Abstract
Background
Stenosing tenosynovitis or trigger finger is a common clinical condition regularly treated with steroid injections. Varied success is reported at early time points following injection. We present a prospective, randomized IRB-approved study to confirm these findings at a long-term follow-up.
Methods
Adult patients presenting with symptoms of stenosing tenosynovitis who agreed to participate were randomized into two groups. Group 1 received an initial injection of triamcinolone and local anesthetic mixture. Group 2 received the same initial injection and an additional staged injection at 6 weeks. The patients were then followed beyond 2 years. If Group 1 patients were still symptomatic at 6 weeks, another injection was given. An additional injection or surgery was defined as treatment failure. DASH scores were obtained at baseline, 3, 6, and 12 months.
Results
Ninety-seven patients (101 trigger digits) were enrolled in the prospective trial. Fifty-six digits were randomized to the one-injection group versus 45 digits randomized to the two-injection group (“intention to treat analysis”—ITT). After accounting for crossover between the groups, 42 patients received one-injection versus fifty-nine patients receiving two injections (“actual” analysis).
Overall failure was the same between the two groups. However, a higher surgery rate was noted for patients having undergone two injections versus one injection [47 % versus 27 % (p < 0.013), ITT]. Diabetes was associated with a higher surgery rate at 1 year within the group of overall failures [56 % versus 37 % (p = 0.0505), ITT]. High baseline DASH score (>40) was associated with a median time of 10 months for failure and 6 months for surgery as per a Kaplan–Meier survival analysis (p < 0.005 and p < 0.001, respectively, ITT).
Conclusions
As overall failure of steroid injection for trigger finger is not improved with staged, two-injection treatment, we recommend a single injection initial treatment for trigger finger with a second injection given in cases of recurrence or failure. Diabetes was a risk factor for needing surgery if failure occurred within 1 year. The baseline DASH score is helpful in predicting which patients have a higher chance of failing as well as needing surgery.
Level of evidence
Prospective, randomized trial, level I.
Keywords: Trigger finger, Stenosing tenosynovitis, Cortisone injection, DASH
Introduction
Trigger finger, or stenosing tenosynovitis, is a common condition that causes difficulty in finger flexion or extension. It can also create snapping or locking when flexing the affected digit and can cause significant pain. There is no universal definition for trigger finger, nor is there a specific laboratory test or radiographic finding, and as such, the clinical diagnosis is made by history and physical examination. It has been estimated that the lifetime prevalence in non-diabetics is 2.2 %. The condition affects females more often than males, and it follows a bimodal distribution, with peaks before the age of six and above the age of 40. It can affect a single or multiple fingers, with the thumb, middle and ring fingers being the most frequently affected digits. It occurs more frequently in diabetics and is also frequently associated with rheumatoid arthritis, Dupuytren’s disease, carpal tunnel syndrome, and hypothyroidism [2, 3].
Historically, trigger fingers were treated surgically. A review article by Fahey in 1954 stated that while conservative therapy such as bracing and stretching can be employed, the vast majority of patients required surgical release, leading to good results in the majority of patients [5]. Lapidus and colleagues came to the same conclusion in 1953, stating that operative release of constricted tendon sheaths was preferable to conservative treatment [10]. However, in a follow-up paper by Lapidus in 1972, he advocated steroid injections as a better alternative to surgical treatment, with good results in 67 patients treated with injections alone [11]. In 1970, Kolind-Sorensen reported a 67 % success rate with prednisolone injection alone for the treatment of trigger finger [9]. Similarly, Clark and colleagues reported an 82 % success rate in a series of 50 trigger fingers in 1973 [4]. A prospective study by Rhoades et al. reported a 72 % success rate in a series of 53 patients in 1984 [16]. Freiberg and colleagues injected 93 trigger fingers, separating patients into a “nodular type” or “diffuse type”, and found a 79 % success rate overall, divided into 93 % success for nodular type versus 48 % success for diffuse type [7].
In 1989, Marks performed a prospective study of 74 patients injected with triamcinolone. He found an 84 % success rate after a single injection, which increased to 91 % with a second injection [13]. Wang and colleagues focused on injections for diabetic patients and found a transient rise in blood sugars and only a 50 % success rate [20].
None of these studies were prospective randomized trials. The purpose of this study was to compare the efficacy of one versus two staged corticosteroid injections for the treatment of trigger finger. The hypothesis was that a second staged injection given at 4 to 6 weeks after the first injection would significantly increase the chances for a cure. The one-injection group received a single injection of Kenalog and lidocaine, while the two-injection group received an additional injection of the same dosage, 4 to 6 weeks following the first injection. The patients were evaluated for symptoms of pain, stiffness, clicking, or locking at the 4 to 6 week interval. If the one-injection group still had painful clicking or locking at the 4 to 6 week time point, then another injection would be given allowing for crossover.
Materials and Methods
An institutional review board has approved this study, and informed consent was obtained from all participants. Ninety-seven consecutive, consenting patients with 101 trigger digits seen from 2009 to 2011 were prospectively randomized into two treatment groups. They were assigned to either a single injection of 0.5 mL Kenalog (triamcinolone) (40 mg/mL) with 0.5 mL lidocaine (10 mg/mL) (Group 1) or two (staged) injections of the same mixture, the second occurring 4 to 6 weeks later (Group 2). Patients presenting with symptoms of stenosing tenosynovitis were included in the study if they were over the age of 18 years, male or female, and willing and able to provide informed consent. We included patients with insulin-dependent and non-insulin dependent diabetes mellitus. We excluded patients who had previously ongoing trigger finger treatment or had concomitant disease of the digit (i.e., fracture, sprain, or mucous cyst). For the purpose of the study, patients with multiple digits involved were specifically treated according to the methods of the study, for the digit of greatest subjective complaints upon initial office evaluation. Women who were pregnant or thought they may be pregnant were excluded from the study. We recorded patient age, gender, smoking status, hand dominance, affected hand, affected digit, and whether they had diabetes mellitus. Patients were assigned to each group based on their previously randomly assigned medical record number (odd or even).
Two hand surgeons were involved in the recruitment and treatment of these patients. Both surgeons performed a similar technique for injection. Specifically, the injection was given at the level of the A1 pulley via volar approach with injection administered just outside of the flexor sheath, not intratendinous or subcutaneous. Post-injection pain was managed conservatively with over-the-counter medications.
We clinically evaluated the patients at 6 weeks, 3 months, 6 months, 1 year, and 2 years after the injection. Follow-up was performed with history and physical exam during office visit for the 6 weeks, 3 months, and 6 months, and phone follow-up was made at the 1 and 2 year intervals. If Group I patients were still symptomatic at the 6 week evaluation, a second injection was therapeutically administered. This reevaluation of Group 1 patients as members of Group 2 was accounted for in the crossover “actual” analysis. Treatment failure was defined in a Group I patient if either an additional injection after 6 weeks or surgery was performed. Group II were offered surgery at the point of treatment failure. Statistical analysis on the failure and surgery rates for both groups was carried out using a Fisher’s exact test at the 3-month, 6 month, 1 year, and 2 year time points. Multivariate logistic analysis was performed to compare the two groups at the 1-year and 2 year time points for failure rate as well as surgery rate. No funding was received for this research.
Results
Ninety-seven patients with 101 trigger digits were recruited and randomized into the two treatment groups. Figure 1 represents the age distribution by decade of the 97 patients randomized into the two treatment groups.
Fig. 1.
Age distribution of patients
The patients randomized homogenously (Table 1) with the exception of a significantly greater number of smokers to the two-injection group (8 patients versus 2 patients). Of note, the proportion of thumbs was not significantly different for Group 1 versus 2.
Table 1.
Demographics of two randomized groups
| Group 1 (n = 56) | Group 2 (n = 45) | p-Value | |
|---|---|---|---|
| Age, mean (years) | 61.7 years | 60.0 years | 0.313 |
| Male | 28 (50.0 %) | 16 (35.6 %) | 0.163 |
| Diabetes mellitus | 10 (17.9 %) | 3 (6.7 %) | 0.134 |
| Smoker | 2 (3.6 %) | 8 (17.8 %) | 0.042 |
| Thumb affected | 16 (28.6 %) | 7 (15.6 %) | 0.458 |
| Right-hand dominant | 46 (82.1 %) | 42 (93.3 %) | 0.124 |
| Dominant hand affected | 36 (64.3 %) | 27 (60.0 %) | 0.681 |
The distribution of the involved digits is depicted in Table 2. Although thumb involvement is not statistically significant between groups, there is a statistically significant sparing of the index and little fingers versus the remaining digits in each of the treatment groups (p < 0.001).
Table 2.
Distribution of trigger digits
| Thumb | Index | Long | Ring | Little | |
|---|---|---|---|---|---|
| One injection | 16 | 3 | 18 | 17 | 2 |
| Two injection | 7 | 4 | 13 | 19 | 2 |
The breakdown for each treatment group by baseline DASH score is illustrated for the ITT analysis (Table 3) and “actual” analysis after cross-over (Table 4). No statistical significance was found between treatment groups for either analysis. The cross-over of patients was also not found to be statistically significant (p < 0.27). Statistical analysis was performed using Fischer’s exact test for count data.
Table 3.
Distribution of DASH scores in ITT group (p < 1.0)
| DASH 0-20 | DASH 20-40 | DASH 40+ | |
|---|---|---|---|
| One injection | 14 | 15 | 15 |
| Two injection | 11 | 12 | 12 |
Table 4.
Distribution of DASH scores in ITT group (p < 0.47)
| DASH 0-20 | DASH 20-40 | DASH 40+ | |
|---|---|---|---|
| One injection | 13 | 10 | 10 |
| Two injection | 12 | 17 | 17 |
Of the original 97 patients, 19 patients were lost to follow-up at 2 years with the average follow-up being 23.0 months with a range of 0 to 30 months. Two-year follow-up for the trigger digits was 81 %. Using a Cox proportional hazards analysis, overall failure and surgery rates were evaluated as a function of single versus staged two injections, initial DASH score, age, gender, thumb versus finger involvement, ipsilateral dominant hand involvement, diabetes mellitus, and smoking status. No difference was noted between ITT and actual analyses. Therefore, further investigation and analyses provided were performed on ITT (intention to treat) basis.
Overall treatment failure (reinjection or surgery) was not statistically different between the one- and two-injection groups. Only the initial DASH score was predictive of overall failure (p < 0.005). The median time to failure was 10 months for the group with an initial DASH score of greater than 40 (Fig. 2).
Fig. 2.
Kaplan–Meier survival: overall failure vs. initial DASH score (p < 0.005) (X-axis: months after first injection; Y-axis: percentage survival-patients without failure)
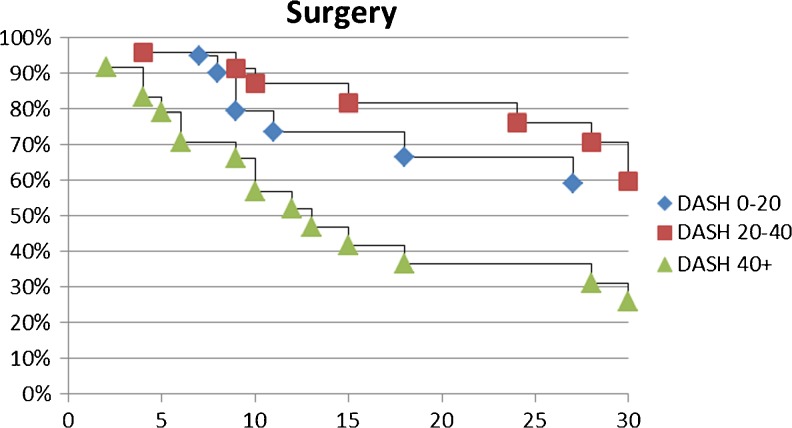
However, specifically for surgery outcome, both the number of injections (Fig. 3, p < 0.013) and initial DASH score were predictive of surgery (p < 0.001) (Fig. 4). For patients with an initial DASH score of more than 40, the median time to failure was 10 months (Fig. 2), whereas median time to surgery was 13 months (Fig. 4).
Fig. 3.
Kaplan–Meier Survival: Surgery outcome vs. Injection Treatment Group (p < 0.013) (X-axis: months after first injection; Y-axis: percentage survival-patients without surgery)
Fig. 4.
Kaplan–Meier survival: surgery outcome vs. initial DASH score (p < 0.001) (X-axis: months after first injection; Y-axis: percentage survival-patients without surgery)
In addition, when looking within the failures specifically, two factors were predictive of surgery: number of injections and diabetes. The surgery rate among failures was higher in the two-injection group (63 %) versus the single injection group (24 %) at the 1-year time point (p < 0.013). At the 2 year time point, this was even more disparate: 87 % vs. 44 %, respectively (p < 0.005). The median time to surgery was >30 months and 18 months for the one-injection and two-injection groups, respectively. The presence of diabetes also increased the rate of surgery among failures (56 % vs. 37 %) but only at the 1 year time point (p < 0.05), not at 2 years (p < 0.26).
Discussion
In contrast to other tendinopathies, stenosing flexor tenosynovitis (trigger finger) is associated with an inflammatory component rather than a tendinosis with degenerative changes alone [18]. Subsequently, it is common practice to use corticosteroid injections to treat trigger finger symptomology. Steroid injection has been shown to be effective in various studies [6, 12, 19], including a randomized, controlled prospective study where steroid injections with anesthetic were noted to be significantly more effective than anesthetic injection alone [14]. Success after steroid injections for trigger finger has been cited at greater than 50 %, even in diabetics [1, 17]. However, the Cochrane Systematic Review in 2009 reported a pooled success rate of only 37 % [15].
Repeated corticosteroid injections may have cumulative, detrimental sequelae including atrophy of the skin, fat, and tendon. Therefore, injections are not pursued indefinitely. If corticosteroid injections are not successful, surgery (dividing the A1 pulley) is offered to the patient with success rates greater than 90 % [13]. Kerrigan et al. concluded that the most cost-effective algorithm for treatment was to perform open surgical release for persistent or recurrent symptoms after two therapeutic attempts with corticosteroid injections [8].
Our prospective study was aimed at determining whether performing a corticosteroid injection in a staged fashion 6 weeks after the first was more effective than doing one injection. Follow-up was chosen at up to 2 years to determine whether success often cited between 37 % and 91 % would persist at a longer time point (10, 17, 19). The data was then evaluated with an “intention-to-treat” analysis (“ITT”) where patients’ assignment to each arm of the study was maintained for statistical analysis. As this does not account for any crossover of patients in the one-injection group who wished to have a second injection on follow-up, this reevaluation was accounted for in a “cross-over” analysis (“actual”). Statistically, there were no significant differences when the Cox proportional hazards model was performed on both. We believe that the injection technique performed by the hand surgeons in this study was effective as our failure rates were similar or better than others in the literature. In fact, compared to the recent randomized trial by Sato et al. in which a 43 % failure at 6 months was noted after corticosteroid injection for trigger finger [17], our overall failure rate at 6 months was 22 %.
Regarding overall failure, defined as needing additional injections or surgery, there was no statistically significant difference noted between the groups receiving a single corticosteroid injection for trigger finger versus the group receiving two injections in a staged fashion 6 weeks apart. The overall failure rate was noted to be 22 % at 6 months versus 54 % at 1 year.
Having a two-injection treatment did not reduce overall failure but did increase the chance of undergoing surgery within a year. This is not surprising since the one-injection group was offered another injection instead of surgery. It is possible that the second injection produces a tendinous reaction causing increasing tendon thickness or scarring. However, with two injections being the maximum we offered in our study, surgery was the inevitable outcome in the two-injection failures.
We used a Kaplan–Meier survival model to determine that the median time to surgery was greater than 30 months and 18 months for the one-injection and two-injection groups (p < 0.013), respectively. Certainly, a study with longer follow-up would be useful to evaluate how many patients in the one-injection group would have recurrence after a second injection (given after 1 year) and need surgery eventually.
Furthermore, looking specifically at the outcome of surgery, a Cox proportional hazards model was utilized to determine the independent predictors of needing surgery within a year. In addition to two staged injections, a higher baseline DASH score also carried a higher chance of needing surgery within a year. This was independent of having a one- or two-injection treatment. However, at 1 year, diabetes was a predictor of surgery within the patients with failure, but not at 2 years. This suggests that diabetes is a predictor of earlier surgery in patients that have overall failure within 1 year of their first injection. If the diabetic patient has failure after 1 year, the chances of needing surgery are not increased versus a nondiabetic.
Using the conclusions from Sato et al. [17] and the findings of our study, we propose an algorithm for trigger finger patients. Anecdotally, trigger finger patients are treated with corticosteroid injections if more conservative measures are determined to be ineffective. If injection therapy is given, a single injection should be given for the trigger digit with the understanding that approximately half of the patients will have recurrence within a year. At the point of recurrence, a patient may opt for another injection with the goal of delaying surgery. However, for diabetics with recurrence in less than a year or patients with a higher baseline DASH score, we may consider surgery at the time of recurrence after single injection. A greater proportion of patients with baseline DASH scores over 20 crossed over from the one-injection to the two-injection group. There was no statistical difference between crossover rates for the patients with a baseline DASH score greater than 20 versus those with less than 20. This may be due to the study being underpowered. However, the trend implies that perhaps a baseline DASH score over 20 may predict patients, which will likely have symptoms after one injection or earlier recurrence. Contrastingly, logistic regression analysis did reveal that a baseline DASH score greater than 40 independently portends an increased chance of needing surgery.
Interestingly, dominant hand involvement was not associated with increased failure or need for surgery at the 1 or 2 year time points. This may be due to compensatory mechanisms with opposite hand usage. This study did not have enough patients with index and little finger involvement to assess their specific significance. However, thumb involvement was not statistically significant in predicting overall failure or surgery. A larger or specific study may help elucidate whether specific digit involvement reflects a worse diagnosis as index and little digit incidence uncommon, thus making surgery an earlier consideration. Conversely, their lower incidence may make surgery a less likely option, if recurrence is less after injection.
Conclusion
Undergoing a staged, two-injection corticosteroid treatment for trigger digits was not shown to be superior to a single-injection treatment. Therefore, we do not recommend staged, two-injection treatment of trigger digits. Diabetes is an independent predictor of surgery among patients who have failed injection at 1 year. However, baseline DASH scores are predictive of not just surgery but also overall failure (reinjection or surgery) up to 30 months after initial injection.
Acknowledgments
The authors would like to acknowledge the work of James Dowdell, BS for his help in the collection of the data presented in this study.
Conflict of Interest
Charles F. Leinberry declares he has no conflict of interest.
Emran Sheikh declares he has no conflict of interest.
Mithchell Maltenfort declares he has no conflict of interest.
Will Sayde declares he has no conflict of interest.
John D Peters declares he has no conflict of interest.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent
All patients enrolled in this study gave informed consent to participate and no identifying factors were used.
Contributor Information
Emran Sheikh, Phone: +1-201-4704647, Email: e_sheikh@yahoo.com.
John D. Peters, Phone: +1-570-4361289, Email: john.peters@jefferson.edu
Will Sayde, Phone: +1-551-4274652, Email: saydew@gmail.com.
Mitchell Maltenfort, Phone: +1-267-3393753, Email: mitchell.maltenfort@rothmaninstitute.com.
Charles Leinberry, Email: charlie.leinberry@rothmaninstitute.com.
References
- 1.Baumgarten KM, Gerlach D, Boyer MI. Corticosteroid injection in diabetic patients with trigger finger. A prospective, randomized, controlled double-blinded study. J Bone Joint Surg Am. 2007;89(12):2604–2611. doi: 10.2106/JBJS.G.00230. [DOI] [PubMed] [Google Scholar]
- 2.Blyth MJ, Ross DJ. Diabetes and trigger finger. J Hand Surg (Br) 1996;21(2):244–245. doi: 10.1016/S0266-7681(96)80106-9. [DOI] [PubMed] [Google Scholar]
- 3.Chammas M, Bousquet P, Renard E, Poirier JL, Jaffiol C, Allieu Y. Dupuytren’s disease, carpal tunnel syndrome, trigger finger, and diabetes mellitus. J Hand Surg [Am] 1995;20(1):109–114. doi: 10.1016/S0363-5023(05)80068-1. [DOI] [PubMed] [Google Scholar]
- 4.Clark DD, Ricker JH, MacCollum MS. The efficacy of local steroid injection in the treatment of stenosing tenovaginitis. Plast Reconstr Surg. 1973;51(2):179–180. doi: 10.1097/00006534-197302000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Fahey JJ, Bollinger JA. Trigger-finger in adults and children. J Bone Joint Surg Am. 1954;36-A(6):1200–1218. [PubMed] [Google Scholar]
- 6.Fleisch SB, Spindler KP, Lee DH. Corticosteroid injections in the treatment of trigger finger: a level I and II systematic review. J Am Acad Orthop Surg. 2007;15(3):166–171. doi: 10.5435/00124635-200703000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Freiberg A, Mulholland RS, Levine R. Nonoperative treatment of trigger fingers and thumbs. J Hand Surg [Am] 1989;14(3):553–558. doi: 10.1016/S0363-5023(89)80024-3. [DOI] [PubMed] [Google Scholar]
- 8.Kerrigan CL, Stanwix MG. Using evidence to minimize the cost of trigger finger care. J Hand Surg [Am] 2009;34(6):997–1005. doi: 10.1016/j.jhsa.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 9.Kolind-Sorensen V. Treatment of trigger fingers. Acta Orthop Scand. 1970;41(4):428–432. doi: 10.3109/17453677008991530. [DOI] [PubMed] [Google Scholar]
- 10.Lapidus PW. Stenosing tenovaginitis. Surg Clin North Am. 1953 Oct:1317–47 PMD 13102191. [DOI] [PubMed]
- 11.Lapidus PW, Guidotti FP. Stenosing tenovaginitis of the wrist and fingers. Clin Orthop Relat Res. 1972;83:87–90. doi: 10.1097/00003086-197203000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Maneerit J, Sriworakun C, Budhraja N, Nagavajara P. Trigger thumb: results of a prospective randomised study of percutaneous release with steroid injection versus steroid injection alone. J Hand Surg (Br) 2003;28(6):586–589. doi: 10.1016/S0266-7681(03)00172-4. [DOI] [PubMed] [Google Scholar]
- 13.Marks MR, Gunther SF. Efficacy of cortisone injection in treatment of trigger fingers and thumbs. J Hand Surg [Am] 1989;14(4):722–727. doi: 10.1016/0363-5023(89)90199-8. [DOI] [PubMed] [Google Scholar]
- 14.Murphy D, Failla JM, Koniuch MP. Steroid versus placebo injection for trigger finger. J Hand Surg [Am] 1995;20(4):628–631. doi: 10.1016/S0363-5023(05)80280-1. [DOI] [PubMed] [Google Scholar]
- 15.Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B. Corticosteroid injection for trigger finger in adults. Cochrane Database Syst Rev. 2009;1 doi: 10.1002/14651858.CD005617.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhoades CE, Gelberman RH, Manjarris JF. Stenosing tenosynovitis of the fingers and thumb. Results of a prospective trial of steroid injection and splinting. Clin Orthop Relat Res. 1984;190:236–238. [PubMed] [Google Scholar]
- 17.Sato ES, Gomes Dos Santos JB, Belloti JC, Albertoni WM, Faloppa F. Treatment of trigger finger: randomized clinical trial comparing the methods of corticosteroid injection, percutaneous release and open surgery. Rheumatology (Oxford) 2012;51(1):93–99. doi: 10.1093/rheumatology/ker315. [DOI] [PubMed] [Google Scholar]
- 18.Speed CA. Fortnightly review: corticosteroid injections in tendon lesions. BMJ. 2001;323(7309):382–386. doi: 10.1136/bmj.323.7309.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taras JS, Raphael JS, Pan WT, Movagharnia F, Sotereanos DG. Corticosteroid injections for trigger digits: is intrasheath injection necessary? J Hand Surg [Am] 1998;23(4):717–722. doi: 10.1016/S0363-5023(98)80060-9. [DOI] [PubMed] [Google Scholar]
- 20.Wang AA, Hutchinson DT. The effect of corticosteroid injection for trigger finger on blood glucose level in diabetic patients. J Hand Surg [Am] 2006;31(6):979–981. doi: 10.1016/j.jhsa.2006.03.022. [DOI] [PubMed] [Google Scholar]