR) |
*Median OR Time (IQR) |
Morbidity (%) |
SAE (%) |
Mortality (%) |
|---|---|---|---|---|---|---|---|---|
| 11.92 | 49560 | Repair of first abdominal wall hernia | 533 (4) | 2 (1–4) | 88.5 (57–128) | 11 | 3 | <1 |
| 15.85 | 19303 | Simple mastectomy | 639 (4) | 1 (1–2) | 89 (64–130) | 6 | 2 | <1 |
| 16.22 | 60240 | Total thyroidectomy | 1470 (10) | 1 (1-1) | 110 (83–145) | 2 | 1 | 0 |
| 18.1 | 43280 | Laparoscopic Nissen fundoplication | 1043 (7) | 2 (1–2) | 111 (84–151) | 4 | 3 | <1 |
| 22.59 | 44140 | Open partial colectomy | 1487 (10) | 5 (4–7) | 109 (82–147) | 23 | 14 | 2 |
| 26.42 | 44204 | Laparoscopic partial colectomy | 2245 (16) | 4 (3–5) | 128 (99–170) | 15 | 8 | <1 |
| 29.4 | 43644 | Laparoscopic roux-n-y gastric bypass | 6306 (44) | 2 (2) | 117 (88–152) | 5 | 3 | <1 |
| 35.14 | 43632 | Distal gastrectomy with gastrojejunostomy | 88 (1) | 7 (5–8) | 149 (115–190) | 20 | 11 | 3 |
| 39.01 | 47120 | Partial liver resection | 250 (2) | 4 (3–6) | 151 (113–201.5) | 25 | 22 | <1 |
| 44.18 | 43107 | Trans-hiatal esophagectomy | 19 (<1) | 9 (8–11) | 223 (194–281) | 32 | 21 | 5 |
| 52.84 | 48150 | Whipple | 401 (3) | 8 (7–11) | 351 (280.5–421) | 45 | 35 | 2 |
Only patients without any post-operative morbidity or mortality were included in these calculations.
To avoid possible confounding of our data from the effect of multiple procedures with overlapping and/or additive morbidities, we limited our cases to those where only one procedure was performed. We also excluded patients who were ASA 1 or ≥4 in order to reduce the impact of co-morbid disease on our observed outcome variables. We were not able to capture data on the variation in hospital re-admission or complications after 30 days by procedure or RVU level. We were not able to capture data on the number of postoperative visits or the generation of additional RVUs in the 90-day global period because of additional evaluation and management (E&M) coding or for the surgical management of postoperative complications.
Linear regression was used to correlate operative time and LOS with RVUs. For this part of our analysis, patients who experienced any post-operative morbidity or mortality were excluded since the type and severity of the morbidity could function as a modifier variable and affect operative time and LOS independent of RVU. Multivariable linear regression using all pre-operative NSQIP variables was then used to determine whether RVUs were significant predictors of these outcome variables. Descriptive statistics were used to analyze frequency of overall 30-day morbidity, SAEs, and mortality per primary procedural RVU. These outcomes were included as outcome variables in our analysis since the evaluation and management postoperative morbidity and mortality require time, work, and effort.
SAEs were defined as the presence of one or more of the following: organ space infection, wound dehiscence, septic shock, myocardial infarction, cardiac arrest, CVA, coma, renal failure, pneumonia, re-intubation, pulmonary embolism, or bleeding (3, 4). We also performed multivariable logistic regression using all pre-operative NSQIP variables, including RVUs, to determine if RVUs were significant predictors of overall morbidity, SAEs, and mortality. Missing variables were excluded, and statistical analyses were performed using STATA.
Because NSQIP patient information is de-identified, this study was exempt from University of California, Davis institutional review board approval.
Results
A total of 14,481 patients met inclusion criteria. The frequency of primary procedures and associated RVUs are depicted in Table 1. Laparoscopic Roux-en-Y gastric bypass was the most frequently performed procedure (44%), followed by laparoscopic (16%) and open (10%) partial colectomy.
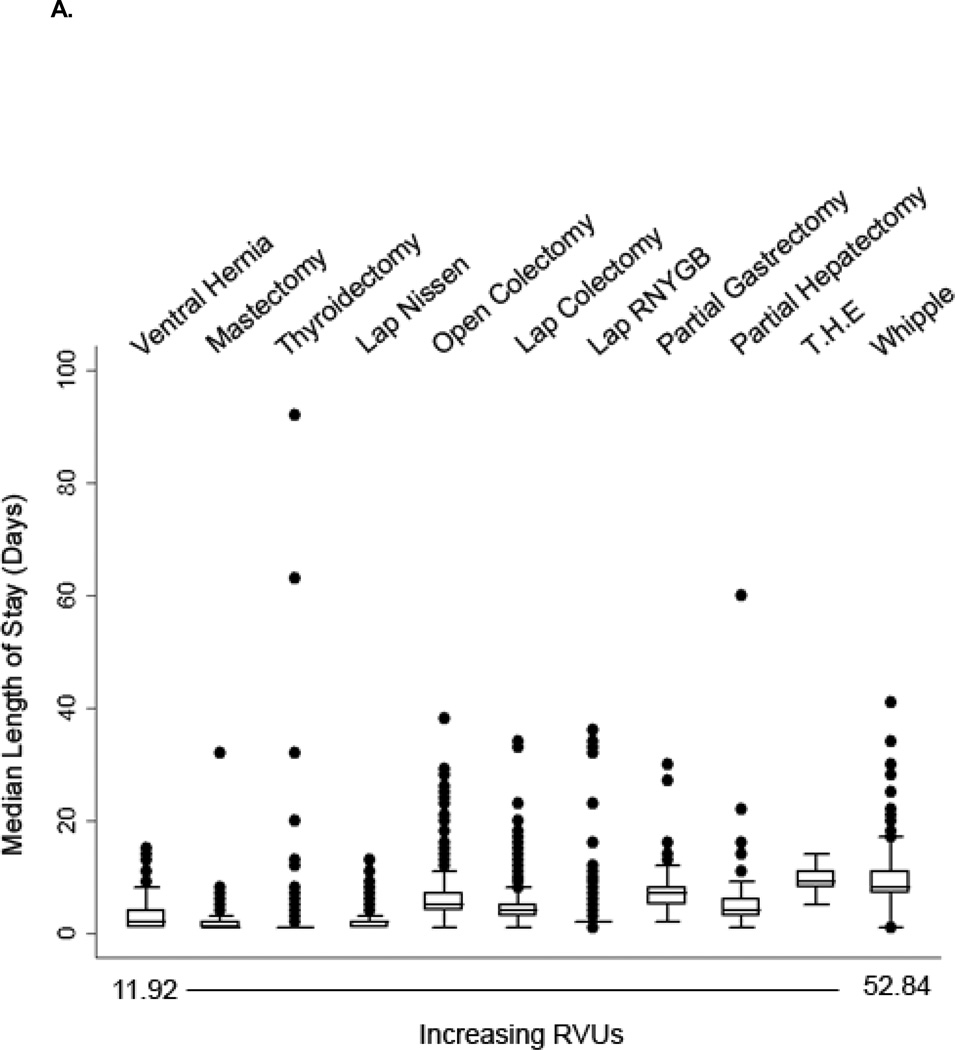
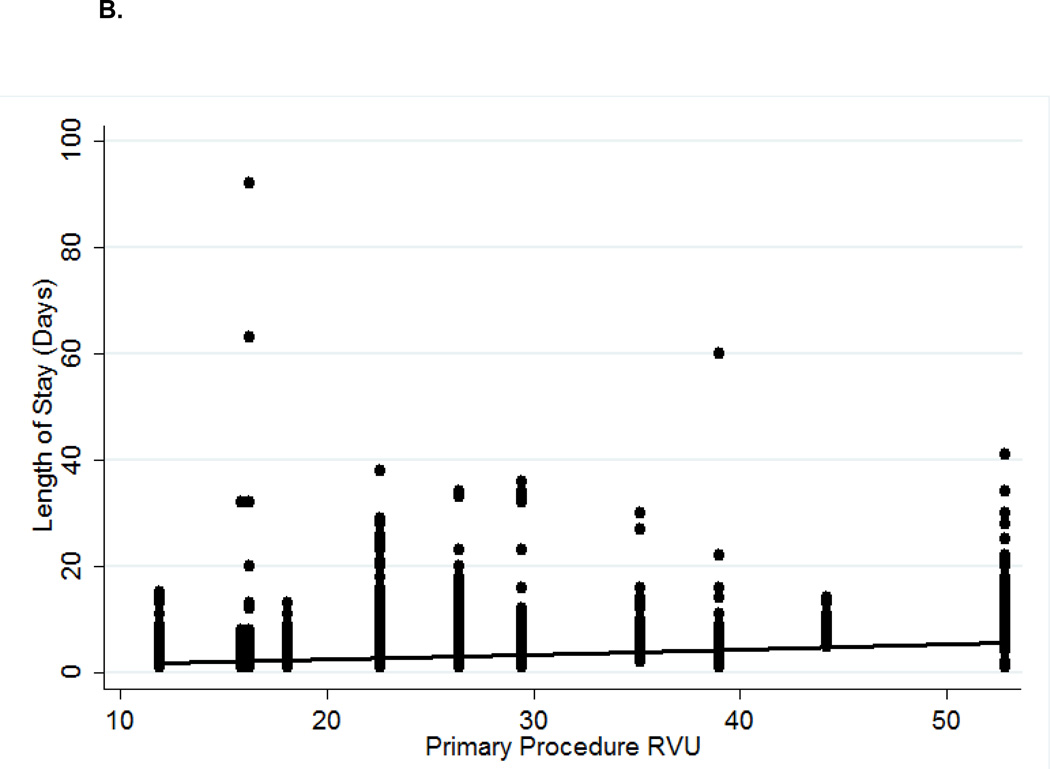
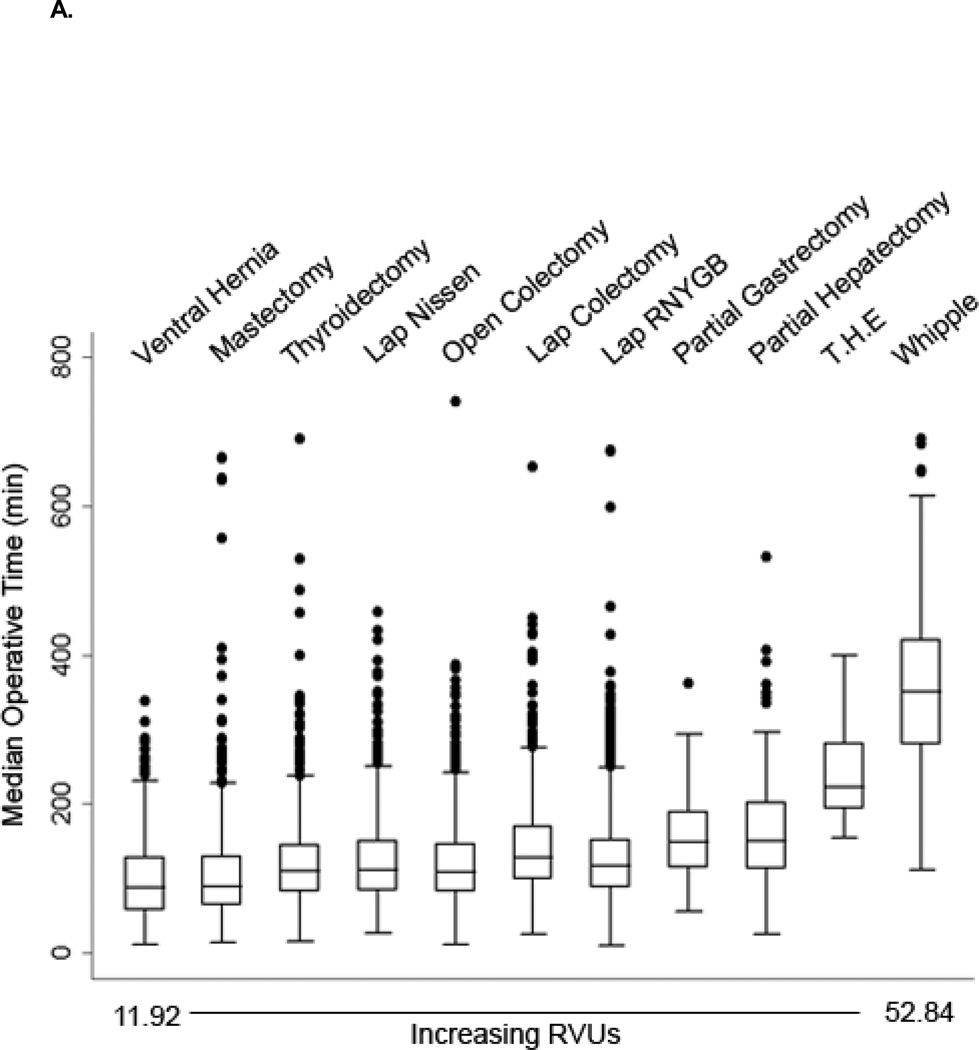
As depicted in Figures 1A and 2A, there was substantial variability in median LOS and median operative time, particularly among the low to mid-level RVU procedures (11 to 35). The median LOS for patients who did not experience any post-operative morbidity ranged from 1 (IQR: 1–2) day for thyroidectomy to 9 (IQR: 8–11) days for trans-hiatal esophagectomy. Median operative time was shortest for repair of abdominal wall hernia (88.5, IQR: 57–128) and longest for Whipple procedure (351, IQR: 280–421).
Figure 1.
A. Median length of stays in days (horizontal line) along with interquartile range (boxed region) per primary procedure RVU in patients with no 30-day post-operative complications. All other dots represent patient outliers. Abbreviations: RNYGB - roux-n-y gastric bypass, T.H.E - trans-hiatal esophagectomy.
B. RVU vs. individual length of stay (days) in patients with no 30-day post-operative complications.
R2=0.06
Figure 2.
A. Median operative time in minutes (horizontal line) along with interquartile range (boxed region) per primary procedure RVU in patients with no 30-day post-operative complications. All other dots represent patient outliers. Abbreviations: RNYGB - roux-n-y gastric bypass, T.H.E - trans-hiatal esophagectomy.
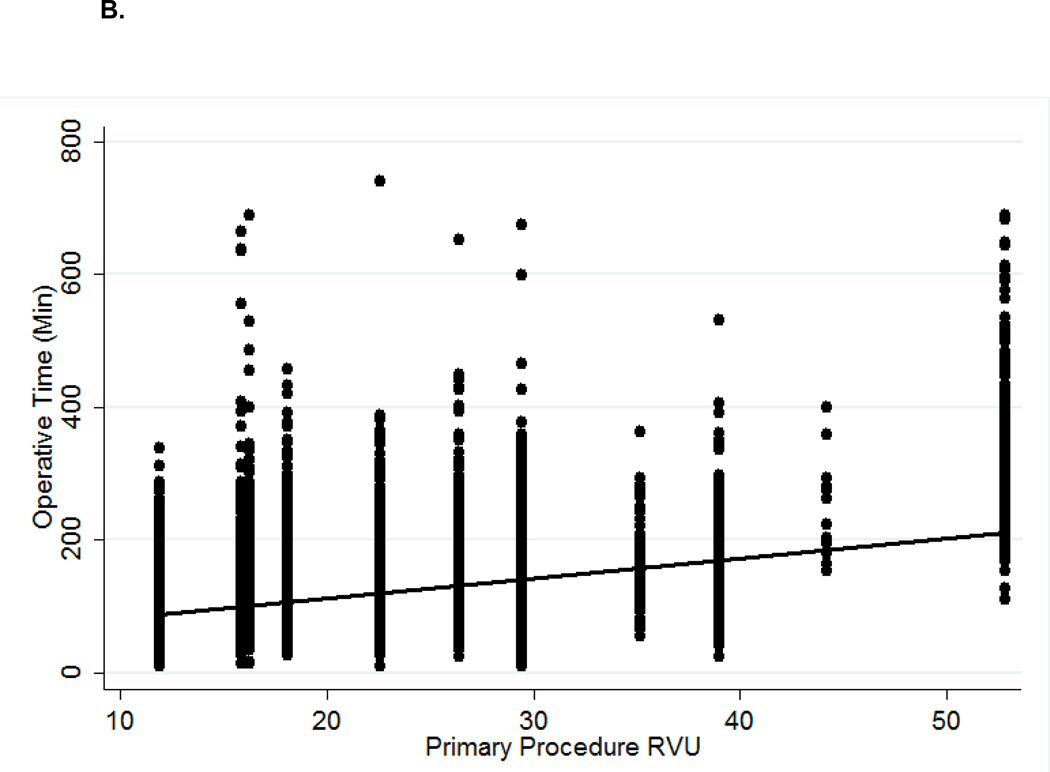
B. RVU vs. individual operative time (minutes) in patients with no 30-day post-operative complications.
R2=0.10
As depicted in Figures 1B and 2B, increasing RVUs poorly correlated with LOS (R2=0.06) and total operative time (R2=0.10) at the individual patient level. However, linear regression did reveal a relatively strong correlation when evaluating median LOS (R2=0.68) and median operative time (R2=0.76) at the aggregate procedural level. Among patients undergoing low to mid-level RVU procedures (11 to 35), the correlation with median LOS (R2=0.24) and median operative time (R2=0.66) became weaker. On multivariable linear regression (data not shown), RVUs were a statistically significant predictor of both operative time (p<0.001) and length of stay (p<0.001).
We also analyzed the correlation between RVU level and median LOS and operative time irrespective of whether post-operative morbidity occurred. We observed no significant differences in our results with poor correlation between RVU level and median LOS and operative time, particularly for low and mid-level RVU procedures. We then repeated our analyses after excluding laparoscopic gastric bypass operations. It is interesting to note that we did observe some differences in our results with this approach. For example, the correlation coefficients between RVUs and morbidity (R2=0.75), RVUs and mortality (R2=0.42), RVUs and serious adverse events (R2=0.74), RVUs and median length of stay (R2=0.77), and RVUs and median operative time (R2=0.68) were all improved.
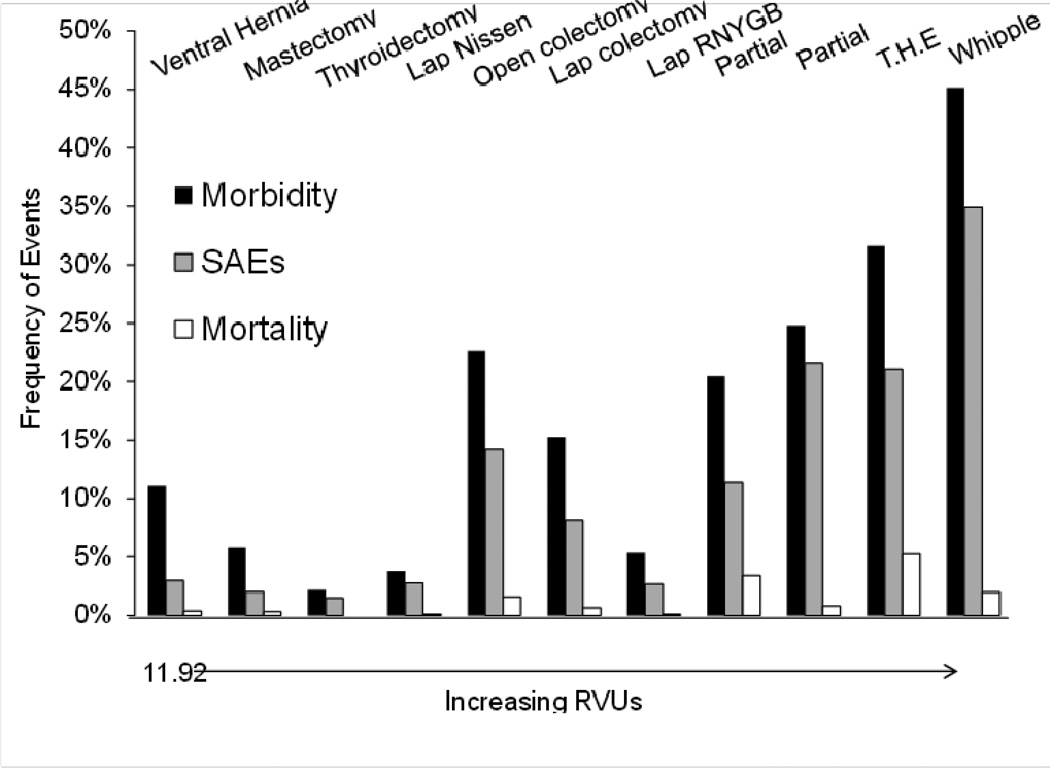
As depicted in Figure 3, there was substantial variation in 30-day overall morbidity and frequency of SAEs between procedure RVUs, especially among mid-level (11 to 35) RVU procedures. For example, the lowest RVU procedure, repair of abdominal wall hernia was associated with greater 30-day overall morbidity (11%) than simple mastectomy (6%), total thyroidectomy (2%), laparoscopic Nissen fundoplication (4%), and laparoscopic Roux-en-Y gastric bypass (5%). In addition, laparoscopic Roux-en-Y gastric bypass, despite having one of the higher RVU designations, had one of the lowest rates of post-operative morbidity, frequency of SAEs, and mortality. These rates were substantially lower than laparoscopic partial colectomy, which is assigned 3 fewer RVUs (an approximately 10% difference) by the current system.
Figure 3.
Frequency of overall 30-day morbidity, serious adverse events (SAEs), and mortality by procedure RVU. Abbreviations: RNYGB - roux-n-y gastric bypass, T.H.E - trans-hiatal esophagectomy.
There was a trend towards increasing morbidity and frequency of SAEs with procedures assigned RVUs greater than 35. For example, Whipple procedure (52.8 RVUs) had the highest 30-day overall morbidity and frequency of SAEs (45% and 35%, respectively), while trans-hiatal esophagectomy (44.2 RVUs) had the second highest (32% and 21%, respectively), and partial hepatectomy (39 RVUs) had the third highest (25% and 22% respectively).
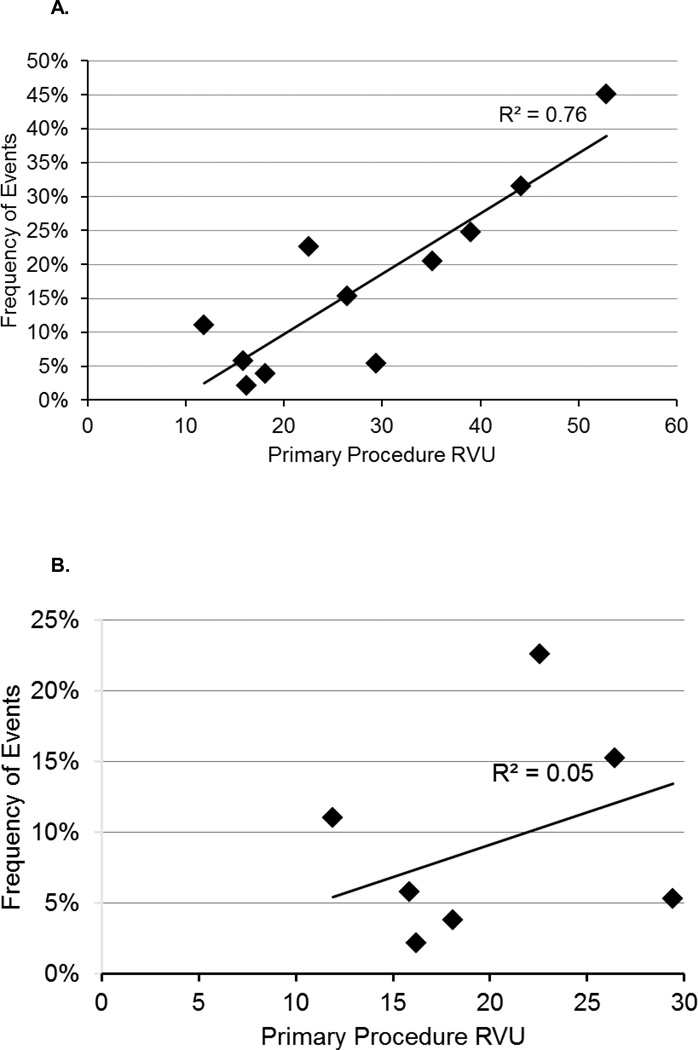
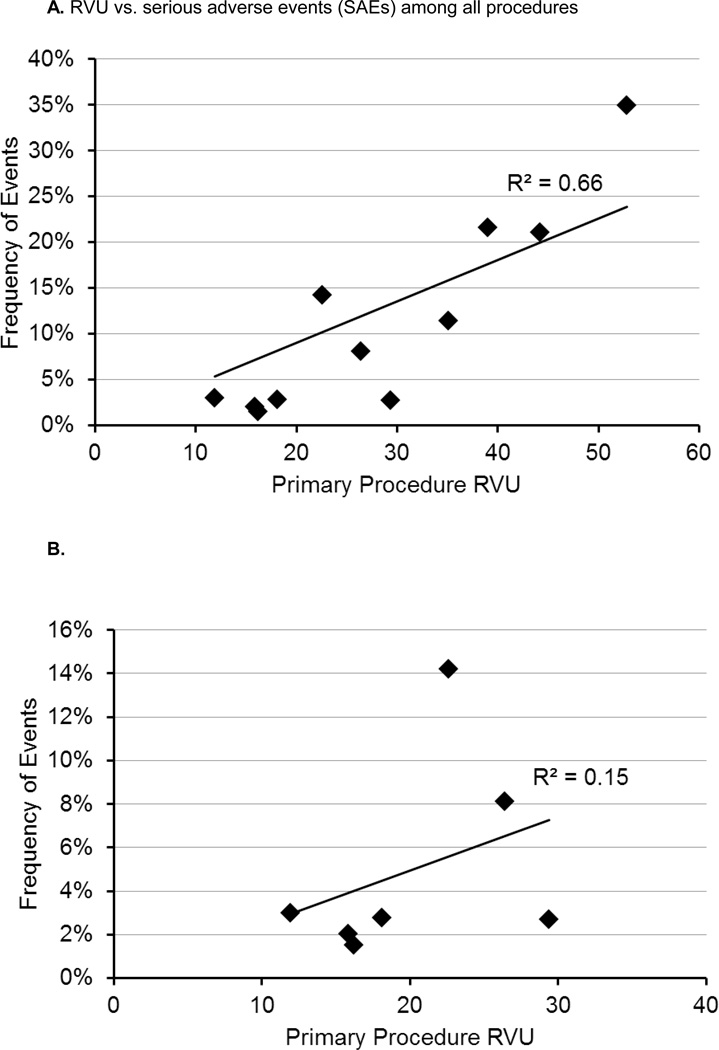
On regression analysis, among the entire spectrum of procedures, there was a moderate correlation between RVUs and overall morbidity (R2=0.75) and SAEs (R2=0.79), as shown in Figures 4A and 5A. However, similar to median LOS and median operative time, among the low to mid-level RVUs (11 to 35) there was a much weaker correlation between RVUs and overall morbidity (R2=0.05) and SAEs (R2=0.15), as depicted in Figures 4B and 5B.
Figure 4.
A. RVU vs. overall morbidity among all procedures
B. RVU vs. overall morbidity among low to mid-level RVU (11 to 35) procedures.
Figure 5.
A. RVU vs. serious adverse events (SAEs) among all procedures
B. RVU vs. serious adverse events (SAEs) among low to mid-level RVU (11 to 53) procedures.
Although postoperative mortality rates were overall low, the highest rates were observed among trans-hiatal esophagectomy (5%), distal gastrectomy (3%), partial colectomy (2%), and Whipple procedure (2%). These mortality rates also correlated relatively poorly with increasing RVU levels (R2=0.36).
On multivariable analysis (data not shown) RVUs were a statistically significant predictor of SAEs (OR 1.06, 95%CI: 1.05–1.07), but not mortality (OR 1.02, 95%CI: 0.99–1.05).
Discussion
Limited data exist validating the assumption that RVUs proportionately and accurately reflect the time and work required by surgeons to provide complete care to their patients. Resnick et al (5) demonstrated the substantial disconnect between revenues generated and RVUs reported by the thoracic and transplant services; thus highlighting the misrepresentation of surgeon value to a hospital based solely on reported work RVUs. Little et al (6) demonstrated a relatively linear relationship between RVU and mean operative time among outpatient pediatric general surgery, urologic, and minimally invasive procedures. However, there was substantial variability in the mean operative time among the low to mid-level RVU procedures. In addition, the authors did not evaluate the relationship between RVUs and other outcome measures such as post-operative LOS and/or morbidity and mortality. In a separate analysis, Nguyen et al (7) observed that RVUs were an independent risk factor for the occurrence of post-operative morbidity. However, these authors chose to analyze RVU levels from combined procedures, and this approach may have biased their analysis toward combined procedures which are expected to have prolonged operative time and LOS by definition. In addition, a large proportion of these combined procedures were the product of multiple surgeons, thereby obscuring the relationship between RVUs and other metrics of individual surgeon work.
Our study demonstrates that RVUs appear to poorly correlate with individual operative time and patient LOS. Since there are multiple factors which may contribute to operative time, including surgeon experience, surgeon proficiency, and patient factors such as obesity, we further analyzed the relationship of RVUs with median operative time. Although we observed a stronger correlation between RVUs and median operative time (R2 =0.78), among the low to mid-level (11 to 35) RVU procedures, the correlation was weaker (R2=0.66).
Our data also demonstrated that RVUs only moderately correlated with morbidity and SAEs. However, as with median operative time and length of stay, among lower to mid-level (11to 35) RVU procedures, this correlation remained weak. It is possible that with a different case mix, biased towards higher RVU procedures, we may have observed a stronger overall correlation between RVUs, morbidity and SAEs. In addition, with the lower proportion of high RVU procedures in our study, our reported morbidity and SAE rates for these procedures may accurately represent national trends. However, our reported morbidity and SAEs rates for transhiatal esophagectomy (8, 9), Whipple (10), and partial distal gastrectomy (11) are similar to what have been reported in the literature, making this less likely.
We acknowledge that selection bias is an important limitation to our study. However, this is partially reflective of the inherent selection bias within the NSQIP dataset since not all reported cases are represented and the frequency of reported procedures can vary year to year. Within our dataset, laparoscopic Roux-en-Y gastric bypass represented 44% of our total cases. This strong bias towards bariatric operations within our data set is reflective of national trends (12). Thus, we felt obligated to include this operation within our case mix. However, while appendectomies and cholecystectomies also comprise a large proportion of surgeon work load, we did not include these operations in our analysis to minimize a skewed distribution towards lower RVU and potentially less morbid procedures. Given our negative hypothesis, we wanted to maximize our ability to identify any positive correlations between RVUs and our outcome measures. It is possible that with a different case mix may, we may have observed different results. This could be evaluated in a follow up study.
Finally, our outcome measures are metrics that primarily quantify surgeon time spent as a representation of actual work performed. However, we acknowledge they are also not ideal markers to measure surgeon productivity since were unable to track the amount of procedures performed by a surgeon within a time period. It is possible that skilled and experienced surgeons can perform a particular operation faster, more frequently, and with less associated morbidity than other less experienced surgeons, and thus be more productive while working the same amount of time. Despite this potential inverse relationship between operative time and surgeon work, we felt that outcome variable was an important objective metric to use since it is one of the criteria used by the RUC to determine RVUs (13). However, the RUC primarily uses survey data, which are highly subjective, to estimate operative time.
In addition, there are other less easily quantifiable factors that comprise surgeon work that are not abstracted by NSQIP. These include time spent in pre-operative activities such as counseling, operative planning, committee work, and especially administrative work which has increased substantially, comprising 10 to 15% of surgeon work (14). Among surgeons at academic centers, medical education and outreach activities are still not represented in RVU productivity despite attempts to develop metrics for such activities (15). These activities may comprise a significant portion of surgeon work that may strengthen or weaken the correlation of RVUs with surgeon work for which we are unable to control in our dataset.
In summary, our data indicate that the current RVU based system poorly correlates with certain metrics of surgeon work, while moderately correlating with others. Given the increasing emphasis on measuring and tracking surgeon productivity, more objective measures of surgeon work and productivity should be developed.
Footnotes
Author Contributions
D.R. Shah – conception and design, analysis and interpretation of data, writing the article
R.J. Bold – critical revision of the article
A.D. Yang – critical revision of the article
V.P. Khatri – critical revision of the article
S.R. Martinez – critical revision of the article
R.J. Canter – conception and design, analysis and interpretation of data, writing the article, critical revision of the article
Presented in part as oral presentation at the 2014 Academic Surgical Congress 9th Annual Meeting, February 4–6th in San Diego, CA.
References
- 1.Hsiao WC, Yntema DB, Braun P, Dunn D, Spencer C. Measurement and analysis of intraservice work. JAMA : the journal of the American Medical Association. 1988;260:2361–2370. [PubMed] [Google Scholar]
- 2.Beyer DC, Mohideen N. The role of physicians and medical organizations in the development, analysis, and implementation of health care policy. Seminars in radiation oncology. 2008;18:186–193. doi: 10.1016/j.semradonc.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Ehlert BA, Durham CA, Parker FM, Bogey WM, Powell CS, Stoner MC. Impact of operative indication and surgical complexity on outcomes after thoracic endovascular aortic repair at National Surgical Quality Improvement Program Centers. Journal of vascular surgery. 2011;54:1629–1636. doi: 10.1016/j.jvs.2011.05.116. [DOI] [PubMed] [Google Scholar]
- 4.Ingraham AM, Cohen ME, Ko CY, Hall BL. A current profile and assessment of north american cholecystectomy: results from the american college of surgeons national surgical quality improvement program. Journal of the American College of Surgeons. 2010;211:176–186. doi: 10.1016/j.jamcollsurg.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Resnick AS, Corrigan D, Mullen JL, Kaiser LR. Surgeon contribution to hospital bottom line: not all are created equal. Ann Surg. 2005;242:530–537. doi: 10.1097/01.sla.0000184693.61680.24. discussion 537–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Little DC, St Peter SD, Calkins CM, Shah SR, Murphy JP, Gatti JM, Gittes GK, Sharp RJ, Andrews WS, Holcomb GW, 3rd, Ostlie DJ, Snyder CL. Relative value units correlate with pediatric surgeons' operating time: when perceived myth becomes reality. Journal of pediatric surgery. 2006;41:234–238. doi: 10.1016/j.jpedsurg.2005.10.044. discussion 234–238. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen KT, Gart MS, Smetona JT, Aggarwal A, Bilimoria KY, Kim JY. The relationship between relative value units and outcomes: a multivariate analysis of plastic surgery procedures. Eplasty. 2012;12:e60. [PMC free article] [PubMed] [Google Scholar]
- 8.Shah DR, Martinez SR, Canter RJ, Yang AD, Bold RJ, Khatri VP. Comparative morbidity and mortality from cervical or thoracic esophageal anastomoses. Journal of surgical oncology. 2013;108:472–476. doi: 10.1002/jso.23423. [DOI] [PubMed] [Google Scholar]
- 9.Connors RC, Reuben BC, Neumayer LA, Bull DA. Comparing outcomes after transthoracic and transhiatal esophagectomy: a 5-year prospective cohort of 17,395 patients. Journal of the American College of Surgeons. 2007;205:735–740. doi: 10.1016/j.jamcollsurg.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Behrman SW, Rush BT, Dilawari RA. A modern analysis of morbidity after pancreatic resection. The American surgeon. 2004;70:675–682. discussion 682–673. [PubMed] [Google Scholar]
- 11.Degiuli M, Sasako M, Calgaro M, Garino M, Rebecchi F, Mineccia M, Scaglione D, Andreone D, Ponti A, Calvo F. Morbidity and mortality after D1 and D2 gastrectomy for cancer: interim analysis of the Italian Gastric Cancer Study Group (IGCSG) randomised surgical trial. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology. 2004;30:303–308. doi: 10.1016/j.ejso.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 12.Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J. Trends in use of bariatric surgery, 2003–2008. Journal of the American College of Surgeons. 2011;213:261–266. doi: 10.1016/j.jamcollsurg.2011.04.030. [DOI] [PubMed] [Google Scholar]
- 13.McCall N, Cromwell J, Braun P. Validation of physician survey estimates of surgical time using operating room logs. Medical care research and review : MCRR. 2006;63:764–777. doi: 10.1177/1077558706293635. [DOI] [PubMed] [Google Scholar]
- 14.Satiani B. Use, misuse, and underuse of work relative value units in a vascular surgery practice. Journal of vascular surgery. 2012;56:267–272. doi: 10.1016/j.jvs.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Berger JR, Maher RF., Jr An innovative approach for calculating the work relative value units of clinical activities otherwise concealed. Academic medicine : journal of the Association of American Medical Colleges. 2011;86:853–857. doi: 10.1097/ACM.0b013e31821deade. [DOI] [PubMed] [Google Scholar]