Abstract
As persons living with HIV/AIDS live longer, both the prevalence and incidence of HIV infection in older women is expected to increase, and this review presents a model and review of the extant literature on older women with HIV/AIDS in the United States. Older women are rarely addressed in the discourse about HIV risk and prevention, and their concerns are often missed by risk reduction programs that typically target men and younger adults. Societal biases around aging can compound factors such as stigma and disclosure for older women. Primary care providers are often not recommending routine HIV testing to older women, or addressing the impact of age related physiological changes on risk and sexual health. Many older women may be starting new relationships and the role of relational variables that are specific to this group of women are key in understanding prevention and treatment. Empirical research focused on the needs of older women, and recognition of the diverse composition and needs of this group is needed to inform prevention, intervention and best practices with this population of women.
Keywords: HIV, older women, sexuality, risk, stigma
Yolanda Diaz, 50, is experiencing a joy she never expected: menopause. When she first received her AIDS diagnosis in 1989, she had no interest in treatment — instead she smoked more crack and heroin, bounced in and out of prison, and let the father of her children raise them. But age and the disease have mellowed her. Now she follows her regimen and works for an AIDS organization called Iris House, performing interventions for women with addictions. AIDS has given her life meaning and community. “Man, I’m going to be 51,” she said, lingering over the number like a fresh miracle. “I don’t think I’m going to die from H.I.V. and AIDS. But in the long run, I am going to die from O.I.’s, from opportunistic infections. I just don’t think about it on a daily basis.” 1
As Ms. Diaz’s story illustrates, HIV infection and AIDS in older women represents a longer story, typically these are nuanced narratives of relationships, families, children, stigma, illness, substance use, and the evolution of the illness as a person ages. The clinical snapshots often generated of women living with HIV/AIDS miss the myriad factors that can change over a lifetime and impact health, wellness, and life. Older adults with HIV have been termed the “unserved, unseen, and unheard”, 2 a characterization that is even more pronounced for older women with HIV. The relative dearth of literature addressing women is notable, and remains a major knowledge gap, particularly as the current population of HIV seropositive women ages, and we observe more incident infections in women over 50.
The shifting demographic of HIV/AIDS is best manifested in older adults. It is predicted that by 2015, 50% of all cases of HIV/AIDS in the US will be in persons over the age of 50. At the end of 2009, over 50,000 women over the age of 50 are HIV seropositive. 3 These shifts are being evidenced differentially in men and women. Since the beginning of the HIV epidemic, women have manifested lower rates of infection, and this has resulted in a relative dearth of research and targeted clinical care for women. The pocketed disproportionalities of the distribution of infection (e.g. the proportion of African American women represented in the overall epidemiology of the disease), as well as the disparate types of stressors, treatments, and experiences of HIV-infected women (e.g caregiving duties, implications for reproduction, stigma related issues) call for more research not only on women, but with a specific focus on older women who bring variegated experiences. 4
In older adults (for purposes of this paper, older adults will be defined as those adults over the age of 50), the shifts in epidemiology are notable. Rates of infection in women age 50 and over remained stable from 2007–2010, with incidence rates during that time period for women of approximately 4.2/100,000, with comparable incidence rates for men at 13.6/100,000 5 and a similar trend is observed for prevalence rates at the end of 2009 in this population (women 113.2/100,000; men 476.3/100,000). Women over the age of 50 are largely contracting HIV through heterosexual contact, and in incident infections in the period of 2007–2010, 82% were attributed to heterosexual infection, while prevalence rates reveal that 66% of infections were due to heterosexual infection. Older women evidenced a higher percentage increase in deaths due to HIV compared to men (32% increase for women, 18% for men).
These prevalence statistics suggest that while older men are still disproportionately represented in the epidemiological data on HIV/AIDS in older adults, the ground is shifting for women, who may also fare more poorly with the illness, and bring different types of psychosocial and psychological burdens. However, little research exists that focuses solely on older women living with HIV/AIDS or on risk behaviors in older women. The advent and evolution of better treatments for HIV implies that as survival times for all individuals with HIV increase, the confluence of health problems due to HIV/AIDS as well as normal aging is going to be an issue for both men and women. As the issue of older adults, and particularly older women is addressed via intervention and prevention programs, there must be recognition of 2 distinct groups –those who became infected at a younger age and are growing old with HIV/AIDS and those who are becoming newly infected over the age of 50. 6 Both groups bring different clinical challenges in terms of prevention, testing, and monitoring, but regardless of age at the time of infection, as the HIV seropositive population ages – the burden on the health care system will proliferate and models of care delivery tailored to older women will be needed.
Consistently, there has been significantly less empirical literature focusing on the psychological, psychiatric, and psychosocial needs of women, as well as the unique medical and biological vulnerabilities both HIV-infected women and women at risk for HIV face. This has resulted in delays in treatment, as well as tailored prevention and intervention programs for women. In addition, the entire population of men and women with HIV is living longer and getting older. There is an even greater dearth of literature addressing women over 50 living with HIV. This review endeavors to address key issues in understanding key issues in HIV/AIDS in older women: (a) sexual risk; (b) testing; (c) primary care; (d) neuropsychiatric issues; (e) psychosocial factors (f) substance use/abuse; (g) targeted intervention. These issues are also considered within a contextualized framework of structural variables including ageism, stigma, and power/oppression. The initial literature review focused on literature published since 2000 to account for the advent of highly active antiretroviral therapy. Because of the relative paucity of literature on older women, older empirical studies were pulled to round out understanding of key concepts as needed.
The literature review was conducted using multiple search databases to ensure coverage of research deriving from multiple disciplines related to this topic. Specifically, the search databases included AccessMedicine, PILOTS Database, Google Scholar, ProQuest Psychology Database, PsycArticles, PsychINFO, PubMed (includes MEDLINE) and employed keywords and various combinations of search terms as follows: women, older, elderly, HIV, AIDS. The decision to choose articles published 2000 and later was largely driven by the fact that treatment, health outcomes, and survival times in persons living with HIV/AIDS shifted significantly after the mid-1990’s with the advent of highly active antiretroviral therapies, and this choice of publication date was meant to draw from literature that is congruent with the contemporary prevention and intervention environment for HIV/AIDS. Additional and often older literature was then utilized to build upon points raised by studies focusing on older adults, or to highlight issues specific to women, or specific subpopulations of women, and to address the contextual factors listed above. Epidemiology statistics were derived from CDC publications and data. After ruling out articles that were deemed inappropriate for this paper’s focus (e.g. focus on international samples, younger women, men) we selected roughly 75 articles to use for this paper.
Conceptual Model
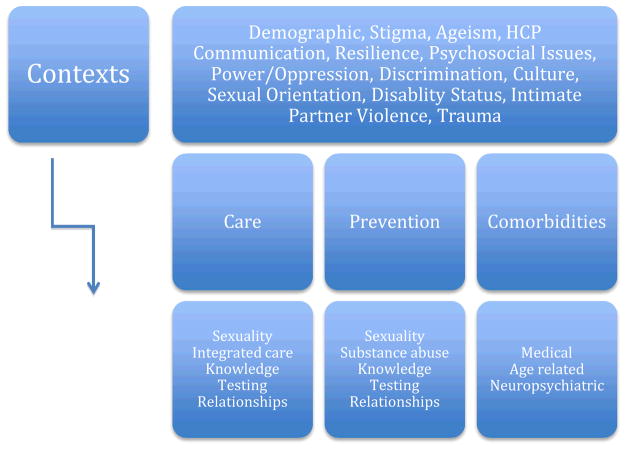
Based on the extant literature, figure 1 depicts the three key issues to address in older women living with HIV/AIDS (a) Care; (b) Prevention; and (c) Comorbidities. Most importantly, this model also recognizes that these 3 key elements must always be viewed within the contexts of issues specific to this group of women. Given that intersectionality of multiple statuses, as well as the societal context in which these contexts occur have direct impacts on the experience of older women with HIV/AIDS –each of the issues put forth in the paper will address the reciprocal relationship between these individual factors and the larger context.
Figure 1.
Contextualized Model for HIV/AIDS Care and Prevention for Older Women
Flawed Assumptions
The research literature and data from primary care together reveal assumptions that can have deleterious or downright dangerous impacts for the care of older women at risk for HIV/AIDS or who may already be infected. Foremost amongst these are (a) older women do not have sex; and (b) older women don’t know and don’t want to talk about HIV/AIDS. The disconnect between valuing a sex life in a culture that “de-sexualizes” older women and the attendant shame of talking about having sex, compounded by issues of stigma about HIV results in an unfortunate synergy that can make older women reluctant to discuss stigmatized issues such as sex or HIV/AIDS. 7 There is a robust literature suggesting that among older adults, both men and women still want to have sex, are having sex, and want to talk about sex with their healthcare providers, but often look to healthcare providers to start the discussion. 8–10 In addition, flawed assumptions about the uniformity of older women with HIV/AIDS can be damaging. Older women with HIV/AIDS may not only be ethnic minority group members, but also may be sexual minorities, disabled, and carried these statuses at a time when discrimination and severe societal approbation resulted in a lifetime of oppression, stress, isolation, and in some cases violence and trauma. Attempts at progressive legislation and more open dialogue about equality, acceptance and access were simply often not part of the developmental histories of these women, and continuing to maintain stereotyped assumptions about these women only perpetuates ignorance of their experience.
Older adults with HIV often must face down two chronic sources of stigma –HIV seropositivity and ageist biases. 11,12 Ageism is a pervasive influence in our culture and promulgated through stereotyping, media, and pejorative attitudes toward older adults. Given the overfocus on sexuality and appearance as a salient characteristic in women, ageist beliefs toward women can have deleterious impacts on identity, self esteem, and engagement in health care. In a series of qualitative interviews conducted by Emlet et al 11 with a small sample of older adults living with HIV/AIDS (N = 8), women revealed that rejection, stereotyping, and isolation emerged as intersecting themes of HIV stigma and ageism. Of note, HIV serostatus may be but one of many stigmas that older HIV infected women may struggle with. For example older lesbian and bisexual women in particular came of age in a time when criminalization and stigmatization of same-sex relationships were endemic and identities were forced to be closeted from society and family. Such stigmatized identities are often repeated in multiple ways for older women whether as a function of sexual orientation, ethnic minority status, disability status, HIV serostatus and older age. While there may have been greater evolution in societal acceptance of some of these statuses, it is critical to remain mindful of the fact that older women came of age at a time when these statuses placed them more acutely in the cross hairs of stigma and isolation. 13
HIV Testing in Older Women
While the CDC recommends regular HIV/AIDS testing in persons up to the age of 64 14, few older adults report being offered testing. Women over the age of 50 may delay HIV testing, even in the face of symptoms, because in older adults, symptoms may be interpreted as indicative of other health conditions. 15 In one community sample of 101 older adults (70% women), 90% reported that their health care providers had never discussed HIV or other sexually transmitted infections (STIs) with them. 16 Overall, research suggests that 15–30% of women ages 55 and older have previously been tested for HIV. 16 Rates of HIV testing in the population indicate that 44% of adults have been tested during their lifetime, but only 10–15% of those 45–64 years of age have undergone testing, 17 with some studies reporting rates as few as 3% of older samples receiving a recommendation for testing. 16 When older adults are tested, they are often tested later in the course of HIV, and are more likely to have opportunistic infections, progress more rapidly to AIDS, or die within a year of HIV diagnosis. As such, testing of older adults is essential to manage new infections in older adults and mitigate morbidity and mortality in those who are infected.
Older women themselves may not perceive themselves as being at risk and simply report a lack of interest in being tested. Akers et al18 found that 71% of women in their sample were not interested in testing despite nearly 50% having moderate to high levels of lifetime risk and exposure. This also intersects with patient reports that less than 25% experienced a provider ever recommending HIV testing. 18 Risk based screening may not be sufficient in this population as women’s perceptions of risk are not always accurate, and older women’s motivation for pursuing HIV testing is influenced not only by knowledge about HIV but also perceptions and misperceptions about risk of contracting the virus and actual risk status. When comparing cohorts of older women to younger women, especially when older women evidence patterns of less drug use, fewer sex partners, and lowered likelihood of having an STI, there may be an attendant lowered perception of risk and less opportunities in which testing is offered, which can result in delays in diagnosis and treatment. 19
Shifts in relationship factors
Midlife women are more likely to have had changes in relationship status (e.g. divorce, separation, or death of a partner) and as such may be more likely to acquire new partners, but may be doing so after a long period of not seeking new partners. 20 In our data on 71 HIV+ women, 67% of older women reported that they were not in a committed relationship compared to 38% of younger women. 21 Older women in newer relationships (6 months duration or shorter) were more likely to report having multiple partners. 22 These women may be less efficacious in discussing issues such as HIV serostatus, protection against HIV and STIs, and even in the development of new relationship dynamics that can facilitate or hamper healthy sexual communication. 20 Relational variables such as trust, dependence on a partner, and taking personal responsibility for obtaining condoms have all been associated with safer sex decisions, and found to be more important than general knowledge about HIV transmission. 23 Sexual communication has been found to be a greater challenge for older women. 24 In general, the literature suggests that older women are less willing to be assertive in asking partners about their sexual risk histories. This is a notable finding as it suggests that useful interventions with this population of women may focus on enhancement of communication within a relationship or even take a dyadic approach with a focus on both partners within a relationship.
Intimate partner violence (IPV) is also a factor to be considered when assessing the role of the relationship in HIV risk. IPV has been associated with greater risk for HIV and overall, women living with HIV/AIDS have a higher likelihood of having experienced IPV. 25–27 In older women, IPV is associated with greater risks for HIV including multiple sexual partners, a history of STIs, and greater risk behaviors in partners. 22 Because older women may feel less agentic in their relationships and in cases of IPV, fearful of their partners, ongoing IPV may place older women at risk for multiple deleterious health outcomes including HIV as well as physical injuries from which recovery may be more complicated, and psychological distress for which they may be less likely to seek help. 28 However, reports of fear of reprisal from partners if requests for condom use were made were not reported in all cohorts of older women. 29 As such, interventions with older women may need to account for IPV but also assume that women can also take on the mantle of sexual advocacy around condoms. In addition, assumptions about the likelihood of IPV may mean that certain subpopulations of older women may be overlooked. For example, the misassumption that IPV is only about man on woman violence may mean that women who have female partners are overlooked, and in addition, women with disabilities are particularly vulnerable to IPV.
The traditionally reductionistic approach to risk reduction has been skills development, capacity building, and communications training. However, this ignores the subtext of power and oppression that can characterize heterosexual relationships for women, especially ethnic minority and low income women, and this is likely to be potentiated in older women. Ultimately, behavioral interventions will not be viable without addressing power dynamics. Relationship power has been described as a factor that can impact the ability of women to work with partners to engage in risk protective behavior. 30 Amaro & Raj et al30 highlight three dynamics of oppression: silencing, violence/fear of violence, and internalized oppression – all of which they suggest must be considered when developing, implementing, and maintaining HIV risk reduction strategies in women. In the absence of such contextualization, behavioral and communication skills are unlikely to be implemented, even if women are able to articulate or demonstrate skills and knowledge in clinical settings. The dynamics of oppression are likely to be magnified in groups who face what could be termed “intersectional oppression” – with etiologies driven by multiple factors including poverty, minority statuses, disability status, and the fact that developmentally, older women grew up in a time when oppression was culturally mandated against many of the roles and identities they hold.
The relationship between stigma, the negative impact on communication, knowledge, and the potential for subsequent risk behaviors is impacted by relational variables or variables that are brought into starker focus in a relational setting. 7 Variables found to contribute to HIV stigma in older women include self esteem, self silencing, and sexual assertiveness. 7 Societal and relational variables including oppression of women, economic dependence on men, loneliness, discrimination, and the valuation of close relationships by women can foster variables such as self silencing, which may maintain stigma and risk.
Siegel and Scrimshaw 31 examined older women’s narratives about sexuality and HIV, and in their sample of 63 older adults found that older HIV-infected women were more likely to choose celibacy (78% of women compared to 36% of men). The reasons for celibacy provided by these women included loss of interest in sex since their diagnosis, aversion to sex, and fear of infecting someone else. They also indicated that pulling back from the time required by a close relationship provided them with the time to focus on their own needs rather than the needs of a partner. This dynamic of time allotment and having to “attend” to a relationship is likely to be more pronounced for women. The narratives accumulated by these authors also reveal strong themes of distrust and anger toward men, and particularly toward the partner that infected them. The choice to abstain from sexual activity and intimate relationships was found to be more emotionally driven for women when compared to the men in this cohort. While celibacy certainly is its own form of “prevention”, the authors astutely point out that the psychological fallout of HIV may result in these women becoming isolationist – which could have implications for mental health, social support, and willingness to engage in and access health care relationships. As such, successful interventions would address the feelings of anger, distrust, and betrayal these women may experience within the context of their own sexual drives to ensure that celibacy represents a true choice that is not diminishing overall quality of life. In addition, social isolation must also be observed through the viewpoint of policies that do not facilitate committed relationships (e.g. lack of support for same sex marriage, housing and other discrimination facing same sex couples), as such, lesbian or bisexual women may be at greater risk for social isolation and by extension for outcomes such as decrements in physical and mental health, poor adherence, and morbidity and mortality. 13
Heterosexist assumptions that all women are in intimate relationships with men can be isolating for women, particularly older women – who may have faced lifelong discrimination and isolation for sexual minority status, or for women who may find themselves in non-traditional living arrangements. Awareness and understanding of a diversity of womens’ relationship statuses, and avoidance of presumption is key in ensuring that those that are providing medical and mental health care services are being maximally responsive to client needs. Fredriksen-Goldsen et al32 found that in older LGB adults that in the dyadic relationships in their sample, high levels of depressive symptomatology were observed, and also highlighted the function of the caregiving relationship as a protection from the negative impacts of discrimination. Dyadic relationships bring numerous benefits and challenges to older women, but they must be considered within a larger social context. Biased assumptions based on traditional relational structures must be avoided and instead objective assessment of these relationships must be standard in all clinical and research settings.
Relationships between men and women in our culture are frequently characterized by power imbalances that can be magnified in light of economic dependency and abuse as well as societally concretized gender inequities – all of which may be pronounced in older women since these characteristics are often lifelong conditions which can magnify in older age. Older women also face a double burden of ageism and sexism, and this can diminish their power in relationships and their ability to successfully interact with health care systems that may leave them feeling misunderstood and ashamed around issues such as later life sexuality. 7 This can be a triple burden or even more pronounced in other groups of older women. For example, older lesbian women are far more likely than men to be living in poverty, 33 and ethnic minority women and disabled women are more likely to be living in poverty than nearly all other groups as well. As such, when examining power imbalances in light of economic inequities, other variables contributing to a greater likelihood of such discrepancies must also be recognized and considered when establishing treatment, research and policy agendas.
Primary Care Issues
Older adults, both men and women, often present with multiple clinical concerns during primary care visits, and as such, routine HIV testing is often missed or not offered. Acute retroviral syndrome may be missed in women over 50, because they are not considered to be probabilistic candidates for HIV infection, however, this can be a critical error as it may delimit the likelihood that women are detected for early infection and given appropriate treatment. For women at any kind of risk, HIV and acute seroconversion should be a differential for flu-like symptoms. However, because many women are not assessed for or presumed to be at risk, this opportunity may often be missed.
Another primary care issue that frequently arises in the population of older adults, including women, is medication interactions and toxicities. These risks are pronounced because of factors including number of medications, patient age, disease severity, renal and hepatic dysfunction, drug metabolic factors, and drug interactions. HAART has also been associated with elevated LH and FSH which in turn can contribute to menstrual irregularities. 34 Santoro et al35 review of menopause in women with HIV suggests that women with HIV evidence earlier menopause, though it is unclear whether this is due to HIV per se or to other risk factors for early menopause that tend to cluster in HIV infected women such as smoking, stress, and drug use.
HIV related symptoms and medication related side effects often mirror age related comorbidities that can be pronounced in older women including anemia, wasting, dyspnea on exertion, rheumatologic disorders, dementia, osteoporosis, lipid abnormalities, insulin resistance, and vulvar and cervical neoplasia. 35,36 Increased cardiovascular disease risk burden is also observed in HIV infected women regardless of whether or not they are receiving HAART. 35 HIV infection has been found to have independent associations with menopause symptoms and in older women, the intersection of HIV and menopause may be observed via greater psychological symptoms from both HIV and menopausal transition. 37
Even more specific issues can arise for trans and gender-nonconforming older adults who may not only be facing the issues around becoming older with HIV but also the use of hormone related treatments as part of gender transition that can further complicate assessment. 38 In addition, many lesbian women, bisexual women, and trans and gender non-conforming adults find that they are misunderstood by health care delivery systems and that these barriers are magnified in the face of poverty, disability status, and ethnic minority status, with a greater likelihood of avoiding healthcare delivery systems due to these systematic prejudices. Because of biases from within their own racial, ethnic and cultural communities, this isolation can result in having few avenues to consider in the face of significant health crises.
Older women report that not only are they having sex, but that they wish to discuss it with their healthcare providers. 10,39 It has been noted that medications and illnesses, including HIV/AIDS can impact sexual health in myriad ways, yet they are often not informed about this possibility, often placing the onus of initiating such communications on the patient. 40 Embarrassment about discussing sex with older adults for fear of offending, especially by younger health care practitioners, can be a barrier to addressing sexual health in older adults. 41
Obesity and the attendant health risks of obesity are more frequently observed in lesbian women, in certain ethnic minority subgroups, can be pronounced in older women who may have limited mobility, and is often associated with socioeconomic status. The health consequences of obesity including diabetes, musculoskeletal stress, and higher cardiovascular risk are likely to be compounded for older women, and once again, the key issue of multiple vulnerabilities as a function of different role statuses cannot be underestimated in assessing and managing health and primary in older women with HIV/AIDS. 13
Medication adherence remains an important issue in HIV care, with adherence to HAART regimens predictive of slower disease progression and better health outcomes. While older adults have been characterized as being more adherent, Bianco et al42 found that only about 50% of older women in their sample were adherent to HAART. They also observed that psychological factors were not useful predictors of adherence in older women, speculating that other factors such as family and caregiving obligations, pill burden, or self efficacy may be more useful predictors in women. 42 Hinkin et al43 observed that older adults per se did not have poorer medication adherence, but rather patients evidencing neuropsychological impairment and with more complex regimens were those that had greater difficulties with medication adherence. As such, it is not presumptive that older adults, or older women specifically would have significant problems in adherence, but that other factors such as cognitive functioning and regimen factors should be considered when monitoring adherence. In general, studies of medication adherence in older HIV infected adults examine both men and women, and do not specifically focus on the needs of HIV positive women.
Knowledge about HIV
Although knowledge about HIV prevention doesn’t necessarily directly translate into behavior, knowledge about transmission, susceptibility, and methods of protection remain an essential ingredient in the arsenal of HIV prevention. In older women who are not infected with HIV, knowledge can be limited, with women maintaining the belief that HIV is not a salient issue for them and maintenance of HIV related stigma. 44,45 Knowledge about the utility of condoms, even amongst those using condoms, has been found to be low in older women who reside in urban communities with high rates of HIV incidence and prevalence, with some studies reporting that only 13% of older women were aware that condoms were very effective in preventing HIV. 23,46 Older women have been observed to maintain some consistent general knowledge about HIV and HIV transmission, but will often have far less personal awareness of their own risks. 47,48 Overall, the literature on knowledge suggests that factual knowledge about HIV/AIDS is generally high, however, personal perceptions and assessments of risk tend to be suboptimal in older women. 24
Risk for HIV
The assumption that older women do not have sex is clearly not supported by the data. Older women do have sex, and value sex as an important part of their lives. 8,9,49,50 As adults live longer, and the advent of medications such as sildenafil make it likely that older men will continue to be able to manage issues such as erectile dysfunction, older adults will continue to want to have sex and will have sex which places them at risk for STIs and HIV. From an infection perspective, incident HIV infections in older women typically occur through heterosexual transmission, but other vectors such as infection through injection drug use are also observed. Mitigation of these risks occurs via safer sex practices or safer injection drug use practices. Older women are less likely to use condoms, with over 90% of women in one national survey reporting no condom use over a 6 month period, and over 90% of those who reported engaging in risky behaviors did not perceive themselves as being at risk. 51 In a sample of sexually active African American and Latina older women (largely HIV negative), Sormanti et al22 observed that 80% of their sample of women had sexual intercourse in the prior 90 days, and 86% reported not using condoms, with 10% indicating that their primary partners placed them at risk for HIV. As will be noted, physiological changes in older women can place them at greater risk for infection, and biological changes due to aging such as decreases in antibody production can also increase vulnerability to HIV. 52
Stigma can be a powerful predictor of risk in women over the age of 50. Compared to gay and bisexual men, older women with HIV are more likely to experience greater stigma across various dimensions including disclosure, negative self-image and public attitudes. 53 Jacobs & Kane 7 found that both personal stigmas about HIV as well as fear of stigma from sexual partners should a woman address safer sex practices can reinforce the likelihood of engaging in risky behaviors (e.g. avoiding condom use instead of talking about it). Stigma can also diminish the likelihood of older women discussing HIV/AIDS and this can in turn diminish the likelihood of older women having accurate information or skills to manage risk behaviors. 54 Stigma also acts to distance women from believing they or their partners are at risk by reinforcing an “us/them” mentality and miscalculation of susceptibility and risk.
Neundorfer et al55 interviewed 24 HIV positive women between the ages of 45 and 71 years and generated narratives which revealed 5 distinct factors that had placed these women at risk for infection with HIV. These risks included (a) drug and alcohol abuse; (b) being unaware of the risk histories of male partners; (c) mental health issues, physical and sexual trauma, and life stressors; (d) taking risks within a relationship; (e) lack of HIV prevention information. These factors are well established in the literature as placing all women at greater risk for infection, and it is also likely that older women may be less likely or less equipped to engage in pointed conversations about partner sexual histories, advocacy for condom use, and seeking out of HIV prevention information, especially since so little of the information and prevention programming is targeted at their experience. The authors observed that for older women, number of partners did decrease, but so too did condom use.
Risk of HIV infection for specific groups such as older lesbian women or trans and gender non-conforming adults occurs within a context not simply of sexual behavior but also of violence, discrimination, and economic instability. Prevention information and education is often predicated on a heterosexist model of disease transmission. In addition, risk is often underestimated in lesbian and bisexual women. Older studies have found that while lesbian and bisexual women may perceive themselves at lower risk, that they were more likely than heterosexual women to report high risk behaviors such as unsafe injection drug use as well as unprotected vaginal and anal sex. 56 In order for risk prevention models to succeed they must develop past presumptive frameworks of sexual risk, and be embedded in contextualized frameworks that account for the intersectionalities facing older women at risk for or living with HIV/AIDS. The stressors associated with sexual minority status have also been associated with not only negative mental and physical health outcomes and distress but also a greater likelihood of high risk sexual behaviors. 57
It has been suggested that some of the success of condom use programs in younger women may emanate from the implementation of such programs within larger sexual education programs that also focus on issues such as pregnancy prevention. Since older women may no longer perceive pregnancy as a risk, the drive for contraception may drop, and subsequently the motivation to use barrier methods such as condoms becomes less salient. In addition, since health care providers are unlikely to discuss sex with older patients, the systems in place may also contribute to older women’s lower perception of risk.
Safe sex practices
The use of barrier methods such as condoms remains a first line of prevention among sexually active adults in new relationships or with partners whose HIV status is unknown. However, the use of condoms and other safe sex practices raises some issues specific to older women. Reproductive health changes in midlife due to perimenopause and menopause can render women more physiologically vulnerable to STIs including HIV. 20 Vaginal dryness secondary to decreasing hormone levels in perimenopausal and menopausal women can heighten the importance of condom use given that lack of lubrication and other changes such as atrophic vaginitis can lead to more efficient viral transmission through mucosal transmission and vaginal tearing. Interventions including the use of water based lubricants and vaginal estrogen preparations should be discussed by primary care and gynecologic health care providers.
Acquiring condoms has also been found to be associated with safer sex practices, and Paranjape et al23 found that personally acquiring condoms was associated with safe sex decisions, which they believe may be a correlate of greater self efficacy. However, these authors also found that safer sex practices were observed even when older women in their sample depended on men to provide condoms.
Neuropsychiatric Factors and HIV in Older Adults
Overall, HIV infected older adults are more likely to have more depressive symptoms, suicidal ideation, AIDS related stigma, and comorbid health conditions. 11,58,59 Loneliness and HIV related stigma are associated with depression in older HIV positive adults. 59 We found that 67% of older women in our dataset reported a current Axis I diagnosis, compared to 50% of younger women. 21
HIV has been well documented to have direct effects on the CNS, and with a range of neurocognitive symptoms ranging from minor cognitive disorder to HIV associated dementia (for a thorough review of the neuropsychological issues of HIV/AIDS in older adults see Hardy & Vance). 60 Very few studies of the neuropsychology of HIV have focused exclusively on older women, and few take on the issue of women at any age. Those studies that have focused on women, suggest that HIV seropositive women evidence more impairment than HIV negative women, with the greatest impairments observed on psychomotor tasks, and that impairment was more frequently observed in those not receiving HAART. 61,62 In general, older age is associated with poorer performance in multiple domains including memory, executive functioning and motor/psychomotor performance when older adults are compared to younger adults. 60,63 Age increases risk for neurocognitive symptoms in women with HIV. In older women with HIV, they may be facing multiple threats to cognition including normal aging, HIV, lifelong issues including substance use or neurological insults, and in a subset of women, low education. Research on the use of post-menopausal hormonal replacement therapies has shown mixed results, and may have some promise for mitigation of symptoms in older women, though further research targeted at HIV infected older women is needed. 64,65
An overview of psychiatric, psychological and cognitive evaluation in older adults reveals that evaluations that encompass all of the following should represent standard of care in evaluation and monitoring of older women with HIV: (a) cognitive impairment; (b) depression; (c) anxiety; (d) PTSD; (e) suicidal ideation; (f) alcohol and substance use; (g) sleep and appetite; (h) psychiatric history and psychiatric medications; (i) psychosocial issues (e.g. IPV, housing, supports); (j) caregiving responsibilities.
Substance Use and Abuse
In the general population of older women, it has been estimated that approximately 10% abuse drugs or alcohol. 66 Older women may also be more physiologically vulnerable to the effects of alcohol and selected drugs. 66 Much like the underassessment of sexual risk because it is assumed that older women don’t have sex, substance use is often also missed in older women because they are not believed to be at risk for drug use or because their use is not causing disruption in the lives of others. While the vast majority of older women report being infected via heterosexual transmission, there is still a significant proportion (10–30%) that were infected via injection drug use. In addition, drug use is often an indirect vector of HIV as it may contribute to risky sexual decision making, and substance dependence may place a woman at risk for exchanging sex for drugs or money.55,67
When compared to cohorts of younger women, older women have been found to have lower rates of substance use. 68 However, in lesbian and bisexual women, older age does not confer a protective effect against alcohol and drug use, and that overall lesbian and bisexual women are at greater risk for alcohol and drug use disorders. 69 In an analysis of the literature on women, substance use and HIV across women of all ages, Barroso & Sandelowski67 found that a diagnosis of HIV often motivated women to want to abstain from drug use as part of taking back their health or taking back custody of children. HIV positive women with substance use histories typically had histories characterized by sexual and physical abuse, familial substance abuse histories, IPV and trauma. Over the course of a lifetime, these variables will have impacts on older women, who may still experience difficulties with sexual decision making or ongoing maintenance of sobriety. Narratives of older HIV seropositive women reveal that large proportions of women reported histories of substance use (71%) but of the 24 women studied in a qualitative study, none reported current alcohol or drug abuse. 55 In our sample of 71 HIV+ women, 20 of whom were over the age of 50, 85% reported a lifetime history of substance abuse/dependence, while 10% reported a current history of abuse. These rates were comparable to those reported by younger women in our sample (12% current, 70% lifetime). 21 Assumptions that drug or alcohol use may be less prevalent in older women, and the potential augmentation of the impact of drug and alcohol use in older women reveals that assessment of substance use in older women must be conducted in a contextualized manner (and mindful of sexual orientation, ethnic minority status, and trauma history).
Psychosocial Issues in Older Women Living with HIV/AIDS
Regardless of HIV serostatus, caregiving issues represent a unique factor for older women who may be assisting adult children with young children, and may even be caring for elderly parents. In addition, older women may also have partners or spouses who may require assistance. These responsibilities can impede self-care in older women and contribute to fatigue, financial burdens, and overall mental, psychological, emotional and physical burden. 70 These issues are likely to be compounded in older women who are also managing the burdens of HIV. In addition, these ongoing stressors contribute to overall burden and allostatic load in women already burdened by the wear and tear of HIV/AIDS, other comorbid health conditions, and normal aging.
Studies of women living with HIV/AIDS at all ages reveal that psychological stressors are a key factor in women’s experience of the illness. Physiological stressors include the infection itself, access to care, gynecologic symptoms, other health conditions, and stigma within the health care system. 71 Psychological stressors are wide ranging and include universal stressors such as finances, employment related stress, and interpersonal relationships, as well as HIV specific stressors such as fear of disclosure, stigma about HIV, body image issues, fear of infecting others or finding a partner, and end of life issues. 71,72 Social support can be a complex issue for women, and especially HIV infected women. The various elements of support including emotional, instrumental, and informational support can be key coping tools for women with HIV, and interventions focused on shoring up social support can have utility for coping with HIV and non-HIV related stressors. 71 However, virtually no studies focus on social support and stressors in older women with HIV/AIDS. While older women may actually have larger networks than younger women or men living with HIV/AIDS, these networks can also be a source of demand and burden. A large proportion of older women have also been observed to not be prepared for the legal and procedural issues that may arise in later life that are related to management of their health care and decision making (e.g. advance directives, power of attorney/conservatorship, probate).
There also remains the issue of caregiving FOR women with HIV/AIDS. A substantial proportion of older women with HIV/AIDS are not married or do not have long term partners that are willing or able to engage in caregiving. Adult children may also not be available for such duties. Literature on caregiving by and for older lesbian women reveals there is often concern about availability of caregiving at the time it would become necessitated, 32 and that prejudice and discrimination can be major impediments to receiving caregiving in older age – an association that would be magnified in sexual minorities, ethnic minority women, disabled women and magnified amongst those with limited financial resources. Intersectional identities and experiences – aging, chronic illness, poverty, disability status, sexual orientation, gender, and HIV – highlight the importance of addressing both discrimination and the additive risk of these intersecting identities on health and disease. 32
Interventions Targeting Older Women Living with HIV/AIDS
Bringing HIV intervention and prevention programs to older women requires awareness of the cultural variables they bring to the table. Older women may be less likely to use technologically driven programs such as those delivered by the internet, or may be less likely to turn to media that may offer safer sex messages and likely skews to a younger demographic. Targeting accessible and approachable spaces where older women may already come together to foster such prevention programs (e.g. churches) may be a useful tool to proliferate safer sex and risk awareness messages, 29 however the content of such communications and programs may still leave women reticent even if they are housed within approachable structures. Curricula that are ethnically responsive, and account for education, skills training, and coping were found to be acceptable by cohorts of older women. 29 In addition, older women may also reside in assisted living settings where they may feel less able to discuss stigmatized issues such as sex, STI’s and HIV because it is their residential community and they may fear stigmatization. This then becomes a training issue for practitioners in these settings, and a mandate that practitioners in these settings make discussion of these issues a normalized part of care and dialogue within these communities. 7
While not specifically targeted at older women, Orel et al12 provide 4 thematic recommendations to account for when developing prevention materials for older adults. They caution that these recommendations must be contextualized for specific target groups on the basis of sociodemographic factors, cultural variables, and physical/cognitive/psychological functioning.
Raise older adults’ perceived sense of susceptibility to HIV/AIDS
Provide appropriate HIV/AIDS factual information
Incorporate HIV/AIDS risk reduction strategies
Emphasize early intervention – testing and treatment options
(Orel et al12 (p.498–499)). When considering the contextualization of these issues into a gendered framework – issues such as awareness of partner characteristics, addressing physiological changes that can impact sexual health in older women, opening up primary care practitioners to being more directive in addressing sex with older women, establishing psychosocial and psychological supports and minimizing testing and treatment delays should remain a key focus in programs for older women.
Age, Culture, Economics, Ethnicity and Risk
Cornelius et al29 also highlight the role of ethnicity in considering relational variables. Citing Utz 73 they point out that 74% of older African American women are not in a relationship due to widowhood or divorce. However, this group of women often has less than accurate appraisals of risk (e.g. believing HIV can be transmitted through coughing), and little regular condom use. Nonetheless, Cornelius et al29 actually found that older African American women were willing to discuss condom use and sexual behavior with their partners.
Lesbian and bisexual women have received virtually no attention in the research on HIV/AIDS. Because lesbian women may have a current or past history of sex with men, a self-identification as being lesbian may not obviate risk. 74 In addition, in older women who presently self-identify as exclusively lesbian, over the course of a lifetime it is still not known whether a woman has had sex with men, and many health care practitioners may not feel comfortable asking an older woman this question. Informed and responsive health care options are often limited for lesbian, trans and gender-nonconforming older adults, and health care providers are often woefully underinformed about the specific health issues facing trans and gender nonconforming populations in particular. 38 Older women are a diverse group, and it would be erroneous to assume that all older women with HIV/AIDS or those who are not infected will behave in similar ways. By recognizing that older women, by dint of age and life experience, bring more experiences, risks, and expectations and who may be at very variable relationship stages (e.g. some who are in long term marriages, others entering new relationships) –interventions with this group must be dynamic and recognize universal factors such as perimenopausal and menopausal changes, but contextualizing such issues in a framework of diversity74
The myriad issues facing older women with HIV – sexual health changes due to aging, gaps in knowledge, inaccurate perceptions of risk, ageism, relational factors, and other transitions due to aging make this a group, that while not overrepresented in prevalence statistics will continue to grow as the HIV infected population lives longer and ages. Economic issues are also critical to understand as many of these women may have had lifelong financial hardship, but are also less likely to garner new employment for age related reasons and are facing the limitations of a fixed income despite greater financial need. It will be critical to transform Emlet & Poindexter’s 2 characterization of this group as “unserved, unseen and unheard” – and develop interventions, responsive primary health care and integrated treatment programs that serve, see and hear this group of women.
Themes of resilience and aspiration
There are some losses and anxieties more specific to older adults, and typically older women with HIV. Murphy et al75 addressed the issue of “empty nest” issues in older HIV positive women and described worries including: (a) identity loss; (b) loss of social support; (c) financial insecurity; (d) worsening physical health; and (e) death and dying. Many of these concerns are universal among any older mothers dealing with the transitions of adult children, but the risks of morbidity and mortality and the psychosocial stressors associated with HIV can magnify these empty nest issues in older HIV seropositive women. The authors also pointed out that the same women also listed hopes including (a) self-improvement; (b) change of life focus; (c) travel; (d) romantic partners; and (e) familial ties. But again, while these are universal hopes for older women, HIV serostatus can complicate the achievement of these hopes and goals. Many older women living with HIV/AIDS managed caregiver duties while also managing illness related issues, and the shifting identity as well as fears of growing older with a potentially stigmatizing illness raises issues that must be addressed in comprehensive intervention programs that work with older women living with HIV/AIDS.
Emlet et al76 highlight the finding of resilience in older adults with HIV, drawn from narratives of both older women and men living with HIV. These themes include (a) self-acceptance; (b) optimism; (c) will to live; (d) generativity; (e) self-management; (f) relational living; and (g) independence. These themes should be built upon and shored up in any interventions with older women with HIV, as they provide a foundational structure which may result in better self-care, and better quality of life for older women living with HIV/AIDS.
Takeaways and Conclusions
A model for contextualized care, prevention and research in older women with HIV/AIDS can guide key recommendations based on the small extant literature targeting this population of women. First of all it is essential to recognize that all of the recommendations issued below must be viewed within the context of poverty, race, ethnicity, culture, systems of care, psychosocial variables (social support, coping resources, role strains, environmental stressors), extant structures of power/oppression that differentially impact older women, discrimination, disability status (which is more likely to be observed or pronounced in older women), history of trauma/violence or ongoing violence within the context of a relationship. In addition, accounting for the strengths that older women with HIV/AIDS maintain such as resilience, is key in harnessing their sense of efficacy as partners in care. Best practices calls for multidisciplinary teams that provide primary care, psychological services, ongoing assessment of change, and address barriers such as housing, nutrition, transportation, and access.
Care
In the early years of the HIV epidemic, research on women lagged, and rates of infection increased before women were sufficiently targeted by prevention programs, as well as tailored primary care. This resulted in delays in responsive care for women, who often presented with very different issues medically and psychologically. The risk for the same delays may occur again with older women. Even societal stigmas such as our avoidance of talking about sex in older people may contribute to more incident infections, ignorance about intersectionality and risk, less targeted prevention programs, and delays in care for older adults, and particularly women. 20
Fundamental recommendations for primary care for older women include the following:
Training in health care provider communication and awareness
Health care providers must be trained to query older women about sexual behavior and drug use as standard of care. Discomfort with such assessment and misassumptions must be addressed to ensure that older women aren’t being missed in terms of HIV testing and early initiation of treatment. HIV testing should be a standard part of comprehensive medical care for older women.
Supporting adherence
Older women with HIV may face unique barriers to adherence that are magnified by issues including socioeconomic status, stigma, discriminatory health care systems, and a dearth of providers that specifically target the clinical needs of older women with HIV/AIDS. Identifying and addressing barriers to adherence specific to older women is an essential element of primary care.
Menopause and treatment issues
Peri-menopausal and menopausal women may face the added vulnerability to becoming infected due to physiological changes and in addition, the ramifications of the interaction of hormone replacement therapy and HAART is still being determined. Health care providers working with older women must remain mindful of the impact of menopause on sexual risk and of the interactions of other medications with HAART in this group.
Shoring up support networks
Traditional expectations of caregiving and support cannot be maintained with older women with HIV/AIDS. Older women with HIV/AIDS may not have traditional relationship or family structures to provide assistance, may have limited access to financial resources to afford care, and may face discriminatory social structures that limit their ability to access care. Health care providers must carefully assess availability of support and caregiving, especially given the impact that this can have on physical and mental health outcomes.
Neuropsychiatric changes
Age related cognitive changes, as well as cognitive and psychiatric changes due to menopause must be considered within the context of HIV/AIDS which can also independently contribute to cognitive slowing, apathy, and other neuropsychiatric sequelae. Careful assessment of neuropsychiatric variables in older women with HIV/AIDS is essential for monitoring changes and to make determinations regarding medications and psychiatric care.
Paniagua & O’Boyle 77 suggest that six domains should be consistently addressed in assessment and research with HIV infected older adults. These recommendations derive from literature as well as their own survey research. They suggest that the domains include (a) knowledge of factual information and inaccuracies regarding HIV transmission; (b) personal sense of internal vs. external control of the cognitive and behavioral factors associated with HIV prevention; (c) perceived peer norms about HIV; (d) intention to change behaviors when faced with HIV risks; (e) communication with partners and family; and (f) assessment of behavioral risks for HIV. All of these factors are contributors to understanding HIV risk in older adults, and by applying a systematic framework, the authors are suggesting that we will better understand risk in diverse populations of older adults.
Prevention
Some basic shifts are needed to ensure that older women who are at risk for HIV/AIDS and those living with HIV/AIDS are recipients of appropriate prevention materials. Age appropriate risk reduction materials must be developed that feature images of older women and address issues specific to older women such as menopause, dating in midlife and later life, and discussing sexuality with primary care providers. There are also needs to be an expansion of simplistic risk reduction training to include broader issues such as relationship dynamics, ensuring that prevention programs specifically address subgroups of women who have been traditionally missed by prevention programs and materials (e.g. lesbian women, disabled women) power and oppression, ageism, self esteem, interpersonal assertiveness, and sexual communication to allow for more authentic and effective programming. In addition, better training of all care providers is needed to better address and assess risk, and this includes patient education, provision of HIV testing, and early detection and treatment.
Comorbidities
Older women with HIV face other comorbidities and age related transitions that must be considered in assessment and treatment:
Neuropsychiatric changes
Health changes due to menopause
Pain and neuropathy
Ongoing drug, alcohol and tobacco use
Shifts in cardiovascular health
Age related immune decline
Musculoskeletal vulnerabilities including osteoporosis
Caregiver issues and access to psychosocial supports
As both men and women with HIV/AIDS live longer and remain sexually active into later life, remaining aware of these comorbidities and co-occurring issues becomes key to ensure that synergistic progressive conditions are being appropriately managed and that misdiagnosis is not resulting in mismanagement and undertreatment of symptomatology.
Research agendas
The model used to guide this review can also serve as a roadmap for the areas of empirical investigation that must be pursued with older women with HIV/AIDS. At a minimum, large, longitudinal studies examining the natural history of HIV/AIDS in older women that also examine variables including menopause, hormone replacement therapy, and other age related shifts such as age related cognitive changes are essential. In addition, speculation about older women’s sexuality must be replaced with data about sexual choice, behavior, and condom use to address both prevention and quality of life in older women with HIV/AIDS. Finally, there is a profound need for better research on the use of HAART in older women with HIV/AIDS, particularly amongst those who may also be receiving hormone replacement, or simply to determine the impact of HAART on older women. Few clinical trials to date have focused specifically on this subgroup, and this will be essential as more women become infected and live longer with HIV. All research must strive to adequately sample this diverse population of interest. The heterogeneity within the sample of older women living with HIV/AIDS can easily be lost if studies do not attempt to address across the spectrum of women on the basis of economic status, race, ethnicity, sexual orientation, disability status, motherhood, and years since infection.
Finally, extant research highlighting themes of resilience focus the need to also move away from a deficit approach to understanding aging and HIV, and to build upon existing strengths in these women. Narratives from older women highlight their hopes for success, relationships, and health in later life despite, and in some cases because of HIV/AIDS. As such, ongoing work with this sample of women should not fall prey to an overfocus on disease, but also address shoring up strengths and promulgating better quality of life in older women living with HIV.
Policy guidelines
While policy guidelines can be developed to ensure that older women receive testing, prevention training, and better primary care, ultimately, shifts in policy that address power/oppression differentials in educational and occupational systems, health care delivery, and intimate relationships must occur in parallel to prevention, care, and research recommendations. For example, legislation such as the Family and Medical Leave Act of 1993 often does not support caregiving that occurs within a same-sex relationship or within networks of friends. 32 The issue of intersectionality may be even more pronounced for older women as primary care, prevention and integrated intervention programs must account for not only HIV serostatus but also ethnicity, disability status, sexual orientation, socioeconomic status, and be mindful of ageism all of which can often complicate information seeking in older women. In addition, groups that face even greater vulnerability due to socioeconomic status, ethnic minority status, sexual orientation, gender orientation, and disability status must be afforded greater access and human rights protections. Societal biases such as HIV related stigma interact with ageist biases, and attempts to address this via policy shifts, education and training are key in generating systems of care, prevention and research that can operate more efficiently and responsively to the needs of an aging population of women with HIV/AIDS.
While the present review was focused on the issues facing older women with HIV/AIDS in the United States, international research focused on older women with HIV/AIDS suggests that key contributors to increased morbidity and mortality for older women with HIV/AIDS include limited health care, lack of resources, caregiving and omission from research and prevention programs. Similarly, in the US, there are certain subgroups of women more vulnerable to these barriers, and ongoing awareness and capacity building to ensure higher standards of care for vulnerable groups of older women living with HIV/AIDS are needed.
Acknowledgments
Dr. Durvasula would like to acknowledge the editorial and literature review assistance provided by Mr. Theodore Miller as well as acknowledging the participants of the Health Adherence Research Project who were willing to share their stories as a part of this research.
This work was supposed in part by NIMH Grant 1SC1MH093181-01A1.
Footnotes
Data referred to by Dr. Durvasula has been collected with the approval of the Institutional Review Boards for both California State University, Los Angeles and Charles Drew University.
References
- 1.Leland J. People think it’s over.’ spared death, aging people with H.I.V. struggle to live. [Accessed 10/15/2013];The New York Times. 2013 Jun 01;2013 Available from: http://www.nytimes.com/2013/06/02/nyregion/spared-death-aging-people-with-hiv-struggle-to-live.html?_r=0. [Google Scholar]
- 2.Emlet CA, Poindexter CC. Unserved, unseen, and unheard: Integrating programs for HIV-infected and HIV-affected older adults. Health Soc Work. 2004;29(2):86–96. doi: 10.1093/hsw/29.2.86. [DOI] [PubMed] [Google Scholar]
- 3.Center For Disease Control and Prevention. HIV/AIDS among persons aged 50 and older. CDC HIV/AIDS FactS. 2008 [Google Scholar]
- 4.Tabnak F, Sun R. Need for HIV/AIDS early identification and preventive measures among middle-aged and elderly women. Am J Public Health. 2000;90(2):287. doi: 10.2105/ajph.90.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Center For Disease Control and Prevention. Diagnoses of HIV infection among adults aged 50 years and older in the united states and dependent areas, 2007–2010. HIV Surveillance Supplemental. 2013;18(3) [Google Scholar]
- 6.Mack KA, Ory MG. AIDS and older americans at the end of the twentieth century. JAIDS J Acquired Immune Defic Syndromes. 2003;33:S68–S75. doi: 10.1097/00126334-200306012-00003. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs RJ, Kane MN. HIV-related stigma in midlife and older women. Soc Work Health Care. 2010;49(1):68–89. doi: 10.1080/00981380903018140. [DOI] [PubMed] [Google Scholar]
- 8.Lindau ST, Leitsch SA, Lundberg KL, Jerome J. Older women’s attitudes, behavior, and communication about sex and HIV: A community-based study. Journal of Women’s Health. 2006;15(6):747–753. doi: 10.1089/jwh.2006.15.747. [DOI] [PubMed] [Google Scholar]
- 9.Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the united states. N Engl J Med. 2007;357(8):762–774. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farrell J, Belza B. Are older patients comfortable discussing sexual health with nurses? Nurs Res. 2012;61(1):51–57. doi: 10.1097/NNR.0b013e31823a8600. [DOI] [PubMed] [Google Scholar]
- 11.Emlet CA. “You’re awfully old to have this disease”: Experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. Gerontologist. 2006;46(6):781–790. doi: 10.1093/geront/46.6.781. [DOI] [PubMed] [Google Scholar]
- 12.Orel NA, Spence M, Steele J. Getting the message out to older adults: Effective HIV health education risk reduction publications. Journal of Applied Gerontology. 2005;24(5):490–508. [Google Scholar]
- 13.Fredriksen-Goldsen KI, Kim H, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: Results from a population-based study. Am J Public Health. 2013;(0):e1–e8. doi: 10.2105/AJPH.2012.301110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Branson B, Handsfield H, Lampe M, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Morbidity and Mortality Weekly Report, MMRW. 2005;RR-14:1–17. [PubMed] [Google Scholar]
- 15.Siegel K, Schrimshaw EW, Dean L. Symptom interpretation: Implications for delay in HIV testing and care among HIV-infected late middle-aged and older adults. AIDS Care. 1999;11(5):525–535. doi: 10.1080/09540129947686. [DOI] [PubMed] [Google Scholar]
- 16.Harawa NT, Leng M, Kim J, Cunningham WE. Racial/ethnic and gender differences among older adults in nonmonogamous partnerships, time spent single, and HIV testing. Sex Transm Dis. 2011;38(12):1110. doi: 10.1097/OLQ.0b013e31822e614b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDavid K, Li J, Lee LM. Racial and ethnic disparities in HIV diagnoses for women in the united states. JAIDS J Acquired Immune Defic Syndromes. 2006;42(1):101–107. doi: 10.1097/01.qai.0000199353.11479.08. [DOI] [PubMed] [Google Scholar]
- 18.Akers A, Bernstein L, Henderson S, Doyle J, Corbie-Smith G. Factors associated with lack of interest in HIV testing in older at-risk women. Journal of Women’s Health. 2007;16(6):842–858. doi: 10.1089/jwh.2006.0028. [DOI] [PubMed] [Google Scholar]
- 19.Schable B, Chu SY, Diaz T. Characteristics of women 50 years of age or older with heterosexually acquired AIDS. Am J Public Health. 1996;86(11):1616–1618. doi: 10.2105/ajph.86.11.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sherman CA, Harvey SM, Noell J. “Are they still having sex?” STIs and unintended pregnancy among mid-life women. J Women Aging. 2005;17(3):41–55. doi: 10.1300/J074v17n03_04. [DOI] [PubMed] [Google Scholar]
- 21.Durvasula RS. Progress report: Psychopathology, decision making and sexual risk. 2013. [Google Scholar]
- 22.Sormanti M, Wu E, El-Bassel N. Considering HIV risk and intimate partner violence among older women of color: A descriptive analysis. Women Health. 2004;39(1):45–63. doi: 10.1300/J013v39n01_03. [DOI] [PubMed] [Google Scholar]
- 23.Paranjape A, Bernstein L, St George DM, Doyle J, Henderson S, Corbie-Smith G. Effect of relationship factors on safer sex decisions in older inner-city women. Journal of Women’s Health. 2006;15(1):90–97. doi: 10.1089/jwh.2006.15.90. [DOI] [PubMed] [Google Scholar]
- 24.Zablotsky D, Kennedy M. Risk factors and HIV transmission to midlife and older women: Knowledge, options, and the initiation of safer sexual practices. JAIDS J Acquired Immune Defic Syndromes. 2003;33:S122–S130. doi: 10.1097/00126334-200306012-00009. [DOI] [PubMed] [Google Scholar]
- 25.Stockman JK, Lucea MB, Campbell JC. Forced sexual initiation, sexual intimate partner violence and HIV risk in women: A global review of the literature. AIDS and Behavior. 2013:1–16. doi: 10.1007/s10461-012-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’campo P. HIV/AIDS and intimate partner violence intersecting women’s health issues in the united states. Trauma, Violence, & Abuse. 2007;8(2):178–198. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- 27.Campbell JC, Baty M, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: A review. International journal of injury control and safety promotion. 2008;15(4):221–231. doi: 10.1080/17457300802423224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wyatt GE, Myers HF, Williams JK, et al. Does a history of trauma contribute to HIV risk for women of color? implications for prevention and policy. Am J Public Health. 2002;92(4):660–665. doi: 10.2105/ajph.92.4.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cornelius JB, Moneyham L, LeGrand S. Adaptation of an HIV prevention curriculum for use with older african american women. Journal of the Association of Nurses in AIDS Care. 2008;19(1):16–27. doi: 10.1016/j.jana.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 30.Amaro H, Raj A. On the margin: Power and women’s HIV risk reduction strategies. Sex roles. 2000;42(7–8):723–749. [Google Scholar]
- 31.Siegel K, Schrimshaw EW. Reasons for the adoption of celibacy among older men and women living with HIV/AIDS. J Sex Res. 2003;40(2):189–200. doi: 10.1080/00224490309552180. [DOI] [PubMed] [Google Scholar]
- 32.Fredriksen-Goldsen KI, Kim H, Muraco A, Mincer S. Chronically ill midlife and older lesbians, gay men, and bisexuals and their informal caregivers: The impact of the social context. Sexuality Research and Social Policy Journal of NSRC. 2009;6(4):52–64. doi: 10.1525/srsp.2009.6.4.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sears JT. Introduction: Queering later life. 2008. [Google Scholar]
- 34.Santoro N, Lo Y, Moskaleva G, et al. Factors affecting reproductive hormones in HIV-infected, substance-using middle-aged women. Menopause. 2007;14(5):859–865. doi: 10.1097/GME.0b013e31802f7369. [DOI] [PubMed] [Google Scholar]
- 35.Santoro N, Fan M, Maslow B, Schoenbaum E. Women and HIV infection: The makings of a midlife crisis. Maturitas. 2009;64(3):160–164. doi: 10.1016/j.maturitas.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.New York State Department of Health AIDS Institute. HIVguidelines. 2008. Medical care for menopausal and older women with HIV infection. 11/5/13. [Google Scholar]
- 37.Ferreira CE, Pinto-Neto AM, Conde DM, Costa-Paiva L, Morais SS, Magalhaes J. Menopause symptoms in women infected with HIV: Prevalence and associated factors. Gynecological Endocrinology. 2007;23(4):198–205. doi: 10.1080/09513590701253743. [DOI] [PubMed] [Google Scholar]
- 38.Finkenauer S, Sherratt J, Marlow J, Brodey A. When injustice gets old: A systematic review of trans aging. J Gay Lesbian Soc Serv. 2012;24(4):311–330. [Google Scholar]
- 39.Hinchliff S, Gott M. Seeking medical help for sexual concerns in mid-and later life: A review of the literature. J Sex Res. 2011;48(2–3):106–117. doi: 10.1080/00224499.2010.548610. [DOI] [PubMed] [Google Scholar]
- 40.Lemieux L, Kaiser S, Pereira J, Meadows LM. Sexuality in palliative care: Patient perspectives. Palliat Med. 2004;18(7):630–637. doi: 10.1191/0269216304pm941oa. [DOI] [PubMed] [Google Scholar]
- 41.Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med. 2004;58(11):2093–2103. doi: 10.1016/j.socscimed.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 42.Bianco JA, Heckman TG, Sutton M, Watakakosol R, Lovejoy T. Predicting adherence to antiretroviral therapy in HIV-infected older adults: The moderating role of gender. AIDS and Behavior. 2011;15(7):1437–1446. doi: 10.1007/s10461-010-9756-2. [DOI] [PubMed] [Google Scholar]
- 43.Hinkin C, Castellon S, Durvasula R, et al. Medication adherence among HIV adults effects of cognitive dysfunction and regimen complexity. Neurology. 2002;59(12):1944–1950. doi: 10.1212/01.wnl.0000038347.48137.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hillman J. Knowledge and attitudes about HIV/AIDS among community-living older women: Reexamining issues of age and gender. J Women Aging. 2007;19(3–4):53–67. doi: 10.1300/J074v19n03_05. [DOI] [PubMed] [Google Scholar]
- 45.Savasta AM. HIV: Associated transmission risks in older adults–an integrative review of the literature. Journal of the Association of Nurses in AIDS Care. 2004;15(1):50–59. doi: 10.1177/1055329003252051. [DOI] [PubMed] [Google Scholar]
- 46.Henderson SJ, Bernstein LB, George DMS, Doyle JP, Paranjape AS, Corbie-Smith G. Older women and HIV: How much do they know and where are they getting their information? J Am Geriatr Soc. 2004;52(9):1549–1553. doi: 10.1111/j.1532-5415.2004.52421.x. [DOI] [PubMed] [Google Scholar]
- 47.Winningham A, Richter D, Corwin S, Gore-Felton C. Perceptions of vulnerability to HIV among older african american women: The role of intimate partners. Journal of HIV/AIDS & Social Services. 2004;3(1):25–42. [Google Scholar]
- 48.Williams PB, Ekundayo O, Udezulu IE, Omishakin AM. An ethnically sensitive and gender-specific HIV/AIDS assessment of african american women: A comparative study of urban and rural american communities. Fam Community Health. 2003;26(2):108–123. doi: 10.1097/00003727-200304000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Robinson JG, Molzahn AE. Sexuality and quality of life. J Gerontol Nurs. 2007;33(3):19–27. doi: 10.3928/00989134-20070301-05. quiz 38–9. [DOI] [PubMed] [Google Scholar]
- 50.DeLamater J, Moorman SM. Sexual behavior in later life. J Aging Health. 2007;19(6):921–945. doi: 10.1177/0898264307308342. [DOI] [PubMed] [Google Scholar]
- 51.Binson D, Pollack L, Catania JA. Aids-related risk behaviors and safer sex practices of women in midlife and older in the united states: 1990 to 1992. Health Care Women Int. 1997;18(4):343–354. doi: 10.1080/07399339709516289. [DOI] [PubMed] [Google Scholar]
- 52.Levy JA. AIDS and injecting drug use in later life. Res Aging. 1998;20(6):776–797. [Google Scholar]
- 53.Brennan DJ, Emlet CA, Brennenstuhl S, Rueda S. Sociodemographic profile of older adults with HIV/AIDS: Gender and sexual orientation differences. Canadian Journal on Aging/La Revue canadienne du vieillissement. 2013;32(1):31–43. doi: 10.1017/S0714980813000068. [DOI] [PubMed] [Google Scholar]
- 54.Montoya ID, Whitsett DD. New frontiers and challenges in HIV research among older minority populations. JAIDS J Acquired Immune Defic Syndromes. 2003;33:S218–S221. doi: 10.1097/00126334-200306012-00019. [DOI] [PubMed] [Google Scholar]
- 55.Neundorfer MM, Harris PB, Britton PJ, Lynch DA. HIV-risk factors for midlife and older women. Gerontologist. 2005;45(5):617–625. doi: 10.1093/geront/45.5.617. [DOI] [PubMed] [Google Scholar]
- 56.Lemp GF, Jones M, Kellogg TA, et al. HIV seroprevalence and risk behaviors among lesbians and bisexual women in san francisco and berkeley, california. Am J Public Health. 1995;85(11):1549–1552. doi: 10.2105/ajph.85.11.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grossman AH, D’augelli AR, O’connell TS. Being lesbian, gay, bisexual, and 60 or older in north america. J Gay Lesbian Soc Serv. 2002;13(4):23–40. [Google Scholar]
- 58.Heckman TG, Heckman B, Kochman A, Sikkema KJ, Suhr J, Goodkin K. Psychological symptoms among persons 50 years of age and older living with HIV disease. Aging & Mental Health. 2002;6(2):121–128. doi: 10.1080/13607860220126709a. [DOI] [PubMed] [Google Scholar]
- 59.Grov C, Golub SA, Parsons JT, Brennan M, Karpiak SE. Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care. 2010;22(5):630–639. doi: 10.1080/09540120903280901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hardy DJ, Vance DE. The neuropsychology of HIV/AIDS in older adults. Neuropsychol Rev. 2009;19(2):263–272. doi: 10.1007/s11065-009-9087-0. [DOI] [PubMed] [Google Scholar]
- 61.Maki PM, Martin-Thormeyer E. HIV, cognition and women. Neuropsychol Rev. 2009;19(2):204–214. doi: 10.1007/s11065-009-9093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Richardson JL, Martin EM, Jimenez N, et al. Neuropsychological functioning in a cohort of HIV infected women: Importance of antiretroviral therapy. Journal of the International Neuropsychological Society. 2002;8(06):781–793. doi: 10.1017/s1355617702860064. [DOI] [PubMed] [Google Scholar]
- 63.Sacktor N, Skolasky R, Selnes OA, et al. Neuropsychological test profile differences between young and old human immunodeficiency virus-positive individuals. J Neurovirol. 2007;13(3):203–209. doi: 10.1080/13550280701258423. [DOI] [PubMed] [Google Scholar]
- 64.Santoro N, Fan M, Maslow B, Schoenbaum E. Women and HIV infection: The makings of a midlife crisis. Maturitas. 2009;64(3):160–164. doi: 10.1016/j.maturitas.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Maki PM, Zonderman AB, Resnick SM. Enhanced verbal memory in nondemented elderly women receiving hormone-replacement therapy. Am J Psychiatry. 2001;158(2):227–233. doi: 10.1176/appi.ajp.158.2.227. [DOI] [PubMed] [Google Scholar]
- 66.Finfgeld-Connett DL. Treatment of substance misuse in older women: Using a brief intervention model. J Gerontol Nurs. 2004;30(8):30–37. doi: 10.3928/0098-9134-20040801-07. [DOI] [PubMed] [Google Scholar]
- 67.Barroso J, Sandelowski M. Substance abuse in HIV-positive women. Journal of the Association of Nurses in AIDS Care. 2004;15(5):48–59. doi: 10.1177/1055329004269086. [DOI] [PubMed] [Google Scholar]
- 68.Schable B, Chu SY, Diaz T. Characteristics of women 50 years of age or older with heterosexually acquired AIDS. Am J Public Health. 1996;86(11):1616–1618. doi: 10.2105/ajph.86.11.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Green KE, Feinstein BA. Substance use in lesbian, gay, and bisexual populations: An update on empirical research and implications for treatment. Psychology of Addictive Behaviors. 2012;26(2):265. doi: 10.1037/a0025424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chimwaza AF, Watkins SC. Giving care to people with symptoms of AIDS in rural sub-saharan africa. 2004. [DOI] [PubMed] [Google Scholar]
- 71.Hudson AL, Lee KA, Miramontes H, Portillo CJ. Social interactions, perceived support, and level of distress in HIV-positive women. Journal of the Association of Nurses in AIDS Care. 2001;12(4):68–76. doi: 10.1016/S1055-3290(06)60218-5. [DOI] [PubMed] [Google Scholar]
- 72.Sowell R, Seals B, Moneyham L, Demi A, Cohen L, Brake S. Quality of life in HIV-infected women in the south-eastern united states. AIDS Care. 1997;9(5):501–512. doi: 10.1080/713613191. [DOI] [PubMed] [Google Scholar]
- 73.Utz RL. The single older woman: Life after marriage. Gerontologist. 2005;45(3):411–414. [Google Scholar]
- 74.Zablotsky D, Kennedy M. Risk factors and HIV transmission to midlife and older women: Knowledge, options, and the initiation of safer sexual practices. JAIDS J Acquired Immune Defic Syndromes. 2003;33:S122–S130. doi: 10.1097/00126334-200306012-00009. [DOI] [PubMed] [Google Scholar]
- 75.Murphy DA, Roberts KJ, Herbeck DM. HIV-positive mothers with late adolescent/early adult children:“Empty nest” concerns. Health Care Women Int. 2012;33(4):387–402. doi: 10.1080/07399332.2012.655395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Emlet CA, Tozay S, Raveis VH. “I’m not going to die from the AIDS”: Resilience in aging with HIV disease. Gerontologist. 2011;51(1):101–111. doi: 10.1093/geront/gnq060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Paniagua FA, O’Boyle M. Comprehensively assessing cognitive and behavioral risks for HIV infection among middle-aged and older adults. Educational Gerontology. 2008;34(4):267–281. [Google Scholar]