Abstract
Efficacy of intraocular lens power calculation formulas in a subset of Indian myopic population. Retrospectively reviewed 43 patients who underwent phacoemulsification with high axial length (AL) (>24.5 mm, range 24.75-32.35 mm). The power of the implanted intraocular lens (IOL) was used to calculate the predicted post-operative refractive error by four formulas: Sanders-Retzlaff-Kraff (SRK II), SRK/T, Holladay 1, and Hoffer Q. The predictive accuracy of the formulas was analyzed by comparing the difference between the “actual” and “predicted” postoperative refractive errors. Repeated measures analysis of variance (ANOVA) tests were done to have pair-wise comparisons between the formulas and P < 0.05 was considered significant. A subcategory of axial length 24.5-26.5 mm was also tested. Holladay 1, Hoffer Q and SRK/T formulas showed a slight tendency toward resultant hyperopia, with mean error of +0.24 diopters (D), +0.58 D, and +0.92 D, respectively. The Holladay 1 formula provided the best predictive result overall.
Keywords: High myopia, intraocular lens power calculation, long axial length
This is an era where refinement of cataract surgery in terms of various techniques is occurring at a fast pace. Cataract surgery being a single stage procedure, one needs to be cautious while determining intraocular lens (IOL) power in patients with high myopia to avoid refractive surprises. Prevalence of myopia as shown in Andhra Pradesh Eye Disease Study is much higher in adult Indian population than similarly aged white population (34.6% vs 17.5%) but there is no study which has been done to check for the efficacy of different IOL power calculation formulas in Indian myopic population.[1] Choice of IOL power in such patients is based on references from Western, Chinese and Japanese population and the optimal formula for the Indian myopic population is inconclusive.
Aim
To determine the accuracy of the Holladay 1, Hoffer Q, Sanders-Retzlaff-Kraff (SRK)/T, and SRK II IOL power calculation formulas in patients with high myopia in a subset of Indian population.
Materials and Methods
Design: Retrospective study
This study was conducted at Sadguru Netra Chikitsalaya, Chitrakoot, Madhya Pradesh, India.
Inclusion criteria
All consecutive patients attending our out patient department (OPD) for phacoemusification with axial length (AL) more than 24.5 mm (range 24.75-32.35 mm) between May 2009-October 2009 (In all patients hydrophilic acrylic foldable within the bag IOL was implanted).
Exclusion criteria
Pre-existing astigmatism >3.0 diopters (D)
Corneal scar
Keratoconus
Complications significantly affecting the refractive status (vitreous loss with IOL implanted in sulcus or anterior chamber, high wound induced astigmatism).
In our study, keratometry measurements were retrieved from records and A scan applanation ultrasonography was done on Echorule2 and analyzed. The implanted IOL power was used to calculate the predicted postoperative refractive error by four commercially available IOL formulas: SRK II, SRK-T, Holladay 1, and Hoffer Q. With each formula, the mean error (ME) was calculated from the difference between the formula predicted refractive error and actual postoperative refractive error. The spherical equivalent was measured by a single trained optometrist using an autorefractor and subjective retinoscopy 1-2 months after cataract surgery. The smallest ME indicated the formula with the best predictive accuracy. Repeated measures ANOVA tests were done after making bonferroni corrections to have pair-wise comparisons between the formulas and P < 0.05 was considered as significant. Subcategoryof long AL (24.5-26.5 mm) was also tested. All surgeries were done by three experienced surgeons.
Results
Forty three eyes of 43 patients with axial length more than 24.5 mm in our set-up were retrospectively studied. The keratometry in most of the patients (81%) was within the normal range of 42.0-46.0 D.
Overall performance of all the formulas in AL more than 24.5 mm showed a tendency to cause a hyperopic refractive error post-operatively [Table 1].
Table 1.
Overall performance of formulas in eye with AL>24.5 mm
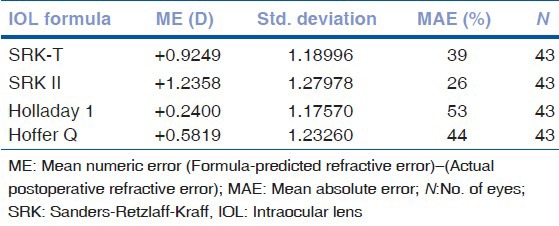
Holladay 1 caused the smallest ME, +0.24 D. Fifty three percent of patients had mean absolute error less than 1.00 D. The Hoffer Q and SRK-T caused a little larger hyperopic shift with MEs of +0.58D and +0.92 D. SRK II caused the largest hyperopic error +1.23 D. [Table 1].
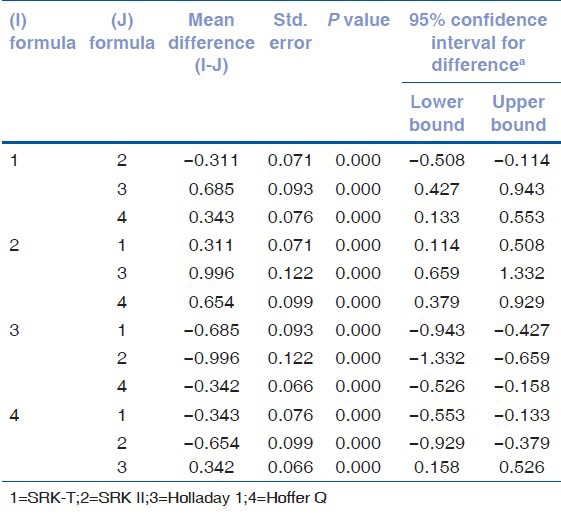
Pair-wise comparisons between different formulas shows that P value between different formulas is significant (P < 0.05) implicating that Holladay 1 with least ME is significantly different from other formulas and have better performance in patients with AL more than 24.5 mm when compared to SRK-T, SRK II, Hoffer Q [Table 2].
Table 2.
Pair-wise comparisons measure: ME (mean error)
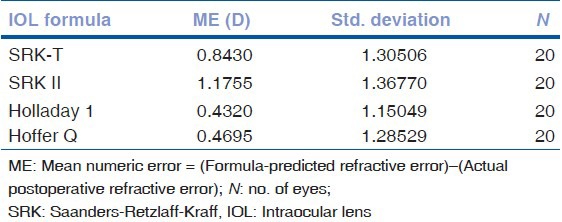
The performance of each formula in AL subcategory in eyes with AL between 24.5-26.5 mm also found Holladay 1 as the best formula [Table 3].
Table 3.
Performance of formulas in eye with axial length 24.5-26.5 mm
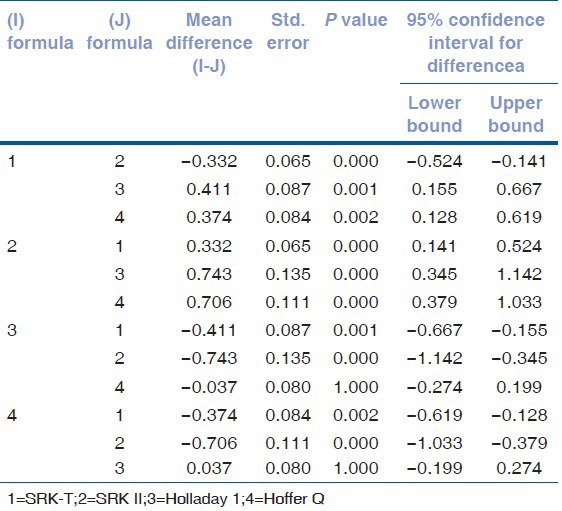
Pair-wise comparisons between different formulas in a subset of patients with a AL 24.5-26.5 mm shows that Holladay 1 (ME = +0.4320 D) and Hoffer Q (ME = +0.4695 D) are comparable, P value not being significant [Table 4].
Table 4.
Pair-wise comparisons measure: ME (mean error)
Discussion
Our preliminary results showed that in our patients with axial myopia with ALs longer than 24.50 mm, the Holladay 1 provided the best predictive result and the Hoffer Q was comparable to Holladay 1 for AL 24.5-26.5 mm for IOL power calculation. The SRK II was the least accurate. This agrees with the results in several studies in which better performances were found in cases with long eyes with the Holladay 1 formula than the SRK II formula. Olsen and co-authors reported that the Holladay formula is more accurate than the SRK II.[2] In a study conducted by Stopyra, in which a study of patients with AL 24.51-26.72 mm and found Holladay 1 formula was the most accurate with 88.5% of the patients achieving full Visual acuity (1.0 on Snellen) after cataract surgery.[3] Stopyra also found SRK/T formula satisfactory with 63.9% of the patients achieving full visual acuity on Snellen but only 36.1% of the patients achieved full visual acuity using Hoffer Q. Kijima et al., report the best results using the Holladay and SRK/T in the midrange AL (24.5-26.9 mm) group and the SRK/T or L-SRK in the long AL (longer than 27.0 mm) group.[4] Tsang CS and co-authors also reported best results in patients with AL 25.0 mm using Hoffer Q and Holladay 1 and SRK-T were comparable with SRK II being least accurate and in patients with AL > 28.0 mm they found Holladay 1 and SRK/T more accurate than Hoffer Q.[5] Narvaez and co-authors also reported better performance of these formulas when compared with SRK-II.[6] In studies by Bang and co-authors on AL > 27.0 mm and Wang and co-authors on AL >25.0 mm using IOL Master reported that Haigis formula is the best.[7,8] Ghanem and El-Sayed reported that in patients with high axial myopia, the performance of SRK-T, Hoffer-Q, Holladay-2, and Haigis formulas are comparable in low plus – powered IOL implantation and Haigis formula is the best formula when minus power IOL is implanted.[9] However, we did not find performance of SRK-T formula better in Indian myopic population. Our recommendation is to avoid using the SRK II and SRK/T formula for IOL power calculation in eyes with axial myopia in Indian population with AL longer than 24.50 mm. In our study, all four formulas had a tendency to cause a postoperative hyperopic refraction. This finding has been reported earlier.[5] Our study had some limitations: (a) It was a single center retrospective study and (b) Surgeons, and time of the postoperative refraction were not standardized. To conclude, the results of our study provide useful information to aid the choice of IOL power in patients with high axial myopia in Indian population during our daily practice with Holladay 1 being the most accurate and SRK II and SRK/T to be avoided.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Krishnaiah S, Srinivas M, Khanna RC, Rao GN. Prevalence and risk factors for refractive errors in the South Indian adult population: The Andhra Pradesh Eye disease study. Clin Ophthalmol. 2009;3:17–27. [PMC free article] [PubMed] [Google Scholar]
- 2.Olsen T, Thim K, Corydon L. Accuracy of the newer generation intraocular lens power calculation formulae in long and short eyes. J Cataract Refract Surg. 1991;17:187–93. doi: 10.1016/s0886-3350(13)80249-0. [DOI] [PubMed] [Google Scholar]
- 3.Stopyra W. The accuracy of IOL power calculation formulas for eyes of axial length exceeding 24.5 mm. Klin Oczna. 2013;115:93–5. [PubMed] [Google Scholar]
- 4.Kijima T, Kozawa T, Kora Y, Yaguchi S, Inatomi M, Koide R, et al. Accuracy of intraocular lens power calculation formulas. Nihon Ganka Gakkai Zasshi. 1999;103:470–6. [PubMed] [Google Scholar]
- 5.Tsang CS, Chong GS, Yiu EP, Ho CK. Intraocular lens power calculation formulas in Chinese eyes with high axial myopia. J Cataract Refract Surg. 2003;29:1358–64. doi: 10.1016/s0886-3350(02)01976-4. [DOI] [PubMed] [Google Scholar]
- 6.Narváez J, Zimmerman G, Stulting RD, Chang DH. Accuracy of intraocular lens power prediction using the Hoffer Q, Holladay 1, Holladay 2, and SRK/T formulas. J Cataract Refract Surg. 2006;32:2050–3. doi: 10.1016/j.jcrs.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Bang S, Edell E, Yu Q, Pratzer K, Stark W. Accuracy of intraocular lens calculations using the IOL Master in eyes with long axial length and a comparison of various formulas. Ophthalmology. 2011;118:503–6. doi: 10.1016/j.ophtha.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Wang JK, Hu CY, Chang SW. Intraocular lens power calculation using the IOLMaster and various formulas in eyes with long axial length. J Cataract Refract Surg. 2008;34:262–7. doi: 10.1016/j.jcrs.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Ghanem AA, El-Sayed HM. Accuracy of intraocular lens power calculation in high myopia. Oman J Ophthalmol. 2010;3:126–30. doi: 10.4103/0974-620X.71888. [DOI] [PMC free article] [PubMed] [Google Scholar]


