Abstract
Background
Cadavers are preserved in a fixing solution containing formalin. Formaldehyde (FA) released from formalin is inhaled by the personnel in the anatomy laboratory. Exposed personnel have reported respiratory problems and various symptoms. Due to the toxicity of FA as a strong irritant and carcinogen and also lack of a national study assessing occupational exposure to FA in gross anatomy labs in Iran, the present study aimed at occupational monitoring of personnel exposed to FA and evaluating relevant symptoms in them.
Materials and Methods
A total of 20 subjects (all the staff) working in a gross anatomy lab and 20 library personnel were considered for occupational monitoring of exposure to FA during three months with various climatic conditions. They were also monitored for respiratory symptoms. Air sampling and analysis of its FA content were conducted according to the NIOSH method No.2016. Symptoms of cases and controls (library personnel) with active and passive exposure to formaldehyde were also studied by a self-report questionnaire.
Results
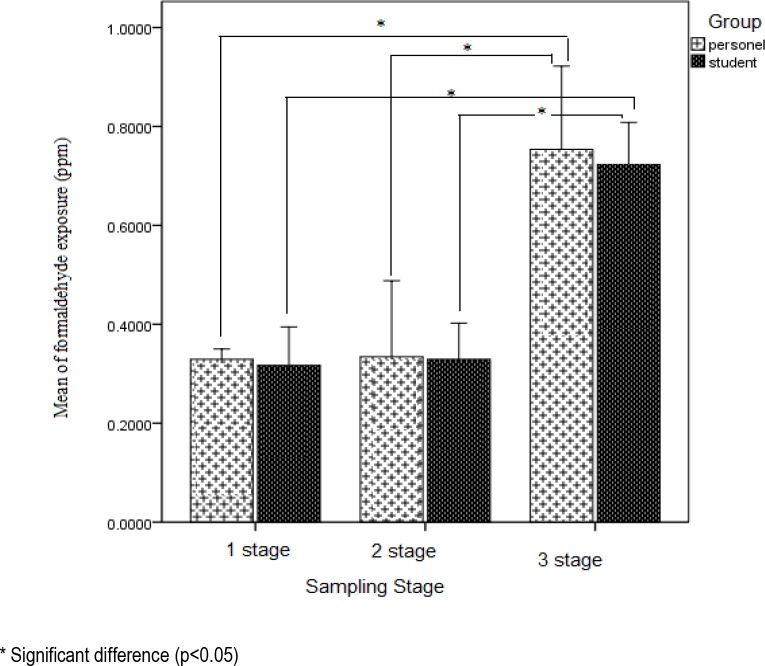
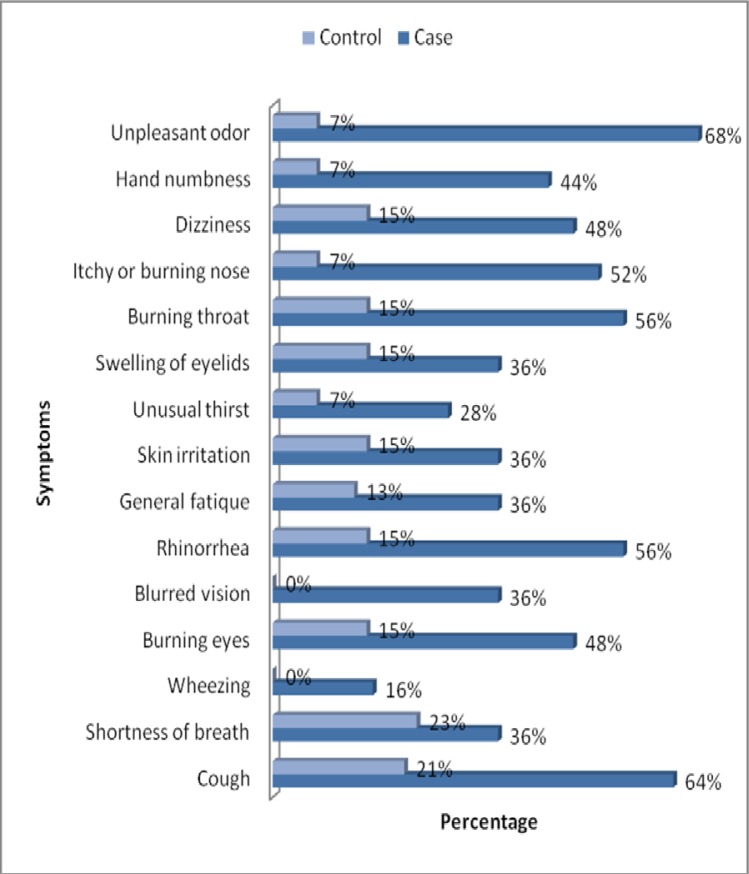
In the first stage of monitoring with ventilation (supply-exhaust) system on, the exposure of personnel (Mean± SE) was 306 ± 21ppb. In the second stage of monitoring the personnel's exposure was 317 ± 26ppb with only the ventilation supply system on and in the final monitoring stage this rate was 698 ± 34ppb with the ventilation system (supply and exhaust) off. In this study, personal's exposure level to FA was higher than the indoor concentration, and the individual exposure levels of instructors were higher than those of the students. Exposure of library personnel in the adjacent department (central library) was about 50ppb. Most important complaints reported by actively exposed staff members and library personnel were the unpleasant odor (68%), cough (64%), throat irritation and runny nose (56%), burning and itching of nose (52%) and irritating eyes (48%).
Conclusion
Considering the level of exposure of all subjects in this study and existence of clinical symptoms, better control of the exhaust system in the gross anatomy lab and use of a more efficient ventilation system are recommended to protect the staff and instructors of the Anatomy Department.
Keywords: Formaldehyde, Personal monitoring, Respiratory symptoms
INTRODUCTION
Cadavers in gross anatomy laboratories are kept in formaldehyde for a longtime. Formaldehyde vapors are emitted from cadavers during dissection, and significant exposure of staff and students has been reported (1). Formaldehyde is a highly reactive one-carbon compound and a very strong irritant (2). World production of formaldehyde in 2006 was 31,912 kt (3). Respiratory symptoms following formaldehyde exposure at low concentrations include irritation of eyes, nose, and upper respiratory airways (4) and nerve toxicity (5) Higher FA concentrations may result in irritation of lower respiratory airways, impairment of pulmonary function and asthma(6, 7). The nasopharyngeal cancer (8, 9) and myeloid leukemia (10–12) in humans have been observed in cases with long term exposure. The American Conference of Government Industrial Hygienist (ACGIH) has established a ceiling limit for occupational exposure (Threshold limit value) of 300 ppb (13). International Agency for Research on Cancer (IARC) In June 2004 classified formaldehyde as a known human carcinogen (group 1) (14). Khanzadeh et al. reported the range of concentration of formaldehyde in gross anatomy laboratory of a Medical College in Ohio, United States as 70-2940ppb (15). Kurose et al. reported formaldehyde concentrations in the range of 250-550ppb in a gross anatomy laboratory (16). In addition, the range of formaldehyde concentration in the indoor air of a dissection room in Australia was 59-219 ppb (17). The present study aimed at occupational monitoring of personnel exposed to FA and their relevant symptoms in three consecutive months with different conditions of ventilation.
MATERIALS AND METHODS
The dimensions of the gross anatomy laboratory were 4.2m × 6.10m × 3.13m (339 m3). In this Laboratory there were four doors in one side of laboratory. All doors remain closed when not in use. The dissection room also has permanently closed glass windows along one side of the room. Six ceiling diffusers arranged in two rows are attached to the central air conditioning system and four exhausts provide general ventilation for the laboratory. Cadavers are wrapped in cotton cloth and kept in a vinyl bag while not in use. During the study, nine cadavers were placed over the tables. Containers and barrels containing formaldehyde and phenol are also located in this Laboratory.
Due to the limited number of instructors (n=6), technicians (n=3) and graduate students (n=11) working in the anatomy lab, all the personnel (n=20) and all the librarians as the control population (n=12) were entered the study. The objectives of this study were explained to all participants and their consent was obtained. Air sampling of formaldehyde in the breathing zone was based on the 2016-NIOSH method. Sample flow rate was 0.1 lit/min and sampling was done for 2 hours through SKC company sorbent tubes (silica gel coated with 2,4 Dinitrophenylhydrazine catalog No. 119-226). Subsequently, Sorbent tubes were extracted by acetonitrile and analyzed by Merck Hitachi High Performance Liquid Chromatography (HPLC). Ultraviolet detector was equipped with stainless steel column, and packed with 5µm C-18 (18). An indoor sample from the center and 4 samples from the corners of the gross anatomy laboratory were collected. The air of corridors, moulage room and classroom was also sampled at breathing height by using moulage. Individual exposures to FA were evaluated in consecutive months with three different climates. In the first stage of monitoring in October, supply and exhaust ventilation system was on. In the second stage in November, only the supply ventilation system was on and in the final stage in December, ventilation systems (supply and exhaust) were off. Dissection sessions usually last for 2 hours. OSHA's self-report questionnaires (19) were completed by all the anatomy lab personnel and library staff and percentage of reported symptoms was determined.
Mean and standard error values were determined for all exposures and results were expressed as Mean ± SE. Repeated measures linear model was used to find differences in exposure levels in three tests. All statistical calculations were done using SPSS version 18.0 software.
RESULTS
The validity of 2016-NIOSH method was reestablished in the laboratory. During the first two stages of monitoring, air pressure in the gross anatomy laboratory was positive. In the third stage, one air change per hour as natural air change was estimated. Individual exposure to formaldehyde (mean ± standard error) in the first, second and third trials was 306±21, 317±26 and 698±34 ppb, respectively. Difference in exposures between first and third, and second and third stages of monitoring was statistically significant (p<0.05)( Figure 1).
Figure 1.
Comparison of formaldehyde exposure (ppm) in the three-stage sampling
Results of personnel's monitoring for exposure to formaldehyde in three groups are presented in Table 1. Exposure level of instructors was higher than that of students and technicians. Results of sampling from different parts of the anatomy department in three different modes of ventilation are presented in Table 2.
Table 1.
Occupational monitoring of personnel to formaldehyde (ppb)
Table 2.
Indoor air concentrations of formaldehyde in ppb
| Sampling place Mode of Ventilation | Indoor Anatomy Laboratory | corridor | Moulage | Classroom |
|---|---|---|---|---|
| Exhaust-supply | 256 | 221 | 232 | 206 |
| Supply | 270 | 241 | 253 | 228 |
| Off | 572 | 445 | 463 | 315 |
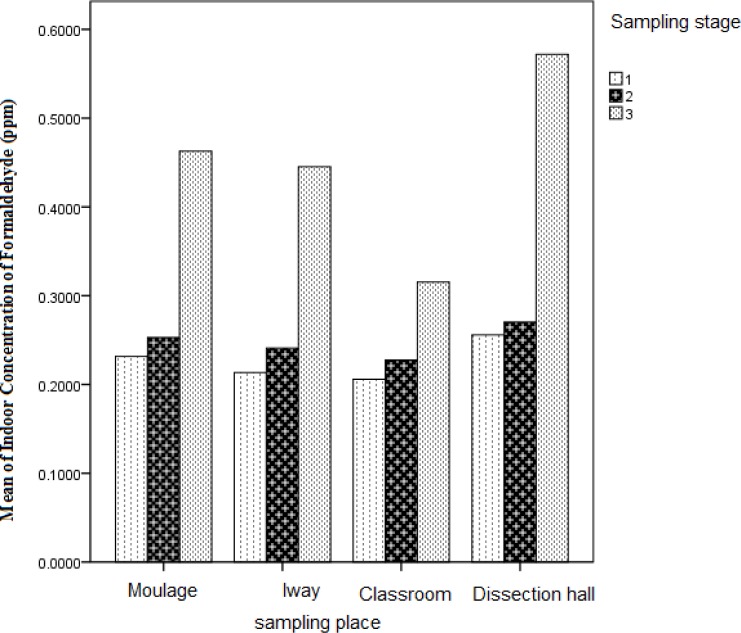
Magnitudes of general indoor concentrations were different in various places of Anatomy Department with higher concentrations in gross anatomy laboratory compared to moulage rooms, corridor and classrooms (Table and Figure 2).
Figure 2.
Comparison of formaldehyde concentration (ppm) in anatomy department
General Indoor concentration of formaldehyde in the library was measured as 50ppb. Prevalence of symptoms due to formaldehyde exposure was greater in cases than in controls (Figure 3). The most commonly reported complaints were unpleasant odor (68%), cough (64%), sore throat and runny nose (56%), nasal irritation and itching (52%) and eye irritation (48%).
Figure 3.
Percentage of clinical symptoms
DISCUSSION
As observed in this study in regard to occupational and environmental exposures from first and second stages, it shows that the ventilation system can reduce the magnitude of exposures, though, differences were not statistically significant. However, comparing the magnitude of exposures between the first and third and second and third monitoring, statistically significant in higher exposures were observed. Considering the uniformity of operations in gross anatomy laboratory, the role of ventilation in reduction of exposures is quite evident.
Based on the standards of occupational hygiene, approximately the exposure of all subjects to FA in the first and second trial of examination was lower than OSHA's Permissible Exposure Limit (750ppb)(20), and only 35% in the third trial had higher exposure than PEL. Comparing exposures levels with Threshold Limit Value-Ceiling by ACGIH (13), about fifty percent of all subjects’ exposure to FA in the first and second stages of monitoring was higher than TLV-C (300ppb), but hundred percent of all subjects in the third stage had exposures higher than TLV-C.
Since the threshold limit value for occupational exposure to formaldehyde is defined as ceiling (TLV-C) due to the severe irritating properties of this compound, the exposures of personnel in the Anatomy Department may result in short term complications such as: lower respiratory airways irritation, impairment of pulmonary function and asthma. Nasopharyngeal cancer (6–9) and myeloid leukemia may occur due to the long term exposures (10–12).
Studies by Costa et al in Portugal (21) and Lakchayapakorn in Thailand (22) reported exposure rates similar to those of our subjects. But Kunugita et al, in Japan (23) reported higher exposure rates than the present study. Higher exposure in Japan can be explained by the greater number of fresh cadavers in the gross anatomy laboratories. Higher exposure of instructors compared to students and technicians in our study was similar to a study in Saudi Arabia (24) which might be due to the fact that instructors stand closer to the cadavers than students.
The average individual exposure level to FA in the gross anatomy laboratory as the result of direct work with cadavers in the present study was higher than the average general indoor concentrations and this finding is consistent with similar previous studies (22, 24, 25).
In addition to measuring the general indoor concentration of formaldehyde in the gross anatomy laboratory, other parts of the Anatomy department were also monitored which has not been done in similar studies. As expected, formaldehyde concentrations in areas closer to the laboratory in all three modes of ventilation, were higher than other areas. Relatively high concentrations of formaldehyde in the moulage room and corridor can be explained by the diffusion of formaldehyde due to positive air pressure in the dissection room. General indoor concentrations of formaldehyde in central library which is relatively close to the Anatomy Department were measured as 50 ppb. Local exhaust ventilation is strongly recommended to control vapors of organic liquids and keep the occupational exposure limit below 100 (26, 27).
The most common complaints reported in other studies were: unpleasant odor (68%), cough (64%), sore throat and runny nose (56%), nasal irritation and itching (52%) and eye irritation (48%). Other authors also reported respiratory problems and burning eyes, runny nose, general fatigue and skin irritation (17, 22, 23, 28 and 29). In this study a few complaints and symptoms were noticed in the control population.
Considering the level of exposure of subjects in this study and incidence of clinical symptoms observed, it can be concluded that the available general ventilation system is not fully capable of reducing the concentration of harmful vapors in the gross anatomy laboratory. The exhausted air flow rate must be 5% more than supplied air flow rates (e.g., Qexhaust= 1.05 Qsupply)(30) and installation of dissection tables equipped with local exhaust ventilation system introduced by Kunugita and Yamato studies in Japan (23, 31) is recommended. In addition, alternative compounds such as Shellac (32), glutaraldehyde, fixing solutions with low concentrations of formaldehyde and formaldehyde to water ratio 1:3 (33), ammonium carbonate (34) and salt-containing solutions can also be used (35).
REFERENCES
- 1.Takayanagi M, Sakai M, Ishikawa Y, Murakami K, Kimura A, Kakuta S, et al. Formaldehyde concentrations in the breathing zone of medical students during gross anatomy laboratory in Toho University. Kaibogaku Zasshi. 2007;82(2):45–51. [PubMed] [Google Scholar]
- 2.Çelik HH, Sargon MF, Çelik MH, Uslu SS, Çelik TH. A Review of the Health Effects of Formaldehyde Toxicity. Morphology J. 2001;9:1–12. [Google Scholar]
- 3.Tang X, Bai Y, Duong A, Smith MT, Li L, Zhang L. Formaldehyde in China: production, consumption, exposure levels, and health effects. Environ Int. 2009;35(8):1210–24. doi: 10.1016/j.envint.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Pala M, Ugolini D, Ceppi M, Rizzo F, Maiorana L, Bolognesi C, et al. Occupational exposure to formaldehyde and biological monitoring of Research Institute workers. Cancer Detect Prev. 2008;32(2):121–6. doi: 10.1016/j.cdp.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Songur A, Ozen OA, Sarsilmaz M. The toxic effects of formaldehyde on the nervous system. Rev Environ Contam Toxicol. 2010;203:105–18. doi: 10.1007/978-1-4419-1352-4_3. [DOI] [PubMed] [Google Scholar]
- 6.Noisel N, Bouchard M, Carrier G. Evaluation of the health impact of lowering the formaldehyde occupational exposure limit for Quebec workers. Regul Toxicol Pharmacol. 2007;48(2):118–27. doi: 10.1016/j.yrtph.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 7. Formaldehyde CAS Registry Number50-00-0[cited; Available from: http://oehha.ca.gov/air/toxic_contaminants/pdf_zip/formaldehyde_final.pdf]
- 8.Shiraishi N. Levels of Formaldehyde, Phenol and Ethanol in Dissection Room Air and Measures for Reduction. Japanese Journal of Occupational Medicine and Traumatology. 2006;54(1):1–10. [Google Scholar]
- 9.Dimenstein IB. A Pragmatic Approach to Formalin Safety in Anatomical Pathology. Lab Medicine. 2009;40(12):740–6. [Google Scholar]
- 10.Hauptmann M, Lubin JH, Stewart PA, Hayes RB, Blair A. Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries. J Natl Cancer Inst. 2003;95(21):1615–23. doi: 10.1093/jnci/djg083. [DOI] [PubMed] [Google Scholar]
- 11.Zhang L, Tang X, Rothman N, Vermeulen R, Ji Z, Shen M, et al. Occupational exposure to formaldehyde, hematotoxicity, and leukemia-specific chromosome changes in cultured myeloid progenitor cells. Cancer Epidemiol Biomarkers Prev. 2010;19(1):80–8. doi: 10.1158/1055-9965.EPI-09-0762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suruda A, Schulte P, Boeniger M, Hayes RB, Livingston GK, Steenland K, et al. Cytogenetic effects of formaldehyde exposure in students of mortuary science. Cancer Epidemiol Biomarkers Prev. 1993;2(5):453–60. [PubMed] [Google Scholar]
- 13.American Conference of Industrial Hygienists (ACGIH) Threshold Limit Values for Chemical Substances and Physical Agents & Biological Exposure Indices (TLVs ® and BEIs); 2010. [Google Scholar]
- 14.Agents Classified by the IARC Monographs. Volumes 1–100 [Available from: www.monographs.iarc.fr/ENG/.../ClassificationsGroupOrder.pdf]
- 15.Akbar-Khanzadeh F, Vaquerano MU, Akbar-Khanzadeh M, Bisesi MS. Formaldehyde exposure, acute pulmonary response, and exposure control options in a gross anatomy laboratory. Am J Ind Med. 1994;26(1):61–75. doi: 10.1002/ajim.4700260106. [DOI] [PubMed] [Google Scholar]
- 16.Kurose T, Kodera H, Aoyama H, Kawamata S. Formaldehyde concentration in the air and in cadavers at the gross anatomy laboratory in Hiroshima University. Hiroshima J Med Sci. 2004;53(3-4):33–7. [PubMed] [Google Scholar]
- 17.Wantke F, Focke M, Hemmer W, Tschabitscher M, Gann M, Tappler P, et al. Formaldehyde and phenol exposure during an anatomy dissection course: a possible source of IgE-mediated sensitization? Allergy. 1996;51(11):837–41. doi: 10.1111/j.1398-9995.1996.tb00031.x. [DOI] [PubMed] [Google Scholar]
- 18.Formaldehyde: Method 2016; 2003. Mar 15, NIOSH Manual of Analytical Methods (NMAM), Fourth Edition; pp. 2–7. [Available from: www.cdc.gov/niosh/docs/2003-154/pdfs/2016.pdf. [Google Scholar]
- 19.Arizona State University (ASU) Department of Environmental Health & Safety: Formaldehyde Exposure Management Plan; 2002. May, pp. 14–22. Pursuant to 29 CFR 1910.1048. [Google Scholar]
- 20.Occupational Safety and Health Administration (OSHA) Safety and Health Topics: Formaldehyde – OSHA Standards. 2004. Available at: https://www.osha.gov/SLTC/formaldehyde/index.html#standards.
- 21.Costa S, Coelho P, Costa C, Silva S, Mayan O, Santos LS, et al. Genotoxic damage in pathology anatomy laboratory workers exposed to formaldehyde. Toxicology. 2008;252(1-3):40–8. doi: 10.1016/j.tox.2008.07.056. [DOI] [PubMed] [Google Scholar]
- 22.Lakchayapakorn K, Watchalayarn P. Formaldehyde exposure of medical students and instructors and clinical symptoms during gross anatomy laboratory in Thammasat University. J Med Assoc Thai. 2010;93(Suppl 7):S92–8. [PubMed] [Google Scholar]
- 23.Kunugita N, Nakashima T, Kikuta A, Kawamoto T, Arashidani K. Exposure to formaldehyde during an anatomy dissecting course. J UOEH. 2004;26(3):337–48. doi: 10.7888/juoeh.26.337. [DOI] [PubMed] [Google Scholar]
- 24.Vohra MS. Personal formaldehyde exposure level in the gross anatomy dissecting room at College of Medicine King Saud University Riyadh. Int J Occup Med Environ Health. 2012;24(1):108–13. doi: 10.2478/s13382-011-0004-4. [DOI] [PubMed] [Google Scholar]
- 25.Ohmichi K, Komiyama M, Matsuno Y, Takanashi Y, Miyamoto H, Kadota T, et al. Formaldehyde exposure in a gross anatomy laboratory--personal exposure level is higher than indoor concentration. Environ Sci Pollut Res Int. 2006;13(2):120–4. doi: 10.1065/espr2005.06.265. [DOI] [PubMed] [Google Scholar]
- 26.ACGIH. 22nd Edition. ACGIH; 1995. Industrial Ventilation A Manual of Recommended Practice. [Google Scholar]
- 27.Jafari MJ, Karimi A, Rezazadeh Azari M. The challenges of controlling organic solvents in a paint factory due to solvent impurity. Ind Health. 2009;47(3):326–32. doi: 10.2486/indhealth.47.326. [DOI] [PubMed] [Google Scholar]
- 28.Takahashi S, Tsuji K, Fujii K, Okazaki F, Takigawa T, Ohtsuka A, et al. Prospective study of clinical symptoms and skin test reactions in medical students exposed to formaldehyde gas. J Dermatol. 2007;34(5):283–9. doi: 10.1111/j.1346-8138.2007.00274.x. [DOI] [PubMed] [Google Scholar]
- 29.Mizuki M, Tsuda T. Relationship between atopic factors and physical symptoms induced by gaseous formaldehyde exposure during an anatomy dissection course. Arerugi. 2001;50(1):21–8. [PubMed] [Google Scholar]
- 30.Jafari MJ, Karimi A, Azari MR. The role of exhaust ventilation systems in reducing occupational exposure to organic solvents in a paint manufacturing factory. Indian J Occup Environ Med. 2008;12(2):82–7. doi: 10.4103/0019-5278.43266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamato H, Nakashima T, Kikuta A, Kunugita N, Arashidani K, Nagafuchi Y, et al. A novel local ventilation system to reduce the levels of formaldehyde exposure during a gross anatomy dissection course and its evaluation using real-time monitoring. J Occup Health. 2005;47(5):450–3. doi: 10.1539/joh.47.450. [DOI] [PubMed] [Google Scholar]
- 32.Al-Hayani AA, Hamdy RM, Abd El-Aziz GS, Badawoud MH, Aldaqal S, Bedir Y. Shellac: A Non-Toxic Preservative for Human Embalming Techniques. Journal of Animal and Veterinary Advances. 2011;10(12):1561–7. [Google Scholar]
- 33.Dixit D. Role of Standardized Embalming Fluid in Reducing the Toxic Effect of Formaldehyde. Indian Journal of Forensic Medicine & Toxicology. 2008;2(1):33–9. [Google Scholar]
- 34.Kawamata S, Kodera H. Reduction of formaldehyde concentrations in the air and cadaveric tissues by ammonium carbonate. Anat Sci Int. 2004;79(3):152–7. doi: 10.1111/j.1447-073x.2004.00075.x. [DOI] [PubMed] [Google Scholar]
- 35.Coleman R, Kogan I. An improved low-formaldehyde embalming fluid to preserve cadavers for anatomy teaching. J Anat. 1998;192(Pt 3):443–6. doi: 10.1046/j.1469-7580.1998.19230443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]