INTRODUCTION
Omega-3 fatty acids are among the most commonly prescribed supplements with a remarkable worldwide market. In 2011, people spent around $25 billion on omega-3 supplements. This amount is estimated to approach $35 billion in 2016 (1). While these supplements have been tried in various medical conditions including gastrointestinal, rheumatic, psychiatric, metabolic, renal, dermatologic, and pulmonary problems, they have been most commonly used for primary and secondary prevention of cardiovascular disease (CVD) (2–13).
Structure, Sources, and Biosynthesis
Omega-3 fatty acids are a group of poly-unsaturated fatty acids with multiple double bonds, with the first being on the third carbon counting from the methyl end (omega carbon) of the chain (14). The major types of long chain omega-3 fatty acids include eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) with 20 and 22 carbons, respectively. EPA and DHA are mainly gained from seafood consumption. Small amounts of EPA and DHA can also be synthesized in the body using alpha linolenic acid (ALA), an 18-carbon omega-3 fatty acid found in plants such as flaxseed, canola and walnuts (15). Docosapentaenoic acid (DPA) is another long chain omega-3 fatty acid and a metabolite of DHA thought to be formed through the internal metabolic pathways rather than dietary intake.
Molecular and Cellular Effects of Omega-3 Fatty Acids
The composition of lipids in the cell membrane affects multiple cellular functions. Animal studies show that adding omega-3 fatty acids to cell membrane can alter cellular function by interaction with and modulation of membrane channels and proteins; thereby changing the physiochemical properties of cell membrane. Membrane-incorporated omega-3 fatty acids might be able to alter membrane protein signaling. Also, the integration of omega-3 fatty acids into cell membrane in animal studies resulted in changes in H-Ras signaling protein and suppressed protein kinase C-theta signaling (15).
Omega-3 fatty acids exert anti-inflammatory properties through different mechanisms. Some animal studies show that omega-3 fatty acids can suppress the production of interleukin-2 and inhibit lipopolysaccharide-induced inflammation (15). They also bind to specific nuclear receptors and transcription factors such as PPAR-α, HNF-4α and SREBP-1c that regulate gene expression (15). The rapid modulation of transcription can directly impact the inflammatory pathways. Furthermore, omega-3 fatty acids suppress the acute phase reactants (16). Omega-3 fatty acids also modify the production of eicosanoids (such as reducing the levels of thromboxane A2 and leukotriene B4); thereby leading to reduced inflammation. It has been hypothesized that such anti-inflammatory properties may reduce vascular atherogenic inflammation (15).
Some studies, however, have questioned the effect of omega-3 fatty acids on inflammation. In a rat model of spinal cord injury, EPA and DHA administration could not reverse the hepatic inflammatory response induced by laminectomy or spinal cord injury. The study showed some anti-inflammatory effects for DHA, but none for EPA (17). In a trial of 20 healthy athletes, daily supplementation with 3.6 grams of omega-3 fatty acids for 6 weeks did not alter cytokine response to strenuous exercise; nor did it change the blood concentrations of neutrophils and lymphocytes (18).
Omega-3 fatty acids may also lead to improved endothelial function by promoting the release of nitric oxide from endothelial cells (19). Omega-3 fatty acids also decrease resting systolic and diastolic blood pressure by incorporation of EPA and DHA into membrane phospholipids and therefore increasing systemic arterial compliance (19).
Omega-3 fatty acids are also considered anti-thrombotic at very high doses, potentially increasing the bleeding time (20). This might be explained by the ability of omega-3 fatty acids to inhibit platelets. EPA and DHA can lower tissue levels of arachidonic acid and replace it in cell membrane. EPA-derived eicosanoids are less vasoconstrictive and lead to less platelet aggregating effects than those derived from arachidonic acid (21). In contrast to arachidonic acid that is metabolized to thromboxane A2, omega-3 fatty acids are metabolized to thromboxane A3, which is not as potent as thromboxane A2 in activating platelets and triggering vasoconstriction (20). However, human trials are not suggestive of a consistent effect on coagulation factors and platelet aggregation, at least for commonly prescribed doses of omega-3 fatty acids (15).
Omega-3 fatty acids might directly influence heart rate because they can inhibit myocyte voltage-gated sodium channels and prolong the relative refractory period. Therefore, higher voltages will be required to depolarize the cell membrane and the heart rate will decrease (19).
Effects on CVD Risk Factors
It is well established that omega-3 fatty acids decrease serum levels of triglycerides, partly through reduced hepatic synthesis of very low-density lipoprotein and partly by boosting the degradation of fatty acids and accelerating triglyceride clearance from the plasma (15, 22).
With regard to their effects on lipoproteins, randomized controlled trials have yielded mixed results. Most trials using DHA have shown an increase in low-density lipoprotein; while this happened in less than half of the trials using EPA (22). High-density lipoprotein has been shown to increase in most patients using DHA supplementation; however, the response to EPA supplementation has been variable (22).
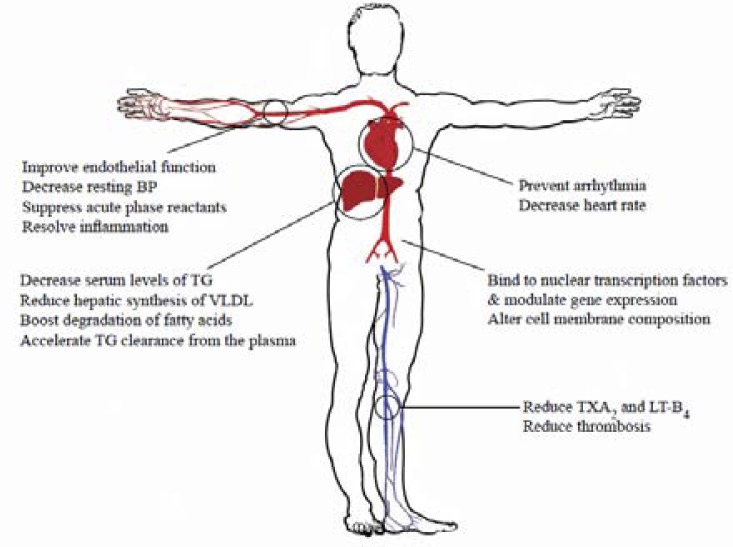
Some studies have shown the effect of omega-3 fatty acid supplements on improving flow-mediated arterial dilation and improvement of the mechanical function of the heart (Figure 1) (15, 19).
Figure 1.
Possible Effects of Omega-3 Fatty Acids on Cardiovascular Risk.
Mediterranean Diet, Fatty fish and Heart Disease
Large population-based studies have shown that consuming boiled or baked fish, is strongly associated with reduced heart rate and systemic vascular resistance and lower incidence of ischemic heart disease and heart failure (23–25).
Dietary guidelines offered by the American Heart Association recommend the consumption of a variety of fish (preferably oily fish such as salmon, herring, and mackerel) at least twice a week (26). There is consistent evidence of benefits of fish consumption for cardiovascular health. Modest consumption of fish (e.g. 1-2 servings per week), especially species higher in EPA and DHA is associated with reduced risk of coronary death and total mortality (27).
Fish and other seafood are a major component of the Mediterranean diet. This diet is also rich in olive oil, fruits and vegetables, nuts, and cereals; besides a moderate consumption of poultry as well as a low intake of red meat, processed milk and dairy products (28).
Multiple studies have suggested benefits for Mediterranean diet in reducing CVD risk factors (28). More importantly, a recent primary prevention randomized trial of over 7000 people with high risk of vascular events showed that the Mediterranean diet supplemented with extra virgin olive oil, or with nuts, can reduce the rate of major cardiovascular events including myocardial infarction (MI), stroke and death from cardiovascular causes (28).
Omega-3 Supplements
Omega-3 products are mostly available as over the counter supplements, but a few such as icosapent ethyl (Vascepa®) and EPA & DHA ethyl esters (Lovaza®) are prescription drugs. Over the past 2 decades multiple randomized trials have evaluated the efficacy of omega-3 supplements in various cardiovascular conditions, and have yielded mixed results.
Some trials have investigated the impact of omega-3 supplementation on decreasing cardiovascular events and mortality among patients with a history of MI or chronic heart failure. (Table 1) (29–33); whereas others have determined their efficacy in mixed secondary prevention settings.
Table 1.
Trials investigating the role of omega-3 supplementation in decreasing cardiovascular events after acute coronary syndromes.
| Study | Patients Characteristics | Median age (years) | Omega-3 dose g/day | Control | Duration (years) | Number of controls | Number of controls | Number of controls | Outcomes assessed | Effect size |
|---|---|---|---|---|---|---|---|---|---|---|
| GISSI-Prevenzione Investigators (30) | With history of MI | 59.4 (mean) | 1 | None | 3.5 | 2828 | 2828 | 2828 | All-cause mortality, MI, stroke | RR 0.80 [95% CI 0.67-0.94] for all-cause mortality |
| Galan et al (29) | With history of MI, unstable angina, ischemic stroke | 61 | 0.6 | Placebo | 4.7 | 626 | 626 | 626 | All-cause mortality, MI, stroke | HR 1.03 [95% CI 0.72-1.48] P = 0.88 for all-cause mortality |
| Kromhout et al (31) | With history of MI | 69 | 0.4 | Placebo | 3.3 | 1236 | 1236 | 1236 | Cardiovascular events and mortality, cardiac interventions | HR 1.01 [95% CI 0.87-1.17] P = 0.93 for major cardiovascular events |
| Rauch et al (32) | With history of MI | 64 | 1 | Placebo | 1 | 1893 | 1893 | 1893 | All-cause mortality, sudden cardiac death | OR 1.25 [95% CI 0.90-1.72] P = 0.18 for all-cause mortality |
MI: myocardial infarction, CVD: cardiovascular diseases, RR: relative risk, HR: hazard ratio, OR: odds ratio, CI: confidence interval
Four trials studied patients with history of acute coronary syndromes. An open-label randomized controlled trial in the pre-statin era in Italy demonstrated that supplementation with 1 gram per day omega-3 significantly decreased combined primary endpoint of death, non-fatal MI, and non-fatal stroke among 2836 patients over a median follow up period of 42 months (30). A double blind, randomized, placebo controlled trial in France found no significant decrease in major cardiovascular events including cardiovascular mortality among 633 patients following the daily consumption of 600 mg omega-3 supplement for a median period of 4.7 years (29). Another randomized double blind placebo controlled trial in the Netherlands showed that supplementation with an average of 226 mg EPA and 150 mg DHA per day did not significantly reduce the incidence of major cardiovascular events among 1192 patients during a period of 40 months (31). The OMEGA, (a randomized, double blind placebo controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction) in Germany found no additional protection against sudden cardiac death and other cardiovascular events among 1925 patients treated with guideline-adjusted treatment of acute MI plus 1 gram omega-3 per day for one year (32).
In the context of heart failure, a randomized double-blind placebo-controlled trial in Italy showed a slight decrease in the risk of CVD mortality and hospital admissions due to cardiovascular reasons following daily consumption of 1 gram of omega-3 supplement for a median period of 3.9 years among 3494 patients (33). However, surprising for a well-designed randomized trial, the study endpoints reached statistically significant differences across the arms only after adjustment for imbalances in baseline characteristics.
Electrophysiological effects of omega-3 fatty acids on animal myocytes are suggestive of their anti- arrhythmic properties; but human trials concerning arrhythmia show conflicting results (15). Multiple clinical trials have tried to determine the clinical utility of such presumable electrophysiological properties; while a trial of 205 patients with atrial fibrillation (AF) showed that 1 year supplementation with a daily dose of 2 grams omega-3 helped maintain sinus rhythm after direct current cardioversion, two other trials among 586 patients with AF and 546 patients with implantable cardioverter defibrillators and history of malignant ventricular tachycardia or ventricular fibrillation did not show a decrease in recurrent AF and tachyarrhythmia after nearly a year of supplementation with 1 and 2 grams omega-3 supplements, respectively (34–36).
There are no pure primary prevention trials to have tested the impact of omega-3 supplements on hard endpoints. However, a trial of 328 healthy individuals aged 18 to 37 years in England showed that despite lower levels of serum triglycerides and very low-density lipoprotein, no improvement in endothelial function occurred after supplementation with 1.6 gram DHA for 16 weeks.
Net Benefit
As summarized above, results of multiple prior randomized trials were mixed, with some suggestive of cardiovascular benefits for omega-3 supplements and some not confirming their efficacy. To address this important clinical dilemma, a recent systematic review investigated all randomized trials that were completed about the cardiovascular effects of omega-3 supplementation in adult participants between 1989 and 2012 (37). This review included 20 studies of a total of 68,680 randomized patients. The median follow-up period for these trials was 2 (1.0-6.2) years, and half of the included trials had been conducted during the period when statins were routinely recommended for cardiovascular risk modification (i.e. 1998 or later). The study showed that omega-3 fatty acids were not associated with significant decrease or increase in all-cause mortality (relative risk [RR]= 0.96; 95% confidence interval: 0.91-1.02; risk reduction: −0.004, 95% confidence interval: −0.01 to 0.02), sudden death, MI, or stroke (37). Another recent systematic review by Kotwal et al, also showed that omega-3 supplementation was not associated with a significant reduction in composite cardiovascular endpoints (RR=0.96; 95% confidence interval: 0.90-1.03; P=0.24)(38).
Since publication of these systematic reviews, 3 additional trials have been published. OPERA (the Omega-3 Fatty Acids for Prevention of Post-operative Atrial Fibrillation), a double-blind placebo-controlled randomized trial; which was published later, investigated the effects of perioperative omega-3 supplementation on postoperative atrial fibrillation (AF) among patients undergoing cardiac surgery. The results showed no significant decrease of the risk of postoperative AF by omega-3 supplements compared with placebo (39). This finding is compatible with that of Kowey et al, who investigated more than 600 patients with AF in a randomized double blind placebo controlled trial. In their study, a 24-week treatment with omega-3 supplements did not decrease the rate of recurrent AF (40). Finally, another double-blind placebo-controlled clinical trial investigated the effects of omega-3 supplementation on a cohort of more than 12,500 patients with multiple cardiovascular risk factors or atherosclerotic vascular disease with no history of MI. After a median of 5 years of follow up, daily supplementation with 1 gram omega-3 fatty acids did not reduce the incidence of the study’s primary endpoint, defined as time to death from cardiovascular causes or hospital admission due to cardiovascular causes (41).
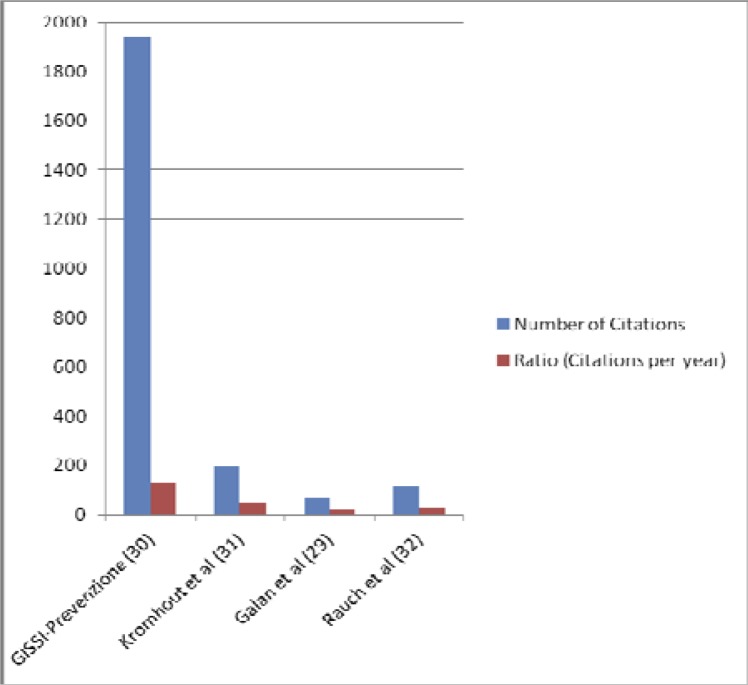
Considering the benefits of omega-3 fatty acids on CVD risk factors, how can we justify the conflicting and uncertain effect of omega-3 supplements on hard cardiovascular endpoints? There could be several explanations. First, publication bias, selective reporting, or even selective citation in favor of studies suggestive of beneficial effects of omega-3 fatty acids on CVD risk factors is possible. For example, the positive GISSI-Prevenzione trial (30) has been much more frequently cited compared with similar trials that yielded negative results (Figure 2).
Figure 2.
Comparison of citations to trials with positive and negative results.
In other words, it is possible that the presumed basic and clinical benefits of these supplements are less robust than widely thought. However, due to selective reporting, publication bias, or selective citation, positive studies get more popularized. Second, it has been known that improving a risk factor would not necessarily lead to an improvement in hard endpoints such as mortality (42). In fact, it might be reductionist to consider fatty fish identical to omega-3 fatty acids, as some authors do. Fish may contain many more active ingredients that we are not yet fully aware of. Aside from omega-3 fatty acids, fish would contain other proteins, vitamin D, selenium, and several mineral elements. A recent systematic review of 26 prospective cohort studies and 12 randomized controlled trials determined the association between fish consumption and also omega-3 supplements with cerebrovascular diseases including ischemic and hemorrhagic stroke, or transient ischemic attack with aggregate data on 794,000 non-overlapping people (43). The systematic review indicated that although consumption of fish had a moderate inverse association with the risk of cerebrovascular events, there was no such association between circulating levels of omega-3 fatty acids and supplements with cerebrovascular diseases (43).
Financial and Safety Issues
The widespread use of omega-3 supplements implies huge financial expenditure on products of dubious benefits (44). Furthermore, contrary to the common public belief, supplements are not necessarily devoid of harm (45, 46). One potential safety concern with omega-3 supplement use is the risk for hemorrhagic stroke. At very high doses (e.g. 15 grams per day), omega-3 fatty acids increase bleeding time (15). In a randomized trial of more than 18,600 hypercholesterolemic Japanese patients for supplementation with 1.8 gram per day of EPA (the JELIS trial) the adverse experience of hemorrhage (cerebral, fundal, epistaxis, and subcutaneous) was significantly more frequent among the patients in supplement group and though not significant, the incidence of hemorrhagic stroke was also higher (47). In a secondary prevention trial with 1.7 gram per day omega-3 supplementation among patients undergoing regular hemodialysis, reported cases of bleeding (including gastrointestinal, cerebral, and other) were 15 among 103 patients in treatment group versus 7 among 103 patients in control group (48). Numerically higher cerebrovascular events were also observed in GISSI-HF and OMEGA trials among patients using supplements (32, 33). Although not significant, GISSI-Prevenzione trial also showed a trend toward excess strokes in the omega-3 arm (30). The systematic review by Chowdhury et al. showed that in secondary prevention trials cerebrovascular events were more common among participants in the supplement group than the control group (43).
CONCLUSIONS
Despite the abundance of studies concerning omega-3 supplements, evidence is not clear about the benefits of these supplements, with both positive and negative trials. One potential challenge over the past several years has been the reporting of positive pieces of evidence by both industry and pro-omega-3 nutritionists/academics while undervaluing the equally robust, if not more robust, negative studies. Also, these products might not be free from risk and the particular risks for bleeding and hemorrhagic stroke deserve further attention.
In summary and in light of the current best evidence, we can conclude that omega-3 supplements might possibly confer cardiovascular benefits but their benefits will be minimal, if any. We are also unsure if there is a subset of patients that would benefit most from this supplementation. Further ongoing investigations could be helpful in that regard. And finally, would the current best evidence lend support to widespread use of omega-3 supplements for primary or secondary CVD prevention? Our answer given the existing evidence would be “no”. Why not starting with the well-balanced Mediterranean diet, instead?
Acknowledgements
We would like to thank Seyed-Mohammad Abooturabi, MD for his precious help on this manuscript.
Disclosures: None
REFERENCES
- 1.Schultz H. Retail omega-3s sales to hit $34.7 billion in 2016, report predicts. 2012. [cited 2013 September 17]; Available from: http://www.nutraingredients-usa.com/Markets/Retail-omega-3s-sales-to-hit-34.7-billion-in-2016-report-predicts.
- 2.Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis. Mol Psychiatry. 2012;17(12):1272–82. doi: 10.1038/mp.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cabré E, Mañosa M, Gassull MA. Omega-3 fatty acids and inflammatory bowel diseases - a systematic review. Br J Nutr. 2012;107(Suppl 2):S240–52. doi: 10.1017/S0007114512001626. [DOI] [PubMed] [Google Scholar]
- 4.Friedman A, Moe S. Review of the effects of omega-3 supplementation in dialysis patients. Clin J Am Soc Nephrol. 2006;1(2):182–92. doi: 10.2215/CJN.00740805. [DOI] [PubMed] [Google Scholar]
- 5.Gerber M. Omega-3 fatty acids and cancers: a systematic update review of epidemiological studies. Br J Nutr. 2012;107(Suppl 2):S228–39. doi: 10.1017/S0007114512001614. [DOI] [PubMed] [Google Scholar]
- 6.Knapp HR. Omega-3 fatty acids in respiratory diseases: a review. J Am Coll Nutr. 1995;14(1):18–23Suppl 2. doi: 10.1080/07315724.1995.10718468. [DOI] [PubMed] [Google Scholar]
- 7.Wu JH, Micha R, Imamura F, Pan A, Biggs ML, Ajaz O, et al. Omega-3 fatty acids and incident type 2 diabetes: a systematic review and meta-analysis. Br J Nutr. 2012;107(Suppl 2):S214–27. doi: 10.1017/S0007114512001602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Filion KB, El Khoury F, Bielinski M, Schiller I, Dendukuri N, Brophy JM. Omega-3 fatty acids in high-risk cardiovascular patients: a meta-analysis of randomized controlled trials. BMC Cardiovasc Disord. 2010;10:24. doi: 10.1186/1471-2261-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsuyama W, Mitsuyama H, Watanabe M, Oonakahara K, Higashimoto I, Osame M, et al. Effects of omega-3 polyunsaturated fatty acids on inflammatory markers in COPD. Chest. 2005;128(6):3817–27. doi: 10.1378/chest.128.6.3817. [DOI] [PubMed] [Google Scholar]
- 10.Giudetti AM, Cagnazzo R. Beneficial effects of n-3 PUFA on chronic airway inflammatory diseases. Prostaglandins Other Lipid Mediat. 2012;99(3-4):57–67Suppl 2. doi: 10.1016/j.prostaglandins.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Miles EA, Calder PC. Influence of marine n-3 polyunsaturated fatty acids on immune function and a systematic review of their effects on clinical outcomes in rheumatoid arthritis. Br J Nutr. 2012;107(Suppl 2):S171–84. doi: 10.1017/S0007114512001560. [DOI] [PubMed] [Google Scholar]
- 12.Zheng JS, Hu XJ, Zhao YM, Yang J, Li D. Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies. BMJ. 2013;346:f3706. doi: 10.1136/bmj.f3706. [DOI] [PubMed] [Google Scholar]
- 13.Zulfakar MH, Edwards M, Heard CM. Is there a role for topically delivered eicosapentaenoic acid in the treatment of psoriasis? Eur J Dermatol. 2007;17(4):284–91. doi: 10.1684/ejd.2007.0201. [DOI] [PubMed] [Google Scholar]
- 14.Weylandt KH, Chiu CY, Gomolka B, Waechter SF, Wiedenmann B. Omega-3 fatty acids and their lipid mediators: towards an understanding of resolvin and protectin formation. Prostaglandins Other Lipid Mediat. 2012;97(3-4):73–82. doi: 10.1016/j.prostaglandins.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011;58(20):2047–67. doi: 10.1016/j.jacc.2011.06.063. [DOI] [PubMed] [Google Scholar]
- 16.Adkins Y, Kelley DS. Mechanisms underlying the cardioprotective effects of omega-3 polyunsaturated fatty acids. J Nutr Biochem. 2010;21(9):781–92. doi: 10.1016/j.jnutbio.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 17.Weylandt KH, Chiu CY, Gomolka B, Waechter SF, Wiedenmann B. Omega-3 fatty acids and their lipid mediators: towards an understanding of resolvin and protectin formation. Prostaglandins Other Lipid Mediat. 2012;97(3-4):73–82. doi: 10.1016/j.prostaglandins.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Toft AD, Thorn M, Ostrowski K, Asp S, Moller K, Iversen S, et al. N-3 polyunsaturated fatty acids do not affect cytokine response to strenuous exercise. J Appl Physiol (1985) 2000;89(6):2401–6. doi: 10.1152/jappl.2000.89.6.2401. [DOI] [PubMed] [Google Scholar]
- 19.Massaro M, Scoditti E, Carluccio MA, De Caterina R. Basic mechanisms behind the effects of n-3 fatty acids on cardiovascular disease. Prostaglandins Leukot Essent Fatty Acids. 2008;79(3-5):109–15. doi: 10.1016/j.plefa.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Cohen MG, Rossi JS, Garbarino J, Bowling R, Motsinger-Reif AA, Schuler C, et al. Insights into the inhibition of platelet activation by omega-3 polyunsaturated fatty acids: beyond aspirin and clopidogrel. Thromb Res. 2011;128(4):335–40. doi: 10.1016/j.thromres.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 21.Harris WS, Miller M, Tighe AP, Davidson MH, Schaefer EJ. Omega-3 fatty acids and coronary heart disease risk: clinical and mechanistic perspectives. Atherosclerosis. 2008;197(1):12–24. doi: 10.1016/j.atherosclerosis.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Jacobson TA, Glickstein SB, Rowe JD, Soni PN. Effects of eicosapentaenoic acid and docosahexaenoic acid on low-density lipoprotein cholesterol and other lipids: a review. J Clin Lipidol. 2012;6(1):5–1 8. doi: 10.1016/j.jacl.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 23.Mozaffarian D, Bryson CL, Lemaitre RN, Burke GL, Siscovick DS. Fish intake and risk of incident heart failure. J Am Coll Cardiol. 2005;45(12):2015–21. doi: 10.1016/j.jacc.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 24.Mozaffarian D, Gottdiener JS, Siscovick DS. Intake of tuna or other broiled or baked fish versus fried fish and cardiac structure, function, and hemodynamics. Am J Cardiol. 2006;97(2):216–22. doi: 10.1016/j.amjcard.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 25.Mozaffarian D, Prineas RJ, Stein PK, Siscovick DS. Dietary fish and n-3 fatty acid intake and cardiac electrocardiographic parameters in humans. J Am Coll Cardiol. 2006;48(3):478–84. doi: 10.1016/j.jacc.2006.03.048. [DOI] [PubMed] [Google Scholar]
- 26.Kris-Etherton PM, Harris WS, Appel LJ, American Heart Association. Nutrition Committee Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002;106(21):2747–57. doi: 10.1161/01.cir.0000038493.65177.94. [DOI] [PubMed] [Google Scholar]
- 27.Mozaffarian D, Rimm EB. Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA. 2006;296(15):1885–99. doi: 10.1001/jama.296.15.1885. [DOI] [PubMed] [Google Scholar]
- 28.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 29.Galan P, Kesse-Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg S, et al. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo controlled trial. BMJ. 2010;341:c6273. doi: 10.1136/bmj.c6273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto miocardico. Lancet. 1999;354(9177):447–55. [PubMed] [Google Scholar]
- 31.Kromhout D, Giltay EJ, Geleijnse JM, Alpha Omega Trial Group n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med. 2010;363(21):2015–26. doi: 10.1056/NEJMoa1003603. [DOI] [PubMed] [Google Scholar]
- 32.Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, et al. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation. 2010;122(21):2152–9. doi: 10.1161/CIRCULATIONAHA.110.948562. [DOI] [PubMed] [Google Scholar]
- 33.Tavazzi L, Maggioni AP, Marchioli R, Barlera S, Franzosi MG, Latini R, et al. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372(9645):1223–30. doi: 10.1016/S0140-6736(08)61239-8. [DOI] [PubMed] [Google Scholar]
- 34.Nodari S, Triggiani M, Campia U, Manerba A, Milesi G, Cesana BM, et al. n-3 polyunsaturated fatty acids in the prevention of atrial fibrillation recurrences after electrical cardioversion: a prospective, randomized study. Circulation. 2011;124(10):1100–6. doi: 10.1161/CIRCULATIONAHA.111.022194. [DOI] [PubMed] [Google Scholar]
- 35.Macchia A, Grancelli H, Varini S, Nul D, Laffaye N, Mariani J, et al. Omega-3 fatty acids for the prevention of recurrent symptomatic atrial fibrillation: results of the FORWARD (Randomized Trial to Assess Efficacy of PUFA for the Maintenance of Sinus Rhythm in Persistent Atrial Fibrillation) trial. J Am Coll Cardiol. 2013;61(4):463–8. doi: 10.1016/j.jacc.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 36.Brouwer IA, Zock PL, Camm AJ, Böcker D, Hauer RN, Wever EF, et al. Effect of fish oil on ventricular tachyarrhythmia and death in patients with implantable cardioverter defibrillators: the Study on Omega-3 Fatty Acids and Ventricular Arrhythmia (SOFA) randomized trial. JAMA. 2006;295(22):2613–9. doi: 10.1001/jama.295.22.2613. [DOI] [PubMed] [Google Scholar]
- 37.Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS. Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis. JAMA. 2012;308(10):1024–33. doi: 10.1001/2012.jama.11374. [DOI] [PubMed] [Google Scholar]
- 38.Kotwal S, Jun M, Sullivan D, Perkovic V, Neal B. Omega 3 Fatty acids and cardiovascular outcomes: systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2012;5(6):808–18. doi: 10.1161/CIRCOUTCOMES.112.966168. [DOI] [PubMed] [Google Scholar]
- 39.Mozaffarian D, Marchioli R, Macchia A, Silletta MG, Ferrazzi P, Gardner TJ, et al. Fish oil and postoperative atrial fibrillation: the Omega-3 Fatty Acids for Prevention of Post-operative Atrial Fibrillation (OPERA) randomized trial. JAMA. 2012;308(19):2001–11. doi: 10.1001/jama.2012.28733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kowey PR, Reiffel JA, Ellenbogen KA, Naccarelli GV, Pratt CM. Efficacy and safety of prescription omega-3 fatty acids for the prevention of recurrent symptomatic atrial fibrillation: a randomized controlled trial. JAMA. 2010;304(21):2363–72. doi: 10.1001/jama.2010.1735. [DOI] [PubMed] [Google Scholar]
- 41.Risk and Prevention Study Collaborative Group. Roncaglioni MC, Tombesi M, Avanzini F, Barlera S, Caimi V, Longoni P, et al. n-3 fatty acids in patients with multiple cardiovascular risk factors. N Engl J Med. 2013;368(19):1800–8. doi: 10.1056/NEJMoa1205409. [DOI] [PubMed] [Google Scholar]
- 42.Bikdeli B, Barreto-Filho JA. Reducing the cardiovascular disease burden: justified means for getting to the end. Circ Cardiovasc Qual Outcomes. 2012;5(4):580–6. doi: 10.1161/CIRCOUTCOMES.111.964072. [DOI] [PubMed] [Google Scholar]
- 43.Chowdhury R, Stevens S, Gorman D, Pan A, Warnakula S, Chowdhury S, et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: systematic review and meta-analysis. BMJ. 2012;345:e6698. doi: 10.1136/bmj.e6698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kennedy ET, Luo H, Ausman LM. Cost implications of alternative sources of (n-3) fatty acid consumption in the United States. J Nutr. 2012;142(3):605S–609. doi: 10.3945/jn.111.152736. [DOI] [PubMed] [Google Scholar]
- 45.Kuehn BM. Dietary supplement linked to cases of acute hepatitis. JAMA. 2013;310(17):1784. doi: 10.1001/jama.2013.281868. [DOI] [PubMed] [Google Scholar]
- 46.Xiao Q, Murphy RA, Houston DK, Harris TB, Chow WH, Park Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2013;173(8):639–46. doi: 10.1001/jamainternmed.2013.3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369(9567):1090–8. doi: 10.1016/S0140-6736(07)60527-3. [DOI] [PubMed] [Google Scholar]
- 48.Svensson M, Schmidt EB, Jørgensen KA, Christensen JH. N-3 fatty acids as secondary prevention against cardiovascular events in patients who undergo chronic hemodialysis: a randomized, placebo-controlled intervention trial. Clin J Am Soc Nephrol. 2006;1(4):780–6. doi: 10.2215/CJN.00630206. [DOI] [PubMed] [Google Scholar]