Abstract
Central airway stenosis may be a manifestation of benign or malignant lesions and can be a life threatening condition.
There are different surgical and endoscopic modalities for treatment of these lesions. Balloon bronchoscopy is an interventional pulmonologic modality and can be performed under direct vision or fluoroscopic guidance.
This technique can be used along with other interventional modalities for treatment of patients with tracheal stenosis.
In this study we report balloon bronchoscopy as an interventional modality in a series of patients with tracheal stenosis and assess the outcome.
Keywords: Tracheal stenosis, Balloon bronchoplasty
INTRODUCTION
Central airway stenosis may occur as the result of benign or malignant lesions and may be of congenital or acquired origin. These lesions include primary malignant tumors like adenoid cystic carcinoma, carcinoid tumor, bronchogenic carcinoma, mucoepidermoid tumor, and malignant metastatic tumors like renal cell carcinoma, breast cancer, colon cancer, thyroid cancer, sarcoma and melanoma. Benign causes of central airway stenosis include iatrogenic causes like stenosis following long term intubation, obstruction following stenting and stenosis at the site of surgical anastomosis, and also infectious causes like tuberculosis, epiglottitis, and papillomatosis. Congenital causes, inflammatory causes, and autoimmune causes like Wegener's granulomatosis, recurrent polychondritis, sarcoidosis, amyloidosis and other causes like goiter, tracheomalacia, bronchomalacia, mucus plug and blood clot (1–9).
Tracheal stenosis especially of iatrogenic origin is among the problems of contemporary medicine and has an increasing trend due to the increased number of ICUs all over the country that admit critically ill patients and start the treatment without following the necessary guidelines for prevention of intubation complications (10).
Suggested techniques for treatment of airway stenoses include surgical and endoscopic interventions.
Surgical interventions include use of tracheostomy to pass the stricture and maintain an adequate airway or surgical resection of the stricture and if possible, resecting the tumor and anastomosing the 2 free tracheal ends into each other.
Among endoscopic procedures we can mention balloon bronchoplasty, Bougie dilatation, cryotherapy, electrocautery (11), laser, stent placement, brachytherapy (12), photoresection (13) and APC. Most of these procedures can be performed by both rigid and flexible bronchoscope. However, rigid bronchoscopy provides better control of the airways along with proper ventilation for the patient (14, 15).
For tracheal stenoses that are not associated with tracheal destruction, 3 times dilation with rigid bronchoscope and procedures like laser, APC, mitomycin application and electrocautery are performed and then the patient undergoes resection and anastomosis surgery.
Dilation with rigid bronchoscope is associated with a high rate of recurrence. One of the reasons for recurrence following dilation is mucosal injury. The lower the rate of mucosal injury, the lower the risk of recurrence (10). Infection in the stenotic area is another reason for recurrence of stricture.
Balloon bronchoplasty (BB), also known as endoscopic balloon dilatation is a beneficial interventional treatment for both benign and malignant lesions (8, 16, 17).
BB has been used alone or in combination with other treatment modalities as an interventional method for treatment of airway obstruction (18, 19). Balloon bronchoplasty can be performed by flexible or rigid bronchoscope. It can be performed under direct vision or along with fluoroscopy. Balloon should be made of silicone and cause radial pressure.
Balloons are available in different sizes and each one can be inserted in 3 sizes. Each size applies a specific amount of pressure.
Theoretically, dilatation with balloon through causing radial pressure is associated with less mucosal injury but when using rigid bronchoscope for dilation, shearing force is created causing more mucosal injury (20). Complications of balloon bronchoscopy are few and limited to chest pain when inflating the balloon, bronchospasm or atelectasis. Other more severe complications may include rupture of the airway as the result of over-inflation of the balloon, pneumothorax, pneumomediastinitis and bleeding. In the primary studies, dilatation with angioplasty balloon was used for more severe strictures while balloon and alveoloplasty were performed for milder strictures (21, 16).
In this study, we discuss BB as a method for treating airway stenosis to further explain this method and evaluate its outcome in a few patients.
MATERIALS AND METHODS
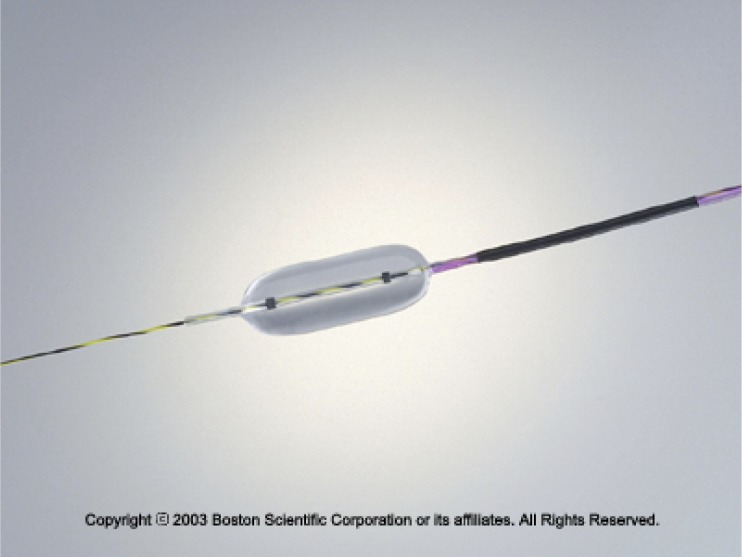
In this study a balloon dilator (Boston Scientific Corporation) matching the size and type of stricture was used.
Understudy patients had tracheal stenosis due to long term intubation, inflammatory lesions, or autoimmune diseases or stenosis at the anastomosis site after lung transplant.
After performing flexible bronchoscopy and evaluating the status and length of stricture, patients were selected for the procedure. The required pressure for dilatation based on the diameter of balloon and stricture has been suggested by the manufacturer.
Boston Scientific Corporation balloon sizes that are used in our center are as follows:
8, 9, 10 mm causing 3, 5.5, and 9 atmospheric pressures, respectively
10, 11, 12 mm causing 3, 5 and 8 atmospheric pressures, respectively
12, 13.5 and 15 mm causing 3, 4.5 and 8 atmospheric pressures, respectively
15, 16.5, 18 mm causing 3, 4.5 and 7 atmospheric pressures, respectively
18, 19, 20 mm causing 3, 4.5 and 6 atmospheric pressures, respectively (Figures are from www.bostonscientific.com)
The mentioned sizes are the outer circumference of the balloon in mm after inflation.
Deflated balloon is inserted into the bronchoscope, passes the stricture and then is inflated using an inflator gun with designated pressures.
Figure 1.
Balloon and guide wire
At first, the balloon is inflated in its smallest size and maintained for 2 minutes. Then, it is deflated and extracted. In the next phase, the balloon is inflated with higher pressure and in the third phase the highest pressure is used.
For web-like strictures APC probe was used. Before dilation, 3 radial incisions were made at 4, 8 and 12 o'clock on the web and then balloon dilator was used for dilation of stricture.
Case 1
Our first patient was a 22 year-old male with tracheal stenosis following long term intubation in the ICU after trauma. Due to the very severe stenosis, tracheostomy had been done for patient. Subglottic stenosis above the tracheostomy had caused almost 99% obstruction. Rigid bronchoscope could not pass the stenotic site.
At first, APC was used for radial incisions and then the lumen was dilated up to 50% using balloon dilator. By doing so, an evaluable lumen was obtained. Mitomycin C was used locally for destruction of granulation tissue. In the next session of assessment, lumen was so dilated that did not require rigid bronchoscope or balloon dilator for further dilation. Only a small amount of granulation tissue was present that was removed with APC.
Figure 2.
Special syringe for inflating the balloon with the designated pressure.
Case 2
Our 2nd patient was a 52 year-old man and a candidate for lung transplantation that was referred to us with the stenosis of the anastomotic site. After performing fiberoptic bronchoscopy in the left main bronchus, lots of granulation tissue were observed all along the lumen. These tissues were removed using APC and then stenosis at the anastomotic site was revealed.
At this time, the stricture was dilated using balloon dilator and local mitomycin solution was applied at the dilated site.
In the 2nd session of evaluation, lumen was completely patent and acceptable. Therefore, 8*3 covered polyflex stent was inserted into the left main bronchus 1 cm past the carina. The patient died during the course of disease as the result of post-transplant sepsis.
Case 3
Our 3rd patient was an 18 year-old male with tracheal stenosis following long term intubation. Flexible bronchoscopy showed a web-like stricture in the middle segment of trachea.
After rigid bronchoscopy, 3 radial incisions were made on the stricture using APC and then dilation was performed using a balloon.
In the next 2 sessions, patient had no problem during bronchoscopy but in the 4th follow up session it was revealed that the stenosis had recurred. APC was used again and the stricture was dilated 3 times using a balloon. Local mitomycin was applied at the site of stricture. It has been 4 months since the procedure and the patient does not need another intervention so far.
Case 4
Our 4th patient was a 24 year-old female with Wegener's granulomatosis suffering from severe respiratory distress. Bronchoscopy showed a very severe subglottic stenosis. After maintaining a safe airway and performing tracheostomy the patient underwent bronchoscopy and intervention. First rigid bronchoscopy and dilation of the stricture were done but the stenosis relapsed. In the 2nd session, after performing APC the stricture was dilated 3 times using a balloon. Methyl prednisolone was injected at the stenotic site and mitomycin was applied.
In the next session, dilation was not needed and only injection of methyl prednisolone and local application of mitomycin were done.
Case 5
Our 5th patient was a 20 year-old female with bronchiectasis. She had a stricture in LMB. Radial APC was performed at the stenotic site and then the site was dilated 3 times using a balloon. No recurrence was observed afterwards and no further intervention was required.
Case 6
Our 6th patient was a candidate of lung transplantation. In LMB, he had a very severe stenosis at the site of anastomosis. Rigid bronchoscopy could not pass the lesion. After performing fiberoptic bronchoscopy the stricture was radially cut in 3 points using APC and then was dilated 3 times with a balloon.
Case 7
This patient was a 34 year-old woman with tracheal stenosis following long term intubation. Bronchoscopy showed a web-like stricture in the middle of trachea. Using APC, 3 radial incisions were made in the stricture and then the stenotic site was dilated using balloon dilator. Mitomycin was applied at the site of stricture. The patient had no recurrence after 9 months of follow up.
Case 8
The patient was a 16 year-old male with tracheal stenosis following long term intubation. Bronchoscopy revealed a stricture of 2 mm diameter and 5 cm length at the upper trachea. The patient underwent intervention and the stricture was dilated 3 times using a balloon. Mitomycin was then applied at the site. This procedure was repeated 3 times. In the next follow up 4 months later severe relapse of the stenosis was observed at the same location and the patient was eventually referred for resection and anastomosis surgery.
Case 9
Case 9 was a 26 year-old woman presented with tracheal stenosis of unknown cause. Bronchoscopy revealed a limited stenosis in the subglottic area. The stricture was first electrocauterized and then balloon dilation was performed. In the follow up session 1 month later, no sign of stenosis was detected.
Case 10
This patient was a 27-year-old man suffering from subglottic stenosis following long term intubation who had undergone surgical resection and anastomosis. However, the stricture relapsed at the site of anastomosis. The stricture was removed by APC to some extent. Balloon dilation and another APC were then performed. In the next session, the stricture had relapsed in the form of web which was dilated using a balloon. In the next session, mild recurrence was observed in the same site. Rigid bronchoscopy was done this time which resulted in full recovery of patient.
DISCUSSION
Advancements in bronchology and development of various invasive diagnostic and treatment methods known as interventional pulmonology in the recent years have set new horizons in the field of lung diseases. In previous reports, parts of the activities of interventional pulmonology unit of Masih Daneshvari Hospital, Shahid Beheshti University of Medical Sciences were published (22, 23).
Tracheal stenosis is among the most important complications that we encounter in this unit every day and people from all over the country suffering from this condition are referred to this unit for diagnosis and treatment.
Tracheal stenosis is one of the most common complications of long term intubation in patients hospitalized in the ICU. Considering the annual incidence rate of accidents and disasters in our country, high number of admissions to the ICU and repeated and sometimes long term intubations for patients with reduced level of consciousness due to cardiovascular diseases, cerebrovascular accidents, head traumas and etc. We can estimate the incidence of tracheal stenosis to be high in our country.
The most definite and well known treatment modality for tracheal lesions is open surgery as resection of the stricture and end to end anastomosis. This is a major operation and requires pre and post-op measures. However, if the stricture has not resulted in destruction of the tracheal cartilages and is web like or made of granulation tissue that does not damage the cartilage, surgery is not required and the lesion usually responds well to interventional procedures. To date, many endoscopic interventions have been tested and used for this purpose.
Limited studies have evaluated the use of BB along with other therapeutic techniques for control and treatment of tracheal stenosis (20).
Ferretti et al. studied 19 patients with airway stenosis and detected that 50% of strictures were in the main bronchi. Of 19 patients, 13 responded well to balloon dilation out of which 7 developed recurrence during a 30 day period. By repeating the procedure, 3 out of 7 recovered. In general, 9 patients in a follow up period of 21 months responded well to balloon bronchoplasty alone (24).
Mathur and Sheski used balloon bronchoplasty in 14 patients with benign lesions out of which, 10 were successfully treated after a long treatment course (10).
Also, there are reports regarding treatment of strictures due to sarcoidosis and tuberculosis in the main airways with BB (25–27).
In a study on patients whose strictures had been dilated with balloon, long-term maintenance of an open trachea was reported to be 50%. This rate was more than expected in fibrotic stenosis (8). In this study pyloroplasty balloon with the length of 5 cm was used. Dilation was performed in one patient with a 5 cm length and 2mm diameter stricture. Recurrence did not occur until 4 months post-operatively but eventually due to severe recurrence, the patient was referred for surgery (patient number 8).
Tremblay conducted a study on 3 patients. He made radial incisions on web-like strictures at 4, 8 and 12 o'clock using electrocautery probe followed by dilation. After balloon dilatation, methyl prednisolone was injected at the site of incisions and after 16 weeks the results were satisfactory. However, number of patients was small and follow up period was short (28). Some authors have recommended the use of corticosteroid or antibiotics following dilation (7, 29).
Overall, it seems that BB is a safe method for management and treatment of tracheal stenosis that can be done easily even with a flexible bronchoscope. Studies have reported a high success rate and low failure rate for BB. However, its repeated use is sometimes required (20). This method has very rare side effects including bronchospasm, airway laceration, bleeding, pneumomediastinum, atelectasis and pneumothorax (20). Balloon rupture during the procedure is another possible complication that we encountered once but since the balloon was filled with distilled water no specific problem occurred.
CONCLUSION
Tracheal stenosis is among the serious complications of contemporary medicine especially in developing countries. Its definite treatment is resection and end to end anastomosis. Balloon bronchoplasty is an interventional modality for control and treatment of this condition. By using this method, we are able to dilate very severe strictures that cannot be dilated with rigid bronchoscope. In the present study, a series of patients with tracheal stenoses underwent BB. In most cases the stricture was managed with no specific complication or severe recurrence. Therefore, this method can be used as an appropriate safe method with good outcome for treatment of tracheal stenosis along with other treatment modalities.
Further investigations in the form of case control studies on larger populations are recommended for the assessment of the efficacy of this interventional procedure.
REFERENCES
- 1.Olsson T, Björnstad-Pettersen H, Stjernberg NL. Bronchostenosis due to sarcoidosis: a cause of atelectasis and airway obstruction simulating pulmonary neoplasm and chronic obstructive pulmonary disease. Chest. 1979;75(6):663–6. doi: 10.1378/chest.75.6.663. [DOI] [PubMed] [Google Scholar]
- 2.Nakamura K, Terada N, Ohi M, Matsushita T, Kato N, Nakagawa T. Tuberculous bronchial stenosis: treatment with balloon bronchoplasty. AJR Am J Roentgenol. 1991;157(6):1187–8. doi: 10.2214/ajr.157.6.1950862. [DOI] [PubMed] [Google Scholar]
- 3.Ferretti G, Jouvan FB, Thony F, Pison C, Coulomb M. Benign noninflammatory bronchial stenosis: treatment with balloon dilation. Radiology. 1995;196(3):831–4. doi: 10.1148/radiology.196.3.7644651. [DOI] [PubMed] [Google Scholar]
- 4.Sarodia BD, Dasgupta A, Mehta AC. Management of airway manifestations of relapsing polychondritis: case reports and review of literature. Chest. 1999;116(6):1669–75. doi: 10.1378/chest.116.6.1669. [DOI] [PubMed] [Google Scholar]
- 5.Keller C, Frost A. Fiberoptic bronchoplasty. Description of a simple adjunct technique for the management of bronchial stenosis following lung transplantation. Chest. 1992;102(4):995–8. doi: 10.1378/chest.102.4.995. [DOI] [PubMed] [Google Scholar]
- 6.Fowler CL, Aaland MO, Harris FL. Dilatation of bronchial stenosis with Gruentzig balloon. J Thorac Cardiovasc Surg. 1987;93(2):308–9. [PubMed] [Google Scholar]
- 7.Noppen M, Schlesser M, Meysman M, D'Haese J, Peche R, Vincken W. Bronchoscopic balloon dilatation in the combined management of postintubation stenosis of the trachea in adults. Chest. 1997;112(4):1136–40. doi: 10.1378/chest.112.4.1136. [DOI] [PubMed] [Google Scholar]
- 8.Hautmann H, Gamarra F, Pfeifer KJ, Huber RM. Fiberoptic bronchoscopic balloon dilatation in malignant tracheobronchial disease: indications and results. Chest. 2001;120(1):43–9. doi: 10.1378/chest.120.1.43. [DOI] [PubMed] [Google Scholar]
- 9.Ernst A, Feller-Kopman D, Becker HD, Mehta AC. Central airway obstruction. Am J Respir Crit Care Med. 2004;169(12):1278–97. doi: 10.1164/rccm.200210-1181SO. [DOI] [PubMed] [Google Scholar]
- 10.Jabbardarjani HR, Mirminachi F, Arami S, Abbasi A, Masjedi MR. Treatment of post-intubation tracheal stenosis with Nd-YAG laser. Tanaffos. 2002;1(1):36. [Google Scholar]
- 11.Koufman JA, Thompson JN, Kohut RI. Endoscopic management of subglottic stenosis with the CO2 surgical laser. Otolaryngol Head Neck Surg. 1981;89(2):215–20. doi: 10.1177/019459988108900214. [DOI] [PubMed] [Google Scholar]
- 12.Mayse ML, Greenheck J, Friedman M, Kovitz KL. Successful bronchoscopic balloon dilation of nonmalignant tracheobronchial obstruction without fluoroscopy. Chest. 2004;126(2):634–7. doi: 10.1378/chest.126.2.634. [DOI] [PubMed] [Google Scholar]
- 13.Jabardarjani HR, Dabir Sh, Edrissian MO, Masjedi MR. Nd-YAG Laser in Management of Endobronchial Lesions, a Five -Year Report. Tanaffos. 2004;3(9):19–25. [Google Scholar]
- 14.Mathisen DJ, Grillo HC. Endoscopic relief of malignant airway obstruction. Ann Thorac Surg. 1989;48(4):469–73. doi: 10.1016/s0003-4975(10)66842-7. discussion 473- 5. [DOI] [PubMed] [Google Scholar]
- 15.Jabbardarjani H, Kiani A, Sheikhi N. Argon plasma coagulation in treatment of post intubation tracheal stenosis. J Lasers Med Sci. 2011;2(2):49–53. [Google Scholar]
- 16.Noppen M, Schlesser M, Meysman M, et al. Bronchoscopic Balloon Dilatation in the Combined Management of Postintubation Stenosis of the Trachea in Adults. Chest. 1997;112(4):1136–40. doi: 10.1378/chest.112.4.1136. [DOI] [PubMed] [Google Scholar]
- 17.Carlin BW, Harrell JH, 2nd, Moser KM. The treatment of endobronchial stenosis using balloon catheter dilatation. Chest. 1988;93(6):1148–51. doi: 10.1378/chest.93.6.1148. [DOI] [PubMed] [Google Scholar]
- 18.Chhajed PN, Malouf MA, Glanville AR. Bronchoscopic dilatation in the management of benign (non-transplant) tracheobronchial stenosis. Intern Med J. 2001;31(9):512–6. doi: 10.1046/j.1445-5994.2001.00135.x. [DOI] [PubMed] [Google Scholar]
- 19.Sheski FD, Mathur PN. Long-term results of fiberoptic bronchoscopic balloon dilation in the management of benign tracheobronchial stenosis. Chest. 1998;114(3):796–800. doi: 10.1378/chest.114.3.796. [DOI] [PubMed] [Google Scholar]
- 20.McArdle JR, Gildea TR, Mehta AC. Balloon Bronchoplasty. Its Indications, Benefits, and Complications. J Bronchol. 2005;12:123–7. [Google Scholar]
- 21.Brichet A, Verkindre C, Dupont J, Carlier ML, Darras J, Wurtz A, Ramon P, Marquette CH. Multidisciplinary approach to management of postintubation tracheal stenoses. Eur Respir J. 1999;13(4):888–93. doi: 10.1034/j.1399-3003.1999.13d32.x. [DOI] [PubMed] [Google Scholar]
- 22.Jabbardarjani HR, Herth F, Kiani A, Arab A, Masjedi MR. Central Airway Obstruction Masquerading as Difficult to treat Asthma. A retrospective Study. J Bronchol Intervent Pulmonol. 2009;16(1):6–9. doi: 10.1097/LBR.0b013e318194b41b. [DOI] [PubMed] [Google Scholar]
- 23.Jabbardarjani HR, Kiani A, Arab A, et al. A Case of 50 pneumonia in 13 years. J Bronchol Intervent Pulmonol. 2009;16(2):112–14. doi: 10.1097/LBR.0b013e31819c6a20. [DOI] [PubMed] [Google Scholar]
- 24.Ferretti G, Jouvan FB, Thony F, Pison C, Coulomb M. Benign noninflammatory bronchial stenosis: treatment with balloon dilation. Radiology. 1995;196(3):831–4. doi: 10.1148/radiology.196.3.7644651. [DOI] [PubMed] [Google Scholar]
- 25.Iles PB. Multiple bronchial stenoses: treatment by mechanical dilatation. Thorax. 1981;36(10):784–6. doi: 10.1136/thx.36.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ball JB, Delaney JC, Evans CC, Donnelly RJ, Hind CR. Endoscopic bougie and balloon dilatation of multiple bronchial stenoses: 10 year follow up. Thorax. 1991;46(12):933–5. doi: 10.1136/thx.46.12.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee KW, Im JG, Han JK, Kim TK, Park JH, Yeon KM. Tuberculous stenosis of the left main bronchus: results of treatment with balloons and metallic stents. J Vasc Interv Radiol. 1999;10(3):352–8. doi: 10.1016/s1051-0443(99)70042-4. [DOI] [PubMed] [Google Scholar]
- 28.Tremblay A, Coulter DT, Mehta AC. Modification of a Mucosal-Sparing Technique Using Electrocautery and Balloon Dilatation in the Endoscopic Management of Web-Like Benign Airway Stenosis. J Bronchol. 2003;10:268–71. [Google Scholar]
- 29.Shapshay SM, Beamis JF, Jr, Hybels RL, Bohigian RK. Endoscopic treatment of subglottic and tracheal stenosis by radial laser incision and dilation. Ann Otol Rhinol Laryngol. 1987;96(6):661–4. doi: 10.1177/000348948709600609. [DOI] [PubMed] [Google Scholar]