Abstract
Background and Aims:
Children with facial clefts are usually difficult to intubate and it is considered safer to keep them spontaneously breathing while securing the airway. This prospective comparative study was conducted to evaluate endotracheal intubating conditions in pediatric patients undergoing cleft surgeries, without the use of muscle relaxants following induction with propofol and sevoflurane.
Materials and Methods:
Sixty patients aged 1month to 3 years, were randomly allocated into two equal groups. Anesthesia was induced with sevoflurane 8% in oxygen in group 1 and with propofol 3 mg/kg in group 2. Laryngoscopy and intubation were attempted 150 s after induction in both groups and ease of laryngoscopy, position of vocal cords, degree of coughing, jaw relaxation, and limb movements were assessed and scored. Total score of 5 was considered excellent, 6-10 good, 11-15 poor, and 16-20 bad. Total score ≤ 10 was considered clinically acceptable, and >10 as clinically unacceptable. Chi-square and Wilcoxon Mann-Whitney tests were used to analyze data.
Results:
There was no significant difference between groups when ease of laryngoscopy was compared. Sevoflurane induced patients had significantly better position of vocal cords at intubation and the propofol group had significantly more episodes of coughing. Significantly less number of patients had limb movements in sevoflurane group. There was no significant difference in degree of jaw relaxation between groups. The sevoflurane group had significantly better total scores and clinically acceptable intubating conditions.
Conclusion:
Sevoflurane 8% in oxygen provides clinically acceptable intubating conditions without use of muscle relaxants in pediatric cleft patients.
Keywords: Intubation without muscle relaxants, pediatric cleft surgeries, sevoflurane induction
Introduction
Children with cleft lip and palate are commonly associated with retrognathia, micrognathia, and glossoptosis;[1] and laryngoscopy is considered difficult in these cases. Delay in intubation in an apneic child is risky as they are prone for rapid desaturation. Hence, it is considered wiser to keep the patient spontaneously breathing while securing the airway, if a difficult airway is anticipated. In this study we aimed to evaluate endotracheal intubating conditions following induction with propofol and sevoflurane in pediatric patients undergoing cleft lip and palate surgeries, while preserving their spontaneous breathing, by avoiding use of muscle relaxants.
Materials and Methods
After approval from hospital ethical committee, this prospective, comparative study was conducted during the period October 2011-December 2012. Based on the available figures for the various study parameters,[2] with 95% confidence and 80% power, minimum sample size was calculated as 26 in each group to obtain statistically significant results. Hence, this study was conducted in 60 patients of American Society of Anesthesiologists (ASA) I and II, aged 1 month-3 years undergoing cleft surgeries, after taking consent from parents.
Patients were randomly allotted into two groups, Groups 1 and 2 of 30 patients each, by a closed envelope technique. Group 1 patients were induced with sevoflurane while Group 2 patients with propofol.
After a thorough preanesthetic checkup, children were kept nil per oral for 2 h for clear fluids, 4 h for milk, and 6 h for formula feeds and solids. Syrup triclofos 75 mg/kg bodyweight was given to children above 6 months, 2 h prior to induction. EMLA cream was applied to potential sites of venous cannulation 1 h prior to induction. In the preanesthesia room, an intravenous (IV) cannula of 22 or 24 G was inserted and patient's were shifted into the operating theater and preinduction monitoring initiated with monitors like noninvasive blood pressure, pulse oximetry, and electrocardiogram.
All the patients were given injection midazolam 0.05 mg/kg body weight, inj. glycopyrrolate 5 mg/kg body weight, and inj. fentanyl 3 mg/kg body weight intravenously.
In Group 1, anesthesia was induced with sevoflurane 8% in oxygen using a Jackson-Rees circuit. After the loss of eyelash reflex, intermittent positive pressure ventilation was commenced. Laryngoscopy and tracheal intubation were attempted at 150 s.
In Group 2, anesthesia was induced with inj. propofol 3 mg/kg body weight over a period of 30 s intravenously. Laryngoscopy and intubation were attempted 150 s after induction of anesthesia and patients were ventilated via face mask with 100% oxygen in the meantime. Additional bolus of 1 mg/kg of propofol was given if laryngoscopy was not possible due to muscle spasm, coughing, or excessive movements.
In both groups laryngoscopy was done using Macintosh blade and trachea was intubated with an appropriate sized uncuffed, preformed south pole oral endotracheal tube. Intraoperatively patients were ventilated with 60% nitrous oxide, 40% oxygen, and isoflurane 0.8-1% with gas flow rates of 2-3 l/min using a closed circuit. After intubation, inj. atracurium 0.5 mg/kg body weight was given intravenously. Intra-operatively mechanical ventilation was done at the rate of 20-25 breaths per min with a tidal volume of 8-10 ml/kg body weight to maintain end tidal carbon dioxide between 30 and 35 mmHg.
During laryngoscopy and intubation, each patient was assessed for five variables namely; ease of laryngoscopy, position of vocal cords, degree of coughing, jaw relaxation, and limb movements and scored accordingly.[3]
The sum of the scores of these five individual variables was computed as the Helbo-Hansen (Steyn's modification, Table 1) score.[4] Total score of 5 was considered to be excellent, 6-10 good, 11-15 poor, and 16-20 bad. Total scores were divided into clinically acceptable and not acceptable scores (total score ≤ 10 acceptable, >10 unacceptable).
Table 1.
Steyn's modification of Helbo-Hansen scoring system

Measurements of heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) were noted at different time intervals (preinduction, postinduction, postintubation at 0, 1, 3 5, 10, and 15 min). Measurements at 1 min after injection of glycopyrrolate were taken as baseline values.
In patients of both groups if intubation was not possible after two attempts, suxamethonium 2 mg/kg body weight was given and intubation was completed.
Statistical analysis
Percentage of patients with intubation score ≤10 was computed in both the groups and statistical significance of the difference was tested by applying chi-square test. In each group the change in clinical parameters from preinduction to other time points of observation were computed in terms of mean and standard deviation, and its statistical significance was tested by applying Wilcoxon Mann-Whitney test depending upon the distribution of values of the variable.
P < 0.05 was regarded as statistically significant, P < 0.001 highly significant, and P > 0.05 not significant.
Results
Both the groups were comparable with regards to age, sex, weight, ASA status, and surgery performed.
There were no statistically significant differences between groups when ease of laryngoscopy was compared. Laryngoscopy was easy in 96.7% of patients in group 1 and 93.3% of patients in group 2 [Table 2, Figure 1]. Sevoflurane induced patients had significantly better position of the vocal cords at intubation. In group 1, 83.3% had vocal cords in the open position vs 26.7% in group 2 [Table 2, Figure 2]. On comparing degree of coughing, it was seen that patients induced with propofol had significantly more coughing episodes than in patients induced with sevoflurane (19 vs 1) [Table 2].
Table 2.
Comparison of ease of laryngoscopy, position of vocal cords, and degree of coughing

Figure 1.
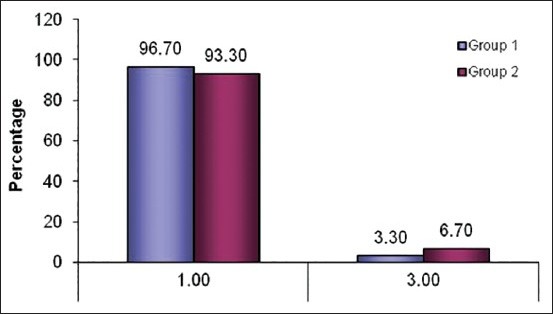
Distribution of ease of laryngoscopy
Figure 2.
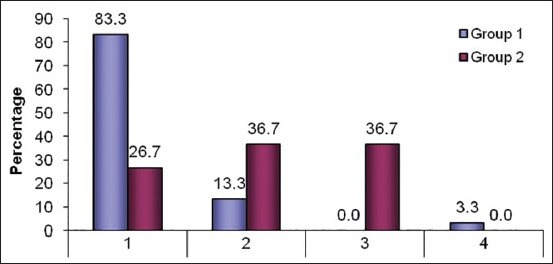
Distribution of position of vocal cords
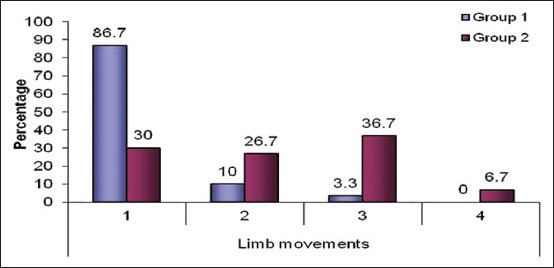
Significantly less number of patients had limb movements during intubation in group 1 when compared to group 2 (13.3 vs 70.1%) [Table 3, Figure 3]. There was no statistically significant difference in the degree of jaw relaxation between the two groups (P-value 0.221), as most patients in both groups had complete jaw relaxation (29 vs 28) [Table 3, Figure 4].
Table 3.
Comparison of limb movements and degree of jaw relaxation
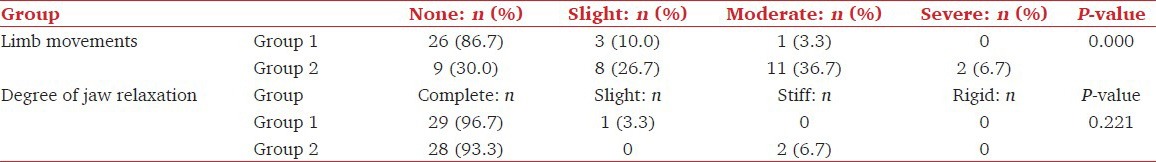
Figure 3.
Distribution of limb movements
Figure 4.
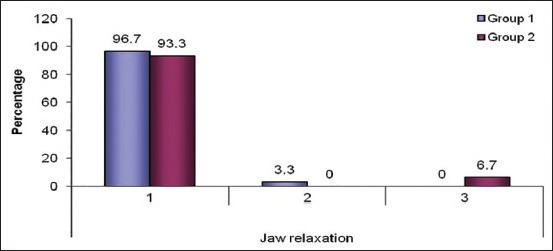
Distribution of jaw relaxation
The sevoflurane group 1 had significantly better total scores than group 2 [Table 4, Figure 5]. In group 1, 29 out of 30 had acceptable intubating conditions. In group 2, only 19 patients out of 30 had acceptable intubating conditions. Group 1 had significantly better intubating condition which was clinically acceptable than with group 2 [Table 5, Figure 6].
Table 4.
Comparison of total scores between the groups

Figure 5.

Distribution of total scores
Table 5.
Comparison of acceptable and unacceptable scores
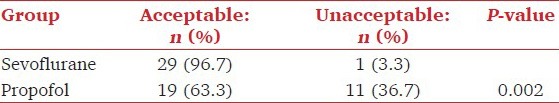
Figure 6.
Distribution of acceptable and unacceptable scores
Succinylcholine was used in one patient in group 1 and in two patients in group 2 which was not significant statistically [Table 6].
Table 6.
Comparison of use of suxamethonium among the groups

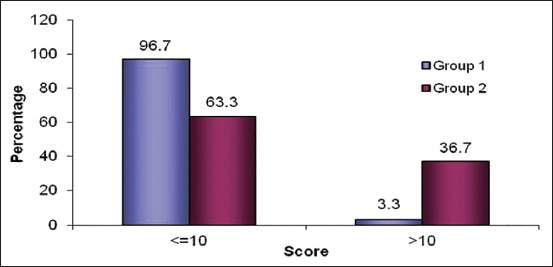
The mean HR, SBP, DBP, and MAP at preinduction did not show any significant difference between groups. After intubation, mean HR achieved was significantly lower in group 2 till 3 min [Table 7, Figure 7]. There was a significant fall in SBP after intubation in group 2 at 1 min after intubation which persisted till 15 min [Figure 8]. Group 2 patients had a significant fall in the DBP and MAP at 3 min following intubation which persisted till 15 min [Figures 9 and 10].
Table 7.
Comparison of heart rate at various time intervals

Figure 7.

Changes in heart rate
Figure 8.
Changes in systolic blood pressure (BP)
Figure 9.
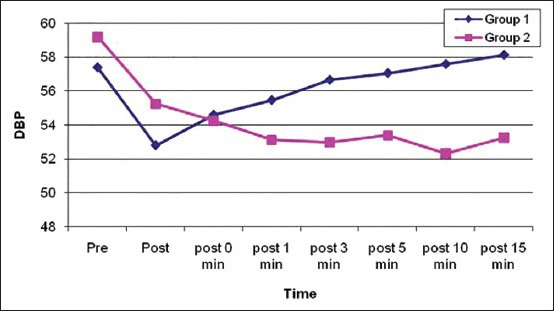
Changes in diastolic blood pressure (BP)
Figure 10.

Changes in mean arterial pressure (MAP)
Discussion
Cleft lip and cleft palate can be part of many syndromes like Pierre Robin, Treacher-Collin's, or Goldenhar; notoriously associated with difficulty in airway maintenance, mask ventilation, and endotracheal intubation. The high incidence of retrognathia, micrognathia, and glossoptosis in these patients make laryngoscopy difficult.[1,5] Though the incidence of failed intubation is reportedly only in 1% cases, it is wiser and safer to keep the patients spontaneously breathing until securing the airway,[5] especially if a difficult to ventilate scenario is anticipated. This practice increases the margin of safety markedly.
Suxamethonium, though provides almost ideal intubating conditions, has been contraindicated in the United States for routine use in children and adolescents due to the increased incidence of fatal or near fatal cardiac arrests following its use. This is attributed to hyperkalemia, developing especially in patients with undiagnosed muscular dystrophies. Other side effects include myalgia, prolonged apnea, and rarely precipitation of malignant hyperpyrexia.[3,4,6,7]
If difficult airway is anticipated, prolonged neuromuscular blockade and inability to quickly reverse the neuromuscular blockade make the use of nondepolarizing muscle relaxants for intubation less desirable.[3,4,6,7,8] They too have their share of side effects and complications like development of awareness under general anesthesia, residual paralysis, and allergic reactions.[9] Hence if laryngoscopy and intubation could be performed by avoiding the use of muscle relaxants, without compromising on the ease or success of the procedure, many adverse events during anesthesia can be avoided.
As newer IV induction agents and short acting potent opioids, which suppress the airway reflexes, were introduced into clinical practice, the scope for tracheal intubation without muscle relaxants was evaluated further.[2] Propofol, one of the most frequently used induction agent, has favorable depressant effect on the pharyngeal and laryngeal reflexes[10] and the muscle tone.[8,9] The induction with propofol is quick and smooth, with rapid awakening during recovery.[11] Propofol along with fentanyl is a good suppressor of stress response to laryngoscopy and intubation.
Among the inhalational agents which are presently available for clinical use, sevoflurane has merits of a pleasant smell, low airway irritability and low blood gas solubility, thereby facilitating a rapid and smooth induction.[12,13] Because of its stable hemodynamics,[13] less potential for myocardial depression and arrhythmogenecity,[14] it is considered a safe inhalational agent for induction.
There are many previous studies comparing intubating conditions following induction with various agents without use of muscle relaxants. Comparison of sevoflurane with propofol for intubation is a lesser explored area. There are studies comparing these agents, but sevoflurane induction was always done along with nitrous oxide and oxygen. In one such study, Sabapathy et al.,[2] showed superiority of 8% sevoflurane in 50% nitrous oxide with oxygen to propofol 3 mg/kg. Sevoflurane 8% with nitrous oxide (both 60[15] and 66%[12]) in oxygen also provided a clinically acceptable alternative to propofol 3 mg/kg and succinylcholine 2 mg/kg for tracheal intubation.[12]
Even though addition of nitrous oxide to the inhaled gases will deepen the plane of anesthesia, it may be disadvantageous in a difficult to ventilate and/or intubate patient, especially a child, as a reduction in the inhaled oxygen concentration will fasten desaturation if intubation somehow gets delayed. Moreover as spontaneous respiration is maintained, these patients will be breathing room air which may cause even faster desaturation due to diffusion hypoxia. For these reasons we chose not to use nitrous oxide before the airway was secured. But, despite avoiding nitrous oxide, the observations made during our study were almost similar to previous studies which employed nitrous oxide during induction. Thus it can be inferred that induction with 8% sevoflurane in oxygen increases the margin of safety without compromising the favorable intubating conditions.
Another extensively evaluated combination for providing acceptable intubating conditions without the use of neuromuscular blocking agent is a combination of opioid and propofol. Propofol with fentanyl,[16] alfentanil,[14,15] or remifentanil[17] proved to be feasible and safe in this regard. The stress responses associated with intubation were also completely inhibited.[17] However on comparison with sevoflurane, intubating conditions were less favorable with propofol, even when combined with an opioid.[2]
In situations of inability to ventilate or intubate in difficult airway patients, sevoflurane induction carries a definitive advantage of over propofol induction, as waking the patient up from anesthesia is easier and quicker following inhalation induction as compared to IV induction. It is because, the IV induction agent will have to get redistributed from brain or metabolized for awakening, whereas an inhalational agent with low blood gas solubility will provide a much rapid emergence.
Conclusions
Thus to conclude, considering the observations made in our study, we recommend sevoflurane 8% in oxygen to be used as induction agent in pediatric cleft patients as it provides clinically acceptable intubating conditions while maintaining spontaneous breathing.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Chandy TT, Pragasam AA, Joselyn AS. 2 nd ed. New Delhi: B.I Publications; 2008. Anaesthesia for cleft lip and palate repair. Understanding Pediatric Anesthesia; pp. 197–202. [Google Scholar]
- 2.Sabapathy VA, Thilaak P, Gopal SS, Pongiyanadar S. Endotracheal intubation without muscle relaxants in children undergoing cleft lip, palate and alveolar surgery. A comparative study of sevoflurane and propofol. J Clin Diagn Res. 2011;5:1421–5. [Google Scholar]
- 3.Srivastava U, Kumar A, Gandhi NK, Saxena S, Agarwal S. Comparison of propofol and fentanyl with thiopentone and suxamethonium for tracheal intubation in children. Ind J Anaesth. 2001;45:263–6. [Google Scholar]
- 4.Steyn MP, Quinn AM, Gillespie JA, Miller DC, Best CJ, Morton NS. Tracheal intubation without neuromuscular block in children. Br J Anaesth. 1994;72:403–6. doi: 10.1093/bja/72.4.403. [DOI] [PubMed] [Google Scholar]
- 5.Gunawardhana RH. Difficult laryngoscopy in cleft lip and palate surgery. Br J Anesth. 1996;76:757–9. doi: 10.1093/bja/76.6.757. [DOI] [PubMed] [Google Scholar]
- 6.Gupta A, Kaur R, Malhotra R, Kale S. Comparative evaluation of different doses of propofol, preceded by fentanyl on the intubating conditions and the pressor response during tracheal intubation without muscle relaxants. Paediatr Anaesth. 2006;16:399–405. doi: 10.1111/j.1460-9592.2005.01783.x. [DOI] [PubMed] [Google Scholar]
- 7.Robinson AL, Jerwood DC, Stokes MA. Routine suxamethonium in children. Anaesthesia. 1996;51:874–8. doi: 10.1111/j.1365-2044.1996.tb12623.x. [DOI] [PubMed] [Google Scholar]
- 8.Scheller MS, Zornow MH, Saidman LJ. Tracheal intubation without the use of muscle relaxants: A technique by using propofol and varying doses of alfentanil. Anesth Analg. 1992;75:788–93. doi: 10.1213/00000539-199211000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Donati F. Tracheal intubation: unconsciousness, analgesia and muscle relaxation. Can J Anaesth. 2003;50:99–103. doi: 10.1007/BF03017838. [DOI] [PubMed] [Google Scholar]
- 10.McKeating K, Bali IM, Dundee JW. The effects of thiopentone and propofol on upper airway integrity. Anaesthesia. 1988;43:638–40. doi: 10.1111/j.1365-2044.1988.tb04146.x. [DOI] [PubMed] [Google Scholar]
- 11.Kumar AA, Sanikop CS, Kotur PF. Effect of the priming principle on the induction dose requirement of propofol — A randomized clinical trial. Ind J Anaesth. 2006;50:283–7. [Google Scholar]
- 12.Thwaites AJ, Edmends S, Tomlinson AA, Kendall JB, Smith I. Double blind comparison of sevoflurane vs propofol and succinylcholine for tracheal intubation in children. Br J Anaesth. 1999;83:410–4. doi: 10.1093/bja/83.3.410. [DOI] [PubMed] [Google Scholar]
- 13.Swadia VN, Mamta GP. Comparison of the induction and intubation characteristics of sevoflurane and halothane in paediatric patients. Indian J Anaesth. 2001;45:294–9. [Google Scholar]
- 14.Coghlan SF, McDonald PF, Csepregi G. Use of alfentanil with propofol for nasotracheal intubation without neuromuscular block. Br J Anaesth. 1993;70:80–91. doi: 10.1093/bja/70.1.89. [DOI] [PubMed] [Google Scholar]
- 15.Blair JM, Hill DA, Bali IM, Fee JP. Tracheal intubating conditions after induction with sevoflurane 8% in children. A comparison with two intravenous techniques. Anaesthesia. 2000;55:774–8. doi: 10.1046/j.1365-2044.2000.01470.x. [DOI] [PubMed] [Google Scholar]
- 16.Shaikh SI, Bellagali VP. Tracheal intubation without neuromuscular block in children. Indian J Anaesth. 2010;54:29–34. doi: 10.4103/0019-5049.60493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Batra YK, Al Qattan AR, Ali SS, Qureshi MI, Kuriakose D, Migahed A. Assessment of tracheal intubating conditions in children using remifentanil and propofol without muscle relaxant. Paediatr Anaesth. 2004;14:452–6. doi: 10.1111/j.1460-9592.2004.01208.x. [DOI] [PubMed] [Google Scholar]


