Abstract
Traumatic brain injury (TBI) consists of varied pathophysiological consequences and alteration of intracranial dynamics, reduction of the cerebral blood flow and oxygenation. In the past decade more emphasis has been directed towards optimizing cerebral perfusion pressure (CPP) in patients who have suffered TBI. Injured brain may show signs of ischemia if CPP remains below 50 mmHg and raising the CPP above 60 mmHg may avoid cerebral oxygen desaturation. Though CPP above 70 mmHg is influential in achieving an improved patient outcome, maintenance of CPP higher than 70 mmHg was associated with greater risk of acute respiratory distress syndrome (ARDS). The target CPP has been laid within 50-70 mmHg. Cerebral blood flow and metabolism are heterogeneous after TBI and with regional temporal differences in the requirement for CPP. Brain monitoring techniques such as jugular venous oximetry, monitoring of brain tissue oxygen tension (PbrO2), and cerebral microdialysis provide complementary and specific information that permits the selection of the optimal CPP. This review highlights the rationale for use CPP directed therapies and neuromonitoring to identify optimal CPP of head injured patients. The article also reviews the evidence provided by various clinical trials regarding optimal CPP and their application in the management of head injured patients.
Keywords: Cerebral perfusion pressure, evidence, management protocols, neuromonitoring, optimal, traumatic brain injury
Introduction
The primary aim of managing patients with acute brain injury is to minimize secondary injury by maintaining cerebral perfusion and oxygenation. The inability of the brain to store metabolic substrates, in the face of high oxygen and glucose requirements, makes it very susceptible to ischemic damage. Cerebral perfusion pressure (CPP) has been used as an index of the input pressure determining cerebral blood flow and therefore perfusion. The question whether the management of patients with TBI should be directed towards CPP or intracranial pressure (ICP) as the target is still a matter of debate. An attempt to optimize the patient care in terms of one parameter may appear defeating in terms of another. Consequently, laying down specific target for patient management in requisites for overall outcome seems difficult. In the past decade, more emphasis has been directed toward CPP in patients who have suffered traumatic brain injury (TBI). This attention has primarily arisen from study data documenting the occurrence of brain ischemia early after injury and intensive care unit (ICU) based study data documenting the occurrence of reduced CPP and jugular venous desaturation due to increased ICP supporting the concept that relative cerebral perfusion is more important than any potential increase in ICP.[1] Given that CPP is a modifiable target of intensive care in the patient with TBI, a great deal of effort has been expended in optimizing CPP. In fact, this emphasis has been codified into the current Brain Trauma Foundation guidelines for severe TBI[2] (www.braintrauma.org). Nonetheless, considerable uncertainty exists about the optimal level of CPP. This article will address the main evidence for a CPP threshold and attempt to define the optimal CPP for patients with TBI based on this evidence.
CPP in normal brain
Understanding the basic physiology of cerebral oxygenation is important for the development of effective strategies in management of head injuries. Cerebral oxygenation involves three main factors, namely the cerebral blood flow (CBF), arterial content of oxygen, and cerebral metabolic rate of oxygen consumption. CPP is the surrogate for CBF measurements and is defined as the mathematical difference between mean arterial pressure (MAP) and the pressure in the small cerebral veins just before they enter the dural sinuses. This represents the pressure gradient driving CBF and thereby, oxygen and metabolite delivery. Normal brain autoregulates its blood flow to provide a constant flow regardless of changes in blood pressure. The regulation of CBF is done by altering the resistance of cerebral blood vessels. Cerebral autoregulation is under the influence of myogenic, metabolic, and neurogenic factors; however, how these factors interact is at present poorly understood. Cerebral blood flow is directly related to CPP and inversely to cerebral vascular resistance (CVR). Because CVR is high when intravascular pressure is high, and CVR is low when intravascular pressure is low; CBF remains constant over the wide range of blood pressures. This constancy of CBF is termed autoregulation of CBF. Though classic description of the, CBF-pressure autoregulation of an autoregulatory plateau or a slightly modified with a sloped plateau is widely accepted, a significant variation in intersubject pattern or shape of the circulatory response to hypotension has been reported. It can vary from the classic pattern usually associated with CBF-pressure autoregulation to hyperregulation or peak on one hand and “none pattern” on the other.[3] The variations in CPP at the lower limit of autoregulation is described as “horizontal variations” and the variations of CBF at the lower limit of autoregulation is described as “vertical variations.”[4] Given that none pattern is a natural variation in the physiology of cerebral autoregulation, the arbitrary lower limit of autoregulation, a MAP of 50 mmHg, may have serious consequences. The “none pattern”, characterized as vasomotor paralysis with loss of autoregulation, can occur as a result of brain damage in conditions such as severe trauma, excessive increases in ICP, subarachnoid hemorrhage, and cerebral ischemia. It is safest to assume that an individual patient has limited autoregulatory capacity to maintain tight control cerebral perfusion.[4]
Alterations of CPP in injured Brain
The homeostatic mechanisms are often lost after head trauma (CVR is usually increased), and the brain becomes susceptible to blood pressure changes.[5] Other factors that may impair autoregulation include hypoxemia, hypercapnia, and large dose volatile anesthetic. CBF normally decreases in response to hyperventilation. This carbon dioxide reactivity is usually, but not always, preserved following head injury. Cerebral ischemia would be further aggravated by the presence of systemic hypotension.
In the absence of intracranial pathology, ICP is low, usually 5 mmHg or less, and CPP changes reflect alterations in MAP. Either a decrease in MAP or an elevation in ICP will deleteriously alter the effective perfusion pressure, the CPP. When elevated profoundly, ICP alters perfusion of cortical and subcortical structures. Historically, maintenance of a CPP greater than 50 mmHg was considered acceptable in head injury patients. However, following trauma, if autoregulation is preserved it is shifted to the right, therefore a higher CPP is needed to maintain adequate CBF. Increasing CPP also minimizes ICP by reducing intracranial blood volume and cerebral edema via autoregulatory vasoconstriction. Rosner, et al., recommended maintaining CPP greater than 70 mmHg in head injured patients to minimize cerebral ischemia and prevent the cascade of events that result from inadequate perfusion.[6] However, autoregulation is often impaired causing an increase in arterial pressure that leads to an increase in CBF, as well as capillary hydrostatic, increased cerebral edema, and intracranial hypertension; the main tenets of this “Lund” approach.[7] Thus, there is a controversy on the optimal CPP following TBI.
Rationale for use of ICP and CCP directed therapy in TBI
ICP directed therapy
Continuous monitoring of ICP has become the cornerstone in neuromonitoring as it reflects the mass effect that predisposes to cerebral injury and herniation. Though there is substantial evidence that ICP monitoring improves outcome,[8,9] there are no randomized trials confirming the benefit of ICP monitoring and treatment in TBI. Large observation studies[10] and retrospective analysis[11] with severe TBI have shown that patients with monitored and controlled ICP had better outcome than those whose ICP was not controlled. They support an ICP of 20 mmHg as the upper threshold beyond which treatment should generally be initiated.[12] But some studies have indicated that despite extremely high ICP, intense, aggressive management of CPP can lead to good neurological outcomes.[1] Moreover, treatment of ICP has adverse effects, and there are several questions about ICP management that have yet to be definitively answered. The risk of infection increases significantly after 3 days of monitoring.[13] In the case of continuous cerebrospinal fluid (CSF) drainage, continuous intraventricular measurement of ICP may become unreliable.[14]
CPP directed therapy
The clinical use of CPP is based on theoretical suggestions that maintaining optimal cerebral blood flow (CBF) is necessary to meet the metabolic needs of the injured brain. The goal is to preserve the ischemic penumbra and avoid exacerbation of secondary insults, such as excitotoxicity, free radical production, and inflammation. Higher CPP may contribute to various complications and low CPP has concerns of their own. The issue now is to balance CPP and the question of optimal CPP needs to be addressed.
The “Lund therapy” is a therapeutic approach that focuses on the reduction of ICP by decreasing intracranial volumes.[15] This theory contends that by reducing CPP, there is a reduced risk of promoting vasogenic edema and, therefore, less risk of elevating ICP. However, low CPP causes reduction in cerebral blood flow and predisposes the injured brain to cerebral ischemia and infarction. Within the range of autoregulation, low CPP is associated with increased ICP through compensatory vasodilation in response to decreased perfusion pressure.[16,17] Studies associated with use of microdialysis, jugular venous oximetry, and brain tissue oxygen saturation (PbO2) have found that injured brain that may show signs of ischemia if CPP remains below 50 mmHg and raising CPP above 60 mmHg may avoid cerebral oxygen desaturation.[18,19,20] These studies suggest that the critical threshold for CPP lies between 50 and 60 mmHg and CPP of less than 50 mmHg be avoided.[21] Rosner and Daughton have shown that a CPP above 70 mmHg is influential in achieving an improved patient outcome.[22] Therefore the concept of prophylactically elevating CPP to avoid brain ischemia and to maintain an ideal CBF has gained support. Subsequently, the randomized controlled trials demonstrated that maintenance of CPP higher than 70 mmHg was associated with five times greater risk of acute respiratory distress syndrome (ARDS).[23] Moreover CPP values higher than 70 mmHg did not offer any outcome benefits.[24] Accordingly, CPP above 70 mmHg has been recommended to be avoided. The CPP to target has been laid within 50-70 mmHg. The cerebral injury following trauma is heterogeneous and therefore the optimal CPP at which cerebral oxygenation is best maintained needs to be identified.
Optimal threshold for CPP following TBI
The individual parameters of CPP (blood pressure and ICP) have been shown to be critically related to outcome from TBI. Systemic hypotension is highly associated with poor outcome.[25,26] As well, elevated ICP predicts increased mortality and less recovery.[25] However, the critical CPP threshold is still debatable.
Role of neuromonitoring to determine optimum CPP
The response of brain to injury is heterogenous. Considerable uncertainty exists about the optimal level of CPP required to restore the cerebral oxygenation. The role of neuromonitoring in determining the optimal CPP for patients with TBI is investigated.
Invasive cerebral monitoring
ICP monitoring
Measurement of ICP is the mainstay of both ICP and CPP directed therapy of TBI. It allows measurement of absolute ICP, calculation of CPP, and identification of optimal CPP.[27] While various methods are available for the measurement of ICP, the “gold standard” is the intraventricular catheter placed in the lateral ventricle. However, placement may be difficult in cases of severe brain swelling and there is also a risk of ventriculitis and hemorrhage.[13] Transducer tipped systems can also be placed in the brain parenchyma or subdural space through a skull bolt or during surgery, with minimal infection and complications. Inaccuracies can occur due to presence of transtentorial and interhemispheric pressure gradients after head injury[28] and zero drifts.
Although it is slowly becoming integral in the management of TBI in most centers, there still exists no Class I evidence supporting its efficacy and its use is still not universal.[29] A host of studies lend support to the fact that ICP monitoring can act as an early warning system that allows appropriate therapy to be instituted.[9,10] However, a few including a recent randomized controlled trials with severe TBI has shown that maintaining monitored ICP at 20 mmHg or less was not superior to care based on imaging and clinical examination.[30,31]
Continuous monitoring ICP also enables online calculation of secondary indices and intervention before the onset of intracranial hypertension. Analysis of pathological waveforms[32,33,34] cerebrovascular reactivity,[35,36,37,38] pressure-volume compensatory reserve using indices like pressure volume index (PVI),[39] correlation coefficient (R) between the amplitude of the fundamental component (A) and mean pressure (P) (RAP),[40,41] and compliance by volume-pressure response (VPR)[42,43] can be calculated. Another ICP-derived index is the cerebrovascular pressure reactivity (PRx), which assesses cerebrovascular reactions by observing the response of ICP to slow spontaneous changes in arterial blood pressure (ABP) by calculating the correlation coefficient between time-averaged data points of ICP and ABP. A positive PRx is associated with passive behavior of a nonreactive vascular bed. A negative value of PRx reflects a normally reactive vascular bed. Changes in PRx guide the treatment of patients. The PRx plotted against CPP shows a U-shaped curve. This indicates that in the majority of patients there is a value of the CPP at which pressure reactivity is optimal. This optimal perfusion pressure can be estimated by plotting and analyzing the PRx-CPP curve in a sequential time-moving window. This potentially useful method is used in an attempt to refine CPP-oriented therapy.[38] The PRx may be useful for defining age-specific and possibly patient-specific optimal targets for CPP after TBI.[36]
Jugular venous oximetry (SjVO2)
Continuous monitoring of SjVO2 performed though the fibreoptic catheter placed in the dominant internal jugular bulb can be used to estimate the balance between global cerebral oxygen delivery and utilization.[44,45] Under conditions of stable cerebral metabolism, changes in SjVO2 reflect changes in CBF.[46] SjVO2 has a prognostic value after neurotrauma and a fall in SjVO2 to below 55% is associated with a poor outcome.[47] CPP level below 60 mmHg was associated with abnormal arteriovenous lactate difference (AVDL) and SjO2.[48] SjVO2 helps to determine the optimal CPP required for the maintenance of cerebral oxygenation. There are several limitations of being a global measure with limited sensitivity to regional changes.[49] SjVO2 does not decrease by <50% until more than 13% of the brain becomes ischemic.[50]
Brain tissue oxygen tension
Continuous measurement of brain oxygen tension can be measured by an invasive probe with sensor using polarographic Clarke type electrode[51] or fibreoptic technology.[52] Normal PbrO2 is in the range of 35-50 mmHg.[53] Ischemic thresholds of between 5 and 20 mm Hg have been suggested.[54,55,56] Reduced PbrO2 has been associated with a poor outcome after neurotrauma.[57]
Optimal CPP can individualized by monitoring the levels of brain oxygenation. A number of studies have examined the relationship between CPP and cerebral oxygenation. After TBI, PbrO2 increases with CPP and the ceiling of this effect is higher in the areas of focal ischemia The increase in PbrO2 relative to an increase in arterial PO2 is termed brain tissue oxygen reactivity. It is believed that this reactivity is controlled by an oxygen regulatory mechanism (CBF autoregulation), and that this mechanism may be disturbed after brain injury. Soehle and colleagues introduced the concept of ‘autoregulation’, defined as the ability of the brain to maintain PbrO2 despite changes in CPP,[58] thereby identifying appropriate individual CPP targets. Following these findings, manipulation of PbrO2 by altering PO2 (by increases) or altering the CPP (by MAP increases, ICP decreases, or both) have been investigated with the view to therapy optimization and potential prognostication.[58,59] While some studies showed a relationship between CPP and cerebral metabolic rate of oxygen (CMRO2), Sahuquillo, et al., could not demonstrate a direct relationship between CPP and PbrO2.[60] The PbrO2 readings varied with both normal and supernormal CPP. Stiefel, et al., demonstrated that although PbO2 directed therapy led to improved outcomes, CPP was similar between the groups.[61] CPP and ICP are not surrogates for PbrO2. Evidence that guided therapy using brain tissue oxygenation in addition to ICP and CPP monitoring leads to better outcomes after TBI is also increasing.[62,63,64,65,66,67]
Cerebral microdialysis
Cerebral microdialysis catheter placement in the vulnerable area after TBI provides on line analysis biochemical changes such as glucose, lactate, pyruvate, glycerol, glutamate, and pH. The use of cerebral microdialysis in TBI can predict poor outcome, assist in clinical decision-making and management of CPP.[20] An increase in the lactate-pyruvate ratio above established thresholds is associated with poor outcome in neurotrauma.[68,69] Biochemical changes of microdialysis occur before low CPP is detectable.[70] Nordstrom demonstrated that lactate in the injured brain increased both when CPP was less than 50 mmHg as well as more than 70 mmHg.[20] Stahl, et al., showed that reducing CPP led to normalization of microdialysis constituents only if CPP was more than 50 mmHg and significant ischemia developed below this threshold.[71] Although increased CPP with vasopressors improved CBF and oxygenation it failed to demonstrate any significant change in microdialysis indices.[63,72] There is no clear consensus on relation between CPP and microdialysis.
Noninvasive cerebral monitoring
Transcranial doppler (TCD)
Currently a lot of work is being done to investigate the application of TCD as a noninvasive estimation of ICP or CPP.[73] Use of the dimensionless TCD-pulsatility index (PI) permit the early identification of patients with low CPP and high risk of cerebral ischemia.[74] Although this work is in its early stages, there has been limited success in correlating CPP derived from TCD with invasive CPP measurement.
It has also been used to test autoregulatory reserve by monitoring changes in CBF velocity in response to changes in MAP.[75] By continuous recording of the flow velocity in the middle cerebral artery (FVmca), the autoregulatory ‘threshold’ or ‘break point’ (the CPP at which autoregulation fails) can be easily detected, providing a target CPP value for treatment.[73,76] A decline in autoregulation is associated with poor outcomes.[77] Critical closing pressure (CCP) is calculated from pressure-flow velocity plots from TCD and by linear extrapolation to zero flow. The driving pressure gradient for cerebral perfusion is the difference between MAP and CCP (CCP = zero flow pressure). Therefore, determination of the difference between MAP and CCP should provide an appropriate monitoring of the effective CPP (eff).[78]
Near infrared spectroscopy
Cerebral oximetry records regional saturation of the brain using near infrared spectroscopy (NIRS) and provides a noninvasive method to continuously monitor brain oxygen imbalance. Tentative ischemic thresholds have been described, but clinical data on application of NIRS after TBI is still limited.[79] In patients with neuronal injury, the knowledge of the status of cerebrovascular autoregulation can help to optimize the management of the CPP. NIRS shows promise for the continuous assessment of cerebrovascular reactivity[80] and cerebral autoregulation in adults.[81] NIRS-based index of cerebrovascular reactivity, called total hemoglobin reactivity (THx) was found to have significant correlation with standard measurements of PRx which requires invasive ICP monitoring. There was a significant agreement with the optimal CPP and ABP assessed with THx and PRx. THx may be of diagnostic value to optimize therapy oriented toward restoration and continuity of cerebrovascular reactivity, especially in patients for who direct ICP monitoring is not feasible.[80] The clinical significance of this new information will need further validation studies.
Evidence for CPP management in TBI
The evidence for CPP in the management of TBI is varied, some supporting increase in CPP and against the rising CPP. The studies have used physiological variables and clinical variables to define the end point. Much of the definition of the former can come from simple physiologic monitoring; the latter requires clinical evidence from controlled trials using outcome as their dependent variable.
Evidence supporting increasing CPP
Physiological indices
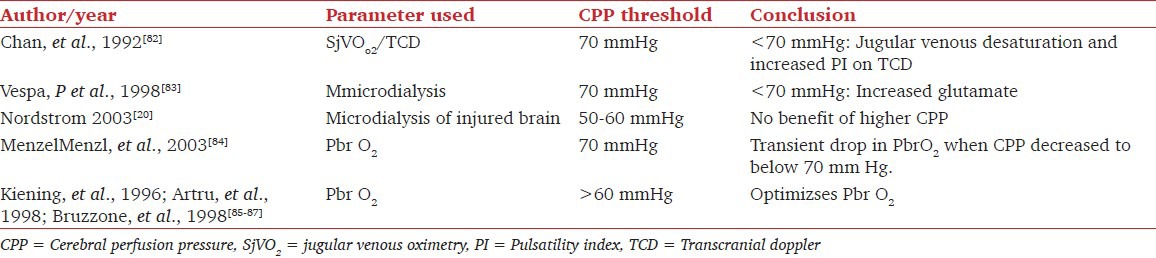
When physiological indices are used as dependent variables, there is evidence that low CPP is associated with unfavorable physiological values. Various physiological monitoring parameters have been used to define the optimal CPP [Table 1]. It is important to differentiate physiologic thresholds representing potential injury from clinical thresholds to treat.
Table 1.
Evidence for a critical CPP threshold from physiological indices
Evidence from clinical indices
When CPP per se is evaluated in terms of human clinical outcome, low CPP is frequently found to correlate with poor outcome. Several retrospective and prospective studies have demonstrated clinical benefit of monitoring and maintenance of CPP. But the threshold CPP varies among the studies [Table 2]. Some of these studies, however, were retrospective data analyses without risk adjustment for other parameters.
Table 2.
Evidence for critical CPP threshold from clinical indices
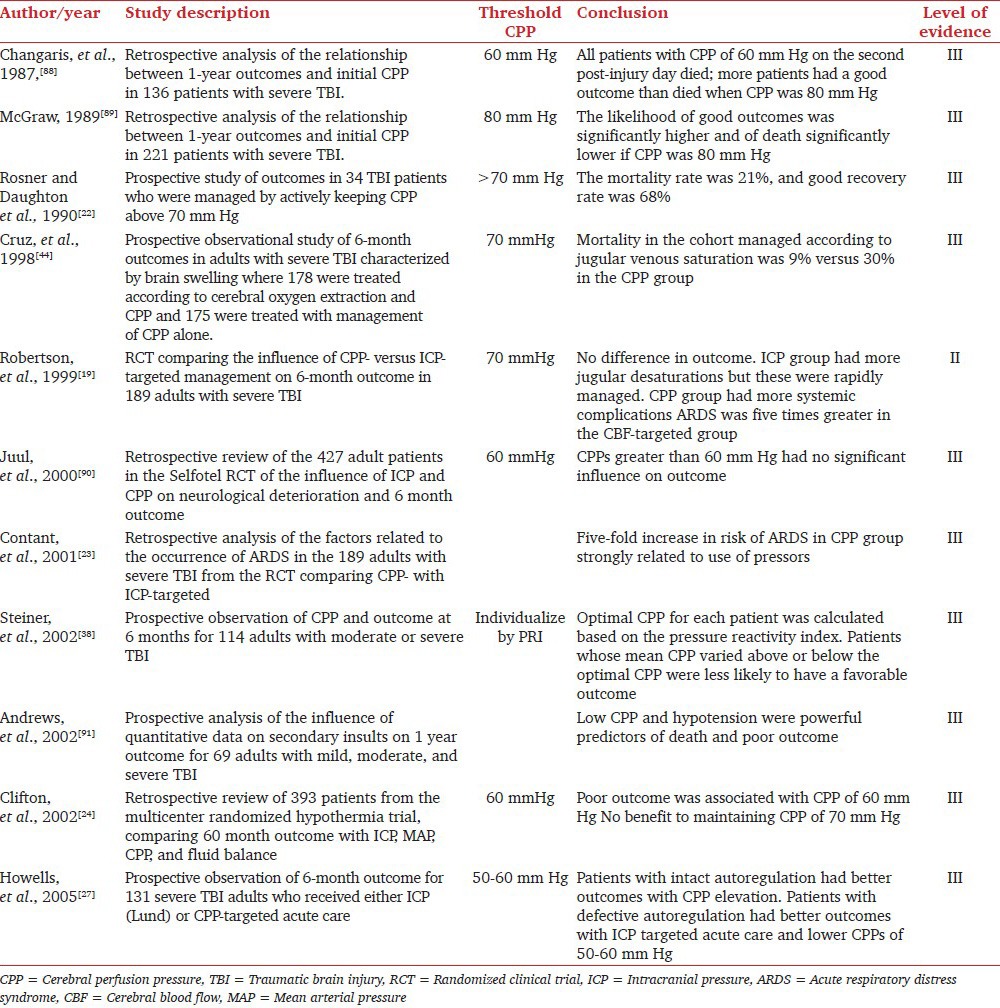
There is no single optimal CPP following TBI. Moreover, there are no Class 1 study data that indicate an optimal CPP threshold. The aforementioned evidence points to different thresholds of CPP above which physiological markers of injury are decreased, but no single study has involved a clear test of any single CPP threshold in a randomized controlled manner. These studies support CPP as a valuable monitoring parameter in managing patients with severe TBI. It appears that the critical threshold for ischemia generally lies in the realm of 50-60 mmHg and can be further delineated in individual patients by ancillary monitoring.
Evidence against increasing CPP
Early proponents of CPP management reported improved outcomes for severe TBI patients whose CPPs were higher during their treatment course. Subsequent reports call into question whether there is any marginal gain by maintaining the CPP at an elevated level. There is a growing body of clinical evidence that elevating the CPP above the threshold for ischemia may not be beneficial and may indeed have detrimental cerebral and systemic effects. [Table 3]
Table 3.
Evidence against increasing CPP
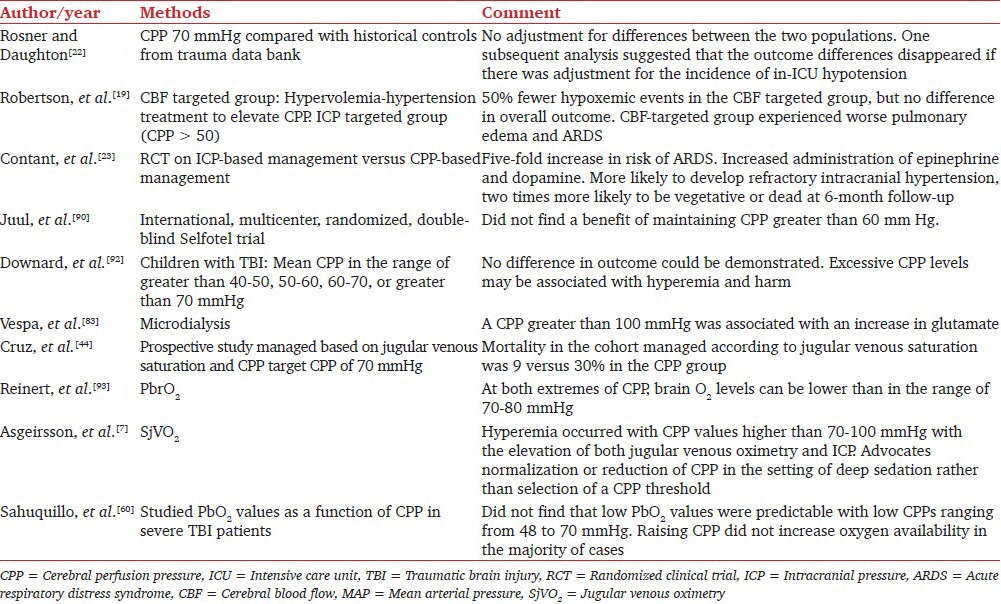
At this time, it is not possible to posit an optimal level of CPP to target to improve outcome in terms of avoiding clinical episodes of ischemia and minimizing the cerebral vascular contributions to ICP instability. It is becoming increasingly apparent that elevating the CPP via pressors and volume expansion is associated with serious systemic toxicity, may be incongruent with frequently encountered intracranial conditions, and is not clearly associated with any benefit in terms of general outcome. Based on a purely pragmatic analysis of the randomized, controlled trial; Clifton, et al., noted that a CPP target threshold should be set approximately 10 mm Hg above what is determined to be a critical threshold in order to avoid dips below the critical.[24]
Age based thresholds in pediatric patients
The CBF, CMRO2, and cerebral blood volume (CBV) are thought to be affected in the same manner in children as in adult brain by physiologic and pharmacologic maneuvers. The CPP increases with age, starting from 25 mmHg in neonates and increasing to 80-90 mmHg in adults. Current guidelines for ICP and CPP thresholds suggest that age-based thresholds should be adopted, but few studies have included the youngest children affected by TBI (those <2 years of age). A retrospective analysis of pediatric TBI concluded that initial CPPs between 40 and 70 mmHg were found to have a better neurological prognosis than those with CPPs either higher or lower than that range.[94] A recent retrospective analysis has shown that despite good ICP control in pediatrics, there was still a 50% incidence of unfavorable outcome, suggesting that there may be unique physiologic parameters that need to be targeted in infants with severe TBI. Data from 22 children (of whom 81% had suffered from inflicted childhood neurotrauma) were analyzed in the first 7 days. Children with unfavorable outcome had more hourly readings of CPP of <45 mmHg compared to children with favorable outcome. There was no difference between the number of hourly readings of ICP of >20 mmHg between the outcome groups. This study suggests a CPP target threshold of 45 mmHg.[95] Monitoring of tissue oxygen, PRx, and autoregulation were found to be useful in determining optimal CPP in pediatric TBI also.[36,96,97] A prospective study is needed to fully determine what goals should be targeted for this vulnerable population.
Selection of the optimal CPP following TBI
Steiner, et al., used an on-line method of measuring cerebral pressure autoregulation and estimated the CPP at which autoregulation appeared most robust in 60% of their patient group.[38] The more closely the mean CPP at which individual patients were maintained approximated the CPP at which their autoregulation was optimal, the more likely that patient was to have a favorable outcome. The use of SjVO2 in conjunction with measuring CPP may provide a method of selecting the optimal CPP for an individual patient. Based on continuous SjvO2 values, a CPP level can be selected that provides adequate O2 delivery and CBF. In many cases, especially under conditions of deep sedation, a CPP greater than 70 mmHg will provide O2 delivery and CBF in excess of O2 demand[7] and may promote hyperemia and therefore raised ICP. Similarly, using other brain monitoring devices,[71,98,99,100] such as PbrO2 probes and microdialysis probes, optimization of CPP to lower or higher levels may be possible. Nonetheless, the more studies are required to determine how best to integrate additional brain monitors in the decision process about the optimization of CPP. Based on the currently available evidence Brain Trauma Foundation has made the following recommendations for threshold CPP[21] (www.braintrauma.org).
Recommendations of brain trauma foundation
Level I: There are insufficient data to support a Level I recommendation for this topic.
Level II: Aggressive attempts to maintain CPP above 70 mmHg with fluids and pressors should be avoided because of the risk of adult respiratory distress syndrome (ARDS).
Level III: CPP of 50 mmHg should be avoided. The CPP value to target lies within the range of 50-70 mmHg. Patients with intact pressure autoregulation tolerate higher CPP values. Ancillary monitoring of cerebral parameters that include blood flow, oxygenation, or metabolism facilitates CPP management.
Conclusions
The selection of an optimal CPP following TBI is possible in theory, but in practice many uncertainties remain. Cerebral blood flow and metabolism are heterogeneous after TBI both in space (regional differences) and time (temporal profile). Thus, different regions of the brain may require different levels of CPP and different levels of CPP may be needed at different time points after injury. Although optimal CPP is essentially an imaginary number, brain monitoring techniques such as jugular venous oximetry, monitoring of PbrO2, and cerebral microdialysis provide complementary and specific information that permits the selection of the best CPP for an individual patient over time.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Young JS, Blow O, Turrentine F, Claridge JA. Schulman A: Is there an upper limit of intracranial pressure in patients with severe head injury if cerebral perfusion pressure is maintained? Neurosurg Focus. 2003;15:E2. doi: 10.3171/foc.2003.15.6.2. [DOI] [PubMed] [Google Scholar]
- 2.Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. XV. Steroids. 2007;24(Suppl 1):S91–5. doi: 10.1089/neu.2007.9981. [DOI] [PubMed] [Google Scholar]
- 3.Jones SC, Radinsky CR, Furlan AJ, et al. Variability in the magnitude of the cerebral blood flow response and the shape of the cerebral blood flow-pressure autoregulation curve during hypotension in normal rats [corrected] Anesthesiology. 2002;97:488–96. doi: 10.1097/00000542-200208000-00028. [DOI] [PubMed] [Google Scholar]
- 4.Sanders RD, Degos V, Young WL. Cerebral perfusion under pressure: Is the autoregulatory ‘plateau’ a level playing field for all? Anaesthesia. 2011;66:968–72. doi: 10.1111/j.1365-2044.2011.06915.x. [DOI] [PubMed] [Google Scholar]
- 5.Czosnyka M, Smielewski P, Piechnik S, Steiner LA, Pickard JD. Cerebral autoregulation following head injury. J Neurosurg. 2001;95:756–63. doi: 10.3171/jns.2001.95.5.0756. [DOI] [PubMed] [Google Scholar]
- 6.Rosner MJ, Rosner SD, Johnson AH. Cerebral perfusion pressure: Management protocol and clinical results. J Neurosurg. 1995;83:949–62. doi: 10.3171/jns.1995.83.6.0949. [DOI] [PubMed] [Google Scholar]
- 7.Asgeirsson B, Grande PO, Nordstrom CH. A new therapy of post-trauma brain oedema based on haemodynamic principles for brain volume regulation. Intensive Care Med. 1994;20:260–7. doi: 10.1007/BF01708961. [DOI] [PubMed] [Google Scholar]
- 8.Stein SC, Georgoff P, Meghan S, Mirza KL, El Falaky OM. Relationship of aggressive monitoring and treatment to improved outcomes in severe traumatic brain injury. J Neurosurg. 2010;112:1105–12. doi: 10.3171/2009.8.JNS09738. [DOI] [PubMed] [Google Scholar]
- 9.Patel HC, Bouamra O, Woodford M, King AT, Yates DW, Lecky FE. Trends in head injury outcome from 1989 to 2003 and the effect of neurosurgical care: An observational study. Lancet. 2005;366:1538–44. doi: 10.1016/S0140-6736(05)67626-X. [DOI] [PubMed] [Google Scholar]
- 10.Marmarou A, Saad A, Aygok G, Rigsbee M. Contribution of raised ICP and hypotension to CPP reduction in severe brain injury: Correlation to outcome. Acta Neurochir Suppl. 2005;95:277–80. doi: 10.1007/3-211-32318-x_57. [DOI] [PubMed] [Google Scholar]
- 11.Narayan RK, Kishore PR, Becker DP, et al. Intracranial pressure: To monitor or not to monitor? A review of our experience with severe head injury. J Neurosurg. 1982;56:650–9. doi: 10.3171/jns.1982.56.5.0650. [DOI] [PubMed] [Google Scholar]
- 12.Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma. 2007;24(Suppl 1):S55–8. doi: 10.1089/neu.2007.9988. [DOI] [PubMed] [Google Scholar]
- 13.Aucoin PJ, Kotilainen HR, Gantz NM, Davidson R, Kellogg P, Stone B. Intracranial pressure monitors. Epidemiologic study of risk factors and infections. Am J Med. 1986;80:369–76. doi: 10.1016/0002-9343(86)90708-4. [DOI] [PubMed] [Google Scholar]
- 14.Exo J, Kochanek PM, Adelson PD, et al. Intracranial pressure-monitoring systems in children with traumatic brain injury: Combining therapeutic and diagnostic tools. Pediatr Crit Care Med. 2010 doi: 10.1097/PCC.0b013e3181e8b3ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nordstrom CH. Physiological and biochemical principles underlying volume-targeted therapy — the “Lund concept”. Neurocrit Care. 2005;2:83–95. doi: 10.1385/NCC:2:1:083. [DOI] [PubMed] [Google Scholar]
- 16.Bouma GJ, Muizelaar JP. Relationship between cardiac output and cerebral blood flow in patients with intact and with impaired autoregulation. J Neurosurg. 1990;73:368–74. doi: 10.3171/jns.1990.73.3.0368. [DOI] [PubMed] [Google Scholar]
- 17.Bouma GJ, Muizelaar JP, Bandoh K, Marmarou A. Blood pressure and intracranial pressure-volume dynamics in severe head injury: Relationship with cerebral blood flow. J Neurosurg. 1992;77:15–9. doi: 10.3171/jns.1992.77.1.0015. [DOI] [PubMed] [Google Scholar]
- 18.Kiening KL, Hartl R, Unterberg AW, Schneider GH, Bardt T, Lanksch WR. Brain tissue pO2-monitoring in comatose patients: Implications for therapy. Neurol Res. 1997;19:233–40. doi: 10.1080/01616412.1997.11740805. [DOI] [PubMed] [Google Scholar]
- 19.Robertson CS, Valadka AB, Hannay HJ, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999;27:2086–95. doi: 10.1097/00003246-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Nordstrom CH. Assessment of critical thresholds for cerebral perfusion pressure by performing bedside monitoring of cerebral energy metabolism. Neurosurg Focus. 2003;15:E5. doi: 10.3171/foc.2003.15.6.5. [DOI] [PubMed] [Google Scholar]
- 21.Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. IX. Cerebral perfusion thresholds. J Neurotrauma. 2007;24(Suppl 1):S59–64. doi: 10.1089/neu.2007.9987. [DOI] [PubMed] [Google Scholar]
- 22.Rosner MJ, Daughton S. Cerebral perfusion pressure management in head injury. J Trauma. 1990;30:933–40. doi: 10.1097/00005373-199008000-00001. discussion 40-1. [DOI] [PubMed] [Google Scholar]
- 23.Contant CF, Valadka AB, Gopinath SP, Hannay HJ, Robertson CS. Adult respiratory distress syndrome: A complication of induced hypertension after severe head injury. J Neurosurg. 2001;95:560–8. doi: 10.3171/jns.2001.95.4.0560. [DOI] [PubMed] [Google Scholar]
- 24.Clifton GL, Miller ER, Choi SC, Levin HS. Fluid thresholds and outcome from severe brain injury. Crit Care Med. 2002;30:739–45. doi: 10.1097/00003246-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Bullock R, Chesnut RM, Clifton G, et al. Guidelines for the management of severe head injury. Brain Trauma Foundation. Eur J Emerg Med. 1996;3:109–27. doi: 10.1097/00063110-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Pietropaoli JA, Rogers FB, Shackford SR, Wald SL, Schmoker JD, Zhuang J. The deleterious effects of intraoperative hypotension on outcome in patients with severe head injuries. J Trauma. 1992;33:403–7. doi: 10.1097/00005373-199209000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Howells T, Elf K, Jones PA, et al. Pressure reactivity as a guide in the treatment of cerebral perfusion pressure in patients with brain trauma. J Neurosurg. 2005;102:311–7. doi: 10.3171/jns.2005.102.2.0311. [DOI] [PubMed] [Google Scholar]
- 28.Sahuquillo J, Poca MA, Arribas M, Garnacho A, Rubio E. Interhemispheric supratentorial intracranial pressure gradients in head-injured patients: Are they clinically important? J Neurosurg. 1999;90:16–26. doi: 10.3171/jns.1999.90.1.0016. [DOI] [PubMed] [Google Scholar]
- 29.Bulger EM, Nathens AB, Rivara FP, Moore M, MacKenzie EJ, Jurkovich GJ. Management of severe head injury: Institutional variations in care and effect on outcome. Crit Care Med. 2002;30:1870–6. doi: 10.1097/00003246-200208000-00033. [DOI] [PubMed] [Google Scholar]
- 30.Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367:2471–81. doi: 10.1056/NEJMoa1207363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cremer OL, van Dijk GW, van Wensen E, et al. Effect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injury. Crit Care Med. 2005;33:2207–13. doi: 10.1097/01.ccm.0000181300.99078.b5. [DOI] [PubMed] [Google Scholar]
- 32.Carrera E, Kim DJ, Castellani G, et al. What shapes pulse amplitude of intracranial pressure? J Neurotrauma. 2010;27:317–24. doi: 10.1089/neu.2009.0951. [DOI] [PubMed] [Google Scholar]
- 33.Hu X, Xu P, Asgari S, Vespa P, Bergsneider M. Forecasting ICP elevation based on prescient changes of intracranial pressure waveform morphology. IEEE Trans Biomed Eng. 2010;57:1070–8. doi: 10.1109/TBME.2009.2037607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu X, Glenn T, Scalzo F, et al. Intracranial pressure pulse morphological features improved detection of decreased cerebral blood flow. Physiol Meas. 2010;31:679–95. doi: 10.1088/0967-3334/31/5/006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asgari S, Bergsneider M, Hamilton R, Vespa P, Hu X. Consistent Changes in Intracranial Pressure Waveform Morphology Induced by Acute Hypercapnic Cerebral Vasodilatation. Neurocrit Care. 2010 doi: 10.1007/s12028-010-9463-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brady KM, Shaffner DH, Lee JK, et al. Continuous monitoring of cerebrovascular pressure reactivity after traumatic brain injury in children. Pediatrics. 2009;124:e1205–12. doi: 10.1542/peds.2009-0550. [DOI] [PubMed] [Google Scholar]
- 37.Czosnyka M, Brady K, Reinhard M, Smielewski P, Steiner LA. Monitoring of cerebrovascular autoregulation: Facts, myths, and missing links. Neurocrit Care. 2009;10:373–86. doi: 10.1007/s12028-008-9175-7. [DOI] [PubMed] [Google Scholar]
- 38.Steiner LA, Czosnyka M, Piechnik SK, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30:733–8. doi: 10.1097/00003246-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Lavinio A, Rasulo FA, De Peri E, Czosnyka M, Latronico N. The relationship between the intracranial pressure-volume index and cerebral autoregulation. Intensive Care Med. 2009;35:546–9. doi: 10.1007/s00134-008-1311-5. [DOI] [PubMed] [Google Scholar]
- 40.Czosnyka M, Smielewski P, Timofeev I, et al. Intracranial pressure: More than a number. Neurosurg Focus. 2007;22:E10. doi: 10.3171/foc.2007.22.5.11. [DOI] [PubMed] [Google Scholar]
- 41.Zweckberger K, Sakowitz OW, Unterberg AW, Kiening KL. Intracranial pressure-volume relationship. Physiology and pathophysiology. Anaesthesist. 2009;58:392–7. doi: 10.1007/s00101-009-1522-3. [DOI] [PubMed] [Google Scholar]
- 42.Abdullah J, Zamzuri I, Awang S, et al. Preliminary report on spiegelberg pre and post-operative monitoring of severe head-injured patients who received decompressive craniectomy. Acta Neurochir Suppl. 2005;95:311–4. doi: 10.1007/3-211-32318-x_64. [DOI] [PubMed] [Google Scholar]
- 43.Piper I, Dunn L, Contant C, et al. Multi-centre assessment of the Spiegelberg compliance monitor: Preliminary results. Acta Neurochir Suppl. 2000;76:491–4. doi: 10.1007/978-3-7091-6346-7_103. [DOI] [PubMed] [Google Scholar]
- 44.Cruz J. The first decade of continuous monitoring of jugular bulb oxyhemoglobinsaturation: Management strategies and clinical outcome. Crit Care Med. 1998;26:344–51. doi: 10.1097/00003246-199802000-00039. [DOI] [PubMed] [Google Scholar]
- 45.Lam JM, Chan MS, Poon WS. Cerebral venous oxygen saturation monitoring: Is dominant jugular bulb cannulation good enough? Br J Neurosurg. 1996;10:357–64. doi: 10.1080/02688699647276. [DOI] [PubMed] [Google Scholar]
- 46.Robertson CS, Narayan RK, Gokaslan ZL, et al. Cerebral arteriovenous oxygen difference as an estimate of cerebral blood flow in comatose patients. J Neurosurg. 1989;70:222–30. doi: 10.3171/jns.1989.70.2.0222. [DOI] [PubMed] [Google Scholar]
- 47.Murr R, Schurer L. Correlation of jugular venous oxygen saturation to spontaneous fluctuations of cerebral perfusion pressure in patients with severe head injury. Neurol Res. 1995;17:329–33. [PubMed] [Google Scholar]
- 48.Chieregato A, Marchi M, Zoppellari R, et al. Detection of early ischemia in severe head injury by means of arteriovenous lactate differences and jugular bulb oxygen saturation. Relationship with CPP, severity indexes and outcome Preliminary analysis. Acta Neurochir. 2002;81(Suppl):289–93. doi: 10.1007/978-3-7091-6738-0_74. [DOI] [PubMed] [Google Scholar]
- 49.Gupta AK, Zygun DA, Johnston AJ, et al. Extracellular Brain pH and Outcome following Severe Traumatic Brain Injury. J Neurotrauma. 2004;21:678–84. doi: 10.1089/0897715041269722. [DOI] [PubMed] [Google Scholar]
- 50.Coles JP, Fryer TD, Smielewski P, et al. Incidence and mechanisms of cerebral ischemia in early clinical head injury. J Cereb Blood Flow Metab. 2004;24:202–11. doi: 10.1097/01.WCB.0000103022.98348.24. [DOI] [PubMed] [Google Scholar]
- 51.Eriksson EA, Barletta JF, Figueroa BE, et al. Cerebral perfusion pressure and intracranial pressure are not surrogates for brain tissue oxygenation in traumatic brain injury. Clin Neurophysiol. 2012;123:1255–60. doi: 10.1016/j.clinph.2011.08.035. [DOI] [PubMed] [Google Scholar]
- 52.Nortje J, Gupta AK. The role of tissue oxygen monitoring in patients with acute brain injury. Br J Anaesth. 2006;97:95–106. doi: 10.1093/bja/ael137. [DOI] [PubMed] [Google Scholar]
- 53.Hoffman WE, Charbel FT, Edelman G, Hannigan K, Ausman JI. Brain tissue oxygen pressure, carbon dioxide pressure and pH during ischemia. Neurol Res. 1996;18:54–6. doi: 10.1080/01616412.1996.11740378. [DOI] [PubMed] [Google Scholar]
- 54.van Santbrink H, vd Brink WA, Steyerberg EW, Carmona Suazo JA, Avezaat CJ, Maas AI. Brain tissue oxygen response in severe traumatic brain injury. Acta Neurochir (Wien) 2003;145:429–38. doi: 10.1007/s00701-003-0032-3. discussion 38. [DOI] [PubMed] [Google Scholar]
- 55.Vespa P. What is the optimal threshold for cerebral perfusion pressure following traumatic brain injury? Neurosurg Focus. 2003;15:E4. doi: 10.3171/foc.2003.15.6.4. [DOI] [PubMed] [Google Scholar]
- 56.Jodicke A, Hubner F, Boker DK. Monitoring of brain tissue oxygenation during aneurysm surgery: Prediction of procedure-related ischemic events. J Neurosurg. 2003;98:515–23. doi: 10.3171/jns.2003.98.3.0515. [DOI] [PubMed] [Google Scholar]
- 57.Rangel-Castilla L, Lara LR, Gopinath S, Swank PR, Valadka A, Robertson C. Cerebral hemodynamic effects of acute hyperoxia and hyperventilation after severe traumatic brain injury. J Neurotrauma. 2010;27:1853–63. doi: 10.1089/neu.2010.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Soehle M, Jaeger M, Meixensberger J. Online assessment of brain tissue oxygen autoregulation in traumatic brain injury and subarachnoid hemorrhage. Neurol Res. 2003;25:411–7. doi: 10.1179/016164103101201580. [DOI] [PubMed] [Google Scholar]
- 59.Manwaring ML, Durham CA, McNally MM, Agle SC, Parker FM, Stoner MC. Correlation of cerebral oximetry with internal carotid artery stump pressures in carotid endarterectomy. Vasc Endovascular Surg. 2010;44:252–6. doi: 10.1177/1538574410361785. [DOI] [PubMed] [Google Scholar]
- 60.Sahuquillo J, Amoros S, Santos A, et al. Does an increase in cerebral perfusion pressure always mean a better oxygenated brain? A study in head-injured patients. Acta Neurochir Suppl. 2000;76:457–62. doi: 10.1007/978-3-7091-6346-7_95. [DOI] [PubMed] [Google Scholar]
- 61.Stiefel MF, Spiotta A, Gracias VH, et al. Reduced mortality rate in patients with severe traumatic brain injury treated with brain tissue oxygen monitoring. J Neurosurg. 2005;103:805–11. doi: 10.3171/jns.2005.103.5.0805. [DOI] [PubMed] [Google Scholar]
- 62.Adamides AA, Cooper DJ, Rosenfeldt FL, et al. Focal cerebral oxygenation and neurological outcome with or without brain tissue oxygen-guided therapy in patients with traumatic brain injury. Acta Neurochir (Wien) 2009;151:1399–409. doi: 10.1007/s00701-009-0398-y. [DOI] [PubMed] [Google Scholar]
- 63.Spiotta AM, Stiefel MF, Gracias VH, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113:571–80. doi: 10.3171/2010.1.JNS09506. [DOI] [PubMed] [Google Scholar]
- 64.Narotam PK, Burjonrappa SC, Raynor SC, Rao M, Taylon C. Cerebral oxygenation in major pediatric trauma: Its relevance to trauma severity and outcome. J Pediatr Surg. 2006;41:505–13. doi: 10.1016/j.jpedsurg.2005.11.069. [DOI] [PubMed] [Google Scholar]
- 65.Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: Outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg. 2009;111:672–82. doi: 10.3171/2009.4.JNS081150. [DOI] [PubMed] [Google Scholar]
- 66.Martini RP, Deem S, Yanez ND, et al. Management guided by brain tissue oxygen monitoring and outcome following severe traumatic brain injury. J Neurosurg. 2009;111:644–9. doi: 10.3171/2009.2.JNS08998. [DOI] [PubMed] [Google Scholar]
- 67.Jaeger M, Dengl M, Meixensberger J, Schuhmann MU. Effects of cerebrovascular pressure reactivity-guided optimization of cerebral perfusion pressure on brain tissue oxygenation after traumatic brain injury. Crit Care Med. 2010;38:1343–7. doi: 10.1097/CCM.0b013e3181d45530. [DOI] [PubMed] [Google Scholar]
- 68.Zauner A, Doppenberg EM, Woodward JJ, Choi SC, Young HF, Bullock R. Continuous monitoring of cerebral substrate delivery and clearance: Initial experience in 24 patients with severe acute brain injuries. Neurosurgery. 1997;41:1082–91. doi: 10.1097/00006123-199711000-00011. discussion 91-3. [DOI] [PubMed] [Google Scholar]
- 69.Zauner A, Doppenberg E, Woodward JJ, et al. Multiparametric continuous monitoring of brain metabolism and substrate delivery in neurosurgical patients. Neurol Res. 1997;19:265–73. doi: 10.1080/01616412.1997.11740812. [DOI] [PubMed] [Google Scholar]
- 70.Belli A, Sen J, Petzold A, Russo S, Kitchen N, Smith M. Metabolic failure precedes intracranial pressure rises in traumatic brain injury: A microdialysis study. Acta Neurochir (Wien) 2008;150:461–9. doi: 10.1007/s00701-008-1580-3. discussion 70. [DOI] [PubMed] [Google Scholar]
- 71.Stahl N, Ungerstedt U, Nordstrom CH. Brain energy metabolism during controlled reduction of cerebral perfusion pressure in severe head injuries. Intensive Care Med. 2001;27:1215–23. doi: 10.1007/s001340101004. [DOI] [PubMed] [Google Scholar]
- 72.Johnston AJ, Steiner LA, Chatfield DA, et al. Effect of cerebral perfusion pressure augmentation with dopamine and norepinephrine on global and focal brain oxygenation after traumatic brain injury. Intensive Care Med. 2004;30:791–7. doi: 10.1007/s00134-003-2155-7. [DOI] [PubMed] [Google Scholar]
- 73.Czosnyka M, Smielewski P, Piechnik S, et al. Continuous assessment of cerebral autoregulation — clinical verification of the method in head injured patients. Acta Neurochir Suppl. 2000;76:483–4. doi: 10.1007/978-3-7091-6346-7_101. [DOI] [PubMed] [Google Scholar]
- 74.Voulgaris SG, Partheni M, Kaliora H, Haftouras N, Pessach IS, Polyzoidis KS. Early cerebral monitoring using the transcranial Doppler pulsatility index in patients with severe brain trauma. Med Sci Monit. 2005;11:CR49–52. [PubMed] [Google Scholar]
- 75.Czosnyka M, Smielewski P, Kirkpatrick P, Piechnik S, Laing R, Pickard JD. Continuous monitoring of cerebrovascular pressure-reactivity in head injury. Acta Neurochir Suppl. 1998;71:74–7. doi: 10.1007/978-3-7091-6475-4_23. [DOI] [PubMed] [Google Scholar]
- 76.Jagersberg M, Schaller C, Bostrom J, Schatlo B, Kotowski M, Thees C. Simultaneous bedside assessment of global cerebral blood flow and effective cerebral perfusion pressure in patients with intracranial hypertension. Neurocrit Care. 2010;12:225–33. doi: 10.1007/s12028-009-9300-2. [DOI] [PubMed] [Google Scholar]
- 77.Reinhard M, Neunhoeffer F, Gerds TA, et al. Secondary decline of cerebral autoregulation is associated with worse outcome after intracerebral hemorrhage. Intensive Care Med. 2011;36:264–71. doi: 10.1007/s00134-009-1698-7. [DOI] [PubMed] [Google Scholar]
- 78.Thees C, Scholz M, Schaller MDC, et al. Relationship between intracranial pressure and critical closing pressure in patients with neurotrauma. Anesthesiology. 2002;96:595–9. doi: 10.1097/00000542-200203000-00014. [DOI] [PubMed] [Google Scholar]
- 79.Al-Rawi PG, Kirkpatrick PJ. Tissue oxygen index: Thresholds for cerebral ischemia using near-infrared spectroscopy. Stroke. 2006;37:2720–5. doi: 10.1161/01.STR.0000244807.99073.ae. [DOI] [PubMed] [Google Scholar]
- 80.Zweifel C, Castellani G, Czosnyka M, et al. Noninvasive monitoring of cerebrovascular reactivity with near infrared spectroscopy in head-injured patients. J Neurotrauma. 2010;27:1951–8. doi: 10.1089/neu.2010.1388. [DOI] [PubMed] [Google Scholar]
- 81.Steiner LA, Pfister D, Strebel SP, Radolovich D, Smielewski P, Czosnyka M. Near-infrared spectroscopy can monitor dynamic cerebral autoregulation in adults. Neurocrit Care. 2009;10:122–8. doi: 10.1007/s12028-008-9140-5. [DOI] [PubMed] [Google Scholar]
- 82.Chan KH, Miller JD, Dearden NM, Andrews PJ, Midgley S. The effect of changes in cerebral perfusion pressure upon middle cerebral artery blood flow velocity and jugular bulb venous oxygen saturation after severe brain injury. J Neurosurg. 1992;77:55–61. doi: 10.3171/jns.1992.77.1.0055. [DOI] [PubMed] [Google Scholar]
- 83.Vespa P, Prins M, Ronne-Engstrom E, et al. Increase in extracellular glutamate caused by reduced cerebral perfusion pressure and seizures after human traumatic brain injury: A microdialysis study. J Neurosurg. 1998;89:971–82. doi: 10.3171/jns.1998.89.6.0971. [DOI] [PubMed] [Google Scholar]
- 84.Menzel M, Soukup J, Henze D, et al. Brain tissue oxygen monitoring for assessment of autoregulation: Preliminary results suggest a new hypothesis. J Neurosurg Anesthesiol. 2003;15:33–41. doi: 10.1097/00008506-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 85.Bruzzone P, Dionigi R, Bellinzona G, Imberti R, Stocchetti N. Effects of cerebral perfusion pressure on brain tissue PO2 in patients with severe head injury. Acta Neurochir Suppl. 1998;71:111–3. doi: 10.1007/978-3-7091-6475-4_33. [DOI] [PubMed] [Google Scholar]
- 86.Artru F, Jourdan C, Perret-Liaudet A, Charlot M, Mottolese C. Low brain tissue oxygen pressure: Incidence and corrective therapies. Neurol Res. 1998;20(Suppl 1):S48–51. doi: 10.1080/01616412.1998.11740610. [DOI] [PubMed] [Google Scholar]
- 87.Kiening KL, Unterberg AW, Bardt TF, Schneider GH, Lanksch WR. Monitoring of cerebral oxygenation in patients with severe head injuries: Brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg. 1996;85:751–7. doi: 10.3171/jns.1996.85.5.0751. [DOI] [PubMed] [Google Scholar]
- 88.Changaris DG, McGraw CP, Richardson JD, Garretson HD, Arpin EJ, Shields CB. Correlation of cerebral perfusion pressure and Glasgow Coma Scale to outcome. J Trauma. 1987;27:1007–13. doi: 10.1097/00005373-198709000-00009. [DOI] [PubMed] [Google Scholar]
- 89.McGraw CP. A cerebral perfusion pressure greater than 80 mmHg is more beneficial. In: Hoff JT, Betz AL, editors. Intracranial Pressure VII. Berlin: Springer-Verlag; 1989. pp. 839–841. [Google Scholar]
- 90.Juul N, Morris GF, Marshall SB, Marshall LF. Intracranial hypertension and cerebral perfusion pressure: Influence on neurological deterioration and outcome in severe head injury. The Executive Committee of the International Selfotel Trial. J Neurosurg. 2000;92:1–6. doi: 10.3171/jns.2000.92.1.0001. [DOI] [PubMed] [Google Scholar]
- 91.Andrews PJ, Sleeman DH, Statham PF, et al. Predicting recovery in patients suffering from traumatic brain injury by using admission variables and physiological data: A comparison between decision tree analysis and logistic regression. J Neurosurg. 2002;97:326–36. doi: 10.3171/jns.2002.97.2.0326. [DOI] [PubMed] [Google Scholar]
- 92.Downard C, Hulka F, Mullins RJ, et al. Relationship of cerebral perfusion pressure and survival in pediatric brain-injured patients. J Trauma. 2000;49:654–8. doi: 10.1097/00005373-200010000-00012. discussion 58-9. [DOI] [PubMed] [Google Scholar]
- 93.Reinert M, Barth A, Rothen HU, Schaller B, Takala J, Seiler RW. Effects of cerebral perfusion pressure and increased fraction of inspired oxygen on brain tissue oxygen, lactate and glucose in patients with severe head injury. Acta Neurochir (Wien) 2003;145:341–9. doi: 10.1007/s00701-003-0027-0. discussion 49-50. [DOI] [PubMed] [Google Scholar]
- 94.Catala-Temprano A, Claret Teruel G, Cambra Lasaosa FJ, Pons Odena M, Noguera Julian A, Palomeque Rico A. Intracranial pressure and cerebral perfusion pressure as risk factors in children with traumatic brain injuries. J Neurosurg. 2007;106:463–6. doi: 10.3171/ped.2007.106.6.463. [DOI] [PubMed] [Google Scholar]
- 95.Mehta A, Kochanek PM, Tyler-Kabara E, et al. Relationship of intracranial pressure and cerebral perfusion pressure with outcome in young children after severe traumatic brain injury. Dev Neurosci. 2010;32:413–9. doi: 10.1159/000316804. [DOI] [PubMed] [Google Scholar]
- 96.Figaji AA, Zwane E, Thompson C, et al. Brain tissue oxygen tension monitoring in pediatric severe traumatic brain injury. Part 1: Relationship with outcome. Childs Nerv Syst. 2009;25:1325–33. doi: 10.1007/s00381-009-0822-x. [DOI] [PubMed] [Google Scholar]
- 97.Brady KM, Lee JK, Kibler KK, et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke. 2007;38:2818–25. doi: 10.1161/STROKEAHA.107.485706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chan KH, Dearden NM, Miller JD, Andrews PJ, Midgley S. Multimodality monitoring as a guide to treatment of intracranial hypertension after severe brain injury. Neurosurgery. 1993;32:547–52. doi: 10.1227/00006123-199304000-00009. discussion 52-3. [DOI] [PubMed] [Google Scholar]
- 99.Globus MY, Busto R, Dietrich WD, Martinez E, Valdes I, Ginsberg MD. Effect of ischemia on the in vivo release of striatal dopamine, glutamate, and gamma-aminobutyric acid studied by intracerebral microdialysis. J Neurochem. 1988;51:1455–64. doi: 10.1111/j.1471-4159.1988.tb01111.x. [DOI] [PubMed] [Google Scholar]
- 100.Vespa PM, McArthur D, O’Phelan K, et al. Persistently low extracellular glucose correlates with poor outcome 6 months after human traumatic brain injury despite a lack of increased lactate: A microdialysis study. J Cereb Blood Flow Metab. 2003;23:865–77. doi: 10.1097/01.WCB.0000076701.45782.EF. [DOI] [PubMed] [Google Scholar]
- 101.al-Rawi PG, Hutchinson PJ, Gupta AK, Piechnik SK, Pickard JD, Kirkpatrick PJ. Multiparameter brain tissue monitoring — correlation between parameters and identification of CPP thresholds. Zentralbl Neurochir. 2000;61:74–9. doi: 10.1055/s-2000-8263. [DOI] [PubMed] [Google Scholar]


