Abstract
Background
Obstructive lung disease is a growing health problem, especially in developed countries. This study aimed to compare Impulse Osillometry System (IOS) and Spirometry for evaluation of Chronic Obstructive Pulmonary Disease and asthma.
Materials and Methods
The study groups contained 87 healthy people, 87 asthmatic patients and 56 COPD patients. Spirometry (FVC, FEV1, FEV1/FVC) and IOS (R5, R20, X5) measurements were performed for all the healthy subjects and patients. The results of IOS were compared with spirometric results.
Results
Significant differences were detected among the 3 groups (control, COPD and asthma) in terms of all the spirometric parameters (FVC, FEV1, FEV1/FVC) and some parameters of IOS (R5,R20,X5) measurements (p<0.05). Among COPD patients, sensitivity for X5 (the best value of IOS measurements in the COPD group) was 76%. Also, in asthmatic patients, sensitivity for R20 (the best value of IOS measurements in the asthma group) was 77%. We found a correlation between R5, R20 and X5 with FEV1 in asthmatic patients, but only R5 had this correlation with FEV1 in COPD patients.
Conclusion
We concluded that IOS can be an alternative for spirometry in the diagnosis of obstructive lung disease in patients with minimal cooperation. R5 can represent COPD severity.
Keywords: Impulse Osillometry System (IOS), Spirometry, Asthma, COPD
INTRODUCTION
Obstructive lung disease is a growing health problem, especially in developed countries. Obstructive lung disease includes asthma and Chronic Obstructive Pulmonary Disease (COPD) and is the 4th cause of overall mortality (1).
COPD should be concerned in all patients suffering from dyspnea, cough or chronic sputum, or those who have a history of exposure to hazardous agents. COPD is confirmed by spirometry when FEV1/FVC is less than 70% after using bronchodilator. Forced Expiratory Volume in the 1st second of expiration (FEV1) decreases with disease severity progression (2).
Asthma is a growing health problem as well (3) which is confirmed by taking history, physical examination, and pulmonary function tests according to the Global Initiative for Asthma (GINA) Guideline (4).
Spirometry evaluates the diagnosis of asthma, its severity, and reversibility of airflow obstruction. Spirometry is the method of choice for evaluating obstructive lung disease. A 12% or 200 cc increase in FEV1 after bronchodilator administration confirms asthma diagnosis (5).
FEV1 is one of the diagnostic and severity indicators of obstructive lung diseases. Evaluation of this parameter depends on patient‘s cooperation (5).
In 1956, Forced Oscillation Technique (FOT) was introduced to resolve previous problems. This technique is applied when the patient is breathing normally (6).
FOT determines the relation between external forces in a respiratory disease and air flow conduction (7). FOT does not need forced expiratory maneuvers, or mouthpiece. It requires minimum patient cooperation (8).
FOT underwent some modifications and was computerized to assess breathing impedance, total airway resistance (Rrs) and reactance (elastic properties of the lung) (Xrs) in specific oscillation frequencies during a measurement lasting several seconds and normal forced breathing. This technique is known as Impulse Oscillation System (IOS) (1).
It showed similar airway resistance and reactance values as those measured by body plethysmography and forced oscillation in adults (9, 10).
Also, IOS has shown to be more sensitive than FEV1 for evaluating bronchodilators’ effects (11–13).
Impulse Osillometry was studied in children, and suggested as an alternative for spirometry (14–19).
Previous reports have studied Impulse Osillometry for evaluation of chronic respiratory disease in adults (20–29).
This study was conducted to compare IOS with conventional pulmonary function tests (spirometry) in Iranian adults with obstructive lung disease.
MATERIALS AND METHODS
In this cross sectional study, 230 new adult patients (87 healthy subjects, 87 asthmatic patients and 56 COPD patients) presenting to Bamdad respiratory and sleep research center were evaluated.
An informed consent was obtained from all patients. The study protocol was approved by Isfahan University of Medical Sciences Ethics Committee, Isfahan, Iran.
Patients’ demographic variables, history and physical examination were obtained by a trained physician.
Subjects were divided into 2 groups of healthy and obstructive lung disease (asthma and COPD) based on their medical history, physical examination, GOLD and GINA guidelines.
COPD was diagnosed by having a positive history of dyspnea (progressive, exertional or persistent), chronic cough (may be intermittent or non productive), chronic sputum and history of exposure to tobacco, occupational dusts, chemicals or other smokes after the age of 40. The diagnosis of COPD was confirmed by having a positive history and FEV1/FVC less than 70% after applying bronchodilator in spirometry according to GOLD guidelines (2).
Asthma was defined as having history of recurrent wheezing, cough, chest tightness or difficult breathing, in accordance with other allergic symptoms which may have a seasonal pattern or may exacerbate in night or by common allergens, exercise or smoke. Diagnosis of asthma was confirmed by finding airway obstruction reversible by bronchodilator in spirometry based on GINA guidelines (4).
Then, one time spirometry (FVC, FEV1, FEV1/FVC) and IOS (R5,R20, X5) measurements were performed for all patients and healthy subjects.
Spirometry and Impulse Osillometry were evaluated using “Master Screen -IOS; Master lab Erich Jaeger, Germany”.
Pulmonary function tests were done with the findings of the ATS/ERS Task Force 2005 by a trained technician (30).
The results of IOS were compared with those of spirometry in 3 groups.
Statistical analysis was done using SPSS version 17 software (Chicago; USA). Data were represented as mean± Standard Deviation (SD) in this article. The Kolmogorov-Smirnov test was used to determine the normal dispersal of the values. X5 and R5 were nonparametric values. The 3 groups were compared using ANOVA and chi-square tests. Specificity, sensitivity, positive and negative predictive values were evaluated by ROC curve. The relation between IOS and Spirometry measurement was determined by Pearson (for normal distribution) or Spearman correlation (for not normal distribution). P≤0.05 was considered significant.
RESULTS
The study comprised 230 participants including 87 healthy people, 87 asthmatic patients and 56 COPD patients. The mean age was 45(±19) yrs. There were 88 males and 142 females. Baseline characteristics, spirometry (FVC, FEV1, FEV1/FVC) and IOS (R5,R20,X5) measurements in 3 groups (control, asthma and COPD) are summarized in Table 1.
Table 1.
Baseline characteristics, spirometry and IOS measurements in 3 groups
| Variable | Control | Asthma | COPD | P-value |
|---|---|---|---|---|
| N | 87 | 87 | 56 | - |
| Age (year) | 37.6 ± 17.8 | 41.4 ± 15.5 | 64.1 ± 15.8 | <0.0001 |
| Male / Female | 38 / 49 | 23 / 64 | 27 / 29 | 0.01 |
| FVC(Lit) | 3.6 ± 1 | 3 ± 0.8 | 2.2 ± 0.9 | <0.0001 |
| FEV1(Lit) | 3.2 ± 0.9 | 2.2 ± 0.6 | 1.4 ± 0.6 | <0.001 |
| FEV1 / FVC (%) | 88.2 ± 5.3 | 72.1 ± 10.1 | 63.6 ± 9.3 | <0.001 |
| R5(kpa.s/l) | 0.40 ± 0.30 | 0.71 ± 0.42 | 0.66 ± 0.40 | <0.001 |
| R20(kpa.s/l) | 0.32 ± 0.16 | 0.40 ± 0.13 | 0.40 ± 0.21 | 0.001 |
| X5(kpa.s/l) | -0.12 ± 0.24 | -0.20 ± 0.24 | -0.33 ± 0.46 | <0.0001 |
COPD patients were older, and the male proportion in the COPD group was greater than in the other 2 groups.
A significant increase in R5 and R20 was seen in COPD and asthmatic patients in comparison with controls, while X5 had a considerable decrease in patients group.
Sensitivity, specificity, negative and positive predictive values of IOS for asthma and COPD detection are described in Tables 2 and 3. For the gold standard diagnosis of asthma and COPD based on GINA and GOLD guidelines, cut off points of Impulse Osillometry parameters were determined.
Table 2.
Sensitivity, specificity, negative and positive predictive values of IOS and spirometry in asthmatic patients
| Variable | Cut off point | Sensitivity | 95% CI | Specificity | 95% CI | +LR | -LR | +PV | -PV |
|---|---|---|---|---|---|---|---|---|---|
| R5 | >0.51 | 68.97 | 58.1 - 78.5 | 86.05 | 76.9 - 92.6 | 4.94 | 0.36 | 83.3 | 73.3 |
| R20 | >0.33 | 77.01 | 66.8 - 85.4 | 65.88 | 54.8 - 75.8 | 2.26 | 0.35 | 69.8 | 73.7 |
| X5 | <=-0.2 | 41.38 | 30.9 - 52.4 | 90.80 | 82.7 - 95.9 | 4.50 | 0.65 | 81.8 | 60.8 |
LR: Positive likelihood ratio, -LR: Negative likelihood ratio, +PV: Positive predictive value, -PV: Negative predictive value.
Table 3.
Sensitivity, specificity, negative and positive predictive values of IOS and spirometry in COPD patients
| Variable | Cut Of Point | Sensitivity | 95% CI | Specificity | 95% CI | +LR | -LR | +PV | -PV |
|---|---|---|---|---|---|---|---|---|---|
| R5 | >0.53 | 58.93 | 45.0 - 71.9 | 89.53 | 81.1 - 95.1 | 5.63 | 0.46 | 78.6 | 77.0 |
| R20 | >0.39 | 41.07 | 28.1 - 55.0 | 82.35 | 72.6 - 89.8 | 2.33 | 0.72 | 60.5 | 68.0 |
| X5 | <=-0.16 | 76.79 | 63.6 - 87.0 | 81.61 | 71.9 - 89.1 | 4.18 | 0.28 | 72.9 | 84.5 |
LR: Positive likelihood ratio, -LR: Negative likelihood ratio, +PV: Positive predictive value, -PV: Negative predictive value.
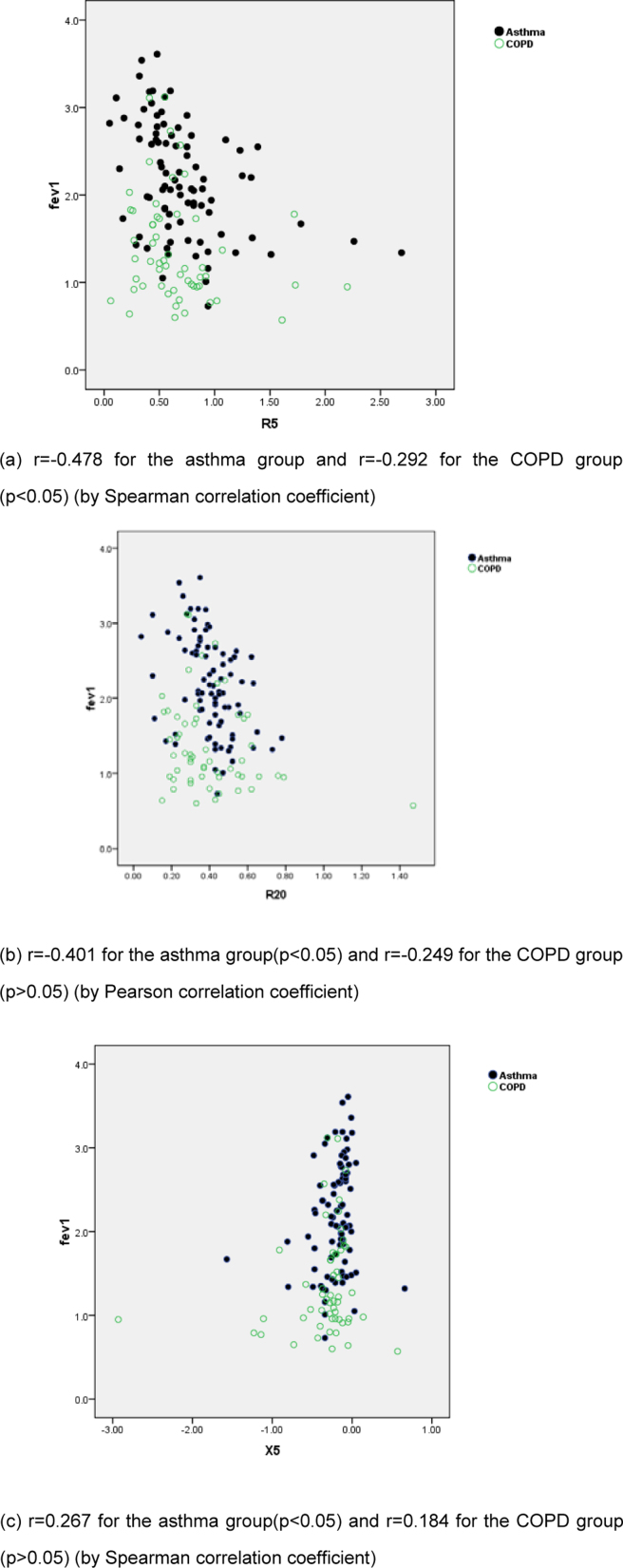
R5 was significantly correlated with FVC (r=-0.327 in the asthma group and r=-0.285 in the COPD group), FEV1 (r=-0.478 in the asthma group and r=-0.292 in the COPD group) and FEV1/FVC in asthmatic patients (r=-0.369).
R20 was significantly correlated with FVC(r=-0.342 for the asthma group and r=-0.289 for the COPD group), FEV1 (only in asthmatic patients r=-0.401) and FEV1/FVC (r=-0.240 for the asthma group and r=0.263 for the COPD group).
X5 was correlated with FEV1 (only in the asthmatic group r=0.267), and FEV1/EVC(r=0.470 for the asthma group and r=0.349 for the COPD group) (Figure 1a, b, c).
Figure 1.
Relationship between FEV1 and IOS measurements (a) FEV1 vs. R5 (b) FEV1vs. R5 (c) FEV1 vs. R20
DISCUSSION
This study compared the accuracy of IOS with spirometry measurements for detection of asthma and COPD. There was a remarkable increase in R5 and R20 and also a considerable decrease in X5 in COPD and asthmatic patients in comparison with the control population.
In our study among COPD patients, sensitivity for X5 (the best value in IOS measurements in COPD group) was 76% and in asthmatic patients, sensitivity of R20 (the best value in IOS measurements in the asthmatic group) was 77%.
In 2007, Al-Mutairi et al, showed a 31.3% sensitivity for IOS for asthma and 19.6% sensitivity for conventional pulmonary function tests. They revealed 38.95% sensitivity for IOS in COPD and 47.4% sensitivity for conventional pulmonary function tests. The sensitivity of IOS was 45.8% for detecting healthy people, and was superior to that of PFT (28.8%). There was 80.5% specificity for IOS and 86.2% for cPFT in detecting healthy people (7). In contrast with Al-Mutairi study, our findings showed greater sensitivity and specificity for IOS.
In 2009, Winkler et al. detected 87-94% of asthmatic and COPD patients by using different IOS measurements (30). These rates were greater than those of ours. It can be attributed to the method of study, which included established COPD and asthmatic patients.
IOS resistance values can be useful for mild COPD diagnosis and small-airway changes after bronchodilator and bronchoprovocation challenges (31–33) but reactance values would do better for detecting the progression of COPD (33).
Similar to previous reports(5), this study found higher sensitivity of reactance compared to resistance measurements in asthmatic patients, but sensitivity of resistance measurements was greater in COPD patients.
Resistance components increased in COPD and asthma, while X5 had a significant decrease in comparison with the control group. These findings are comparable to previous findings (31).
The present study confirms the considerable sensitivity of IOS for detection of obstructive lung disease.
When comparing IOS measurements (R5,R20,X5) and spirometry in asthmatic and COPD patients, we found a correlation between IOS parameters and FEV1 in asthmatic patients (Fig. 1a–c), but only R5 had such correlation with FEV1 in COPD patients. It shows that the severity of COPD is correlated with R5. R5 and X5 were previously shown to be related with FEV1 (5, 19).
Kanda et al. demonstrated larger within-breath changes of Xrs5 in advanced COPD patients (31).
Recent studies suggest that inspiratory-expiratory X5 analysis can differentiate COPD and asthmatic patients better than whole-breath IOS (32). Inspiratory evaluation of IOS is more accurate than expiratory evaluation (33).
In conclusion, IOS can be a good alternative of spirometry for the diagnosis of obstructive lung disease in patients with minimal cooperation. In new patients complaining of acute attack of dyspnea exacerbation, IOS is a suitable measurement for obtaining further details regarding lung function. These patients cannot perform favorable breathing maneuvers; therefore, IOS is suggested for them.
Gaining further knowledge about IOS can greatly improve the process of disease evaluation.
REFERENCES
- 1.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS, GOLD Scientific Committee Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. (updated 2010) Available at http://www.goldcopd.org/
- 3.European Community Respiratory Health Survey II Steering Committee. The European Community Respiratory Health Survey II. Eur Respir J. 2002;20(5):1071–9. doi: 10.1183/09031936.02.00046802. [DOI] [PubMed] [Google Scholar]
- 4.Global Initiative for Asthma (Updated 2008): Global strategy for asthma management and Prevention. Available at www.ginasthma.com.
- 5.Kolsum U, Borrill Z, Roy K, Starkey C, Vestbo J, Houghton C, et al. Impulse oscillometry in COPD: identification of measurements related to airway obstruction, airway conductance and lung volumes. Respir Med. 2009;103(1):136–43. doi: 10.1016/j.rmed.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Dubois AB, Brody AW, Lewis DH, Burgess BF., Jr Oscillation mechanics of lungs and chest in man. J Appl Physiol. 1956;8(6):587–94. doi: 10.1152/jappl.1956.8.6.587. [DOI] [PubMed] [Google Scholar]
- 7.Al-Mutairi SS, Sharma PN, Al-Alawi A, Al-Deen JS. Impulse oscillometry: an alternative modality to the conventional pulmonary function test to categorise obstructive pulmonary disorders. Clin Exp Med. 2007;7(2):56–64. doi: 10.1007/s10238-007-0126-y. [DOI] [PubMed] [Google Scholar]
- 8.Navajas D, Farré R. Oscillation mechanics. Eur Respir Mon. 1999;4(12):112–40. [Google Scholar]
- 9.Chinet T, Pelle G, Macquin-Mavier I, Lorino H, Harf A. Comparison of the dose-response curves obtained by forced oscillation and plethysmography during carbachol inhalation. Eur Respir J. 1988;1(7):600–5. [PubMed] [Google Scholar]
- 10.Hellinckx J, Cauberghs M, De Boeck K, Demedts M. Evaluation of impulse oscillation system: comparison with forced oscillation technique and body plethysmography. Eur Respir J. 2001;18(3):564–70. doi: 10.1183/09031936.01.00046401. [DOI] [PubMed] [Google Scholar]
- 11.Houghton CM, Woodcock AA, Singh D. A comparison of lung function methods for assessing dose-response effects of salbutamol. Br J Clin Pharmacol. 2004;58(2):134–41. doi: 10.1111/j.1365-2125.2004.02105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Houghton CM, Woodcock AA, Singh D. A comparison of plethysmography, spirometry and oscillometry for assessing the pulmonary effects of inhaled ipratropium bromide in healthy subjects and patients with asthma. Br J Clin Pharmacol. 2005;59(2):152–9. doi: 10.1111/j.1365-2125.2004.02262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borrill ZL, Houghton CM, Woodcock AA, Vestbo J, Singh D. Measuring bronchodilation in COPD clinical trials. Br J Clin Pharmacol. 2005;59(4):379–84. doi: 10.1111/j.1365-2125.2004.02261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klug B, Bisgaard H. Measurement of lung function in awake 2-4-year-old asthmatic children during methacholine challenge and acute asthma: a comparison of the impulse oscillation technique, the interrupter technique, and transcutaneous measurement of oxygen versus whole-body plethysmography. Pediatr Pulmonol. 1996;21(5):290–300. doi: 10.1002/(SICI)1099-0496(199605)21:5<290::AID-PPUL4>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 15.Klug B. The impulse oscillation technique applied for measurements of respiratory function in young children. Pediatr Pulmonol Suppl. 1997;16:240–1. doi: 10.1002/ppul.19502308125. [DOI] [PubMed] [Google Scholar]
- 16.Marotta A, Klinnert MD, Price MR, Larsen GL, Liu AH. Impulse oscillometry provides an effective measure of lung dysfunction in 4-year-old children at risk for persistent asthma. J Allergy Clin Immunol. 2003;112(2):317–22. doi: 10.1067/mai.2003.1627. [DOI] [PubMed] [Google Scholar]
- 17.Bisgaard H, Klug B. Lung function measurement in awake young children. Eur Respir J. 1995;8(12):2067–75. doi: 10.1183/09031936.95.08122067. [DOI] [PubMed] [Google Scholar]
- 18.Ortiz G, Menendez R. The effects of inhaled albuterol and salmeterol in 2- to 5-year-old asthmatic children as measured by impulse oscillometry. J Asthma. 2002;39(6):531–6. doi: 10.1081/jas-120004923. [DOI] [PubMed] [Google Scholar]
- 19.Song TW, Kim KW, Kim ES, Kim KE, Sohn MH. Correlation between spirometry and impulse oscillometry in children with asthma. Acta Paediatr. 2008;97(1):51–4. doi: 10.1111/j.1651-2227.2007.00526.x. Erratum in: Acta Paediatr 2008; 97 (4): 520. [DOI] [PubMed] [Google Scholar]
- 20.Johnson BD, Beck KC, Zeballos RJ, Weisman IM. Advances in pulmonary laboratory testing. Chest. 1999;116(5):1377–87. doi: 10.1378/chest.116.5.1377. [DOI] [PubMed] [Google Scholar]
- 21.van Noord JA, Cauberghs M, Van de Woestijne KP, Demedts M. Total respiratory resistance and reactance in ankylosing spondylitis and kyphoscoliosis. Eur Respir J. 1991;4(8):945–51. [PubMed] [Google Scholar]
- 22.Wouters EF. Total respiratory impedance measurement by forced oscillations: a noninvasive method to assess bronchial response in occupational medicine. Exp Lung Res. 1990;16(1):25–40. doi: 10.3109/01902149009064697. [DOI] [PubMed] [Google Scholar]
- 23.Schmekel B, Smith HJ. The diagnostic capacity of forced oscillation and forced expiration techniques in identifying asthma by isocapnic hyperpnoea of cold air. Eur Respir J. 1997;10(10):2243–9. doi: 10.1183/09031936.97.10102243. [DOI] [PubMed] [Google Scholar]
- 24.Kuhnle GE, Brandt T, Roth U, Goetz AE, Smith HJ, Peter K. Measurement of respiratory impedance by impulse oscillometry--effects of endotracheal tubes. Res Exp Med (Berl) 2000;200(1):17–26. [PubMed] [Google Scholar]
- 25.Witte KK, Morice A, Cleland JG, Clark AL. The reversibility of increased airways resistance in chronic heart failure measured by impulse oscillometry. J Card Fail. 2004;10(2):149–54. doi: 10.1016/j.cardfail.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Zerah F, Lorino AM, Lorino H, Harf A, Macquin-Mavier I. Forced oscillation technique vs spirometry to assess bronchodilatation in patients with asthma and COPD. Chest. 1995;108(1):41–7. doi: 10.1378/chest.108.1.41. [DOI] [PubMed] [Google Scholar]
- 27.Van Noord JA, Smeets J, Clément J, Van de Woestijne KP, Demedts M. Assessment of reversibility of airflow obstruction. Am J Respir Crit Care Med. 1994;150(2):551–4. doi: 10.1164/ajrccm.150.2.8049845. [DOI] [PubMed] [Google Scholar]
- 28.Van Noord JA, Clément J, Van de Woestijne KP, Demedts M. Total respiratory resistance and reactance in patients with asthma, chronic bronchitis, and emphysema. Am Rev Respir Dis. 1991;143(5 Pt 1):922–7. doi: 10.1164/ajrccm/143.5_Pt_1.922. [DOI] [PubMed] [Google Scholar]
- 29.Govaerts E, Demedts M, Van de Woestijne KP. Total respiratory impedance and early emphysema. Eur Respir J. 1993;6(8):1181–5. [PubMed] [Google Scholar]
- 30.Winkler J, Hagert-Winkler A, Wirtz H, Schauer J, Kahn T, Hoheisel G. Impulse oscillometry in the diagnosis of the severity of obstructive pulmonary disease. Pneumologie. 2009;63(5):266–75. doi: 10.1055/s-0028-1119698. [DOI] [PubMed] [Google Scholar]
- 31.Kanda S, Fujimoto K, Komatsu Y, Yasuo M, Hanaoka M, Kubo K. Evaluation of respiratory impedance in asthma and COPD by an impulse oscillation system. Intern Med. 2010;49(1):23–30. doi: 10.2169/internalmedicine.49.2191. [DOI] [PubMed] [Google Scholar]
- 32.Paredi P, Goldman M, Alamen A, Ausin P, Usmani OS, Pride NB, et al. Comparison of inspiratory and expiratory resistance and reactance in patients with asthma and chronic obstructive pulmonary disease. Thorax. 2010;65(3):263–7. doi: 10.1136/thx.2009.120790. [DOI] [PubMed] [Google Scholar]
- 33.Kubota M, Shirai G, Nakamori T, Kokubo K, Masuda N, Kobayashi H. Low frequency oscillometry parameters in COPD patients are less variable during inspiration than during expiration. Respir Physiol Neurobiol. 2009;166(2):73–9. doi: 10.1016/j.resp.2009.01.007. [DOI] [PubMed] [Google Scholar]