Abstract
Study Objective:
The prevalence of supine-dependent obstructive sleep apnea (sdOSA) in a general population ranges from 20% to 60%, depending on the criteria used. Currently, the prevalence and evolution of sdOSA once oral appliance therapy with a mandibular advancement device (OAm) has started is unknown. In addition, literature on the correlation between sdOSA and treatment success with OAm is not unequivocal. The first purpose of this study was to assess the prevalence of sdOSA before and under OAm therapy. Second, the conversion rate from non-sdOSA to sdOSA during OAm therapy was evaluated. The third and final goal was to analyze the correlation between sdOSA and treatment success with OAm therapy in the patient population.
Methods:
Two hundred thirty-seven consecutive patients (age 48 ± 9 years; male/female ratio 173/64; AHI 20.1 ± 14.7 events/h; BMI 27.2 ± 4.3 kg/m2) starting OAm therapy were included.
Results:
The prevalence of sdOSA before the start of OAm therapy, ranged from 27.0% to 67.5%. The prevalence of residual sdOSA under OAm therapy in this study ranged from 17.5% to 33.9%. Second, the conversion rate from non-sdOSA to sdOSA ranged from 23.0% to 37.5%. Third, the presence of sdOSA at baseline was not a significant factor for treatment success with OAm therapy.
Conclusions:
The results of this study indicate that the prevalence of sdOSA before and under OAm therapy is relatively high. One-third of patients shift from non-sdOSA to sdOSA. Finally, treatment success for OAm therapy was not significantly correlated with the presence of sdOSA at baseline.
Citation:
Dieltjens M, Braem MJ, Van de Heyning PH, Wouters K, Vanderveken OM. Prevalence and clinical significance of supine-dependent obstructive sleep apnea in patients using oral appliance therapy. J Clin Sleep Med 2014;10(9):959-964.
Keywords: oral appliance therapy, body position, prevalence, sleep disordered breathing
Obstructive sleep apnea (OSA) is a prevalent disorder characterized by repetitive upper airway collapse or upper airway narrowing during sleep, often resulting in hypoxemia and arousal from sleep.1 It has been described that undiagnosed or untreated OSA is associated with excessive daytime sleepiness, impaired cognitive performance, a reduced quality of life, an increased risk of motor vehicle and occupational accidents, and cardiovascular and cerebrovascular morbidity and mortality.2,3 The severity of OSA is expressed by the apnea-hypopnea index (AHI), defined as the average number of apneas and hypopneas per hour of sleep.1,4 In so-called supine-dependent OSA (sdOSA) patients the breathing abnormalities are clustered mainly in the supine posture, whereas non-sdOSA patients have breathing abnormalities in both the lateral and supine postures.5–8 Therefore, it could be of clinical importance to split up the total AHI according to sleep position with the supine AHI (defined as the number of apneas and hypopneas per hour of sleep spent in supine position) and the non-supine AHI (defined as the number of apneas and hypopneas per hour of sleep spent in the non-supine position).9 The most frequently and widely used definition is a supine AHI ≥ twice as high as the non-supine AHI and was first described by Cartwright et al.5 The prevalence of sdOSA in a general population ranges from 20% to 60%, depending on the definition used. In general, patients with sdOSA are younger, have a lower body mass index (BMI), and have less severe OSA.6,10
BRIEF SUMMARY
Current Knowledge/Study Rationale: Body position during sleep is known to not only affect the severity of obstructive sleep apnea (OSA), but also the therapeutic outcome of oral appliance therapy with a mandibular advancement device (OAm). The prevalence of supine-dependent OSA (sdOSA) in a general population is relatively high. The prevalence of sdOSA under OAm therapy is currently unknown.
Study Impact: The results of this study show that the prevalence of sdOSA before and under OAm therapy is relatively high. In addition, one-third of patients shifted from non-sdOSA to sdOSA under OAm therapy.
Oral appliance (OA) therapy is increasingly prescribed as a noninvasive treatment for patients with snoring and OSA.11,12 The most common type of oral appliance is the one that reduces upper airway collapsibility by advancing the mandible (OAm).11,13,14 OAm therapy is proven to reduce the severity of OSA,14 with a relatively high compliance rate.15
In the restricted population of patients starting OAm therapy, the prevalence of sdOSA was studied and ranged according to the literature from 46% to 80%, which was comparable to the prevalence of sdOSA in the general population.13,16,17 These results, however, do not reveal the evolution of sdOSA once OAm has started, and the prevalence of sdOSA under OAm therapy is still unknown. Interestingly, in some patients sdOSA and non-sdOSA are dynamic phenotypes8: weight reduction may convert a non-sdOSA patient into sdOSA.18 In addition, it is stated that any OSA treatment that could not completely eliminate all breathing abnormalities leaves the patient with a residual OSA that is mainly supine-dependent.8 With CPAP therapy it was reported that a severe non-sdOSA patient converted to sdOSA during a CPAP titration night.19 In this study, the patient had a non-sdOSA when CPAP pressure was low. When CPAP pressure was higher in the second part of the night, the patient became clearly supine-dependent, with no respiratory events while sleeping on his side, but as soon as he shifted to the supine sleeping position, respiratory events appeared. However, it is unknown whether OAm therapy also leads to such a conversion.
In the past, retrospective analyses of clinical, physiological, and polysomnographic variables were performed in order to identify predictors of treatment success with OAm therapy. There is evidence to support the findings that OAm therapy is more likely to be successful in younger female patients, with lower body mass index, a smaller neck circumference, and less severe sleep apnea.13,20–23 In addition, the majority of studies evaluating the effect of sleep position on OAm efficacy have reported that OA therapy is more efficacious in patients with sdOSA.13,16,17,24–26 However, other studies did not find a difference in success rates between non-sdOSA and sdOSA patients.27,28
The first purpose of the present study was to evaluate the prevalence of sdOSA before and under OAm therapy. The second objective was to describe the conversion rate from non-sdOSA to sdOSA during OAm therapy. Because the literature on the correlation between sdOSA and treatment success with OAm is not unequivocal, the final goal of this study was to analyze the correlation between sdOSA and treatment success in our patient population.
METHODS
All patients in this retrospective analysis were diagnosed with OSA based on a recent polysomnography and underwent a full medical and dental examination including orthopantomography. Patients were not judged suitable for oral appliance therapy if they suffered from any preexisting temporomandibular joint (TMJ) dysfunction, if their dental status or periodontal health precluded them from wearing an oral appliance, or if they were fully edentulous. Three hundred six consecutive adult OSA patients received oral appliance therapy with a custom-made titratable OAm.
The study protocol was approved by the Institutional Review Board of the Antwerp University Hospital, Belgium (B300201110946).
Oral Appliance
Custom-made titratable OAm (Respident Butterfly, Dormoco, Belgium29 or SomnoDent Flex, Somnomed AG, Australia30) was used. Patients were instructed to gradually titrate the OAm until subjective resolution of symptoms occurred, or until the maximum comfortable limit was reached.30,31 The titration procedure lasted on average 137 ± 97 days.
Polysomnography
Patients were diagnosed with OSA based on an overnight level-I polysomnography (PSG) and were invited to undergo a PSG with OAm after the titration procedure. PSG included the recording of electroencephalography (EEG), right and left electrooculography (EOG), submental electromyography (EMG), electrocardiography (ECG), and oxygen saturation using pulse oximetry with a finger probe. Respiratory variables were recorded, including nasal airflow by means of an external thermistor and nasal pressure by using a nasal pressure canula. Respiratory effort was measured using respiratory inductance plethysmography. Body position was monitored using a piezoelectric sensor and was used to differentiate between supine, right lateral, left lateral, prone, and upright sleeping position. Snoring was recorded qualitatively by a microphone.
An apnea was defined as a total cessation of airflow > 10 s, and a hypopnea as decrease of airflow ≥ 50% from baseline, or a clear decrease in airflow associated with an oxygen de-saturation ≥ 4% and/or an arousal for ≥ 10 seconds.1 Baseline was defined as the mean amplitude of stable breathing in the 2 min preceding onset of the event (in individuals with a stable breathing pattern during sleep) or the mean amplitude of the 3 largest breaths in the 2 preceding min where breathing pattern was unstable. The severity of OSA was expressed by the AHI, defined as the number of apneas and hypopneas per hour of sleep. The diagnosis of OSA was confirmed if the AHI was > 5 events per hour of sleep.1
Treatment Outcome Measures
Complete response was defined as a decrease in AHI to < 5/h with the OAm. Partial response was defined as a reduction in AHI with the OAm ≥ 50% compared to baseline.
Supine-Dependent Obstructive Sleep Apnea
Supine AHI is defined as the number of apneas and hypopneas per hour of sleep spent in supine position, while non-supine AHI is defined as the number of apneas and hypopneas per hour of sleep spent in the non-supine position.13 Different definitions of sdOSA are described in literature. The most frequently used definition for defining sdOSA were established by Cartwright et al. as a supine AHI that is at least twice as high as a non-supine AHI5. Mador et al.10 defined SDOSA as an AHI of < 5 events/h in the non-supine position and a supine AHI of at least twice as high as the non-supine AHI, with a 15-min threshold for sleep in both postures. Marklund et al.25 defined sdOSA patients as having a supine AHI ≥ 10 events/h together with a non-supine AHI of < 10 events/h. The results of this study will be evaluated according to these different definitions.
Statistical Analysis
Data analysis was performed using SPSS (SPSS version 17.0, SPSS Inc., Chicago, IL, USA). Descriptive statistics for characteristics of patients were presented as means ± standard deviation (SD). The Shapiro-Wilk test was performed to assess the normality of distribution.
Continuous data between groups were compared with a non-parametric Mann-Whitney U test. A Wilcoxon signed-rank test was used to compare measurements at baseline and at evaluation with OAm. A multiple logistic regression model was used to study the effect of supine-dependent OSA with oral appliance efficacy, correcting for age, gender, baseline AHI, and baseline BMI. Odds ratios and corresponding 95% confidence intervals were reported.
RESULTS
Study Population and Prevalence of Supine-Dependent OSA Prior to OAm Therapy
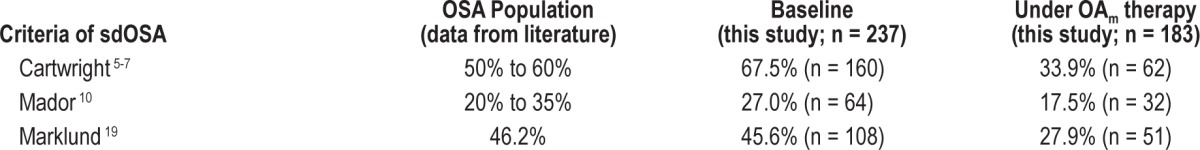
Three hundred six patients with an established diagnosis of OSA and consecutively receiving treatment with a custom-made titratable OAm were included. Anthropomorphic and polysomnographic data prior to OAm therapy were collected in all 306 patients, of whom 237 patients (age 48 ± 9 years; male/female ratio 173:64; AHI 20.1 ± 14.7/h sleep with a range from 5/h to 97.1/h; BMI 27.2 ± 4.3) had a full dataset at baseline, including supine-dependent parameters. Patients were subdivided in 2 groups following the presence or absence of sdOSA according to Cartwright's definition (Table 1). There were no statistically significant differences between these 2 groups for these baseline parameters. One hundred sixty of these 237 patients (67.5%) could be defined as patients with sdOSA following Cartwright's definition. The prevalences of sdOSA before OAm therapy following the definitions of Marklund19 and Mador10 were 45.6% and 27.0%, respectively (Table 2).
Table 1.
Anthropomorphic and polysomnographic data.
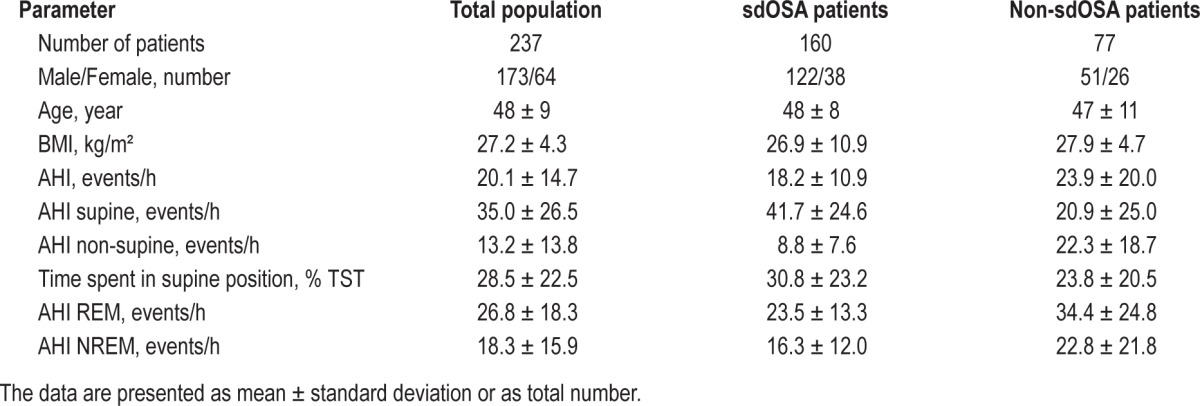
Table 2.
Prevalence of supine-dependent obstructive sleep apnea (sdOSA), according to different criteria.
OAm Efficacy
The overall effect of OAm therapy was assessed using full-night PSG with OAm. In 183 patients, polysomnographic data before and under OAm therapy were available. Overall, the OAm was effective in reducing the AHI from 20.8 ± 14.1/h at baseline to 9.9 ± 8.8/h with (p < 0.05). A significant reduction in both supine AHI, from 35.4 ± 26.0 to 15.6 ± 17.7/h with OAm (p < 0.05), and in non-supine AHI, from 13.5 ± 14.2 to 6.9 ± 7.8 with OAm (p < 0.05) was noted. In addition, both REM AHI and NREM AHI were significantly reduced under OAm therapy: from 26.8 ± 18.7 to 18.1 ± 14.8/h (p < 0.05), and from 18.1 ± 16.1 to 7.6 ± 9.1 (p < 0.05), respectively. Complete and partial response was achieved in 39.9% (73 patients) and 60.1% (110 patients), respectively.
Prevalence of Supine-Dependent OSA under OAm Therapy
In 183 patients, polysomnographic data before and under OAm therapy were available. The prevalence of residual sdOSA under OAm therapy in this study population ranged from 17.5% to 33.9%, depending on the criteria used (Table 2).
Conversion from Non-Supine-Dependent to Supine-Dependent OSA during OAm Therapy
One hundred ten of 183 patients did not achieve a complete response under OAm therapy and suffered therefore from residual OSA with an AHI > 5/h under OAm therapy. In 34 of these patients, the OSA was non-supine-dependent following Cartwright's criterion. In 12 of these patients (35%), OSA became supine-dependent under OAm therapy. In contrast, in almost two-third of patients with sdOSA before start of OAm therapy, the OSA remained supine-dependent under therapy. Following Mador's criteria, 20 of 86 (23%) non-sdOSA patients at baseline became supine-dependent under OAm therapy. Twenty-four of 64 (37.5%) non-sdOSA patients became sdOSA patients under OAm therapy following Marklund's criteria.
OAm Efficacy According to Supine-Dependency
OAm therapy was effective in reducing the AHI in both sdOSA and non-sdOSA patients following Cartwright's definition, from 18.8 ± 11.4/h at baseline to 9.0 ± 7.6/h (p < 0.05) in supine-dependent patients and from 25.1 ± 19.8/h at baseline to 11.7 ± 11.0/h (p < 0.05) in non-sdOSA patients (Figure 1). A significant reduction in supine AHI, non-supine AHI, REM AHI, and NREM AHI was noted in all patients—sdOSA as well as non-sdOSA patients. However, in sdOSA, the decrease in supine AHI (25.0 ± 26.4/h) was significantly higher than that of non-sdOSA patients (8.4 ± 24.4/h; p < 0.05), whereas the decrease in non-supine AHI was higher in non-sdOSA patients (14.8 ± 18.3/h vs 3.0 ± 8.9/h; p < 0.05). The decrease in REM AHI and NREM AHI was not significantly different in sdOSA vs non-sdOSA patients.
Figure 1. Mean apnea-hypopnea index (AHI) pre and post OAm therapy for sdOSA and non-sdOSA patients following Cartwright's definition, as well as AHI supine and AHI non-supine for both subgroups.
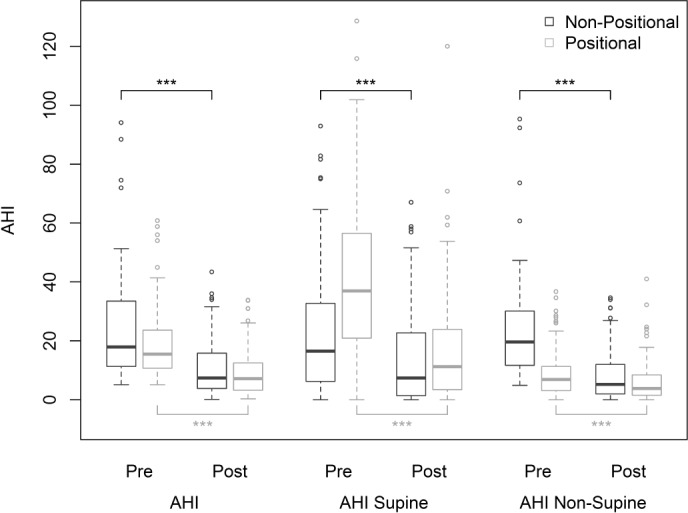
*** p < 0.001.
Complete response rate for the patients with versus without sdOSA at baseline, according to the different criteria for sdOSA, is shown in Table 3. It was noted that the complete response rate was slightly higher in patients without sdOSA at baseline than in patients with sdOSA at baseline; this was not statistically significant for the definition of Cartwright and Marklund but was significant for Mador's criterion (p < 0.05).
Table 3.
Prevalence of sdOSA, cure rate, and shift from non-sdOSA to sdOSA.

Correlation of sdOSA with Partial Response and Complete Response using a Logistic Regression Model
According to a multiple logistic model including sdOSA and the variables age, gender, baseline BMI and baseline AHI, the presence of sdOSA was no predictor of partial or complete response. The odds ratio for partial response was 0.72 (95% CI: 0.36–1.46, p = 0.37), 1.05 (95% CI: 0.54–2.04, p = 0.89), and 0.97 (95% CI: 0.47–1.99, p = 0.93) for the sdOSA criteria of Cartwright, Marklund and Mador, respectively. The odds ratio for complete response was not significant for the different definitions of sdOSA: 0.76 (95% CI: 0.37–1.58, p = 0.46), 0.86 (95% CI: 0.42–1.73, p = 0.67), and 1.12 (95% CI: 0.53–2.35, p = 0.77), respectively. A younger age and lower baseline AHI were predictors of both complete and partial response in this model.
DISCUSSION
In previous studies evaluating the effect of sleep position on OAm therapy, it was shown that the prevalence of sdOSA in patients starting OAm therapy ranged from 46% to 80%. In addition, it has been shown that sdOSA is a dynamic phenotype under varying circumstances, such as weight reduction and unsuccessful CPAP therapy. However, the effect of OAm therapy on sdOSA has not been known.
The results of this study first demonstrate that sdOSA is relatively common in patients starting OAm therapy, with a prevalence ranging between 27.0% and 67.5%, depending on the definition used (Table 2). In patients who did not achieve complete response, the prevalence of sdOSA ranges from 17.5% to 33.9%. The second objective was to describe the conversion rate of the sdOSA phenotype under OAm therapy and revealed that 23% to 37.5% shifted from non-sdOSA to sdOSA. The final goal was to analyze the correlation between sdOSA and a successful OAm treatment; statistical analysis showed that the presence of sdOSA at baseline was no predictor of OAm efficacy using a logistic regression model.
OAm therapy was effective in reducing the AHI in both supine-dependent and non-supine-dependent OSA patients. However, the decrease in supine AHI was significantly higher in sdOSA patients, whereas the decrease in non-supine AHI was higher in the non-sdOSA patients. This difference between the two patient groups is probably due to the fact that the supine AHI is significantly higher in patients with sdOSA at baseline, whereas the non-supine AHI is higher at baseline in patients with non-sdOSA (Table 1).
In the literature, different definitions of sdOSA are used.5,10,25,30 The application of three different sdOSA criteria leads to a wide range in prevalence and makes it hard to compare the prevalence of sdOSA with respect to other prevalence studies. However, Cartwright was the first to categorize patients as supine-dependent if the supine AHI was at least twice as high as the non-supine AHI.5 This criterion is the most widely and frequently used in literature. Some authors have made changes to this definition, such as Mador10 whose criterion of supine-dependent OSA is derived from Cartwright's criterion.
It was noted that almost one of three patients shifted from a non-sdOSA at baseline to sdOSA under OAm therapy. A possible explanation for this high conversion rate is that sdOSA is a dynamic phenotype associated with younger age, lower BMI, and less severe OSA.6 It has been reported previously that decreasing body weight may shift a patients with non-sdOSA to sdOSA and that by increasing body weight a patient with sdOSA may be shifted into non-sdOSA.18 In addition, any OSA therapy that is not able to completely eliminate all breathing abnormalities leaves the patient with a residual OSA, which is less severe than the initial OSA and is therefore probable more supine-dependent. This conversation rate was described under CPAP therapy and is now described for OAm therapy. The exact underlying pathophysiologic mechanism of this dynamic phenotype is unknown. However, one could hypothesize that differences in upper airway collapsibility play a major role.32,33 A possible mechanism is that young, thin patients have initially a low collapsibility of the upper airway, with respiratory events being only present while sleeping in the supine position where the gravitational forces increases the tendency of upper airway collapse. In general, the tendency of upper airway collapse increases with higher age and higher BMI. As a consequence, such patients could develop respiratory events in the lateral position with increasing age and/or weight gain.34
Previous studies of positional therapies using the tennis ball technique showed a compliance of less than 40% after long-term follow-up.35–37 The main reason for discontinuation were discomfort, backache, and no improvement in sleep quality and was attributed to the use of bulky devices placed on patient's back to discourage a supine sleeping position.38 Recently, a new neck-worn device that vibrates when in supine position has shown promising results in overcoming these compliance aspects.39
In the present study, the presence of sdOSA has no effect on OAm efficacy. This finding contrasts previous studies where it was found that the OAm efficacy may be influenced by sleep position in a way that patients with sdOSA have better treatment outcomes under OAm therapy.13,16,17,24–26 Only one other study has found no effect of body position on the outcome of OA therapy.27 This topic needs to be further elucidated in larger prospective randomized and controlled clinical studies to better understand OAm efficacy across all sleep stages and body positions.
It is assumed that the amount of supine sleep varies between nights.40 In patients with position-dependent OSA, this can lead to a possible night-to-night variation in AHI and OSA severity due to the discrepancy between supine and non-supine AHI.41,42 In addition, the relationship between supine sleep time in the sleep lab during a full polysomnography and the supine sleep time at home in the individual patient is yet unknown.42 This clearly illustrates the clinical relevance of defining supine-dependency in patients; therefore, it is recommended to use supine-dependent data in clinical practice, particularly in aid of treatment choices and follow-up of patients with position-dependent sleep apnea.41
The present study has its limitations. The first limitation is that this is a retrospective analysis. This means there were many participants with missing data at baseline and that there was a relatively high participation loss. Second, two types of oral appliances were used. However, statistical analysis revealed that there was no difference in success rate and sdOSA prevalence between the two different oral appliances.
Despite these limitations, the authors believe that the relatively high conversion rate of sdOSA under OAm therapy as well as the high prevalence of sdOSA under OAm therapy have important clinical relevance. Avoidance of the supine sleeping position could have an influence on the overall AHI in those patients, and positional therapy should be considered as a treatment option or as additive treatment in patients with residual sdOSA under OAm therapy.
CONCLUSION
In conclusion, the findings of this study show that the prevalence of sdOSA before and during OAm therapy is clinically relevant. Second, one-third of patients shift from non-supine-dependent to sdOSA. Finally, treatment success was not statistically significant correlated with the presence of sdOSA at baseline.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 2.Vanderveken OM, Boudewyns A, Ni Q, et al. Cardiovascular implications in the treatment of obstructive sleep apnea. J Cardiovasc Transl Res. 2011;4:53–60. doi: 10.1007/s12265-010-9238-y. [DOI] [PubMed] [Google Scholar]
- 3.Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 4.Epstein LJ, Kristo D, Strollo PJ, Jr., et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–76. [PMC free article] [PubMed] [Google Scholar]
- 5.Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep. 1984;7:110–4. doi: 10.1093/sleep/7.2.110. [DOI] [PubMed] [Google Scholar]
- 6.Oksenberg A, Silverberg DS, Arons E, et al. Positional vs nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data. Chest. 1997;112:629–39. doi: 10.1378/chest.112.3.629. [DOI] [PubMed] [Google Scholar]
- 7.Richard W, Kox D, den Herder C, Laman M, van Tinteren H, de Vries N. The role of sleep position in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2006;263:946–50. doi: 10.1007/s00405-006-0090-2. [DOI] [PubMed] [Google Scholar]
- 8.Oksenberg AS. Positional therapy for sleep apnea: a promising behavioral therapeutic option still waiting for qualified studies. Sleep Med Rev. 2014;18:3–5. doi: 10.1016/j.smrv.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Joosten M, Seitz V, Zimmermann K, et al. Histone acetylation and DNA demethylation of T cells result in an anaplastic large cell lymphoma-like phenotype. Haematologica. 2013;98:247–54. doi: 10.3324/haematol.2011.054619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mador MJ, Kufel TJ, Magalang UJ, et al. Prevalence of positional sleep apnea in patients undergoing polysomnography. Chest. 2005;128:2130–7. doi: 10.1378/chest.128.4.2130. [DOI] [PubMed] [Google Scholar]
- 11.Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10:215–27. doi: 10.5664/jcsm.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marklund M, Verbraecken J, Randerath W. Non-CPAP therapies in obstructive sleep apnoea: mandibular advancement device therapy. Eur Res J. 2012;39:1241–7. doi: 10.1183/09031936.00144711. [DOI] [PubMed] [Google Scholar]
- 13.Marklund M, Stenlund H, Franklin KA. Mandibular advancement devices in 630 men and women with obstructive sleep apnea and snoring: tolerability and predictors of treatment success. Chest. 2004;125:1270–8. doi: 10.1378/chest.125.4.1270. [DOI] [PubMed] [Google Scholar]
- 14.Gauthier L, Laberge L, Beaudry M, et al. Mandibular advancement appliances remain effective in lowering respiratory disturbance index for 2.5-4.5 years. Sleep Med. 2011;12:844–9. doi: 10.1016/j.sleep.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Vanderveken OM, Dieltjens M, Wouters K, et al. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax. 2013;68:91–6. doi: 10.1136/thoraxjnl-2012-201900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee CH, Jung HJ, Lee WH, et al. The effect of positional dependency on outcomes of treatment with a mandibular advancement device. Arch Otolaryngol Head Neck Surg. 2012;138:479–83. doi: 10.1001/archoto.2012.452. [DOI] [PubMed] [Google Scholar]
- 17.Chung JW, Enciso R, Levendowski DJ, et al. Treatment outcomes of mandibular advancement devices in positional and nonpositional OSA patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:724–31. doi: 10.1016/j.tripleo.2009.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oksenberg A, Dynia A, Nasser K, et al. Obstructive sleep apnoea in adults: body postures and weight changes interactions. J Sleep Res. 2012;21:402–9. doi: 10.1111/j.1365-2869.2011.00988.x. [DOI] [PubMed] [Google Scholar]
- 19.Siddiqui F, Osuna E, Chokroverty S. Non-positional severe obstructive sleep apnea on polysomnogram became positional OSA with CPAP therapy. Sleep Med. 2006;7:385–6. doi: 10.1016/j.sleep.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Otsuka R, Almeida FR, Lowe AA, Ryan F. A comparison of responders and nonresponders to oral appliance therapy for the treatment of obstructive sleep apnea. Am J Orthodont Dentofac Orthop. 2006;129:222–9. doi: 10.1016/j.ajodo.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 21.Barnes M, McEvoy RD, Banks S, et al. Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med. 2004;170:656–64. doi: 10.1164/rccm.200311-1571OC. [DOI] [PubMed] [Google Scholar]
- 22.Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163:1457–61. doi: 10.1164/ajrccm.163.6.2004213. [DOI] [PubMed] [Google Scholar]
- 23.Liu Y, Lowe AA, Fleetham JA, Park YC. Cephalometric and physiologic predictors of the efficacy of an adjustable oral appliance for treating obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2001;120:639–47. doi: 10.1067/mod.2001.118782. [DOI] [PubMed] [Google Scholar]
- 24.Cartwright RD. Predicting response to the tongue retaining device for sleep apnea syndrome. Arch Otolaryngol. 1985;111:385–8. doi: 10.1001/archotol.1985.00800080071008. [DOI] [PubMed] [Google Scholar]
- 25.Marklund M, Persson M, Franklin KA. Treatment success with a mandibular advancement device is related to supine-dependent sleep apnea. Chest. 1998;114:1630–5. doi: 10.1378/chest.114.6.1630. [DOI] [PubMed] [Google Scholar]
- 26.Yoshida K. Influence of sleep posture on response to oral appliance therapy for sleep apnea syndrome. Sleep. 2001;24:538–44. doi: 10.1093/sleep/24.5.538. [DOI] [PubMed] [Google Scholar]
- 27.Fransson AM, Tegelberg A, Leissner L, Wenneberg B, Isacsson G. Effects of a mandibular protruding device on the sleep of patients with obstructive sleep apnea and snoring problems: a 2-year follow-up. Sleep Breath. 2003;7:131–41. doi: 10.1007/s11325-003-0131-7. [DOI] [PubMed] [Google Scholar]
- 28.Sutherland KT, Phillips C, Darendeliler A, Qian J, Cistulli P. Polysomnographic phenotypes of OSA and mandibular advancement splint treatment outcome. Abstract presented on the second international conference organized by the European Respiratory Society and the European Sleep Research Society.2013. [Google Scholar]
- 29.Dieltjens M, Vanderveken OM, Hamans E, et al. Treatment of obstructive sleep apnea using a custom-made titratable duobloc oral appliance: a prospective clinical study. Sleep Breath. 2012;17:565–72. doi: 10.1007/s11325-012-0721-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gotsopoulos H, Chen C, Qian J, et al. Oral appliance therapy improves symptoms in obstructive sleep apnea: a randomized, controlled trial. Am J Respir Crit Care Med. 2002;166:743–8. doi: 10.1164/rccm.200203-208OC. [DOI] [PubMed] [Google Scholar]
- 31.Dieltjens M, Vanderveken OM, Van de Heyning PH, et al. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med Rev. 2012;16:177–85. doi: 10.1016/j.smrv.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 32.Sforza E, Petiau C, Weiss T, et al. Pharyngeal critical pressure in patients with obstructive sleep apnea syndrome. Clinical implications. Am J Respir Crit Care Med. 1999;159:149–57. doi: 10.1164/ajrccm.159.1.9804140. [DOI] [PubMed] [Google Scholar]
- 33.Kirkness JP, Schwartz AR, Schneider H, et al. Contribution of male sex, age, and obesity to mechanical instability of the upper airway during sleep. J Appl Physiol. 2008;104:1618–24. doi: 10.1152/japplphysiol.00045.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Joosten SA, Hamza K, Sands S, Turton A, Berger P, Hamilton G. Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology. 2012;17:99–107. doi: 10.1111/j.1440-1843.2011.02037.x. [DOI] [PubMed] [Google Scholar]
- 35.Oksenberg A, Silverberg D, Offenbach D, Arons E. Positional therapy for obstructive sleep apnea patients: a 6-month follow-up study. Laryngoscope. 2006;116:1995–2000. doi: 10.1097/01.mlg.0000237674.66716.a7. [DOI] [PubMed] [Google Scholar]
- 36.Bignold JJ, Deans-Costi G, Goldsworthy MR, et al. Poor long-term patient compliance with the tennis ball technique for treating positional obstructive sleep apnea. J Clin Sleep Med. 2009;5:428–30. [PMC free article] [PubMed] [Google Scholar]
- 37.Wenzel S, Smith E, Leiacker R, Fischer Y. [Efficacy and longterm compliance of the vest preventing the supine position in patients with obstructive sleep apnea] Laryngorhinootologie. 2007;86:579–83. doi: 10.1055/s-2007-966179. [DOI] [PubMed] [Google Scholar]
- 38.Ravesloot MJ, Van Maanen JP, Dun L, et al. The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath. 2013;17:39–49. doi: 10.1007/s11325-012-0683-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Maanen JP, Richard W, Van Kesteren ER, et al. Evaluation of a new simple treatment for positional sleep apnoea patients. J Sleep Res. 2012;21:322–9. doi: 10.1111/j.1365-2869.2011.00974.x. [DOI] [PubMed] [Google Scholar]
- 40.Joosten SA, O'Driscoll DM, Berger PJ, Hamilton GS. Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev. 2014;18:7–17. doi: 10.1016/j.smrv.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 41.Sunnergren O, Brostrom A, Svanborg E. Positional sensitivity as a confounder in diagnosis of severity of obstructive sleep apnea. Sleep Breath. 2013;17:173–9. doi: 10.1007/s11325-012-0666-6. [DOI] [PubMed] [Google Scholar]
- 42.Eiseman NA, Westover MB, Ellenbogen JM, et al. The impact of body posture and sleep stages on sleep apnea severity in adults. J Clin Sleep Med. 2012;8:655–66. doi: 10.5664/jcsm.2258. [DOI] [PMC free article] [PubMed] [Google Scholar]


