Abstract
Objective
To determine what if any changes occur to the lumbar discs in the spine after prolonged sitting with and without intermittent breaks during a four hour time period.
Designy
A prospective observational study
Setting
An academic outpatient clinic
Methods
The measurement of lumbar disc changes was performed on twelve subjects following an analysis of a midsagittal lumbar magnetic resonance image (MRI) scan: measuring lumbar disc height and disc diameter. Scanning and analysis were done over a two day period: day 1 at the start of the work day and four hours later after continuous sitting; at the start of work day 2 and after four hours following a change in position and stretching protocol every 15 minutes.
Results
For this study, we first evaluated each level of the lumbar spine for any changes after prolonged sitting for four hours over the two days. Multiple comparisons bias was eliminated by a Bonferroni correction to limit the overall experiment wise error rate to 0.05. The comparison was conducted by using a paired t-test when the normality condition was satisfied and using a Wilcoxon signed rank test when normality was not satisfied. To test for normality a Shapiro-Wilk test was used. We found that for disc height, L4-5 was significantly decreased at the end of the sitting on day 1, but not for day 2. There were no significant height changes for the other lumbar discs. Additionally, for disc diameter, there were no significant differences present for any of the discs.
Conclusions
Analysis of the data shows the greatest change in disc height is at the L4-5 level after prolonged sitting without intermittent breaks. The other levels did not show significant change in their height. The findings also show the L4-5 height changes are not significant with brief positional changes every 15 minutes. Fewer changes in disc height may correlate with an improvement in low back pain and disability.
INTRODUCTION
Low back pain is a very common condition that affects millions of Americans. It is estimated that upwards of 85% of all individuals will experience an episode of low back pain during their lifetime. [1, 2] The duration of pain may vary from a few days to decades. The pain may impact one's function and become debilitating. The disability suffered from low back pain affects individuals and society. It is estimated that low back pain costs the United States 78 billion dollars in both direct and indirect costs on a yearly basis. [3-7]
As the economy and workforce moves from a manufacturing based economy and towards a service based economy, sedentary based jobs have increased. The sedentary worker is more stationary and less active. The sedentary job typically involves the majority of the day seated in front of a computer or workstation. Multiple studies have shown that prolonged sitting can lead to increased low back pain. [8-9] The static seating position has been shown to lead to an increase in intra-discal pressure, and the increased pressures have been shown to lead to disc bulges, protrusions and potentially herniations. [10-13] Additional studies have evaluated the ensuing degenerative cascade which leads to further degenerative changes including ligamentous hypertrophy, facet arthritis and stenosis. [14-21]
The effects of prolonged sitting and potential changes in disc anatomy have also been studied. [22] Further research has also examined the effects of dynamic stimuli and different sitting postures on low back pain. [23-25]. However, very limited research has examined the changes in lumbar disc height with sitting. [26] The intent of this study is to evaluate each level of the lumbar spine for any changes with prolonged sitting for a four hour period. This time period is during the morning part of the typical sedentary eight hour work day. This four hour am period was studied since research has shown on average a 10.6% gain in disc volume overnight with bed rest and Maximal stress of the intervertebral disc is also felt to occur in the am period , with higher intradiscal pressures in the morning[27-29]. The typical four hour am portion of the work day ends with a lunch break and thus an increased likelihood of leaving the work station and seated position changing the loads on the spine, discs and supporting structures.
METHODS
Subjects
The study consisted of twelve volunteers. The subjects were recruited for the study with flyers. All subjects signed an informed consent form. The study was approved by the Pennsylvania State University Institutional Research Board (protocol 34347). The inclusion criteria included a sedentary job, where individuals were seated continuously for four hours at a time, more specifically the jobs were computer based with sitting at work stations for the majority to entirety of their work day. Exclusion criteria included a history of prior lumbar surgery. None of the participants had prior clinical MRIs of their spine nor were currently obtaining treatment for back pain. All subjects completed a data collection questionnaire which included: age, sex, height, weight, years working in a sedentary job and questions to determine a history of LBP, ongoing LBP and the frequency of LBP. A total of 12 patients, eleven female and 1 male were studied, the subjects were between 23 and 66 years of age (39.83±14.33 years mean [SD]). All subjects reported an episode of low back pain in their lifetime, with six of the subjects experiencing current low back pain. Demographic data are summarized in Table 1.
Table 1.
Characteristics of participants (n=12)
| Mean (SD) age in years | 39.83±14.33 |
| Mean (SD) BMI in kg/m2 | 26.29±9.96 |
| Prior history of LBP, number (%) | 12 (100%) |
| Current LBP, number (%) | 6 (50%) |
| Frequency of current LBP, daily- number (%) | 3(50%) |
| weekly-number (%) | 3(50%) |
| monthly-number (%) | 0(0%) |
| yearly-number (%) | 0(0%) |
| Mean (SD) number of years sedentary job (SD) in years | 14.27±10.16 |
Procedure
The participants underwent lumbar spine MRI scanning on two separate days. They had lumbar sacral MRIs performed at the start of their work days and then four hours later. All subjects worked in the same building as the MRI scanner and the scans were initiated within a few minutes after the end of the four hour sitting periods. MRI scan time was less than 15 minutes per participant. The MRI focused on the lumbar discs: L1-2, L2-3, L3-4, L4-5 and L5-S1 for analysis. The participants underwent their initial MRI scanning at the start of the work day. Day 1 protocol then had participants engage in their sedentary jobs and spend the next four hours seated; they then were reimaged with MRI scans. The Day 2 protocol consisted again of a baseline lumbar MRI at the start of the workday. The participants then again went to work, but did not sit continuous. They would arise out of the chair every fifteen minutes and engage in 5 seconds of lumbar flexion, 5 seconds of lumbar extension, 5 seconds of lumbar bending to the right and then 5 seconds of lumbar bending to the left before then returning to a seated position. The 15 minute time period was chosen given the creep response of the lumbar spine was noted to be present after a 20 minute time or prolonged full flexion. [30,31] Day 2 followed this positional change protocol and the participants were again reimaged after four hours of sitting.
All imaging was performed as follows: after changing into scrub top and pants to prevent any clothing-related image artifacts, participants were laid supine on the spine coil in the bore while images were acquired using a 3.0 Tesla MRI clinical scanner (Siemens Tim Trio, Siemens Medical Solutions USA, Malvern PA, USA). The scanner body coil was used for radio-frequency transmission; for signal reception, an 8-channel receive only spine coil (Siemens Medical Systems) was used. The MRI image acquisition parameters were as follows: T2-weighted axial and sagittal images were acquired using the turbo spin-echo with a reduced refocusing pulse. For the axial images, the spatial resolution was 0.63 mm × 0.63 mm inplane with a 4 mm slice thickness and a 5 mm slice gap; TR/TE = 4100 ms / 80 ms, refocusing flip angle = 140 degrees, bandwidth = 170 Hz/pixel, number of acquisitions=2. For the sagittal images, the spatial resolution was 0.67 mm × 0.67 mm inplane with a 3 mm slice thickness and a 3.5 mm slice gap; TR/TE = 4000 ms / 104 ms, refocusing flip angle = 120 degrees, bandwidth = 240 Hz/pixel, number of acquisitions=2. Analysis was performed using the Syngo DICOM viewer, (Siemens Medical Solutions, USA, Malvern PA, USA) using the included measurement tools.
OUTCOME MEASURES
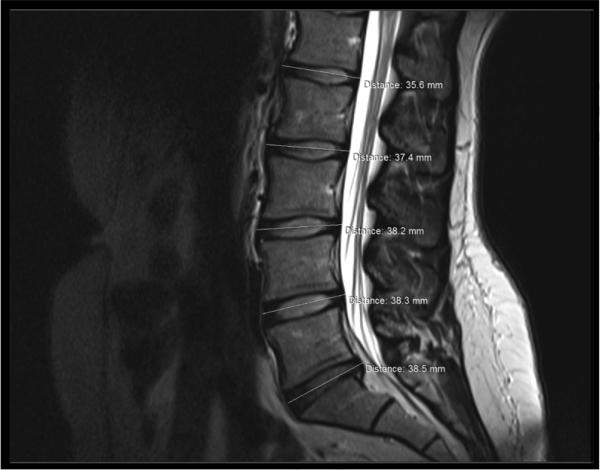
The MRI scans were evaluated using the Syngo DICOM viewer. T2 weighted sagittal images as previously described were evaluated. The midline sagittal image for each patient was chosen for measurements. All scans were then magnified to 1.5× their original size for measurements. Each lumbar disc was then measured for disc diameter in millimeters as shown in Figure 1. Each disc was then also measured for disc height in millimeters as shown in Figure 2. The maximal height and of each disc was measured to the edges of the annulus fibrous following a previously published technique .[32] the maximal diameter of each disc was measured in a similar manner to the edges of the annulus fibrous to maintain consistency. All measurements done on the MRI scans were blinded, as to the day and time of the scan. The data are summarized in Table 2.
Figure 1.
Lumbar disc diameter measurements
Figure 2.
Lumbar disc height measurements
Table 2.
Mean values of MRI assessed disc height (mm) at the start of the work day and 4 hours later for day 1 and for day 2
| Measurement | Day 1 Start | Day 1 End | p-value* | Day 2 Start | Day 2 End | p-value* |
|---|---|---|---|---|---|---|
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |||
| L1-2 | 8.63(1.101) | 9.40(1.19) | 0.156 | 9.29(0.75) | 9.16(0.79) | 0.572 |
| L2-3 | 10.62(1.34) | 10.64(1.12) | 0.433 | 10.51(0.97) | 10.27(1.20) | 0.347 |
| L3-4 | 11.77(1.70) | 11.68(1.82) | 0.646 | 11.40(1.51) | 11.32(1.52) | 0.459 |
| L4-5 | 12.01(0.92) | 11.73(0.88) | 0.009†‡ | 11.48(1.13) | 11.38(1.21) | 0.559 |
| L5-S1 | 11.32(1.36) | 11.27(1.53) | 0.290 | 11.05(1.47) | 11.17(1.88) | 0.553 |
MRI, magnetic resonance imaging; SD, standard deviation.
Paired t-test comparing mean values from start to end (Wilcoxon Signed Rank test comparing median values if normality not satisfied)
Significant at conventional unadjusted alpha level of 0.05 (two-tailed)
Significant at Bonferroni-adjusted alpha level of 0.01 for five simultaneous comparisons (two-tailed)
RESULTS
For this study, we first evaluated each disc level of the lumbar spine for any changes with prolonged sitting for four hours (day 1). Since there were five discs, we eliminated a multiple comparisons bias by a Bonferroni correction to limit the overall experiment wise error rate to 0.05. By dividing 0.05 (a conventional alpha level) by 5, we derived an adjusted two-tailed significance level of p ≤ 0.01. The comparison was conducted by using paired t-test when normality condition was satisfied and Wilcoxon Signed Rank Test if normality was not satisfied. To test for normality the Shapiro-Wilk Test was used.
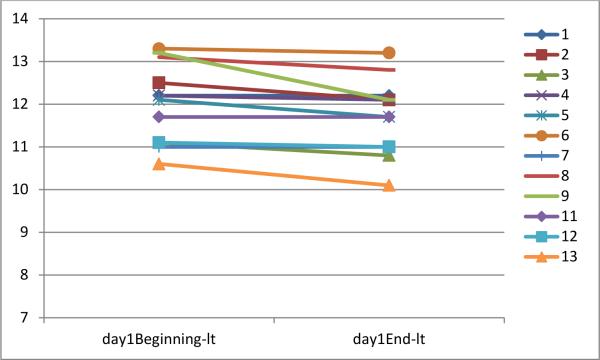
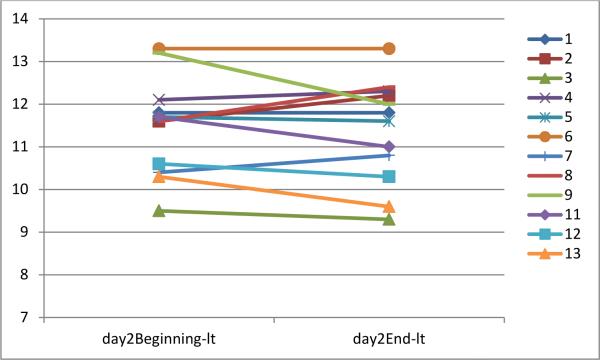
We found that for disc height in this group of participants, L4-5 was significantly decreased at the end of the sitting on day 1, but not for day 2. There was no significant height change for the remaining lumbar discs on either day 1 or day 2. For disc diameter, there were no significant results for any of the discs. The following tables provide a summary of the measurements at the start and end of each session for day 1 and day 2.
DISCUSSION
This study was designed to evaluate the specific changes for each of the five lumbar discs with prolonged sitting. Clinically, the majority of lumbar disc degenerative changes occur at the L4-5 and L5-S1 levels [33-5]. Research has shown multiple reasons including biomechanical forces to account for the increased pressures at these discs [34-40]. The results of this study support this clinical finding. The largest change in disc height with prolonged sitting was found at the L4-5 level. Age and hours sitting were found to be significant risk factors for development of disc herniation at the L4-5 level [41]. Our findings are in agreement with such a relationship. Studies have also shown certain occupational demands including lifting and driving are important risk factors for the development of low back pain [42-44]. The findings of this study may also suggest that prolonged sitting of as little as four hours may also be a factor in increasing pressures of the L4-5 disc. These changes in pressures over a sustained time period may lead towards the disc degeneration cascade. Additionally, the study showed no significant increase in the diameter any disc. This finding perhaps may be explained by the three dimensional shape of the disc. The loss in height is noted in one plane and this can cause a slight increase in the circumference of the disc in the lateral and posterior regions. Measurement of the diameter in the anterior to posterior direction of the disc may not reflect a large enough change in size for significance.
The disc changes in the second day following the change in position protocol showed no changes from baseline in any of the discs, including the L4-5 disc. This suggests that relieving pressure by changing positions every fifteen minutes in this group of participants resulted in no disc height changes over the same four hour period of time. Frequent positional changes could be of benefit to the sedentary workforce. Subjects did comment during day 2 following the change in position protocol that it was a challenge to stop their work and take a break from sitting.
Historically injured workers are evaluated clinically and a medically based return to work plan is formulated. Low back pain patients are frequently returned to work with limitations particularly regarding lifting and carrying duties. The government has identified certain categories with weight restrictions to define these specific classes [45]. Low back pain patients may be returned to work at a sedentary level to avoid lifting and carrying weights above 10lbs. The sedentary job may involve prolonged sitting. This study suggests that a sedentary job which may involve prolonged sitting will increase axial forces at the L4-5 level. The change in position protocol followed in this study may lessen these changes. The data from this study would advocate for brief positional changes every 15 minutes, an accommodation frequently overlooked with return to work prescriptions. Previous research has also focused on the positioning the spine with prolonged sitting and looking at changing the seated angle with back supports and comparing a relaxed sitting posture to an upright sitting posture [46,47]. This study suggests that the simple task of repositioning every 15 minutes may reduce the need for such modifications.
Limitations of this study were the small sample size and female predominance. There has been shown to be a difference in the sexes in their response to static lumbar flexion[48]. Our sample size was nearly all female. The limited study size was unable to show significance with regards to disc changes with a history of low back pain, years in a sedentary position, BMI, VAS scores and age. The small study size did not allow for correlation of disc changes with pain in the subjects. Additional studies with larger numbers of participants could evaluate these relationships further. Individuals with a history of low back pain or after a certain number of years in a sedentary position may be more susceptible to changes and deformities of the lumbar discs.
CONCLUSION
Results from this study showed change in the L4-5 disc height after prolonged sitting of four hours. The study also showed no significant lumbar disc height changes at the L4-5 level when following the day 2 change in position protocol. Additional testing is needed to show the relationship of disc changes in regards to history of low back pain, relationship to active low back pain, years in a sedentary position, BMI and age.
Figure 3.
Height of L4-5 disc at beginning and end of sitting on day 1
Figure 4.
Height of L4-5 disc at beginning and end of sitting on day 2
Table 3.
Mean values of MRI assessed disc diameter (mm) at the start of the work day and 4 hours later for day 1 and for day 2
| Measurement | Day 1 Start | Day 1 End | p-value* | Day 2 Start | Day 2 End | p-value* |
|---|---|---|---|---|---|---|
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |||
| L1-2 | 35.13(1.54) | 34.81(1.89) | 0.256 | 34.67(1.24) | 34.83(2.03) | 0.715 |
| L2-3 | 36.96(1.52) | 36.93(1.87) | 0.870 | 36.83(1.72) | 36.88(1.68) | 0.386 |
| L3-4 | 37.58(1.16) | 37.38(1.48) | 0.548 | 37.45(1.29) | 37.33(0.95) | 0.669 |
| L4-5 | 38.11(1.63) | 37.95(2.14) | 0.665 | 37.13(1.62) | 37.48(1.96) | 0.059 |
| L5-S1 | 36.50(2.16) | 36.99(1.91) | 0.080 | 36.14(1.86) | 36.61(2.08) | 0.130 |
Paired t-test comparing mean values from start to end (Wilcoxon Signed Rank test comparing median values if normality not satisfied)
Table 4.
Mean changes after the four hour session in disc height (mm) and disc diameter (mm) for day 1 and day2
| Measurement | Day 1 Change in Height | Day2 Change in Height | p-value* | Day1 Change in Diameter | Day2 Change in Diameter | p-value* |
|---|---|---|---|---|---|---|
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |||
| L1-2 | 0.23(0.51) | 0.13(0.79) | 0.787 | 0.32(0.92) | −0.16(1.47) | 0.292 |
| L2-3 | −0.03(0.87) | 0.24(0.56) | 0.754 | 0.03(0.69) | −0.05(0.89) | 0.833 |
| L3-4 | 0.09(0.67) | 0.08(0.38) | 0.973 | 0.21(1.16) | 0.13(0.99) | 0.846 |
| L4-5 | 0.28(0.31) | 0.10(0.58) | 0.253 | 0.16(1.23) | −0.36(0.59) | 0.071 |
| L5-S1 | 0.05(0.83) | −0.12(0.66) | 0.367 | −0.49(0.88) | −0.47(0.99) | 1.000 |
ACKNOWLEDGMENTS
We thank all of our participants for their participation. We also thank Amanda Gearhart R.T.(R) (MR) for assistance with data collection.
Funding: None
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None
Contributor Information
Gregory G. Billy, Penn State Orthopaedics Penn State Hershey Bone and Joint Institute-State College Department of Orthopaedics 1850 East Park Avenue-Suite 112 University Park, Pennsylvania 16803.
Susan K. Lemieux, Department of Radiology Penn State Hershey Medical Center Hershey, Pennsylvania.
Mosuk X. Chow, Department of Statistics Eberly College of Science Pennsylvania State University University Park, Pennsylvania.
REFERENCES
- 1.Andersson GBJ. The epidemiology of spinal disorders. In: Frymoyer JW, editor. The adult spine: principles and practice. 2nd ed. Lippincott-Raven; Philadelphia: 1997. pp. 93–141. [Google Scholar]
- 2.Walker BF. The prevalence of low back pain: A systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205–17. doi: 10.1097/00002517-200006000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen TH, Randolph DC. Nonspecific low back pain and return to work. Am Fam Physician. 2007;76(10):1497–1502. [PubMed] [Google Scholar]
- 5.Pai S, Sundaram LJ. Low back pain: An economic assessment in the United States. Orthop Clin North Am. 2004;35:1–5. doi: 10.1016/S0030-5898(03)00101-9. [DOI] [PubMed] [Google Scholar]
- 6.Maetzel A, Li L. The economic burden of low back pain: A review of studies published between 1996 and 2001. Best Pract Res Clin Rheumatol. 2002;16:23–30. doi: 10.1053/berh.2001.0204. [DOI] [PubMed] [Google Scholar]
- 7.Crow WT, Willis DR. Estimating cost of care for patients with acute low back pain: A retrospective review of patient records. J Am Osteopath Assoc. 2009;109(4):229–33. [PubMed] [Google Scholar]
- 8.Hartvigsen J, Leboeuf-Yde C, Lings S, Corder EH. Review article: Is sitting-while-at-work associated with low back pain? A systematic, critical literature review. Scand J Public Health. 2000;28(3):230–9. [PubMed] [Google Scholar]
- 9.Andersson GBJ. Epidemiologic aspects on low-back pain in industry. Spine. 1981 Jan-Feb;6(1):53–60. doi: 10.1097/00007632-198101000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Adams MA, McMillan DW, Green TP, Dolan P. Sustained loading generates stress concentrations in lumbar intervertebral discs. Spine. 1996;21(4):434–8. doi: 10.1097/00007632-199602150-00006. [DOI] [PubMed] [Google Scholar]
- 11.Wilder DG, Pope MH, Frymoyer JW. The biomechanics of lumbar disc herniation and the effect of overload and instability. J Spinal Disord. 1988;1(1):16–32. [PubMed] [Google Scholar]
- 12.Beach TA, Parkinson RJ, Stothart JP, Callaghan JP. Effects of prolonged sitting on the passive flexion stiffness of the in vivo lumbar spine. Spine J. 2005 Mar-Apr;5(2):145–54. doi: 10.1016/j.spinee.2004.07.036. [DOI] [PubMed] [Google Scholar]
- 13.Schultz A, Andersson G, Ortengren R, Haderspeck K, Nachemson A. Loads on the lumbar spine. Validation of a biomechanical analysis by measurements of intradiscal pressures and myoelectric signals. J Bone and Joint Surg. 1982 Jun;64(5):713–20. [PubMed] [Google Scholar]
- 14.Luoma K, Riihimäki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A. Low back pain in relation to lumbar disc degeneration. Spine. 2000 Feb 15;25(4):487–92. doi: 10.1097/00007632-200002150-00016. [DOI] [PubMed] [Google Scholar]
- 15.Urban JPG, Roberts S. Degeneration of the intervertebral disc. Arthritis Res Ther. 2003;5(3):120–30. doi: 10.1186/ar629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luoma K, Vehmas T, Riihimäki H, Raininko R. Disc height and signal intensity of the nucleus pulposus on magnetic resonance imaging as indicators of lumbar disc degeneration. Spine. 2001 Mar 15;26(6):680–6. doi: 10.1097/00007632-200103150-00026. [DOI] [PubMed] [Google Scholar]
- 16.Stokes IA, Iatridis JC. Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine. 2004 Dec 1;29(23):2724–32. doi: 10.1097/01.brs.0000146049.52152.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Podichetty VK. The aging spine: the role of inflammatory mediators in intervertebral disc degeneration. Cell Mol Biol. 2007 May 30;53(5):4–18. [PubMed] [Google Scholar]
- 19.Modic MT, Ross JS. Lumbar degenerative disk disease. Radiology. 2007 Oct;245(1):43–61. doi: 10.1148/radiol.2451051706. [DOI] [PubMed] [Google Scholar]
- 20.Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine. 2006 Aug 15;31(18):2151–61. doi: 10.1097/01.brs.0000231761.73859.2c. [DOI] [PubMed] [Google Scholar]
- 21.Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS. Discs degenerate before facets. Spine. 1990 Feb;15(2):111–3. doi: 10.1097/00007632-199002000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Williams MM, Hawley JA, McKenzie RA, van Wijmen PM. A comparison of the effects of two sitting postures on back and referred pain. Spine. 1991 Oct;16(10):1185–91. doi: 10.1097/00007632-199110000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Dankaerts W, O'Sullivan P, Burnett A, Straker L. Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine. 2006 Mar 15;31(6):698–704. doi: 10.1097/01.brs.0000202532.76925.d2. [DOI] [PubMed] [Google Scholar]
- 24.O'Sullivan PB, Dankaerts W, Burnett AF, Farrell GT, Jefford E, Naylor CS, O'Sullivan KJ. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine. 2006 Sep 1;31(19):E707–12. doi: 10.1097/01.brs.0000234735.98075.50. [DOI] [PubMed] [Google Scholar]
- 25.van Deursen LL, Patijn J, Durinck JR, Brouwer R, van Erven-Sommers JR, Vortman BJ. Sitting and low back pain: the positive effect of rotary dynamic stimuli during prolonged sitting. Eur Spine J. 1999;8(3):187–93. doi: 10.1007/s005860050155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fryer JC, Quon JA, Smith FW. Magnetic resonance imaging and stadiometric assessment of the lumbar discs after sitting and chair-care decompression exercise: a pilot study. Spine J. 2010 Apr;10(4):297–305. doi: 10.1016/j.spinee.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Hutton WC, Malko JA, Fajman WA. Lumbar disc volume measured by MRI: effects of bed rest, horizontal exercise, and vertical loading. Aviat Space Environ Med. 2003 Jan;74(1):73–8. [PubMed] [Google Scholar]
- 28.Adams MA, Dolan P, Hutton WC, Porter RW. Diurnal changes in spinal mechanics and their clinical significance. JJ Bone Joint Surg Br. 1990 Mar;72(2):266–70. doi: 10.1302/0301-620X.72B2.2138156. [DOI] [PubMed] [Google Scholar]
- 29.Zander T, Krishnakanth P, Bergmann G, Rohlmann A. Diurnal variations in intervertebral disc height affect spine flexibility, intradiscal pressure and contact compressive forces in the facet joints. Comput Methods Biomech Biomed Engin. 2010 Oct;13(5):551–7. doi: 10.1080/10255840903337855. [DOI] [PubMed] [Google Scholar]
- 30.McGill SM, Brown S. Creep response of the lumbar spine to prolonged full flexion. Clin Biomech. 1992 Feb;7(1):43–6. doi: 10.1016/0268-0033(92)90007-Q. [DOI] [PubMed] [Google Scholar]
- 31.Au G, Cook J, McGill SM. Spinal shrinkage during repetitive controlled torsional, flexion and lateral bend motion exertions. Ergonomics. 2001 Mar 15;44(4):373–81. doi: 10.1080/00140130010008129. [DOI] [PubMed] [Google Scholar]
- 32.Zhou SH, McCarthy ID, McGregor AH, Coombs RRH, Hughes SPF. Geometrical dimensions of the lower lumbar vertebrae-analysis of data from digitized CT images. Eur Spine J. 2000;9:242–8. doi: 10.1007/s005860000140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boden SD, Davis DO, Dina TS, Patronas, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J. Bone and Joint Surg. 1990 Mar;72(3):403–8. [PubMed] [Google Scholar]
- 34.Butler D, Trafimow JH, Andersson GBJ, McNeill TW, Huckman MS. Discs degenerate before facets. Spine. 1990 Feb;15(2):111–3. doi: 10.1097/00007632-199002000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Takatalo J, Karppinen J, Niinimäki J, et al. Prevalence of degenerative imaging findings in lumbar magnetic resonance imaging among young adults. Spine. 2009 Jul 15;34(16):1716–21. doi: 10.1097/BRS.0b013e3181ac5fec. [DOI] [PubMed] [Google Scholar]
- 36.Farfan HF, Huberdeau RM, Dubow HI. Lumbar intervetebral disc degeneration: The influence of geometrical features on the pattern of disc degeneration-a post mortem study. J Bone Joint Surg Am. 1972 Apr;54(3):492–510. [PubMed] [Google Scholar]
- 37.Skaf GS, Ayoub CM, Domloj NT, Turbay MJ, El-Zein C, Hourani MH. Effect of age and lordotic angle on the level of lumbar disc herniation. Advances in Orthopedics Volume. 2011 doi: 10.4061/2011/950576. Article ID 950576, 6 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Panjabi M, Abumi K, Duranceau J, Oxland T. Spinal stability and intersegemental muscle forces: A biomechanical model. Spine. 1989 Feb;14(2):194–200. doi: 10.1097/00007632-198902000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Posner I, White A, Edwards WT, Hayes W. A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine. 1982 Jul-Aug;7(4):374–89. doi: 10.1097/00007632-198207000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Harrison DD, Harrison SO, Croft AC, Harrison DE, Troyanovich SJ. Sitting biomechanics part I: Review. J Manipulative Physiol Ther. 1999 Nov-Dec;22(9):594–609. doi: 10.1016/s0161-4754(99)70020-5. [DOI] [PubMed] [Google Scholar]
- 41.Kanayama M, Togawa D, Takahashi C, Terai T, Hashimoto T. Cross-sectional magnetic resonance imaging study of lumbar disc degeneration in 200 healthy individuals. J Neurosurg Spine. 2009 Oct;11(4):501–7. doi: 10.3171/2009.5.SPINE08675. [DOI] [PubMed] [Google Scholar]
- 42.Kelsey JL. An epidemiological study of the relationship between occupations and acute herniated lumbar intervertebral discs. Int. J. Epidemiol. 1975;4(3):197–205. doi: 10.1093/ije/4.3.197. [DOI] [PubMed] [Google Scholar]
- 43.Kelsey JL, Hardy RJ. Driving of motor vehicles as a risk factor for acute herniated lumbar intervertebral disc. Am. J. Epidemiol. 1975;102(1):63–73. doi: 10.1093/oxfordjournals.aje.a112135. [DOI] [PubMed] [Google Scholar]
- 44.Lis AM, Black KM, Korn H, Nordin M. Association between sitting and occupational LBP. Eur Spine J. 2007 Feb;16(2):283–98. doi: 10.1007/s00586-006-0143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Code of Federal Regulations §404.1567 [June 5, 2013];Physical exertion requirements. Available at http://www.ssa.gov/OP_Home/cfr20/404/404-1567.htm.
- 46.Makhsous M, Lin F, Hendrix RW, Hepler M, Zhang LQ. Sitting with adjustable ischial and back supports: Biomechanical changes. Spine. 2003 Jun;28(11):1113–1121. doi: 10.1097/01.BRS.0000068243.63203.A8. [DOI] [PubMed] [Google Scholar]
- 47.Leivseth G, Drerup B. Spinal shrinkage during work in a sitting posture compared to work in a standing posture. Clinical Bio Mech. 1997 Oct;12(7-8):409–18. doi: 10.1016/s0268-0033(97)00046-6. [DOI] [PubMed] [Google Scholar]
- 48.Solomonow M, Baratta RV, Banks A, Freudenberger C, Zhou BH. Flexion-relaxation response to static lumbar flexion in males and females. Clin Biomech. 2003 May;18(4):273–9. doi: 10.1016/s0268-0033(03)00024-x. [DOI] [PubMed] [Google Scholar]