Abstract
Background
Pulmonary hypertension (PH) is a significant cause of morbidity and mortality in patients suffering from pulmonary parenchymal diseases. Diagnosis of PH has always been a major clinical dilemma due to its non-specific clinical manifestations. However, diagnosing PH and determining its severity are essential for the prognosis and treatment planning in PH patients. This study aimed at evaluating the correlation between the pulmonary artery diameter (PAD) in the CT-scan and pulmonary artery pressure (PAP) in echocardiography of patients.
Materials and Methods
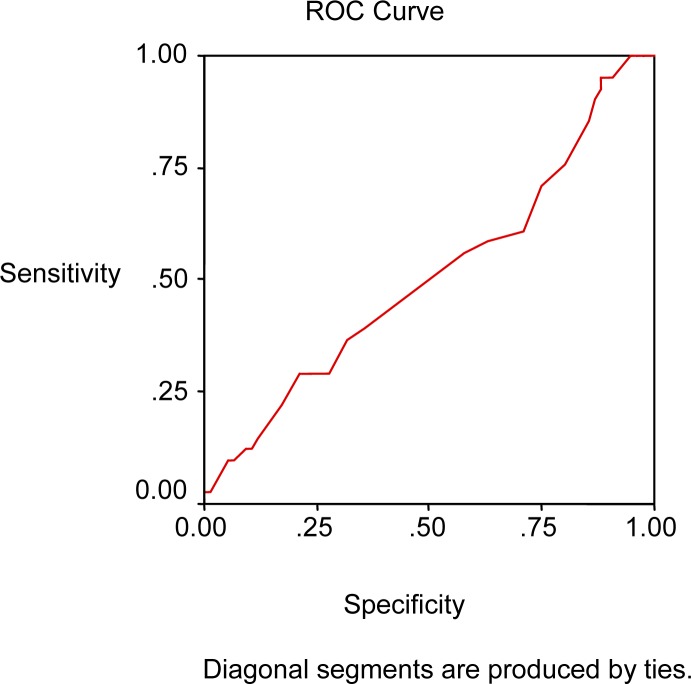
PAD was evaluated in the CT-scan of 117 patients suffering from interstitial lung disease (ILD) and the correlation between PAD and PAP was studied. A receiver operating characteristic curve (ROC curve) which is indicative of the precision of the diagnostic test was drawn to find the cut off point for the MPAD representing PH. The area under the curve was also calculated in order to define the discriminative power of the test.
Results
PAP higher than 25 mmHg was considered as PH. PAD over 29 mm reported in the CT-scan for the diagnosis of PH in ILD patients had sensitivity of 63% and specificity of 41.5%. No significant linear correlation was found between PAD and PAP (P-value = 0.17, r = 0.15). The area under the ROC curve was calculated to be 0.49 in the cutoff point of 29 mm for determining PH (CI 95% = 0.38-0.60, P = 0.89).
Conclusion
ROC curve showed a weak discriminative power. PAD had low sensitivity and specificity in the CT-scan for the diagnosis of PH. Therefore, we conclude that CT-scan alone is not helpful in finding PH cases and further examinations are required.
Keywords: Pulmonary hypertension, Pulmonary artery, Echocardiography, CT-scan, Interstitial lung disease
INTRODUCTION
Pulmonary artery hypertension is a group of diseases characterized by a growing increase in pulmonary artery pressure that can result in right heart failure and early death (1). According to Echocardiographic criteria, PAH is defined as mean pulmonary artery pressure (MPAP) ≥ 25 mm at rest (2). Also, according to CT-scan criteria, MPAD ≥ 29 mm is indicative of PAH (3). Diagnosis of PH is always a medical dilemma due to its nonspecific clinical manifestations. However, diagnosing PH and determining its severity are essential for the prognosis and treatment planning in PH patients. Pulmonary hypertension (PH) is a significant cause of morbidity and mortality in patients suffering from pulmonary parenchymal disease (4–7). PH diagnostic methods include echocardiography and catheterization of the right heart (8). The latter is the gold standard for diagnosis of PH and the majority of studies show the lower precision of echocardiography compared with right heart catheterization for the diagnosis of PAH. However, echocardiography is a key screening method in the diagnostic algorithm because it has special advantages over invasive procedures. It is safe, portable and repeatable. Therefore, echocardiography is more practical for evaluation of PAH at the beginning of the disease and during the follow up (9). On the other hand, CT-scan is a more conventional procedure for evaluation of pulmonary diseases especially interstitial lung diseases (ILD) compared to echocardiography (10–12).
Although echocardiography is not the gold standard for the diagnosis of PAH, in this study we evaluated the correlation between the definitions of PAH by echocardiography (MPAP ≥ 25 mm) and CT-scan (MPAD ≥ 29 mm).
MATERIALS AND METHODS
In a retrospective study, 130 ILD patients presented to Masih Daneshvari Hospital during 2004-2006 who had undergone echocardiography and CT-scan at the same time were evaluated in order to find a correlation between pulmonary artery pressure in echocardiography and pulmonary artery diameter in CT-scan. Patients entered the study had interstitial lung disease and had undergone both CT-scan and echocardiography with determination of pulmonary artery pressure with a maximum of 1 month interval between the two. Among these patients, 10 cases had undergone HRCT. However, they were excluded from the study because the mediastinal image was impossible to interpret. CT-scan of 3 patients could not be studied due to motion artifact and these patients were excluded from the study as well. A total of 117 cases were eventually evaluated in this study. Study protocol was approved by the National Research Institute of Tuberculosis and Lung Disease, Masih Daneshvari Hospital. Echocardiography was conducted by the ultrasound device (ATL Ultra Sound, Nr.HDI-3500, USA) and PAP was determined by an expert cardiologist through the backflow of the tricuspid valve. The cardiologist was not aware of the CT-scan result. We defined pulmonary artery hypertension as pulmonary artery pressure over 25mmHg at rest (2). CT-scan was performed by an expert radiologist using the spiral CT-scan single detector device (Siemens, Emotion, Germany) at supine position all over the chest. Pulmonary artery diameter was measured by hand under the supervision of a radiologist in a way that diameter of the main pulmonary artery was measured at the widest part of the artery above its bifurcation. Obtained data were analyzed using SPSS software and p-value, specificity and sensitivity were calculated. A receiver operating characteristic curve (ROC curve) which is indicative of the precision of the diagnostic test was drawn to find the cut off point for the MPAD representing PH. The area under the curve was also calculated in order to define the discriminative power of the test.
RESULTS
A total of 117 patients were studied. There were 64 females (54.7%) and 53 males (45.3%). The mean age of patients was 58.96±17.66 yrs (range 12-90 yrs). The mean PAD in the CT-scan of patients was 29.63± 5.37 mm. PAD was greater than 29 mm (57.3%) in 67 patients. The mean PAP of all patients was 45.60± 21.80 mmHg. Seventy-six patients (65%) had PAP > 25 mmHg out of which 60 cases (51.3%) had PAP > 35 mmHg (Table 1). PAP > 25 mmHg was considered as PH and PAD over 29 mm reported in the CT-scan for the diagnosis of PH in ILD patients had sensitivity of 63% and specificity of 41.5%. The area under the ROC curve was calculated to be 0.49 in the cutoff point of 29 mm for determining PH (CI 95% = 0.38-0.60, P = 0.89). A weak correlation was found between PAD and PAP (r = 0.15, P-value = 0.17) (Figure 1). Age and PAD were shown to have a direct correlation (r = 0.25, P-value = 0.005). No significant correlation was found between the age and PAP (r = 0.058, P-value = 0.53). No significant correlation was found between sex and PAP (P-value = 0.22) or PAD (P-value = 0.16).
Table 1.
Pulmonary artery pressure and diameter cut off points in under study subjects.
| Variables | No. (%) | |
|---|---|---|
| Sex | Male | 64 (54.7) |
| Female | 53 (45.3) | |
| PAP > 35 | Yes | 60 (51.3) |
| No | 57 (48.7) | |
| PAP cut off:≤25 mmHg | 41 (35) | |
| PAP cut off:>25 mmHg | 76 (65) | |
| PAD cut off:≤29 mmHg | 50 (42.7) | |
| PAD cut off:>29 mmHg | 67 (57.3) |
Figure 1.
Area under the Roc curve.
| Area | Std. errora | Asymptotic sig.b | Asymptotic 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| 0.508 | 0.057 | 0.893 | 0.395 | 0.620 |
The test result variable(s): CT pulmonary artery diameter has at least one tie between the positive actual state group and the negative actual state group. Statistics may be biased.
Under the nonparametric assumption
Null hypothesis: true area = 0.5
DISCUSSION
Some of the previous studies show an association between PAD and PAP. In a study by Tan and colleagues, MPAD ≥ 2 mm had sensitivity of 89% and specificity of 75% for the diagnosis of PH. However, no linear correlation was observed between the severity of PAH and MPAD (8)(r = 0.124). Burakowska and colleagues evaluated the correlation between PAP and MPAD in acute pulmonary embolism and chronic PH and a significant correlation as found between PAD in CT-scan and PAP in echocardiography of patients suffering from acute pulmonary embolism. No such correlation was found in chronic PH patients (13). In a study by NG CS and coworkers, the association between PAP and MPAD in patients under the age of 50 was significantly stronger than that of patients over the age of 50. This association was independent of gender and body surface area (3). In our study, sensitivity and specificity of CT-scan as our diagnostic test of choice for PAH were calculated to be 63% and 41.5%. Also, PAP and PAD in our study had a weak correlation. A major reason for this weak association may be the high mean age (58.96± 17.66) of our study patients. In the above mentioned studies, the diagnostic method of choice was right heart catheterization. However, since this method is not available in the majority of medical centers in our country and also considering its very high cost, we used echocardiography as the alternative method. Therefore, we cannot make a full comparison between our study results and findings of the aforementioned studies. In other words, we found a weak correlation between PAD in the CT-scan and PAP measured via echocardiography. However, according to some studies echocardiography has fewer efficacies than right heart catheterization as the gold standard for the diagnosis of PAH. In another study, PAP was measured by two methods of echocardiography and right heart catheterization in 374 patients who were lung transplantation candidates and the calculated value was 52% which shows high rate of false positive results for the diagnosis of PAH when using echocardiography (14). However, some other studies support the critical role of echocardiography in the diagnosis and follow up of PAH (9).
Since echocardiography is not the gold standard method for the diagnosis of PAH, our study results cannot be used as a reference for sensitivity and specificity of CT-scan. But, they can be used for screening purposes for PAH. In order to recommend CT-scan as the screening method for PAH, a similar study needs to be performed using right heart catheterization instead of echocardiography.
REFERENCES
- 1.Simonneau G, Galiè N, Rubin LJ, Langleben D, Seeger W, Domenighetti G, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2004;43(12 Suppl S):5S–12S. doi: 10.1016/j.jacc.2004.02.037. [DOI] [PubMed] [Google Scholar]
- 2.Barst RJ, McGoon M, Torbicki A, Sitbon O, Krowka MJ, Olschewski H, et al. Diagnosis and differential assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2004;43(12 Suppl S):40S–47S. doi: 10.1016/j.jacc.2004.02.032. [DOI] [PubMed] [Google Scholar]
- 3.Ng CS, Wells AU, Padley SP. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging. 1999;14(4):270–8. doi: 10.1097/00005382-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Grossman W, Alpert JS, Braunwald E. Heart disease, a textbook of cardiovascular medicine. 4th ed. Philadelphia: WB Saunders; 1992. Pulmonary hypertension; pp. 790–816. [Google Scholar]
- 5.Murphy ML, Dinh H, Nicholson D. Chronic cor pulmonale. Dis Mon. 1989;35(10):653–718. doi: 10.1016/0011-5029(89)90009-6. [DOI] [PubMed] [Google Scholar]
- 6.Palevsky HI, Fishman AP. Chronic cor pulmonale. Etiology and management. JAMA. 1990;263(17):2347–53. [PubMed] [Google Scholar]
- 7.Wiedemann HP, Matthay RA. Cor pulmonale in chronic obstructive pulmonary disease. Circulatory pathophysiology and management. Clin Chest Med. 1990;11(3):523–45. [PubMed] [Google Scholar]
- 8.Tan RT, Kuzo R, Goodman LR, Siegel R, Haasler GB, Presberg KW. Utility of CT-scan evaluation for predicting pulmonary hypertension in patients with parenchymal lung disease. Medical College of Wisconsin Lung Transplant Group. Chest. 1998;113(5):1250–6. doi: 10.1378/chest.113.5.1250. [DOI] [PubMed] [Google Scholar]
- 9.Ginghină C, Muraru D, Vlădaia A, Jurcut R, Popescu BA, Călin A, et al. Doppler flow patterns in the evaluation of pulmonary hypertension. Rom J Intern Med. 2009;47(2):109–21. [PubMed] [Google Scholar]
- 10.Bozlar U, Ors F, Deniz O, Uzun M, Gumus S, Ugurel MS, et al. Pulmonary Artery Diameters Measured by Multidetector-Row Computed Tomography in Healthy Adults. Acta Radiol. 2007:1–6. doi: 10.1080/02841850701545755. [DOI] [PubMed] [Google Scholar]
- 11.Sanal S, Aronow WS, Ravipati G, Maguire GP, Belkin RN, Lehrman SG. Prediction of moderate or severe pulmonary hypertension by main pulmonary artery diameter and main pulmonary artery diameter/ascending aorta diameter in pulmonary embolism. Cardiol Rev. 2006;14(5):213–4. doi: 10.1097/01.crd.0000181619.87084.8b. [DOI] [PubMed] [Google Scholar]
- 12.Kuriyama K, Gamsu G, Stern RG, Cann CE, Herfkens RJ, Brundage BH. CT-determined pulmonary artery diameters in predicting pulmonary hypertension. Invest Radiol. 1984;19(1):16–22. doi: 10.1097/00004424-198401000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Burakowska B, Pawlicka L, Oniszh K, Burakowski J, Kurzyna M, Kober J, et al. Value of spiral computed tomography in pulmonary hypertension. Pol Arch Med Wewn. 2004;111(4):431–41. [PubMed] [Google Scholar]
- 14.Arcasoy SM, Christie JD, Ferrari VA, Sutton MS, Zisman DA, Blumenthal NP, et al. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Respir Crit Care Med. 2003;167(5):735–40. doi: 10.1164/rccm.200210-1130OC. [DOI] [PubMed] [Google Scholar]