Abstract
Background and Aims:
The anatomic site and the volume of local anesthetic needed for an ultrasound-guided saphenous nerve block differ in the literature. The purpose of this study was to examine the effect of two different ultrasound-guided low volume injections of local anesthetic on saphenous and vastus medialis nerves.
Materials and Methods:
Recruited patients (N = 48) scheduled for orthopedic surgery were randomized in two groups; Group distal adductor canal (DAC): Ultrasound-guided injection (5 ml of local anesthetic) distal to the inferior foramina of the adductor canal. Group adductor canal (AC): Ultrasound-guided injection (5 ml local anesthetic) within the adductor canal. Following the injection of local anesthetic, block progression was monitored in 5 min intervals for 15 min in the sartorial branches of the saphenous nerve and vastus medialis nerve.
Results:
Twenty two patients in each group completed the study. Complete block of the saphenous nerve was observed in 55% and 59% in Group AC and DAC, respectively (P = 0.88). The proportion of patients with vastus medialis weakness at 15 min in Group AC, 36%, was significantly higher than in Group DAC (0/22), (P = 0.021).
Conclusions:
Low volume of local anesthetic injected within the adductor canal or distally its inferior foramina leads to moderate success rate of the saphenous nerve block, while only the injection within the adductor canal may result in vastus medialis nerve motor block.
Keywords: saphenous nerve block, sonographic, vastus medialis
Introduction
Successful anesthesia of the saphenous nerve is important for surgery of the lower extremity, especially when combined with other peripheral nerve blocks. The saphenous nerve can be blocked at various anatomic locations: Above the knee, at the level of the knee, below the knee, or just above the medial malleolus.[1] It has been shown that saphenous nerve block, at the level or above the knee, provides a more reliable anesthesia compared to the traditional block techniques below the knee.[1,2,3] Recently, a few studies have been published that provide an ultrasonographic identification of the saphenous nerve. However, the exact anatomic area where the nerve is visualized, as well as the volume of local anesthetic used for saphenous nerve block, differ among studies. Most of the published studies used a volume of local anesthetic that ranged from 7 to 15 ml.[4,5,6,7,8,9,10,11,12,13] In addition, the effects of the saphenous nerve block on the vastus medialis muscle have not been thoroughly described at different anatomic levels.
Therefore, the purpose of this study was to compare the efficacy of the saphenous nerve block and its consequences on the vastus medialis muscle function between two different ultrasound-guided low volume injections of local anesthetic: The first injection within the distal part of the adductor canal while the second, distally to its inferior foramen.
Materials and Methods
After institutional Ethics Committee approval of the protocol, patients with body mass index (BMI) <30 kg/m2 scheduled for orthopedic surgery (knee arthroscopy and ankle fracture repair) were recruited in the study. Patients younger than 18 years or older than 85 years, with an allergy to local anesthetics, bleeding disorders, Glasgow Coma Scale <15, pregnancy and neurologic deficits, were excluded from the study.
After written informed consent, patients were randomized in two groups: Group adductor canal (AC): Ultrasound-guided saphenous nerve block within the distal part of the adductor canal, medially to the femoral artery [Figure 1].[8] Group distal adductor canal (DAC): Ultrasound-guided saphenous nerve block at the compartment between the sartorius muscle and the femoral artery distal to the inferior foramina of the adductor canal [Figure 2].[11]
Figure 1.

Ultrasound-guided injection of local anesthetic within the distal part of the adductor canal. A = Femoral artery, S = Saphenous nerve, LA = Local anesthetic
Figure 2.

Ultrasound-guided injection of local anesthetic at the compartment between the sartorius muscle and the femoral artery distal to the inferior foramina of the adductor canal. A = Femoral artery, V = Femoral vein, LA = Local anesthetic
Randomization was attained by computer generated randomization sequence (www.randomizer.org) in pre-prepared opaque envelopes. Sensory and motor block assessments were performed by an anesthesiologist who was blinded to the technique performed.
After applying standard monitoring (pulse oximetry, electrocardiography and non-invasive arterial blood pressure), the patient was pre-medicated with intravenous midazolam (0.03 mg/kg). Skin disinfection of the anterior and medial surface of the distal two thirds of the thigh was performed with 2% chlorhexidine in 70% isopropyl alcohol and the transducer was covered with a sterile sheath. All anatomic structures of the subsartorial region were visualized using a portable ultrasound machine (Vivid I; GE Healthcare, Waukesha, Wisconsin, USA) with a linear 5-12 MHz probe. In both groups 5 ml of 1.5% lidocaine with 5 mcg/ml adrenaline were injected through a 22-gauge needle with extension tubing (Stimulplex D, B Braun, Melsungen, Germany).
Following the injection of local anesthetic, block progression was monitored at 5 min intervals for 15 min in the sartorial branches of the saphenous nerve and the nerve to vastus medialis muscle.
The sensory block was scored as 0 = no sensory block, 1 = decreased partial sensory block, 2 = complete sensory block at each anatomic area that was tested. We considered successful complete saphenous nerve block if absolute absence of sensation to pinprick developed in two different anatomic areas (just proximal to the medial malleolus and just below the tibial tubercle with a maximum score of 4).[1,2,8]
The strength of vastus medialis contraction was examined at the last 20° of knee extension, while at the same time the examiner palpated the inner aspect of the thigh detecting contraction of the muscle. Vastus medialis weakness was rated according to the following scale: 0 = No motor block, 1 = partial motor block (weakness to knee extension at the last 20°), 2 = complete motor block (inability to knee extension at the last 20°).[14,15,16] In every case, after 15 min of block placement, an ultrasound-guided sciatic nerve block was used as an adjuvant and laryngeal mask airway general anesthesia was induced in the usual fashion.
The primary end point of this study was the percentage of complete sensory block of the saphenous nerve at 15 min. Secondary end points were the percentage of complete or partial motor block of the vastus medialis nerve at 15 min. The percentage of complete sensory block of the saphenous at different time points was examined. The incidence of vascular puncture, paresthesia during the procedure and potential neurological complications at 7 days were also recorded.
Statistical analysis
The efficacy of the different techniques of the saphenous nerve block is variable depending on the type of the technique and the volume of the local anesthetic used. The success rate varies considerably in the literature: 80% with the transsartorial and perifemoral approaches, 40% with the below-the-knee field block[1,2,3] and 77% to 100% with ultrasound guidance at different anatomic areas above the knee.[4,5,6,7,8,9,10,11,12] In addition, there was no previous study that examined the efficacy of the saphenous nerve block with a volume of 5 ml of local anesthetic within and distal to the adductor canal. Using data from a small prospective study of ultrasound-guided saphenous nerve block distal to the inferior foramina of the adductor canal in our center (10 patients), we observed a mean success rate of 50% of complete sensory block at 15 min. A sample size of 21 patients per group was thus considered to detect an increase in the success rate at 15 min from 50% in Group DAC to 90% in Group AC, with a β error of 20% and an α error of 5%. To allow for protocol violations or increased variability in data 48 patients were eventually recruited.
For non-parametric data (success rates, proportion of patients with vastus medialis muscle weakness) Chi-square test with Yates correction and for parametric data (patients’ weight and age) t-test for independent variables were performed. Continuous data are presented as mean (SD) and categorical data are presented as n (%). P < 0.05 was considered to be statistically significant.
Results
Two patients randomized in AC group and two in DAC group were removed from further analysis due to unsuccessful spread of the local anesthetic to the targeted anatomic area. The population data of the remaining 44 patients are presented in Table 1.
Table 1.
Population data
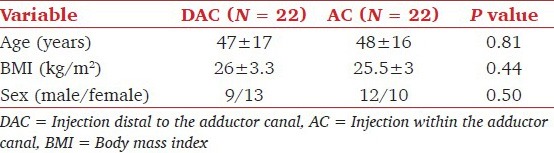
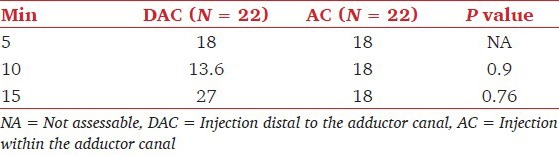
A total of 12/22 (55%) and 13/22 (59%) patients had a complete sensory block (total sensory score 4/4) of the saphenous nerve when the injection was performed either within or distal to the adductor canal, respectively, (P = 0.88). In group AC, 5/22 and in group DAC, 6/22 patients had a total sensory score (3/4), (P = 0.88). 5/22 and 3/22 in AC and DAC group had total sensory score of (2/4), respectively, (P = 0.91). In both groups no patients recorded with total sensory scores (1/4) or (0/4). The percentage of patients with complete sensory saphenous nerve block at each time interval of evaluation up to 15 min were also statistically comparable [Table 2].
Table 2.
Percentage of patients with saphenous nerve block at each examination time point
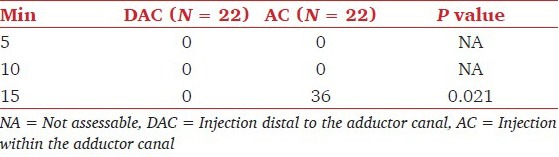
In both techniques complete vastus medialis nerve block was not found at 15 min. The proportion of patients with vastus medialis weakness at 15 min in Group AC 8/22 (36.3%) was significantly larger than in Group DAC (0/22), (P = 0.021) [Table 3].
Table 3.
Percentage of patients with vastus medialis motor block at each examination time point
No statistically significant difference was observed for the incidence of vascular punctures between groups (one in Group DAC). Signs and symptoms of local anesthetic toxicity were not observed. Three cases of transient paresthesia elicited in Group AC and one in Group DAC. In both groups after 1-week follow-up, no neurological complication associated with the anesthetic technique was reported.
Discussion
The use of ultrasound for peripheral nerve blockade is becoming popular. Although the aid of ultrasound guidance has increased interest in blocking the saphenous nerve proximal to the knee, until today there are only a limited number of studies that describe in detail an ultrasound-guided saphenous nerve block.[4,5,6,7,8,9,10,11,12] The local anesthetic volume, the anatomic approach and the success rate of the saphenous nerve block significantly differ among studies. In one study, low volume of levobupivacaine 2.5 mg/ml was injected between the tendons of the sartorius and gracilis muscles with reported success rate of 92% (13/14); the volume of local anesthetic, however, was not constant and ranged between 5 and 7 ml.[6] In our study, the injection of a low volume of local anesthetic distally to the adductor canal may not be sufficient to completely spread around the saphenous nerve. In the adductor canal, the combination of the high saphenous nerve anatomic variability and the vessel sheath might all have been contributed to the incomplete spread of the local anesthetic to the nerve, justifying the moderate success rate of the saphenous nerve block.[11] Additionally, significant number of our patients had total sensory score 3/4 and none of them had scores of 1/4 or 0/4. Perhaps, the low total dose of lidocaine, 75 mg, administered was also a contributory factor of our results.
The vastus medialis muscle is one of the four quadriceps muscles that participate in the extensor apparatus of the knee, contributing in the stabilization of the patella and in the performance of the last 10-20° of the knee extension.[16,17] Therefore, in our study, we considered as vastus medialis nerve block when our patients reported weakness at the last 20° of knee extension.
A previous study using magnetic resonance imaging revealed that 30 ml of local anesthetic injected through a catheter into the adductor canal filled out the entire adductor canal.[18] Additionally, in a study by Jæger et al.,[19] injected 30 ml of local anesthetic in the adductor canal and showed reduced quadriceps muscle strength in 8% of patients. The authors observed delayed and transient response in quadriceps motor strength. This response could be explained by the observation that large volume of local anesthetic could result in diffusion to the motor fibers of the femoral nerve outside the adductor canal.[19,20] In these studies[19,20] a handheld dynamometer was used to assess quadriceps muscle strength. However, while this method is able to precisely quantify quadriceps muscle force in units, it cannot assess the function of each quadriceps “head” separately. Furthermore, profound quadriceps muscle weakness has been reported after a continuous adductor canal block, showing that continuous injection of local anesthetic in the adductor canal can spread in a retrograde fashion, towards the common femoral nerve, that potentially results in quadriceps weakness.[21] Recently, Kim et al.[22] showed that the adductor canal block exhibited early relative sparing of quadriceps strength compared with the femoral nerve block 6-8 h post-anesthesia. However, in this study, dynamometer readings of the quadriceps muscle, but not of the vastus medialis muscle, were evaluated between the two blocks.
In our study, the strength of vastus medialis was manually tested using a semiquantitative approach that is the most common method applied in routine clinical examinations, despite certain limitations.[23] As we specifically examined the motor function of vastus medialis muscle, we considered the vastus medialis muscle motor weakness, observed 15 min immediately after local anesthetic injection, as a result of a block of the nerve to the vastus medialis and not as a result of the diffusion from the adductor canal to other branches of the femoral nerve.
Anatomically, both the saphenous nerve and the nerve to the vastus medialis muscle are branches of the posterior division of the femoral nerve. They travel along the lateral aspect of the superficial femoral artery in the proximal thigh, within the adductor canal.[24] The nerve supply to the vastus medialis muscle is often double; the upper one third of the muscle is usually supplied by a separate branch that is closely associated with the nerve of the vastus intermedius muscle, while the middle and lower thirds of the muscle usually receive branches from a common nerve. The latter is similar to the classical nerve to vastus medialis, which is described in textbooks as running in the adductor canal, along with the saphenous nerve and the vascular bundle.[25] The nerve to vastus medialis mainly pierces the vastus medialis muscle proximal to the site where the saphenous nerve crosses the anterior surface of the femoral artery to become medial to the vessel.[24] Although in our cases, the injection of local anesthetic took place more distally from this anatomic area, vastus medialis muscle weakness was reported when the injection of local anesthetic was performed in the distal part of the adductor canal. Proximal spread of the local anesthetic and/or more distal course of vastus medialis nerve to the corresponding muscle may explain this result. The post-operative visual analog score, the performance time of the nerve blocks and the patients’ satisfaction during the block procedure were not assessed since the end points of this study was the success rate of saphenous nerve block and its consequences on vastus medialis muscle function. Hence these were few limitations of our study which maybe overcome in future studies.
Conclusions
In conclusion, the low volume of local anesthetic injected within the distal part of the adductor canal or distally to its inferior foramen leads to moderate success rate of saphenous nerve block. Additionally, local anesthetic injection within the adductor canal can result in partial vastus medialis nerve motor block and subsequently to weakness of knee extension.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Benzon HT, Sharma S, Calimaran A. Comparison of the different approaches to saphenous nerve block. Anesthesiology. 2005;102:633–8. doi: 10.1097/00000542-200503000-00023. [DOI] [PubMed] [Google Scholar]
- 2.van der Wal M, Lang SA, Yip RW. Transsartorial approach for saphenous nerve block. Can J Anaesth. 1993;40:542–6. doi: 10.1007/BF03009739. [DOI] [PubMed] [Google Scholar]
- 3.De Mey JC, Deruyck LJ, Cammu G, De Baerdemaeker LE, Mortier EP. A paravenous approach for the saphenous nerve block. Reg Anesth Pain Med. 2001;26:504–6. doi: 10.1053/rapm.2001.25925. [DOI] [PubMed] [Google Scholar]
- 4.Andersen HL, Gyrn J, Møller L, Christensen B, Zaric D. Continuous saphenous nerve block as supplement to single-dose local infiltration analgesia for postoperative pain management after total knee arthroplasty. Reg Anesth Pain Med. 2013;38:106–11. doi: 10.1097/AAP.0b013e31827900a9. [DOI] [PubMed] [Google Scholar]
- 5.Kent ML, Hackworth RJ, Riffenburgh RH, Kaesberg JL, Asseff DC, Lujan E, et al. A comparison of ultrasound-guided and landmark-based approaches to saphenous nerve blockade: A prospective, controlled, blinded, crossover trial. Anesth Analg. 2013;117:265–70. doi: 10.1213/ANE.0b013e3182908d5d. [DOI] [PubMed] [Google Scholar]
- 6.Sahin L, Sahin M, Isikay N. A different approach to an ultrasound-guided saphenous nerve block. Acta Anaesthesiol Scand. 2011;55:1030–1. doi: 10.1111/j.1399-6576.2011.02481.x. [DOI] [PubMed] [Google Scholar]
- 7.Tsai PB, Karnwal A, Kakazu C, Tokhner V, Julka IS. Efficacy of an ultrasound-guided subsartorial approach to saphenous nerve block: A case series. Can J Anaesth. 2010;57:683–8. doi: 10.1007/s12630-010-9317-1. [DOI] [PubMed] [Google Scholar]
- 8.Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009;34:578–80. doi: 10.1097/aap.0b013e3181bfbf84. [DOI] [PubMed] [Google Scholar]
- 9.Tsui BC, Ozelsel T. Ultrasound-guided transsartorial perifemoral artery approach for saphenous nerve block. Reg Anesth Pain Med. 2009;34:177–8. doi: 10.1097/AAP.0b013e31819a273e. [DOI] [PubMed] [Google Scholar]
- 10.Horn JL, Pitsch T, Salinas F, Benninger B. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med. 2009;34:486–9. doi: 10.1097/AAP.0b013e3181ae11af. [DOI] [PubMed] [Google Scholar]
- 11.Saranteas T, Anagnostis G, Paraskeuopoulos T, Koulalis D, Kokkalis Z, Nakou M, et al. Anatomy and clinical implications of the ultrasound-guided subsartorial saphenous nerve block. Reg Anesth Pain Med. 2011;36:399–402. doi: 10.1097/AAP.0b013e318220f172. [DOI] [PubMed] [Google Scholar]
- 12.Krombach J, Gray AT. Sonography for saphenous nerve block near the adductor canal. Reg Anesth Pain Med. 2007;32:369–70. doi: 10.1016/j.rapm.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Kirkpatrick JD, Sites BD, Antonakakis JG. Preliminary experience with a new approach to performing an ultrasound-guided saphenous nerve block in the mid to proximal femur. Reg Anesth Pain Med. 2010;35:222–3. doi: 10.1097/AAP.0b013e3181d24589. [DOI] [PubMed] [Google Scholar]
- 14.Javadpour PJ, Finigan PJ, O’Brien M. The an atomy of the extensor mechanism and its clinical relevance. Clin J Sport Med. 1991;1:233–5. [Google Scholar]
- 15.Lieb FJ, Perry J. Quadriceps function. An anatomical and mechanical study using amputated limbs. J Bone Joint Surg Am. 1968;50:1535–48. [PubMed] [Google Scholar]
- 16.Smith TO, Nichols R, Harle D, Donell ST. Do the vastus medialis obliquus and vastus medialis longus really exist? A systematic review. Clin Anat. 2009;22:183–99. doi: 10.1002/ca.20737. [DOI] [PubMed] [Google Scholar]
- 17.Malone T, Davies G, Walsh WM. Muscular control of the patella. Clin Sports Med. 2002;21:349–62. doi: 10.1016/s0278-5919(02)00014-5. [DOI] [PubMed] [Google Scholar]
- 18.Lund J, Jenstrup MT, Jaeger P, Sørensen AM, Dahl JB. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: Preliminary results. Acta Anaesthesiol Scand. 2011;55:14–9. doi: 10.1111/j.1399-6576.2010.02333.x. [DOI] [PubMed] [Google Scholar]
- 19.Jæger P, Zaric D, Fomsgaard JS, Hilsted KL, Bjerregaard J, Gyrn J, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: A randomized, double-blind study. Reg Anesth Pain Med. 2013;38:526–32. doi: 10.1097/AAP.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 20.Jaeger P, Nielsen ZJ, Henningsen MH, Hilsted KL, Mathiesen O, Dahl JB. Adductor canal block versus femoral nerve block and quadriceps strength: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology. 2013;118:409–15. doi: 10.1097/ALN.0b013e318279fa0b. [DOI] [PubMed] [Google Scholar]
- 21.Veal C, Auyong DB, Hanson NA, Allen CJ, Strodtbeck W. Delayed quadriceps weakness after continuous adductor canal block for total knee arthroplasty: A case report. Acta Anaesthesiol Scand. 2014;58:362–4. doi: 10.1111/aas.12244. [DOI] [PubMed] [Google Scholar]
- 22.Kim DH, Lin Y, Goytizolo EA, Kahn RL, Maalouf DB, Manohar A, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: A Prospective, randomized, controlled trial. Anesthesiology. 2014;120:540–50. doi: 10.1097/ALN.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 23.Maffiuletti NA. Assessment of hip and knee muscle function in orthopaedic practice and research. J Bone Joint Surg Am. 2010;92:220–9. doi: 10.2106/JBJS.I.00305. [DOI] [PubMed] [Google Scholar]
- 24.Kapoor R, Adhikary SD, Siefring C, McQuillan PM. The saphenous nerve and its relationship to the nerve to the vastus medialis in and around the adductor canal: An anatomical study. Acta Anaesthesiol Scand. 2012;56:365–7. doi: 10.1111/j.1399-6576.2011.02645.x. [DOI] [PubMed] [Google Scholar]
- 25.Thiranagama R. Nerve supply of the human vastus medialis muscle. J Anat. 1990;170:193–8. [PMC free article] [PubMed] [Google Scholar]


