Abstract
High glucose production contributes to fed and fasted hyperglycemia in Type 1 Diabetes (T1D) and Type 2 Diabetes (T2D). The breakdown of the adiponectin signaling pathway in T1D and the reduction of circulating adiponectin in T2D contribute to this abnormal increase in glucose production. Sufficient amounts of insulin could compensate for the loss of adiponectin signaling in T1D and T2D and reduce hyperglycemia. However, the combination of low adiponectin signaling and high insulin resembles an insulin resistance state associated with cardiovascular disease and decreased life expectancy. Future development of medications that correct the deficiency of adiponectin signaling in the liver could restore the metabolic balance in T1D and T2D and reduce the need for insulin. This article reviews the adiponectin signaling pathway in the liver through T-cadherin, AdipoR1, AdipoR2, AMPK, ceramidase activity, APPL1 and the recently discovered Suppressor Of Glucose from Autophagy (SOGA).
1. Liver contribution to circulating glucose
The liver releases glucose ensuring sufficient amounts of this essential fuel are always available in the circulation for other tissues. Endocrine and neural mechanisms stimulate the liver during fasting, exercise and pregnancy to meet the increased demand for glucose. In addition to ensuring the availability of glucose, the liver plays a major role in preventing hyperglycemia. Hyperglycemia causes increased osmolarity, oxidative damage, glycation end products and other changes that contribute to the life threatening complications of diabetes. Liver glucose production is lowered through (a) the inhibition of gluconeogenesis, glycogenolysis, proteolysis and lipolysis and (b) the stimulation of glycolysis and the synthesis of glycogen, protein and lipids.
2. Adiponectin suppression of liver glucose production
Adiponectin (30 kDa) is a hormone produced by adipocytes that was discovered in 1995 by subtractive hybridization studies aimed at identifying adipocyte differentiation genes [1]. The idea that adipocytes secrete an insulin sensitizing protein was inconceivable before the reduction of adiponectin mRNA in the obese state was reported in 1996 [2]. Computed tomography (CT) scans that showed omental fat expansion is associated with the reduction of circulating adiponectin in 1999 suggested that adiponectin could raise liver insulin sensitivity [3].
Human adiponectin consists of 244 amino acids that generate a collagenous N-terminal domain and a globular C-terminal domain [4]. About 90% of the circulating adiponectin in humans is bound in (a) a high molecular weight (HMW) structure (360–540 kDa) comprised of either 12 or 18 adiponectin molecules or (b) a low molecular weight (LMW) structure (180 kDa) comprised of 6 adiponectin molecules. At 5 μg/ml, the molar concentration of HMW and LMW adiponectin in human plasma is approximately 3 nM [5]. The remaining 10% of the circulating adiponectin in humans is bound in a structure (90 kDa) called the full-length adiponectin trimer comprised of 3 adiponectin molecules.
HMW, LMW adiponectin and full-length trimers are stable in solution, meaning that a decrease in one isoform does not enable the remaining isoforms to restore the balance [6]. However, under reducing conditions (low pH) that result in disulfide bond cleavage in vitro, HMW and LMW adiponectin produce full-length trimers and globular domain trimers that lack the collagenous N-terminal domain [1, 7, 8]. The reduction and proteolytic processing of HMW and LMW adiponectin is reviewed below in the context of receptor binding.
Intraperitoneal injection of HMW and LMW adiponectin lowers plasma glucose in healthy mice as well as mice with Type 1 Diabetes (T1D) and Type 2 Diabetes (T2D) [9]. High doses of adiponectin do not cause hypoglycemia. Insulin lowers plasma glucose by lowering glucose production and raising glucose disposal. Insulin injection does not cause hypoglycemia when its ability to stimulate glucose uptake is eliminated [10]. The absence of hypoglycemia in mice injected with high doses of HMW and LMW adiponectin suggests the glucose lowering effect of adiponectin is primarily mediated through the inhibition of glucose production.
Euglycemic clamp studies using tracers could distinguish whether the reduction of plasma glucose is mediated by a decrease in glucose production, an increase in glucose disposal or both. Intravenous infusion of HMW and LMW adiponectin in mice, causing a 3-fold elevation in circulating adiponectin, lowers glucose production by 65% without any effect on glucose disposal or glycolysis [11]. Targeted genetic modifications in mice, causing a 3-fold elevation or a complete absence of HMW and LMW adiponectin, have effects solely on glucose production as well [12–14].
Cultured liver cells release glucose into the media, but short exposure to HMW and LMW adiponectin inhibits glucose production by 20–40% [9, 15]. Similar exposure to full-length adiponectin trimers, derived by disulfide bond cleavage of HMW and LMW adiponectin, lowers glucose production by 90% [8].
3. Clinical Correlation: Low adiponectin and Type 2 Diabetes
Low circulating adiponectin in the obese and lipodystrophic states can cause an elevation in glucose production that causes an increase in beta cell insulin secretion [16, 17]. Frank diabetes can be avoided as long as the beta cell could compensate for the reduction of circulating adiponectin. However, when the beta cell cannot keep glucose production under control, the decrease in circulating adiponectin could raise glucose production, contributing to the appearance of T2D.
Interest in the therapeutic properties of adiponectin peaked amid reports that a class of highly effective oral diabetes medications cause a 2- to 3-fold elevation in circulating adiponectin [18]. Thiazolinedione (TZD) drugs are amphipathic compounds that interact with the ligand binding domain of peroxisome proliferator-activated receptor-gamma (PPAR-γ), a member of the steroid receptor family of transcription factors and dominant promoter of adipocyte differentiation. Studies in T2D patients, adiponectin transgenic and knockout mice suggest the therapeutic effects of TZD drugs are at least partly mediated by the elevation of adiponectin followed by decreases in liver glucose production, circulating glucose and insulin [8, 12, 13, 18].
TZD drugs restore circulating levels of adiponectin in people with T2D, sparing the beta cell from having to overproduce insulin and reducing the unwanted effects of hyperinsulinemia [19]. When prescribed alone, TZDs lower glucose without the risk of hypoglycemia; however, concerns about their side effects have shifted the focus on adiponectin-based therapeutics away from the elevation of circulating adiponectin [20]. The sheer abundance of circulating adiponectin, its complex structures and short half-life (150 minutes) make the activation of the adiponectin signaling pathway a more promising target in the clinical treatment of T2D than the elevation of circulating adiponectin [21].
4. Liver cell surface receptors
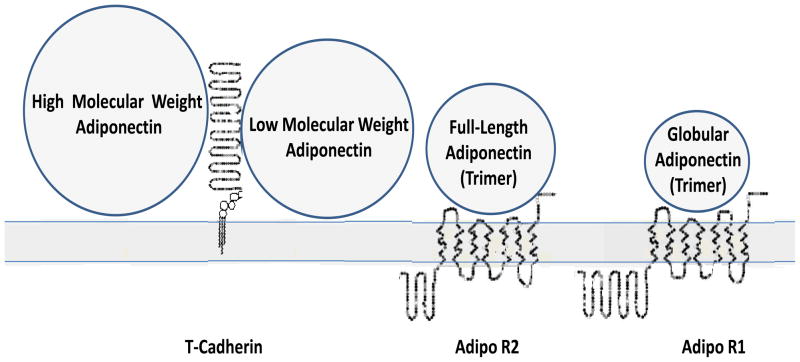
The reduction of Cys-Cys bonds and proteolytic processing of HMW and LMW adiponectin into full-length and globular adiponectin trimers suggests that circulating adiponectin mediates its effects through a cell surface receptor system that depends on multiple proteins. Accordingly, three cell surface receptors were identified between 2003 and 2004. HMW and LMW adiponectin ligands led to the identification of T-cadherin whereas full-length and globular adiponectin trimers led to the identification of adiponectin receptor-1 and -2 (AdipoR1 and AdipoR2) (Figure 1).
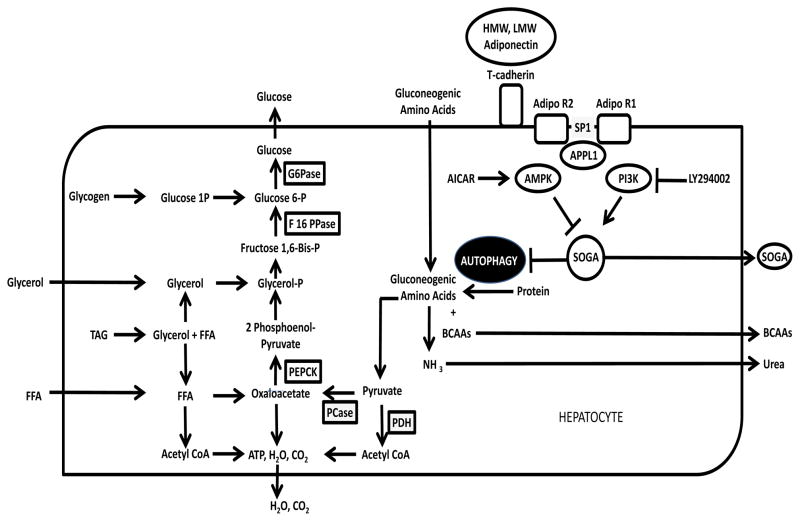
Figure 1. Synergy Model of Adiponectin Receptors.
HMW and LMW adiponectin binding to T-cadherin leads to (a) disulfide bond cleavage producing “full-length adiponectin trimers” that bind to AdipoR2 and (b) proteolytic cleavage producing “globular adiponectin trimers” that bind to AdipoR1. T-Cadherin, AdipoR1 and AdipoR2 expression is not limited to hepatocytes.
Adiponectin binding to T-cadherin (90 kDa) is evident using N-Flag-tagged HMW and LMW murine adiponectin, anti-Flag linked magnetic beads, retroviral transduced murine bone marrow Ba/F3 cells expressing a murine C2C12 myoblast undifferentiated cDNA library and, finally, PCR amplification of isolated clones. T-cadherin-adiponectin binding is also evident by co-immunoprecipitation, ELISA and FACS based binding assays [22]. The half-maximal binding concentration of HMW and LMW adiponectin to stable transfected C-GFP-tagged T-cadherin in Chinese hamster ovary (CHO) cells is 25 nM (trimer equivalents). T-cadherin does not bind to full-length adiponectin trimers or globular adiponectin trimers.
T-cadherin was discovered in the nervous system, but it has widespread tissue distribution including the liver [23]. It belongs to a family of cell surface proteins involved in Ca2+ mediated cell-cell interactions [24]. The globular domain of adiponectin contains a Ca2+ binding site, dependent on Asp 288, that plays a role in T-cadherin binding [6]. Ca2+ chelators like EDTA block T-cadherin binding in Ba/F3 cells suggesting a potential role of a divalent cation such as Ca2+ in hormone-receptor interactions [22]. T-cadherin gene ablation produces a 10-fold elevation in circulating adiponectin due to the release of adiponectin that is normally sequestered to the cell surface [25].
T-cadherin is not an integral membrane protein. It is retained on the extracellular membrane by a glycosylphosphatidylinositol (GPI) anchor that localizes to caveolin-rich microdomains called lipid rafts [26]. The mechanism of T-cadherin mediated signaling may be similar to other GPI-anchored signal-transducing receptors capable of recruiting additional proteins upon ligand binding. The absence of an intracellular domain, the lipid raft link and the absence of full-length or globular adiponectin trimer binding to T-cadherin suggest the adiponectin signaling pathway depends on additional co-receptors.
Adiponectin binding to AdipoR1 (42 kDa) is evident using fluorescent labeled globular adiponectin trimers, retroviral transduced Ba/F3 cells expressing a human skeletal muscle cDNA library and clone selection by fluorescence-activated cell sorting (FACS) [27]. AdipoR1-globular adiponectin trimer binding is also evident by yeast two-hybrid screening of human fetal brain cDNA [28].
AdipoR1 has 7 transmembrane domains, like G-protein coupled receptors, but an inverse topology [27]. Yeast two-hybrid screening shows that the globular adiponectin trimer interacts with C-terminal domain of AdipoR1 (aa 311–375) [28]. AdipoR1 is not a tyrosine kinase receptor like the insulin receptor. In vivo labeling studies reveal little tyrosine phosphorylation of AdipoR1 under basal or adiponectin-stimulated conditions [28].
AdipoR2 (34 kDa), identified on the basis of its homology to AdipoR1, is highly liver specific [27]. Full-length adiponectin trimer has a higher binding affinity to liver membrane fractions than globular adiponectin trimers [29]. In C2C12 myocytes, the globular adiponectin trimer binds with greater affinity to AdipoR1 (Kd = 1.14 nM) than AdipoR2 (Kd = 14.4 nM). Scatchard plot analysis shows siRNA mediated suppression of AdipoR1 decreases globular adiponectin trimer binding without affecting full-length adiponectin trimer binding and vice versa. T-cadherin, AdipoR1 and AdipoR2 do not bind to C1q, a structural homologue of adiponectin that attaches to immunoglobulin for complement fixation [22, 27].
5. A shield against lipotoxicity
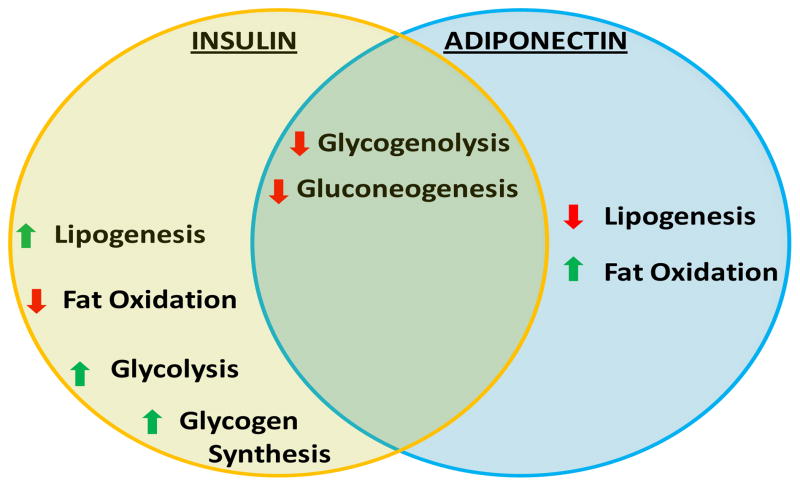
Adiponectin is not an “insulin mimetic” (Figure 2). Increasing circulating levels of insulin to compensate for the loss of adiponectin signaling in T1D and T2D promotes lipid storage which causes an even greater need for insulin. The detrimental effects of high insulin and low adiponectin signaling in humans can be seen in fatty liver and cardiovascular disease [19, 30]. The development of therapies that restore adiponectin signaling in T1D and T2D provides a way to avoid lipotoxicity.
Figure 2. Similarities and Differences between Adiponectin and Insulin Effects in the Liver.
Adiponectin and insulin reduce circulating lipids by different mechanisms. Insulin stimulation of lipogenesis in the liver converts excess glucose into fatty acids that are incorporated into triglyceride molecules that are packed in lipoprotein particles and secreted. Adiponectin increases fatty acid and triglyceride clearance by stimulating fatty acid oxidation in the liver [12].
Adiponectin lowers intracellular lipid content by two mechanisms. Adiponectin inhibition of liver glucose production lowers circulating levels of insulin which decreases insulin mediated lipogenesis and insulin mediated inhibition of fatty acid (FA) oxidation (Figure 2). Adiponectin also stimulates FA oxidation directly. The half-maximal doses for FA oxidation through AdipoR1 and AdipoR2 in C2C12 myocytes are 0.5 nM and 6 nM, respectively [27]. Studies in mice and human hepatoma (HepG2) cells suggest that adiponectin does not affect liver triacylglycerol (TAG) secretion [31].
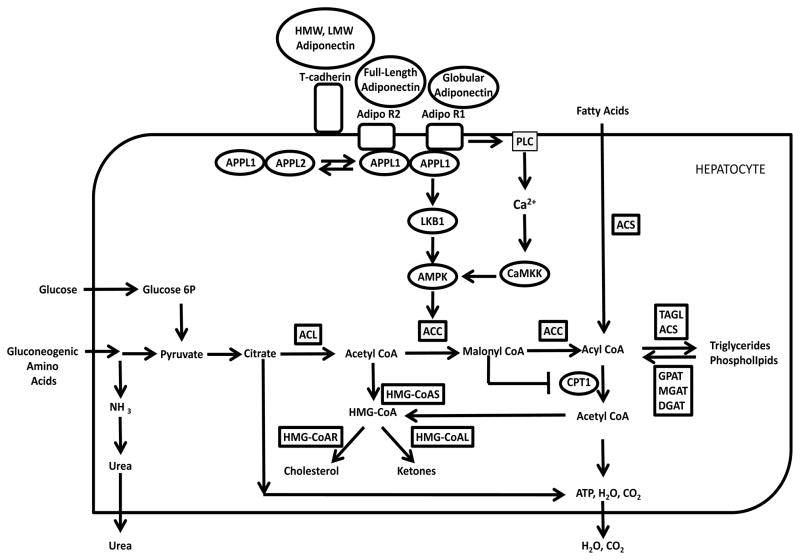
Acute exposure to HMW and LMW adiponectin activates AMP-activated kinase (AMPK) in rat hepatoma McArdle 7777 cells [32]. AMPK is a serine/threonine kinase that inhibits acetyl CoA carboxylase (ACC), a rate limiting enzyme in de novo lipogenesis [33]. AMPK suppression of ACC lowers malonyl-CoA production thereby increasing the oxidation of long chain FAs and circumventing insulin mediated lipid synthesis (Figure 3). Adiponectin activates AMPK through two independent pathways involving liver kinase B1 (LKB1) and Ca2+/calmodulin-dependent protein kinase kinase (CaMKK).
Figure 3. Adiponectin Regulation of Lipid Metabolism.
Adiponectin activation of AMPK by Ca2+ dependent and Ca2+ independent pathways, involving LKB1 and CaMKK, increases FA oxidation decreasing intracellular lipid stores and insulin resistance.
LKB1 is a serine/threonine protein kinase that activates AMPK upon translocating to the cytosol. Adaptor protein, phosphotyrosine interaction, PH domain and leucine zipper containing 1 (APPL1) is a 100 kDa endosomal protein expressed in mouse hepatocytes and other cells that binds to the N-terminal domains of AdipoR1 and AdipoR2 [34]. Yeast two-hybrid screens using a human fetal brain cDNA library show the phosphotyrosine binding (PTB) domain on the C-terminal end of APPL1 (aa 455–693) interacts with the intracellular N-terminal domains of AdipoR1 (aa 4–136) and AdipoR2 (aa 4–142) [28]. APPL1:APPL1 homodimerization is required for AdipoR1 and AdipoR2 binding [35]. In muscle, adiponectin signaling is suppressed by APPL2, an APPL1 homologue that forms an APPL1:APPL2 heterodimer. As such, increased APPL2 expression blocks receptor binding.
CaMKK is an alternate upstream kinase of AMPK that shares significant sequence and structural homology with LKB1 [36]. Both purified HMW adiponectin and recombinant globular adiponectin trimers activate CaMKK [37–39]. AdipoR1 mediated Ca2+ release in C2C12 myotubes activates CaMKK [38, 39]. Intracellular Ca2+ release involves phospholipase C (PLC) production of inositol triphosphate (IP3). Adiponectin receptor mediated activation of PLC is independent of APPL1, but may involve G-proteins used by GPCRs. Besides APPL1, other proteins can bind to the intracellular domain of AdipoR1, including endoplasmic reticulum protein 46 (ERp46), activated protein kinase C1 (RACK1) and protein kinase CK2β subunit (CK2β) [40].
Adiponectin does not stimulate FA oxidation by increasing intracellular AMP concentrations or diacylglycerol (DAG) levels in the plasma membrane. While causing a transient change in adenosine nucleotide levels, the energy status is rapidly restored by the rise in FA oxidation and the drop in lipogenesis and gluconeogenesis, a process referred to as substrate switching [41]. Adrenergic hormones also stimulate lipolysis and FA oxidation. However, adiponectin does not affect membrane DAG content, a second messenger in G-protein coupled receptor signaling and activator of protein kinase C (PKC), in hepatocytes and liver samples from leptin deficient (ob/ob) or high fat diet (HFD) induced obese mice.
6. Adiponectin mediated ceramidase activity
In addition to the accumulation of intracellular lipid droplets, lipotoxicity can be linked to the abundance of specific lipids. Ceramides are bioactive sphingolipids produced by the liver that interfere with insulin signaling. Insulin activation of phosphatidylinositol-3 kinase (PI3K) causes a transient increase of phosphatidylinositol-3,4,5-phosphate (PIP3) in cell membranes that binds to Akt, also known as protein kinase B (PKB). Ceramide activation of PKCζ interferes with PIP3 binding to Akt/PKB in L6 muscle cells [42]. Ceramide also impairs insulin signaling by PP2A and PKC epsilon (PKCε) activation in human embryonic kidney 293 cells (HEK 293) and cancer cells [43, 44]. In contrast, the metabolism of ceramides into phosphorylated sphingoid bases, such as sphingosine-1-phosphate (S1P), reduces insulin resistance [45–47].
Adiponectin lowers liver ceramide content [48, 49]. In agreement with euglycemic clamp results in other mice, adiponectin infusion in ob/ob mice lowers liver ceramide content and glucose production concurrently [11–14]. Notably, it has no effect on glucose disposal. Adiponectin decreases all ceramide and dihydroceramide species regardless of saturation or acyl chain length [14]. It stimulates deacylation of ceramides at neutral pH in a dose-dependent manner producing sphingosine, S1P and dihydrosphingosine-1-phosphate.
AdipoR1 and AdipoR2 belong to the family of progesterone/adiponectin/adipoQ receptors (PAQR) that stimulate intracellular ceramidase activity [50]. Both contain a series of histidine residues that are conserved among ceramidases. Substituting these histidines for arginines lowers the ceramidase activity of AdipoR1 and AdipoR2 [14]. Adenoviral vectors that double liver AdipoR1 and AdipoR2 expression increase ceramidase activity, lowering the ceramide content of the liver while improving insulin sensitivity in HFD-induced insulin resistant mice [14].
Mouse embryonic fibroblasts (MEFs) derived from fetal livers cannot produce glucose, but they demonstrate the synergy between T-cadherin, AdipoR1 and AdipoR2. HMW and LMW adiponectin triggered increases in ceramidase activity are blocked in AdipoR1/AdipoR2 −/− (double-knockout) MEFs [14]. Adiponectin mediated increases in ceramidase activity may lower hepatic glucose production by altering the lipid composition of the plasma membrane. The ceramide content of lipid rafts is higher in AdipoR1 and AdipoR2 deficient MEFs [14].
Catabolic conditions stimulate liver glucose production by cell autonomous mechanisms retained in tissue culture. Nutrient deficient media induce a marked increase in hepatocyte glucose production before triggering apoptosis. However, the addition of HMW and LMW adiponectin increases MEF survival [14]. S1P, a potent stimulator of cell growth, rescues AdipoR1 and AdipoR2 deficient MEFs from cell death [45, 51]. Despite its antiapoptotic effects, adiponectin is associated with tumor suppression in the liver and other tissues [23, 52].
7. Suppression of gluconeogenic enzymes
Tracer studies using deuterated water show that adiponectin lowers glucose production in rat hepatoma (McArdle 7777) cells by suppressing both glycogenolysis and gluconeogenesis [32]. Suppression of glucose-6-phosphatase (G6Pase) and phosphoenolpyruvate carboxy kinase (PEPCK) inhibits glycogenolysis and gluconeogenesis. HMW, LMW and full-length adiponectin trimer lower liver G6Pase and PEPCK mRNA expression in lab rodents [11, 29, 53–55].
Adiponectin inhibition of glucose production can be blocked by (a) the expression of a dominant negative AMPK mutant in hepatoma cells and (b) gene ablation of AMPK in mice [29, 32, 56]. How is it possible for AMPK to exert such a dominant effect on plasma glucose when the reduction of intracellular lipids by itself is insufficient in the clinical treatment of diabetes [18]? The answer is that, in addition to inhibiting ACC and decreasing intracellular lipid stores, AMPK lowers liver G6Pase and PEPCK mRNA expression.
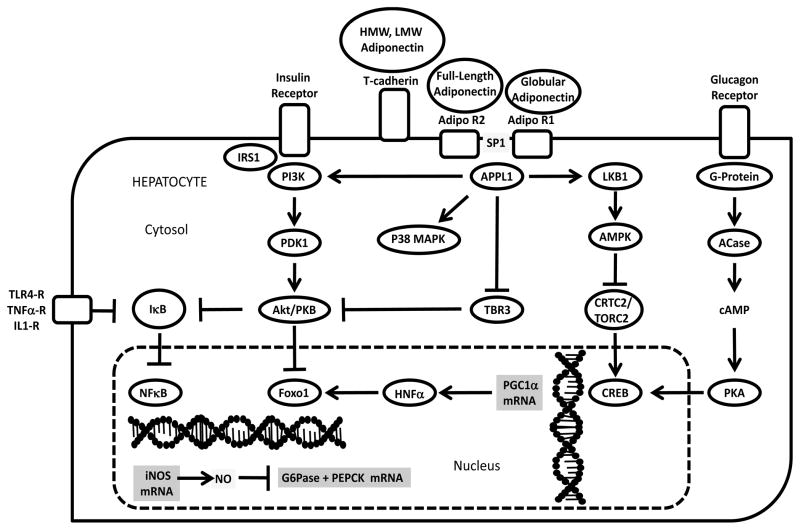
Gluconeogenic hormones such as glucagon stimulate G6Pase and PEPCK mRNA expression by activating the cAMP-responsive element-binding (CREB) (Figure 4). CREB stimulation of G6Pase and PEPCK mRNA expression depends on binding to the CREB-regulated transcription coactivator (CRTC2), also called transducer of regulated cAMP response element–binding protein 2 (TORC2), which drives the expression of PPARγ cofactor-1 alpha (PGC1α). PGC1α binds to the nuclear hormone receptors hepatic nuclear factor-4 α (HNF4α) and the forkhead family member Foxo1 driving G6Pase and PEPCK mRNA expression [57]. Adenoviral small hairpin RNA (shRNA) for TORC2 lowers glucagon-stimulated PGC-1α expression [58]. Glucagon stimulation dephosphorylates TORC2 allowing TORC2 translocation to the nucleus where it enhances CREB-dependent transcription of PGC1α, G6Pase and PEPCK mRNA expression.
Figure 4. Adiponectin Regulation of G6Pase and PEPCK Expression in Hepatocytes in Relation to Insulin Receptor and Glucagon Receptor Action.
The catalytic activity of G6Pase and PEPCK is regulated at the level of gene expression. Adiponectin regulation of PGC1α and iNOS mRNA can play a role the suppression of G6Pase and PEPCK mRNA.
Adiponectin activation of AMPK blocks G6Pase and PEPCK mRNA expression by promoting TORC2 phosphorylation and blocking its translocation to the nucleus (Figure 4). Liver specific knockout of LKB1 through adenovirus bearing CMV-Cre causes TORC2 dephorphorylation and increased PGC1α, PEPCK and G6Pase mRNA expression [58, 59]. AMPK mediated induction of the immediate early transcription factor Early Growth Response 1 (EGR1) and Dual Specificity Phosphatase (DUSP4) also lowers G6Pase and PEPCK expression and glucose production in Fao rat hepatoma cell lines [60]. Other relevant AMPK targets in hepatocytes include glycogen synthase, insulin response substrate 1 and -2 (IRS-1 and IRS-2) [61–63].
Adiponectin mediated suppression of G6Pase and PEPCK mRNA expression in mouse hepatocytes may also occur independently of LKB1, AMPK and TORC2 (Figure 4). Adiponectin mediated decreases in glucogenic gene expression, hepatic glucose production and plasma glucose is partly preserved after liver LKB1 deletion by viral expression of CRE recombinase [54]. LKB1 and AMPK null hepatocytes exhibit a lack of correlation between TORC2 electrophoretic mobility and adiponectin suppression of PEPCK and G6Pase expression. Adiponectin and AMPK do not suppress glucagon and cAMP induced PKA phosphorylation of target proteins. However, hepatocytes from TORC2-null mice demonstrate robust adiponectin-induced repression of PGC1α, a target gene of protein kinase A (PKA).
Adiponectin mediated decreases in G6Pase and PEPCK expression can be triggered independent of AMPK through convergence of the adiponectin and insulin signaling pathways through APPL1. Insulin lowers PEPCK and G6Pase expression through PI3K (Figure 4) [64]. PI3K production of PIP3 promotes Akt/PKB translocation to the nucleus wherein Akt/PKB phosphorylates Foxo1, a member of the Forkhead/winged helix family of transcription factors [65]. Tribble-3 (TRB3) prevents Akt/PKB translocation to the plasma membrane. [66, 67]. APPL1 interferes with TRB3 binding increasing insulin-stimulated Akt/PKB phosphorylation [68]. APPL1 reduces Akt/PKB-TRB3 binding in the liver of leptin receptor deficient (db/db) mice. APPL1 overexpression also increases the phosphorylation of mitogen-activated protein kinase (p38 MAPK) in mouse hepatocytes, but it does not affect every aspect of insulin signaling. APPL1 does not affect insulin stimulated MAP kinase (p42/44 Erk) phosphorylation.
NFκB can also inhibit glucose production by stimulating the production of nitric oxide NO (Figure 4) [69]. Adiponectin stimulation of APPL1 prevents obesity-induced vascular insulin resistance and endothelial dysfunction by modulating the endothelial production of nitric oxide (NO) [70]. In C2C12 myocytes, adiponectin phosphorylates IκB which activates NFκB, a heterodimer of two DNA-binding subunits, p50 and p65 [71]. IκB retains NFκB in the cytoplasm under basal conditions. IκB phosphorylation allows the translocation of NFκB to the nucleus where it can regulate gene expression. However, NFκB also increases NO production in hepatocytes by stimulating inducible NO synthase (iNOS) expression [72]. NFκB inhibits glucocorticoid and glucagon induction of glucose production [73]. TLR4, IL1-R and TNFα–R suppress the gene expression of G6Pase and PEPCK through NFκB [74, 75]. Adiponectin activation of NFκB in macrophages occurs independent of AdipoR1 and AdipoR2 [63]. NFκB targeting must be hepatocyte specific as the liver’s resident macrophages, Kupffer cells, could elicit an innate immune response [76].
8. Suppression of gluconeogenic substrate availability
Besides the regulation of rate limiting enzymes, such as G6Pase and PEPCK, glucose production can be suppressed by decreasing the availability of energy, reducing equivalents and substrates [77–79]. Adiponectin stimulation of FA oxidation generates energy and reducing equivalents making the reduction of substrate availability a potential target for the inhibition of glucose production (Figure 5).
Figure 5. Rate Limiting Enzymes and Biochemical Substrates needed for Liver Glucose Production via Gluconeogenesis and Glycogenolysis.
Liver cell glucose production can be lowered by decreasing the catalytic activity of pyruvate carboxylase (PCase), PEPCK, fructose-1,6-bisphosphatase (F16PPase) and glucose-6-phosphatase (G6Pase) and increasing the catalytic activity of pyruvate dehydrogenease (PDH). Liver cells cannot synthesize or metabolize branched chain amino acids (BCAAs). Adiponectin upregulation of SOGA inhibits autophagy lowering the availability of gluconeogenic amino acids for the synthesis of glucose.
The hydrolysis of peptide bonds through proteasomal and autophagic mechanisms is associated with the presumed elevation of gluconeogenic amino acid availability and the appearance of hyperglycemia [80, 81]. Food withdrawal, streptozotocin induced diabetes, glucagon, epinephrine and glucocorticoids increase autophagy in the liver [82–85]. Adiponectin mediated increases in ceramidase activity may contribute to an inhibition of autophagy; however, the possibility that adiponectin lowers autophagy through AMPK is ruled out as AMPK stimulation of Ulk1 and AMPK inhibition of the mammalian target of rapamycin (mTOR) increase autophagy [86–88].
The search for an inhibitor of autophagy in the adiponectin signaling pathway led to the discovery of a previously unknown protein called the Suppressor of Glucose from Autophagy (SOGA) (Figure 5) [89]. Proteomic analysis shows that HMW and LMW adiponectin upregulate SOGA in hepatoma and hepatocyte cultures. siRNA knockdown of SOGA stimulates autophagy and proteolysis in hepatocytes blocking adiponectin inhibition of glucose production. AICAR, an AMP analogue that stimulates AMPK and glycogenolysis, lowers SOGA in primary hepatocytes [90, 91]. LY294002, which blocks the ATP binding site in PI3K, also lowers SOGA [92].
The elevation of protein turnover suggests that substrate availability is linked to the increase in gluconeogenesis and glucose production in T2D [93, 94]. As such, the loss of adiponectin signaling could lower SOGA in the liver and muscle contributing to the appearance of hyperglycemia. Proteolytic cleavage of SOGA yields a C-terminal fragment that is secreted into the extracellular space and further processed in the circulation (Figure 6) [89]. The circulating SOGA fragment provides a surrogate marker for changes in the intracellular levels of SOGA. TZD treatment and calorie restriction, interventions that increase circulating adiponectin and restore glucose homeostasis, raise SOGA and lower glucose in ob/ob and wild-type mice.
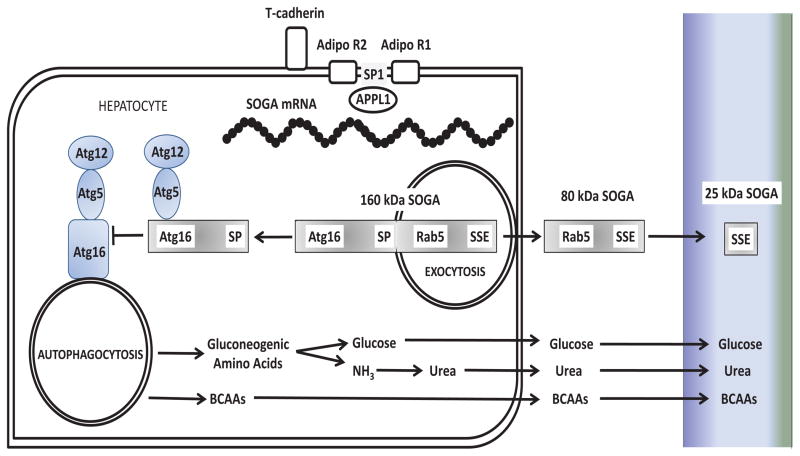
Figure 6. Proteolytic Processing of SOGA and Potential Mechanism of Action.
Full-length SOGA contains Atg16 and Rab5-binding motifs, an internal signal peptide (SP) and a C-terminal species specific antigenic epitope (SSE). Autophagy involves the encapsulation of protein in membrane bound vacuoles that fuse with lysosomes and the release of free amino acids. This model shows (a) the proteolytic processing of full-length SOGA at the internal signal site, (b) the N-terminal fragment of SOGA interfering with the formation of the Atg12-Atg5-Atg16 complex required for the initiation of autophagy, (c) the secretion of the C-terminal fragment of SOGA and (d) further processing of the C-terminal fragment to produce the circulating 25 kDa C-terminal fragment of SOGA.
9. Clinical Correlation: Low Adiponectin Signaling and Type 1 Diabetes
The marked increase of circulating adiponectin with little benefit in people with T1D indicates a breakdown of the adiponectin signaling pathway [95]. In nonobese diabetic (NOD) mice, an autoimmune model of T1D, the loss of adiponectin signaling in the liver is evident from the reduction of SOGA [89]. Insulin injection eliminates hyperglycemia in NOD mice without correcting the deficiency of SOGA. TZD drugs prescribed for the treatment of insulin resistance in T1D may work by stimulating the production of SOGA through adiponectin. However, considering the breakdown of the adiponectin signaling pathway in T1D, the development of medications that stimulate the production of SOGA directly could restore the metabolic balance, diminish the insulin requirement and improve clinical outcomes.
10. Restoring the activity of the adiponectin signaling pathway in the liver
Adiponectin is a hormone that slows down the liver’s production of glucose. The loss of adiponectin signaling in the liver contributes to the elevation of glucose in T1D and T2D. Insulin does not fully compensate for the loss of adiponectin signaling in T1D and T2D. The adiponectin signaling pathway within liver cells provides molecular and phenotypic targets for the development of drugs that can restore the body to the nondiabetic state.
The loss of adiponectin signaling in T1D is due to a breakdown of the adiponectin signaling pathway. The loss of adiponectin signaling in T2D is due to low circulating adiponectin. Chronic calorie restriction and TZD drugs raise circulating levels of adiponectin. The elevation of circulating adiponectin is beneficial in the treatment of T2D, when the adiponectin signaling pathway is intact. The development of “adiponectin sensitizers”, drugs that activate the intermediates in the adiponectin signaling pathway directly, is necessary to restore adiponectin signaling in T1D.
Acknowledgments
Support for this review was provided from the National Institutes of Health to Dr. Combs (Grant DK075573: The Effects of Adiponectin on Liver Insulin Resistance) and the Canadian Institutes of Health Research to Dr. Marliss (Grant MOP-62889: Mechanisms of Insulin Resistance of Protein Metabolism in Human Obesity).
References
- 1.Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF. A novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem. 1995;270(45):26746–26749. doi: 10.1074/jbc.270.45.26746. [DOI] [PubMed] [Google Scholar]
- 2.Hu E, Liang P, Spiegelman BM. AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem. 1996;271(18):10697–10703. doi: 10.1074/jbc.271.18.10697. [DOI] [PubMed] [Google Scholar]
- 3.Matsuzawa Y, Funahashi T, Nakamura T. Molecular mechanism of metabolic syndrome X: contribution of adipocytokines adipocyte-derived bioactive substances. Ann N Y Acad Sci. 1999;892:146–154. doi: 10.1111/j.1749-6632.1999.tb07793.x. [DOI] [PubMed] [Google Scholar]
- 4.Berg AH, Combs TP, Scherer PE. ACRP30/adiponectin: an adipokine regulating glucose and lipid metabolism. Trends Endocrinol Metab. 2002;13(2):84–89. doi: 10.1016/s1043-2760(01)00524-0. [DOI] [PubMed] [Google Scholar]
- 5.Haugen F, Drevon CA. Activation of nuclear factor kappaB by high molecular weight and globular adiponectin. Endocrinol. 2007;148(11):5478–5486. doi: 10.1210/en.2007-0370. [DOI] [PubMed] [Google Scholar]
- 6.Schraw T, Wang ZV, Halberg N, Hawkins M, Scherer PE. Plasma adiponectin complexes have distinct biochemical characteristics. Endocrinol. 2008;149(5):2270–2282. doi: 10.1210/en.2007-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fruebis J, Tsao TS, Javorschi S, Ebbets-Reed D, Erickson MR, Yen FT, Bihain BE, Lodish HF. Proteolytic cleavage product of 30-kDa adipocyte complement-related protein increases fatty acid oxidation in muscle and causes weight loss in mice. Proc Natl Acad Sci U S A. 2001;98 (4):2005–2010. doi: 10.1073/pnas.041591798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pajvani UB, Du X, Combs TP, Berg AH, Rajala MW, Schulthess T, Engel J, Brownlee M, Scherer PE. Structure-function studies of the adipocyte-secreted hormone Acrp30/adiponectin. Implications fpr metabolic regulation and bioactivity. J Biol Chem. 2003;278(11):9073–9085. doi: 10.1074/jbc.M207198200. [DOI] [PubMed] [Google Scholar]
- 9.Berg AH, Combs TP, Du X, Brownlee M, Scherer PE. The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med. 2001;7(8):947–953. doi: 10.1038/90992. [DOI] [PubMed] [Google Scholar]
- 10.Katz EB, Stenbit AE, Hatton K, DePinho R, Cahrron MJ. Cardiac and adipose tissue abnormalilties but not diabetes in mice deficient in GLUT4. Nature. 1995;377:151–155. doi: 10.1038/377151a0. [DOI] [PubMed] [Google Scholar]
- 11.Combs TP, Berg AH, Obici S, Scherer PE, Rossetti L. Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J Clin Invest. 2001;108(12):1875–1881. doi: 10.1172/JCI14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Combs TP, Pajvani UB, Berg AH, Lin Y, Jelicks LA, Laplante M, Nawrocki AR, Rajala MW, Parlow AF, Cheeseboro L, et al. A transgenic mouse with a deletion in the collagenous domain of adiponectin displays elevated circulating adiponectin and improved insulin sensitivity. Endocrinology. 2004;145(1):367–383. doi: 10.1210/en.2003-1068. [DOI] [PubMed] [Google Scholar]
- 13.Nawrocki AR, Rajala MW, Tomas E, Pajvani UB, Saha AK, Trumbauer ME, Pang Z, Chen AS, Ruderman NB, Chen H, et al. Mice lacking adiponectin show decreased hepatic insulin sensitivity and reduced responsiveness to peroxisome proliferator-activated receptor gamma agonists. J Biol Chem. 2006;281(5):2654–2660. doi: 10.1074/jbc.M505311200. [DOI] [PubMed] [Google Scholar]
- 14.Holland WL, Miller RA, Wang ZV, Sun K, Barth BM, Bui HH, Davis KE, Bikman BT, Halberg N, Rutkowski JM, et al. Receptor-mediated activation of ceramidase activity inititates the pleiotropic actions of adiponectin. Nat Med. 2011;17(1):55–65. doi: 10.1038/nm.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Xu A, Knight C, Xu LY, Cooper GJ. Hydroxylation and glycosylation of the four conserved lysine residues in the collagenous domain of adiponectin. Potential role in the modulation of its insulin-sensitizing activity. J Biol Chem. 2002;277(22):19521–19529. doi: 10.1074/jbc.M200601200. [DOI] [PubMed] [Google Scholar]
- 16.Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, Hotta K, Shimomura I, Nakamura T, Miyaoka K, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999;257(1):79–83. doi: 10.1006/bbrc.1999.0255. [DOI] [PubMed] [Google Scholar]
- 17.Mynarcick DC, Combs TP, McNurlan MA, Scherer PE, Komaroff E, Gelato MC. Adiponectin and leptin levels in HIV-infected subjects with insulin resistance and body fat redistribution. JAIDS. 2002;31(5):514–520. doi: 10.1097/00126334-200212150-00009. [DOI] [PubMed] [Google Scholar]
- 18.Combs TP, Wagner JA, Berger J, Doebber T, Wang WJ, Zhang BB, Tanen M, Berg AH, O’Rahilly S, Savage DB, et al. Induction of adipocyte complement-related protein of 30 kilodaltons by PPARgamma agonists: a potential mechanism of insulin sensitization. Endocrinology. 2002;143(3):998–1007. doi: 10.1210/endo.143.3.8662. [DOI] [PubMed] [Google Scholar]
- 19.Brooks NL, Moore KS, Clark RD, Perfetti MT, Trent CM, Combs TP. Do low levels of circulating adiponectin represent a biomarker or just another risk factor for the metabolic syndrome? Diabetes Obes Metab. 2007;9(3):246–58. doi: 10.1111/j.1463-1326.2006.00596.x. [DOI] [PubMed] [Google Scholar]
- 20.Ahmadian M, Suh JM, Hah N, Liddle C, Atkins AR, Downes M, Evans AR. PPARgamma signaling and metabolism: the good the bad and the future. Nature Medicine. 2013;99:557–566. doi: 10.1038/nm.3159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffstedt J, Arvidsson E, Sjolin E, Wahlen K, Arner P. Adipose tissue adiponectin production and adiponectin seum concentration in human obesity and insulin resistance. J Clin IEndocrinol Metab. 2004;89(3):1391–1396. doi: 10.1210/jc.2003-031458. [DOI] [PubMed] [Google Scholar]
- 22.Hug C, Wang J, Ahmad NS, Bogan JS, Tsao TS, Lodish HF. T-cadherin is a receptor for hexameric and high-molecular-weight forms of Acrp30/adiponectin. Proc Natl Acad Sci. 2004;101(28):10, 308–313. doi: 10.1073/pnas.0403382101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan CY, Lee JM, Chan PC, Ng IO. Genetic and epigenetic inactivation of T-cadherin in human hepatocellular carcinoma cells. Cancer Cell Biol. 2008;123(5):1043–1052. doi: 10.1002/ijc.23634. [DOI] [PubMed] [Google Scholar]
- 24.Vestal DJ, Ranscht B. Glycosyl phosphatidylinositol-anchored T-cadherin mediates calcium-dependent, homophilic cell adhesion. J Cell Biol. 1992;119(2):451–461. doi: 10.1083/jcb.119.2.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Denzel MS, Scimia M, Zumstein PM, Walsh K, Ruiz-Lozano P, Ranscht B. T-cadherin is critical for adiponectin-mediated cardioprotection in mice. J Clin Invest. 2010;120(12):4342–4352. doi: 10.1172/JCI43464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Philippova MP, Bochkov VN, Stambolsky DV, Tkachuk VA, Resink TJ. T-cadherin and signal-transducing moleculaes co-localize in caveolin-rich membrane domains of vascular smooth muscle cells. FEBS Letters. 1998;429:207–210. doi: 10.1016/s0014-5793(98)00598-5. [DOI] [PubMed] [Google Scholar]
- 27.Yamauchi T, Kamon J, Ito Y, Tsuchida A, Yokomizo T, Kita S, Sugiyama T, Miyagishi M, Hara K, Tsunoda M, et al. Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature. 2003;423(6941):762–769. doi: 10.1038/nature01705. [DOI] [PubMed] [Google Scholar]
- 28.Mao X, Kikani CK, Riojas RA, Langlais P, Wang L, Ramos FJ, Fang Q, Christ-Roberts CY, Hong JY, Kim RY, et al. APPL1 binds to adiponectin receptors and mediates adiponectin signalling and function. Nat Cell Biol. 2006;8(5):516–523. doi: 10.1038/ncb1404. [DOI] [PubMed] [Google Scholar]
- 29.Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, Yamashita S, Noda M, Kita S, Ueki K, et al. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med. 2002;8(11):1288–1295. doi: 10.1038/nm788. [DOI] [PubMed] [Google Scholar]
- 30.Pagano C, Soardo G, Esposito W, Fallo F, Basan L, Donnini D, Federspil G, Sechi LA, Vettor R. Plasma adiponectin is decreased in nonalcoholic fatty liver disease. Eur J Endocrinol. 2005;152(1):113–118. doi: 10.1530/eje.1.01821. [DOI] [PubMed] [Google Scholar]
- 31.Qiao L, Zou C, van der Westhuyzen DR, Shao J. Adiponectin reduces plasma triglyceride by increasing VLDL triglyceride catabolism. Diabetes. 2008;57(7):1824–1833. doi: 10.2337/db07-0435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brooks NL, Trent CM, Raetzsch CF, Flurkey K, Boysen G, Perfetti MT, Jeong YC, Klebanov S, Patel KB, Khodush VR, et al. Low utilization of circulating glucose after food withdrawal in Snell dwarf mice. J Biol Chem. 2007;282(48):35069–35077. doi: 10.1074/jbc.M700484200. [DOI] [PubMed] [Google Scholar]
- 33.Towler MC, Hardie DG. AMP-activated protein kinase in metabolic control and insulin signaling. Circ Res. 2007;100(3):328–341. doi: 10.1161/01.RES.0000256090.42690.05. [DOI] [PubMed] [Google Scholar]
- 34.Deepa SS, Dong LQ. APPL1: role in adiponectin signaling and beyond. Am J Physiol Endocrinol Metab. 2009;296(1):E22–36. doi: 10.1152/ajpendo.90731.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang C, Xin X, Xiang R, Ramos FJ, Liu M, Lee HJ, Chen H, Mao X, Kikani CK, Liu F, et al. Yin-Yang regulation of adiponectin signaling by APPL isoforms in muscle cells. J Biol Chem. 2009;284(46):31608–31615. doi: 10.1074/jbc.M109.010355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Woods A, Azzout-Marniche D, Foretz M, Stein SC, Lemarchand P, Ferre P, Foufelle F, Carling D. Characterization of the role of AMP-activated protein kinase in the regulation of glucose-activated gene expression using constitutively active and dominant negative forms of the kinase. Mol Cell Biol. 2000;20(18):6704–6711. doi: 10.1128/mcb.20.18.6704-6711.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hattori Y, Nakano Y, Hattori S, Tomizawa A, Inukai K, Kasai K. High molecular weight adiponectin activates AMPK and suppresses cytokine-induced NF-kappaB activation in vascular endothelial cells. FEBS Lett. 2008;582(12):1719–1724. doi: 10.1016/j.febslet.2008.04.037. [DOI] [PubMed] [Google Scholar]
- 38.Zhou L, Deepa SS, Etzler JC, Ryu J, Mao X, Fang Q, Liu DD, Torres JM, Jia W, Lechleiter JD, et al. Adiponectin activates AMP-activated protein kinase in muscle cells via APPL1/LKB1-dependent and phospholipase C/Ca2+/Ca2+/calmodulin-dependent protein kinase kinase-dependent pathways. J Biol Chem. 2009;284(33):22426–22435. doi: 10.1074/jbc.M109.028357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iwabu M, Yamauchi T, Okada-Iwabu M, Sato K, Nakagawa T, Funata M, Yamaguchi M, Namiki S, Nakayama R, Tabata M, et al. Adiponectin and AdipoR1 regulate PGC-1alpha and mitochondria by Ca(2+) and AMPK/SIRT1. Nature. 2010;464(7293):1313–1319. doi: 10.1038/nature08991. [DOI] [PubMed] [Google Scholar]
- 40.Buechler C, Wanninger J, Neumeier M. Adiponectin receptor binding proteins--recent advances in elucidating adiponectin signalling pathways. FEBS Lett. 2010;584(20):4280–4286. doi: 10.1016/j.febslet.2010.09.035. [DOI] [PubMed] [Google Scholar]
- 41.Viollet B, Andreelli F. AMP-activated protein kinase and metabolic control. Handbook of Experimetal Pharamcology. 2011;203:303–330. doi: 10.1007/978-3-642-17214-4_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Powell DJ, Hajduch E, Kular G, Hundal HS. Ceramide disables 3-phosphoinositide binding to the pleckstrin homology domain of protein kinase B (PKB)/Akt by a PKCzeta-dependent mechanism. Molecular and cellular biology. 2003;23(21):7794–7808. doi: 10.1128/MCB.23.21.7794-7808.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mukhopadhyay A, Saddoughi SA, Song P, Sultan I, Ponnusamy S, Senkal CE, Snook CF, Arnold HK, Sears RC, Hannun YA, et al. Direct interaction between the inhibitor 2 and ceramide via sphingolipid-protein binding is involved in the regulation of protein phosphatase 2A activity and signaling. FASEB journal: official publication of the Federation of American Societies for Experimental Biology. 2009;23(3):751–763. doi: 10.1096/fj.08-120550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bourbon NA, Yun J, Berkey D, Wang Y, Kester M. Inhibitory actions of ceramide upon PKC-epsilon/ERK interactions. American journal of physiology Cell physiology. 2001;280(6):C1403–1411. doi: 10.1152/ajpcell.2001.280.6.C1403. [DOI] [PubMed] [Google Scholar]
- 45.Takabe K, Paugh SW, Milstien S, Spiegel S. “Inside-out” signaling of sphingosine-1-phosphate: therapeutic targets. Pharmacol Rev. 2008;60(2):181–195. doi: 10.1124/pr.107.07113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang G, Badeanlou L, Bielawski J, Roberts AJ, Hannun YA, Samad F. Central role of ceramide biosynthesis in body weight regulation, energy metabolism, and the metabolic syndrome. Am J Physiol Endocrinol Metab. 2009;297(1):E211–224. doi: 10.1152/ajpendo.91014.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yew NS, Zhao H, Hong EG, Wu IH, Przybylska M, Siegel C, Shayman JA, Arbeeny CM, Kim JK, Jiang C, et al. Increased hepatic insulin action in diet-induced obese mice following inhibition of glucosylceramide synthase. PLoS One. 2010;5(6):e11239. doi: 10.1371/journal.pone.0011239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holland WL, Bikman BT, Wang LP, Yuguang G, Sargent KM, Bulchand S, Knotts TA, Shui G, Clegg DJ, Wenk MR, et al. Lipid-induced insulin resistance mediated by the proinflammatory receptor TLR4 requires saturated fatty acid-induced ceramide biosynthesis in mice. J Clin Invest. 2011;121(5):1858–1870. doi: 10.1172/JCI43378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lopez X, Goldfine AB, Holland WL, Gordillo R, Scherer PE. Plasma ceramides are elevated in female children and adolescents with type 2 diabetes. J Pediatr Endocrinol Metab. 2013;24 doi: 10.1515/jpem-2012-0407. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 50.Villa NY, Kupchak BR, Garitaonandia I, Smith JL, Alonso E, Alford C, Cowart LA, Hannun YA, Lyons TJ. Sphingolipids function as downstream effectors of a fungal PAQR. Mol Pharmacol. 2009;75 (4):866–875. doi: 10.1124/mol.108.049809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Holland WL, Summers SA. Sphingolipids, insulin resistance, and metabolic disease: new insights from in vivo manipulation of sphingolipid metabolism. Endocr Rev. 2008;29(4):381–402. doi: 10.1210/er.2007-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dalamaga M, Diakopoulos KN, Mantzoros CS. The role of adiponectin in cancer: a review of current evidence. Endocrine reviews. 2012;33(4):547–594. doi: 10.1210/er.2011-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shklyaev S, Aslanidi G, Tennant M, Prima V, Kohlbrenner E, Kroutov V, Campbell-Thompson M, Crawford J, Shek EW, Scarpace PJ, et al. Sustained peripheral expression of transgene adiponectin offsets the development of diet-induced obesity in rats. Proc Natl Acad Sci U S A. 2003;100(24):14217–14222. doi: 10.1073/pnas.2333912100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Miller RA, Chu Q, Le Lay J, Scherer PE, Ahima RS, Kaestner KH, Foretz M, Viollet B, Birnbaum MJ. Adiponectin suppresses gluconeogenic gene expression in mouse hepatocytes independent of LKB1-AMPK signaling. J Clin Invest. 2011;121(6):2518–2528. doi: 10.1172/JCI45942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma Y, Liu D. Hydrodynamic delivery of adiponectin and adiponectin receptor 2 gene blocks high-fat diet-induced obesity and insulin resistance. Gene Ther. 2013 doi: 10.1038/gt.2013.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Andreelli F, Foretz M, Knauf C, Cani PD, Perrin C, Iglesias MA, Pillot B, Bado A, Tronche F, Mithieux G, et al. Liver adenosine monophosphate-activated kinase-alpha2 catalytic subunit is a key target for the control of hepatic glucose production by adiponectin and leptin but not insulin. Endocrinology. 2006;147(5):2432–2441. doi: 10.1210/en.2005-0898. [DOI] [PubMed] [Google Scholar]
- 57.Yoon JC, Puigserver P, Chen G, Donovan J, Wu Z, Rhee J, Adelmant G, Stafford J, Kahn CR, Granner DK, et al. Control of hepatic gluconeogenesis through the transcriptional coactivator PGC-1. Nature. 2001;413(6852):131–138. doi: 10.1038/35093050. [DOI] [PubMed] [Google Scholar]
- 58.Shaw RJ, Lamia KA, Vasquez D, Koo SH, Bardeesy N, Depinho RA, Montminy M, Cantley LC. The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Science. 2005;310(5754):1642–1646. doi: 10.1126/science.1120781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Koo SH, Flechner L, Qi L, Zhang X, Screaton RA, Jeffries S, Hedrick S, Xu W, Boussouar F, Brindle P, et al. The CREB coactivator TORC2 is a key regulator of fasting glucose metabolism. Nature. 2005;437(7062):1109–1111. doi: 10.1038/nature03967. [DOI] [PubMed] [Google Scholar]
- 60.Berasi SP, Huard C, Li D, Shih HH, Sun Y, Zhong W, Paulsen JE, Brown EL, Gimeno RE, Martinez RV. Inhibition of gluconeogenesis through transcriptional activation of EGR1 and DUSP4 by AMP-activated kinase. J Biol Chem. 2006;281(37):27167–27177. doi: 10.1074/jbc.M602416200. [DOI] [PubMed] [Google Scholar]
- 61.Jorgensen SB, Nielsen JN, Birk JB, Olsen GS, Viollet B, Andreelli F, Schjerling P, Vaulont S, Hardie DG, Hansen BF, et al. The alpha2–5′AMP-activated protein kinase is a site 2 glycogen synthase kinase in skeletal muscle and is responsive to glucose loading. Diabetes. 2004;53(12):3074–3081. doi: 10.2337/diabetes.53.12.3074. [DOI] [PubMed] [Google Scholar]
- 62.Jakobsen SN, Hardie DG, Morrice N, Tornqvist HE. 5′-AMP-activated protein kinase phosphorylates IRS-1 on Ser-789 in mouse C2C12 myotubes in response to 5-aminoimidazole-4-carboxamide riboside. J Biol Chem. 2001;276(50):46912–46916. doi: 10.1074/jbc.C100483200. [DOI] [PubMed] [Google Scholar]
- 63.Awazawa M, Ueki K, Inabe K, Yamauchi T, Kubota N, Kaneko K, Kobayashi M, Iwane A, Sasako T, Okazaki Y, et al. Adiponectin enhances insulin sensitivity by increasing hepatic IRS-2 expression via a macrophage-derived IL-6-dependent pathway. Cell metabolism. 2011;13(4):401–412. doi: 10.1016/j.cmet.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 64.Dickens M, Svitek CA, Culbert AA, O’Brien RM, Tavare JM. Central role for phosphatidylinositide 3-kinase in the repression of glucose-6-phosphatase gene transcription by insulin. J Biol Chem. 1998;273(32):20144–20149. doi: 10.1074/jbc.273.32.20144. [DOI] [PubMed] [Google Scholar]
- 65.Nakae J, Kitamura T, Silver DL, Accili D. The forkhead transcription factor Foxo1 (Fkhr) confers insulin sensitivity onto glucose-6-phosphatase expression. J Clin Invest. 2001;108(9):1359–1367. doi: 10.1172/JCI12876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Du K, Herzig S, Kulkarni RN, Montminy M. TRB3: a tribbles homolog that inhibits Akt/PKB activation by insulin in liver. Science. 2003;300(5625):1574–1577. doi: 10.1126/science.1079817. [DOI] [PubMed] [Google Scholar]
- 67.Oberkofler H, Pfeifenberger A, Soyal S, Felder T, Hahne P, Miller K, Krempler F, Patsch W. Aberrant hepatic TRIB3 gene expression in insulin-resistant obese humans. Diabetologia. 2010;53 (9):1971–1975. doi: 10.1007/s00125-010-1772-2. [DOI] [PubMed] [Google Scholar]
- 68.Cheng KK, Iglesias MA, Lam KS, Wang Y, Sweeney G, Zhu W, Vanhoutte PM, Kraegen EW, Xu A. APPL1 potentiates insulin-mediated inhibition of hepatic glucose production and alleviates diabetes via Akt activation in mice. Cell Metab. 2009;9(5):417–427. doi: 10.1016/j.cmet.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 69.Horton RA, Ceppi ED, Knowles RG, Titheradge MA. Inhibition of hepatic gluconeogenesis by nitric oxide: a comparison with endotoxic shock. Biochem J. 1994;299 (Pt 3):735–739. doi: 10.1042/bj2990735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang Y, Cheng KK, Lam KS, Wu D, Wang Y, Huang Y, Vanhoutte PM, Sweeney G, Li Y, Xu A. APPL1 counteracts obesity-induced vascular insulin resistance and endothelial dysfunction by modulating the endothelial production of nitric oxide and endothelin-1 in mice. Diabetes. 2011;60 (11):3044–3054. doi: 10.2337/db11-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tsao TS, Murrey HE, Hug C, Lee DH, Lodish HF. Oligomerization state-dependent activation of NF-kappa B signaling pathway by adipocyte complement-related protein of 30 kDa (Acrp30) The Journal of biological chemistry. 2002;277(33):29359–29362. doi: 10.1074/jbc.C200312200. [DOI] [PubMed] [Google Scholar]
- 72.Geller DA, Nussler AK, Di Silvio M, Lowenstein CJ, Shapiro RA, Wang SC, Simmons RL, Billiar TR. Cytokines, endotoxin, and glucocorticoids regulate the expression of inducible nitric oxide synthase in hepatocytes. Proc Natl Acad Sci U S A. 1993;90(2):522–526. doi: 10.1073/pnas.90.2.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Waltner-Law M, Daniels MC, Sutherland C, Granner DK. NF-kappa B inhibits glucocorticoid and cAMP-mediated expression of the phosphoenolpyruvate carboxykinase gene. J Biol Chem. 2000;275(41):31847–31856. doi: 10.1074/jbc.M003656200. [DOI] [PubMed] [Google Scholar]
- 74.Grempler R, Kienitz A, Werner T, Meyer M, Barthel A, Ailett F, Sutherland C, Walther R, Schmoll D. Tumour necrosis factor alpha decreases glucose-6-phosphatase gene expression by activation of nuclear factor kappaB. Biochem J. 2004;382(Pt 2):471–479. doi: 10.1042/BJ20040160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Raetzsch CF, Brooks NL, Alderman JM, Moore KS, Hosick PA, Klebanov S, Akira S, Bear JE, Baldwin AS, Mackman N, et al. Lipopolysaccharide inhibition of glucose production through the Toll-like receptor-4, myeloid differentiation factor 88, and nuclear factor kappa b pathway. Hepatology. 2009;50(2):592–600. doi: 10.1002/hep.22999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Thakur V, Pritchard MT, McMullen MR, Nagy LE. Adiponectin normalizes LPS-stimulated TNF-alpha production by rat Kupffer cells after chronic ethanol feeding. Am J Physiol Gastrointest Liver Physiol. 2006;290(5):G998–1007. doi: 10.1152/ajpgi.00553.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mittelman SD, Bergman RN. Inhibition of lipolysis causes suppression of endogenous glucose production independent of changes in insulin. Am J Physiol Endocrinol Metab. 2000;279(3):E630–637. doi: 10.1152/ajpendo.2000.279.3.E630. [DOI] [PubMed] [Google Scholar]
- 78.Felig P, Pozefsky T, Marliss E, Cahill GF., Jr Alanine: key role in gluconeogenesis. Science. 1970;167(3920):1003–1004. doi: 10.1126/science.167.3920.1003. [DOI] [PubMed] [Google Scholar]
- 79.Felig P, Marliss E, Owen OE, Cahill GF., Jr Role of substrate in the regulation of hepatic gluconeogenesis in fasting man. Adv Enzyme Regul. 1969;7:41–46. doi: 10.1016/0065-2571(69)90008-9. [DOI] [PubMed] [Google Scholar]
- 80.Molusky MM, Li S, Ma D, Yu L, Lin JD. Ubiquitin-specific protease 2 regulates hepatic gluconeogenesis and diurnal glucose metabolism through 11beta-hydroxysteroid dehydrogenase 1. Diabetes. 2012;61(5):1025–1035. doi: 10.2337/db11-0970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Penn SK, Kao AH, Schott LL, Elliott JR, Toledo FG, Kuller L, Manzi S, Wasko MC. Hydroxychloroquine and glycemia in women with rheumatoid arthritis and systemic lupus erythematosus. J Rheumatol. 2010;37(6):1136–1142. doi: 10.3899/jrheum.090994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mortimore GE, Hutson NJ, Surmacz CA. Quantitative correlation between proteolysis and macro- and microautophagy in mouse hepatocytes during starvation and refeeding. Proc Natl Acad Sci U S A. 1983;80(8):2179–2183. doi: 10.1073/pnas.80.8.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Amherdt M, Harris V, Renold AE, Orci L, Unger RH. Hepatic autography in uncontrolled experimental diabetes and its relationships to insulin and glucagon. J Clin Invest. 1974;54 (1):188–193. doi: 10.1172/JCI107742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shelburne JD, Arstila AU, Trump BF. Studies on cellular autophagocytosis. Cyclic AMP- and dibutyryl cyclic AMP-stimulated autophagy in rat liver. Am J Pathol. 1973;72(3):521–540. [PMC free article] [PubMed] [Google Scholar]
- 85.Lenk SE, Bhat D, Blakeney W, Dunn WA., Jr Effects of streptozotocin-induced diabetes on rough endoplasmic reticulum and lysosomes of rat liver. Am J Physiol. 1992;263(5 Pt 1):E856–862. doi: 10.1152/ajpendo.1992.263.5.E856. [DOI] [PubMed] [Google Scholar]
- 86.Forbes JM. The physiological deadlock between AMPK and gluconeogenesis: SOGA, a novel protein, may provide the key. Am J Pathol. 2010;177(4):1600–1602. doi: 10.2353/ajpath.2010.100679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhao M, Klionsky DJ. AMPK-dependent phosphorylation of ULK1 induces autophagy. Cell Metab. 2011;13(2):119–120. doi: 10.1016/j.cmet.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sarbassov DD, Ali SM, Sabatini DM. Growing roles for the mTOR pathway. Curr Opin Cell Biol. 2005;17(6):596–603. doi: 10.1016/j.ceb.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 89.Cowherd RB, Asmar MM, Alderman JM, Alderman EA, Garland AL, Busby WH, Bodnar WM, Rusyn I, Medoff BD, Tisch R, et al. Adiponectin lowers glucose production by increasing SOGA. Am J Pathol. 2010;177(4):1936–1945. doi: 10.2353/ajpath.2010.100363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Longnus SL, Wambolt RB, Parsons HL, Brownsey RW, Allard MF. 5-Aminoimidazole-4-carboxamide 1-beta -D-ribofuranoside (AICAR) stimulates myocardial glycogenolysis by allosteric mechanisms. Am J Physiol Regul Integr Comp Physiol. 2003;284(4):R936–944. doi: 10.1152/ajpregu.00319.2002. [DOI] [PubMed] [Google Scholar]
- 91.Camacho RC, Pencek RR, Lacy DB, James FD, Donahue EP, Wasserman DH. Portal venous 5-aminoimidazole-4-carboxamide-1-beta-D-ribofuranoside infusion overcomes hyperinsulinemic suppression of endogenous glucose output. Diabetes. 2005;54(2):373–382. doi: 10.2337/diabetes.54.2.373. [DOI] [PubMed] [Google Scholar]
- 92.Gharbi SI, Zvelebil MJ, Shuttleworth SJ, Hancox T, Saghir N, Timms JF, Waterfield MD. Exploring the specificity of the PI3K family inhibitor LY294002. Biochem J. 2007;404(1):15–21. doi: 10.1042/BJ20061489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gougeon R, Morais JA, Chevalier S, Pereira S, Lamarche M, Marliss EB. Determinants of whole-body protein metabolism in subjects with and without type 2 diabetes. Diabetes Care. 2008;31 (1):128–133. doi: 10.2337/dc07-1268. [DOI] [PubMed] [Google Scholar]
- 94.Gougeon R, Pencharz PB, Marliss EB. Effect of NIDDM on the kinetics of whole-body protein metabolism. Diabetes. 1994;43(2):318–328. doi: 10.2337/diab.43.2.318. [DOI] [PubMed] [Google Scholar]
- 95.Imagawa A, Funahashi T, Nakamura T, Moriwaki M, Tanaka S, Nishizawa H, Sayama K, Uno S, Iwahashi H, Yamagata K, et al. Elevated serum concentration of adipose-derived factor, adiponectin, in patients with type 1 diabetes. Diabetes Care. 2002;25(9):1665–1666. doi: 10.2337/diacare.25.9.1665. [DOI] [PubMed] [Google Scholar]